1. Introduction
The skin operates as a complex ecosystem, providing a multi-component habitat with its folds, invaginations, and lesions that support a diverse range of microorganisms. The composition of the skin microbiota varies by body site and includes different types of organisms, such as bacteria (like Proteobacteria, Corynebacterium, and Staphylococcus species), fungi (such as Malassezia), and viruses (for instance, Capripox) [
1]. A healthy skin microbiota is crucial for maintaining skin health. It occupies sites where pathogens could adhere and produces variety of substances that inhibit pathogen growth.
Numerous pathogens, including bacteria, viruses, fungi, and parasites, can induce skin infections in domestic and wild ruminants. Commonly encountered infections include dermatophilosis (rain scald), ringworm (dermatophytosis), lumpy skin disease, sheep pox, goat pox, as well as parasitic infestations like mange, lice and warble fly (hypodermosis genus
Hypoderma). Other prevalent conditions in large ruminants include digital dermatitis in dairy cattle and papillomatosis [
2,
3,
4,
5].
European bison (
Bison bonasus) generally demonstrate robust health and a pronounced capacity to withstand many common diseases. This resilience is likely attributable to their immune system, along with the fact that they are not prone to diseases that commonly affect domestic cattle. However, when the immune system becomes compromised, certain pathogens may exploit this opportunity to induce disease. Documented cases of skin diseases, such as bovine papillomatosis and digital dermatitis, have been observed in captive European bison [
6,
7].
It is important to note that bacterial skin diseases in both domestic and wild ruminants are frequently underdiagnosed. Specific risk factors that compromise the skin’s barrier can allow opportunistic pathogens to proliferate, potentially leading to the onset of disease. Disruption of skin integrity can lead to various skin and soft tissue infections, such as impetigo, cellulitis, folliculitis, furunculosis, and others [
8,
9,
10] reveals that dermal wounds can be colonized by a combination of aerobic bacteria, primarily
Staphylococcus and
Streptococcus spp., as well as anaerobic bacteria such as
Corynebacterium and
Trueperella spp. Among the most commonly isolated bacterial pathogens responsible for skin diseases in animals are staphylococci. Research on wild animals such as red deer, roe deer, and squirrels has confirmed that staphylococci are causative agents of dermatitis, with
Staphylococcus aureus being the most frequently isolated species [
8,
11,
12].
European bison were successfully reintroduced to the Rhodope Mountains in 2013, and their population has been gradually increasing since then. Until 2019, the bison lived in a closed area. That year, they were released into a free-range environment covering 4,000 hectares. As of 2025, the wild population has surpassed 22 individuals.
Case history: On August 13, 2019, the herd made its way down from the mountain in the Studen Kladenets Game Reserve area where they were first brought. Almost all animals were found to have a high tick infestation. Two of the females (one with a calf about three months old) showed weakness and unsteady gait. The condition progressed to lack of coordination and recumbency. According to the local veterinarian, the most likely diagnosis is tick paralysis. All animals in the herd were treated pour-on with deltamethrin (Spotinor® Norbrook), and the sick ones were also treated injectable with ivermectin (Kepromec® Kepro) and tetracycline antibiotic (Tetravet® Ceva). The condition of all animals is gradually improving.
The female calf named Bebsi, born on May 11, 2019, with а pedigree number 14407, has a severe hair loss and scabs. Attempts to treat with ivermectin did not yield results, so a sample of scraped material (crusts and hairs) was obtained for laboratory testing. The result obtained by the laboratory was negative for scabies and ringworm. The condition progresses to involve large parts of the body, which corresponds to decreased appetite and subsequent weight loss.
In early November, reduced solar radiation lowers temperatures as the days grow shorter. The atmospheric conditions contribute to frequent fog and rainfall. During the regular rounds to inspect the herd, the bison calf was found in the mud, unable to stand. The adult herdmates surrounded and guarded it. With great effort, the calf was carefully placed in a car and then moved to a barn (
Figure 1). There, it was warmed and fed by hand. On November 23, 2019, a veterinarian from the Faculty of Veterinary Medicine at Trakia University visited the site.
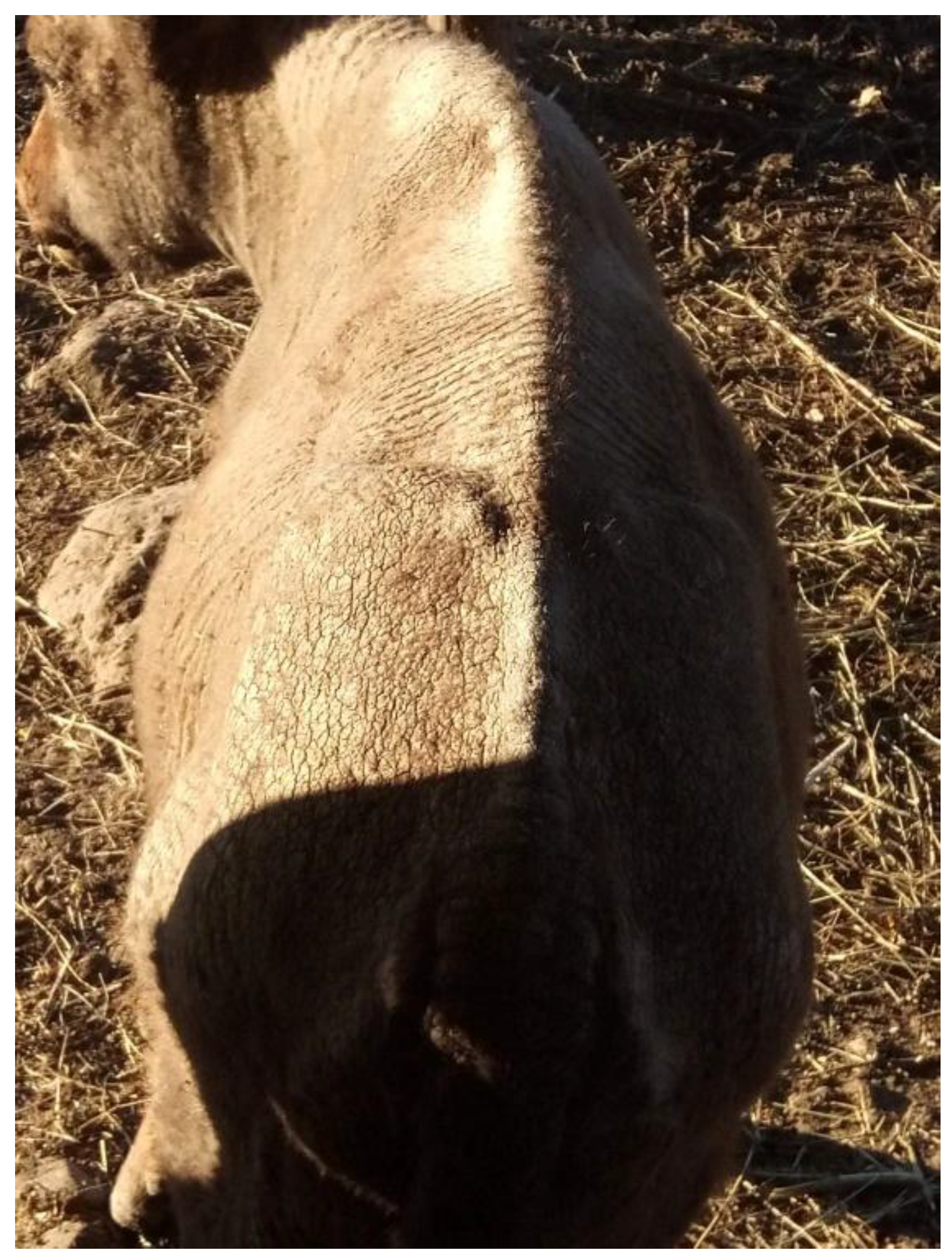
Physical examination: During the general examination, normal temperature, pulse, and respiration were observed, and the calf was alert and interested in both food and its surroundings. Significant changes were observed on the skin, described as generalized dermatitis with alopecia, and crusting. The condition affects multiple regions of the integument, such as the face, neck, back, flanks, limbs, and perineal area. The skin appears flaky, dry, rough, covered with thick crusts and the lesions were not found to cause itching (
Figure 2). Upon removal, inflamed, edematous, and oozing lesions are revealed underneath.
2. Diagnostic Methods, and Laboratory Findings
No bacteriological investigations were conducted previously. During the visit, swab samples were collected for bacteriological investigations from the lesions after the removal of crusts by using a sterile scalpel blade and tweezers. Samples were transported to the laboratory using a cool box filled with cool packs. A conventional microbiological tests were performed, including inoculations of liquid broth media (Tryptone Soy Broth, Oxoid™), as well as culturing on solid nutrient media (Blood Agar Base and MacConkey, Oxoid™), incubated at 37° for 48 hours. At 24 hours of incubation, two different staphylococcal bacteria were isolated. The primary growth consisted of round, raised, opaque colonies that were yellow to golden yellow, measuring 1-2 mm in diameter. These colonies, exhibiting clear beta-hemolysis zones and were later determined to be coagulase-positive. In contrast, the other isolate displayed small, white, opaque, flat, non-hemolytic colonies, also 1-2 mm in diameter. The tube coagulase test for this strain was negative. Microscopic examination revealed that both isolates were composed of similar Gram-positive spherical cells arranged in tetrads or clusters. Further identification of the isolates was subsequently performed using the Vitek 2 system (BioMérieux Inc., Durham, NC) using GP ID cards. Vitek 2 GP card analysis confirmed the isolates as Staphylococcus aureus and Staphylococcus epidermidis, respectively. The antibiotic susceptibility test using the AST-P506 card on the Vitek 2 system showed that the S. aureus strain is sensitive to amoxicillin, benzylpenicillin, cefotaxime, ceftriaxone, chloramphenicol, erythromycin, imipenem, ofloxacin, pristinamycin, trimethoprim-sulfamethoxazole, and vancomycin, and resistant to tetracycline. The S. epidermidis strain was sensitive to all antibiotics tested.
Treatment: When a definitive diagnosis was made, evidence-based therapy was initiated. The treatment of the bison calf was adapted according to the results of in vitro susceptibility testing of the two isolated staphylococci. For this purpose, amoxicillin was administered at a dose of 15 mg/kg of body weight via the intramuscular route. The initial attempts at injection were unsuccessful due to strong muscle tension and difficulties in administering the correct dosage. As a result, the route of administration was changed, and the calculated daily dose was given orally. To facilitate this, food baits made with apples and mushrooms were prepared. The treatment duration was until the skin lesions healed (> 45 days) and hair regrowth appeared (
Figure 3).
Injectable vitamins (Multivitamins® Pantex Holland) at recommended dosage were applied by subcutaneous route. Additionally, the treatment included the use of chlorhexidine solution used to soften and remove necrotic tissue, crusts, and debris. An oral supplement containing zinc (2 mg/kg/day for at least 3 weeks) and zinc oxide applied as a topical cream accompanied the treatment.
3. Discussion
The most skin diseases in wild and domestic animals are caused by a variety of pathogens, including fungi, parasites, viruses and bacteria [
13]. Bacterial dermatitis in European bison in captivity or the wild is rarely reported. Reports of digital dermatitis caused by treponema bacteria have been documented in six females and four males at Berne Animal Park [
14]. This case highlights the potential occurrence of staphylococcal dermatitis in wisent calf and underscores the importance of collecting appropriate samples for a thorough clinical workup of skin diseases in animals.
The skin changes observed during examination support a presumptive clinical diagnosis of dermatitis; however, accurate identification of the cause and appropriate treatment require in-depth laboratory testing. In this particular case, a skin infection in a bison calf was found to be associated etiologically with two types of staphylococci. Among bacterial pathogens, staphylococci are the most common cause of skin problems. Integumentary disorders due to staphylococcal infection in livestock species include folliculitis, impetigo, pyaemia, mastitis, exudative epidermitis, periorbital eczema, furunculosis, scalded skin syndrome and pyoderma [
8,
15].
S. epidermidis is a bacterium commonly found as a part of the skin microbiota in animals and humans. Rather than being a passive inhabitant, it plays an active role in supporting cutaneous immunity, preserving skin homeostasis, and inhibiting the establishment of opportunistic pathogens through competition. Increasing evidence shows, however, that
S. epidermidis displays significant strain-level diversity, and its interactions with the host range from beneficial commensalism to potential pathogenicity [
16]. In this case, considering the uncertain role of
S. epidermidis in disease and its predominantly commensal nature, we assumed that
S. aureus played the primary role in the development of dermatitis.
Most staphylococcal infections are opportunistic, arising secondary to other diseases or a compromised host immune system. Damage to the skin barrier allows commensal and pathogenic bacteria to proliferate and penetrate deeper skin layers [
17,
18]. Bacterial dermatitis may also develop in response to ectoparasite infestations, including fleas, lice, mites, and ticks [
19]. A previously negative result for scabies and ringworm could occur due to improperly selected and stored samples, treatment with ivermectin, or limitations in the laboratory’s diagnostic capabilities. Other possible disease risks may be related to immune system disorders, which can be caused by genetic factors. Due to the limited number of individuals, the European bison is considered a highly inbred species, making it more susceptible to various infectious diseases [
20]. These factors, together with other contributing elements such as moisture, traumatic injuries, and stress, form the basis for the development of staphylococcal dermatitis. In contemporary science, different risk factors are regarded as component causes that act together to form a sufficient cause capable of inducing disease [
21].
In this case, the absence of timely and appropriate therapy, attributable to an initial failure to establish an accurate etiological diagnosis, resulted in over two months of disease progression, leading to chronic, disseminated dermatological lesions and systemic manifestations including weight loss, inappetence, and lethargy. In-depth laboratory investigations, including bacteriological culture and antimicrobial susceptibility testing, are essential to guide the selection of effective therapeutic agents against bacterial pathogens, particularly in view of the prevalence of multi-drug resistant strains. The results of such testing enable the initiation of definitive therapy, thereby optimizing treatment efficacy and reducing the risk of further resistance development [
22]. The drug of choice amoxicillin is distributed well in the body and achieves effective concentrations in the skin, making it a suitable treatment agent. It is also recommended as a first-line antibiotic for canine staphylococcal dermatitis [
23]. The duration of antimicrobial therapy for bacterial skin infections should be individualized based on the severity of clinical signs, the extent and depth of lesion involvement, and the patient’s general condition. In companion animals with deep tissue integumentary diseases, full resolution may take from 4 to 6 weeks or even longer. [
23,
24]. Although numerous topical antimicrobial products are available in veterinary practice, few studies have assessed their efficacy in ruminants, with most research focused on dogs and horses. Nonetheless, topical antiseptics can be employed for their direct activity gainst pathogens responsible for bacterial and fungal skin diseases. In cattle, they are commonly applied for bovine digital dermatitis and dermatophytosis (ringworm) [
25,
26]. Due to the delicate nature of the skin, meticulous care of the affected surface is essential. Based on recommendations from human medicine, topical therapeutic interventions should be applied cautiously to prevent exacerbation of tissue damage [
27,
28].
4. Conclusions
Skin diseases in wild animals are challenging to diagnose and treatment. This case underscores the importance of laboratory testing as a cornerstone of responsible veterinary care. Rigorous health monitoring is essential for preventing infectious diseases and ensuring the success of reintroduction programs. In the vulnerable European bison population, preserving each individual is critical for the species’ survival. Effective collaboration with veterinary specialists is therefore indispensable to achieving better health outcomes and conservation success.
Author Contributions
Conceptualization, B. B.-M. and P.M.; methodology, B. B.-M. and P.M.; investigation, B. B.-M. and P.M.; resources, B. B.-M. and P.M.; writing—original draft preparation, B. B.-M. and P.M.; writing—review and editing, B. B.-M. and P.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in this case are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| GP ID |
Gramm positive identification card |
| GN ID |
Gramm negative identification card |
References
- Mala, L.; Lalouckova, K.; Skrivanova, E. Bacterial skin infections in livestock and plant-based alternatives to their antibiotic treatment. Animals 2021, 11, 2473. [Google Scholar] [CrossRef] [PubMed]
- San Miguel, J. M.; Álvarez, G.; Luzón, M. Hypodermosis of red deer in Spain. Journal of Wildlife Diseases 2001, 37, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Grice, E.A.; Segre, J.A. The skin microbiome. Nat. Rev. Microbiol. 2011, 9, 244–253. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, L. E.; Evans, N. J.; Blowey, R. W.; Grove-White, D. H.; Clegg, S. R.; Duncan, J. S.; Carter, S. D. A molecular epidemiology of treponemes in beef cattle digital dermatitis lesions and comparative analyses with sheep contagious ovine digital dermatitis and dairy cattle digital dermatitis lesions. Veterinary microbiology 2015, 178, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Ugochukwu, I. C. I.; Aneke, C. I.; Idoko, I. S.; Sani, N. A.; Amoche, A. J.; Mshiela, W. P.; Sackey, A. K. B. Bovine papilloma: Aetiology, pathology, immunology, disease status, diagnosis, control, prevention and treatment: A review. Comparative Clinical Pathology 2019, 28, 737–745. [Google Scholar] [CrossRef]
- Literák, I.; Tomita, Y.; Ogawa, T.; Shirasawa, H.; Šmid, B.; Novotný, L.; Adamec, M. Papillomatosis in a European bison. Journal of Wildlife Diseases 2006, 42, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Jucker, S.; Alsaaod, M.; Steiner, A.; Zingre, T.; Kaessmeyer, S.; Gurtner, C.; Hoby, S. Treatment of digital dermatitis using salicylic acid in European bison (Bison bonasus) reveals promising results. Frontiers in veterinary science 2022, 9, 1012226. [Google Scholar] [CrossRef] [PubMed]
- Foster, A.P. Staphylococcal skin disease in livestock. Vet. Dermatol, 3: 23. [CrossRef]
- MacInnes, J. I.; Van Immerseel, F.; Boyce, J. D.; Rycroft, A. N.; Vázquez-Boland, J. A. Pathogenesis of bacterial infections in animals. 2022, J. F. Prescott (Ed.). John Wiley & Sons, Incorporated.
- Abrahamian, F.M.; Goldstein, E.J. Microbiology of animal bite wound infections. Clin. Microbiol. Rev. 2011, 24, 231–246. [Google Scholar] [CrossRef] [PubMed]
- Monecke, S.; Gavier-Widen, D.; Hotzel, H.; Peters, M.; Guenther, S.; Lazaris, A.; Ehricht, R. Diversity of Staphylococcus aureus isolates in European wildlife. PloS one, 2016, 11, e0168433. [Google Scholar] [CrossRef] [PubMed]
- Ringwaldt, E. M.; Brook, B. W.; Carver, S.; Buettel, J. C. The patterns and causes of dermatitis in terrestrial and semi-aquatic mammalian wildlife. Animals 2021, 11, 1691. [Google Scholar] [CrossRef] [PubMed]
- Fong, I.W. Animals and Mechanisms of Disease Transmission. Emerging Zoonoses, 1: 8. [CrossRef]
- Hoby, S.; Jensen, T. K.; Brodard, I.; Gurtner, C.; Eicher, R.; Steiner, A.; Alsaaod, M. Detection of treponemes in digital dermatitis lesions of captive European bison (Bison bonasus). PLoS One, 2021, 16, e0255921. [Google Scholar] [CrossRef] [PubMed]
- Roccaro, M.; Piva, S.; Scagliarini, A.; Giacometti, F.; Serraino, A.; Merialdi, G.; Frasnelli, M. ; Romano A,.; Bellio A., Ed.; Decastelli L.; Peli A. Case report of a pustular dermatitis outbreak in sheep: Clinical and food safety considerations. Ital J Food Saf. 2018 Apr 11, 7:6980. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Severn M., M.; Horswill A., R. Staphylococcus epidermidis and its dual lifestyle in skin health and infection. Nat Rev Microbiol, 9: 21. [CrossRef] [PubMed]
- Faccin, M.; Wiener D., J.; Rech R., R.; Santoro, D.; Rodrigues Hoffmann, A. ; Common superficial and deep cutaneous bacterial infections in domestic animals: A review. Veterinary Pathology, 7: 60. [CrossRef]
- Diegel, K. L.; Andrews-Jones, L.; Wojcinski, Z. W. Integument. Haschek and Rousseaux’s Handbook of Toxicologic Pathology Volume 5: Toxicologic Pathology of Organ Systems 2025, 505-582.
- Kocoń, A.; Nowak-Chmura, M. Skin ectoparasites of domestic animals. Annales Universitatis Paedagogicae Cracoviensis Studia Naturae 2017, (2), 137–158. [Google Scholar] [CrossRef]
- Oleński, K.; Kamiński, S.; Tokarska, M.; et al. Subset of SNPs for parental identification in European bison Lowland-Białowieża line (Bison bonasus bonasus). Conservation Genet Resour. 2018, 10, 73–78. [Google Scholar] [CrossRef]
- Bhopal, R. S. Concepts of Epidemiology: Integrating the Ideas, Theories, Principles, and Methods of Epidemiology. Oxford University Press, 2016.
- Feßler, A. T.; Wang, Y.; Burbick, C. R.; Diaz-Campos, D.; Fajt, V. R.; Lawhon, S. D.; Schwarz, S. Antimicrobial susceptibility testing in veterinary medicine: performance, interpretation of results, best practices and pitfalls. One Health Advances 2023, 1, 26. [Google Scholar] [CrossRef]
- Beco, L.; Guaguère, E.; Lorente Méndez, C.; Noli, C.; Nuttall, T.; Vroom, M. Suggested guidelines for using systemic antimicrobials in bacterial skin infections: part 2-- antimicrobial choice, treatment regimens and compliance. Vet Rec. 1: 9; 172. [CrossRef] [PubMed]
- Paterson, S. Rational use of antibiotics in skin disease. Companion Animal 2017, 22, 632–639. [Google Scholar] [CrossRef]
- Wirt, K. M.; Young, J. M.; Cramer, G.; Wagner, S. A. Topical salicylic acid treatment of digital dermatitis in dairy cows: Drug resides in milk and clinical efficacy. The Bovine Practitioner 2021, 45–51. [Google Scholar] [CrossRef]
- Popova, T. P.; Ignatov, I.; Petrova, T. E.; Kaleva, M. D.; Huether, F.; Karadzhov, S. D. Antimicrobial activity in vitro of cream from plant extracts and nanosilver, and clinical research in vivo on veterinary clinical cases. Cosmetics 2022, 9, 122. [Google Scholar] [CrossRef]
- Hoang, T. P. N.; Ghori, M. U.; Conway, B. R. Topical antiseptic formulations for skin and soft tissue infections. Pharmaceutics 2021, 13, 558. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.; Rathore, C.; Barik, B. B.; Samanta, A.; Rahamanulla, A.; Jafar, M.; Krishna, K. V. Development and Characterization of Calendula officinalis Extract-Loaded Topical Gels For Use In Inflammatory Skin Conditions Associated With Staphylococcus aureus and Pseudomonas aeruginosa in Diabetic Foot Ulcers. Journal of Neonatal Surgery.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).