1. Introduction
All life, from youth to old age, health to disease, and activity to rest, fundamentally depends on energy. The continuity of life relies primarily on oxidative phosphorylation via the electron transport chain (ETC) within mitochondria in every human cell. This process is essential for energy production but also generates inflammation and oxidative stress phenomena central to the pathophysiology of ageing and chronic disease, as well as the inevitable result of life itself. Decades-old biochemical theories link the rate of energy production to the rate of ageing, with reactive oxygen species (ROS) produced by mitochondria acting as the mechanistic bridge, placing mitochondria at the centre of longevity science and medicine [
1,
2,
3,
4,
5,
6].
Both inflammatory and oxidative processes drive biochemical changes that lead to metabolic dysfunction, energy inefficiency, and the loss of physical strength. Mitochondrial dysfunction increases oxidative stress, disrupts metabolism, and alters cell fate. It is increasingly plausible to view ageing as a biochemical progression toward two interdependent pathologies: insulin resistance (metabolic syndrome) and the loss of skeletal muscle mass and power (sarcopenia), with additional individual-specific biochemical processes [
7,
8,
9,
10].
Muscle metabolism, especially under physical exertion, triggers the release of myokines, which act in autocrine, paracrine, and endocrine fashions. These exercise-induced myokines are gaining prominence in the literature for their roles in health, performance, and longevity, with significant implications for treating chronic disease and optimizing structural and metabolic health [
11,
12,
13,
14,
15,
16].
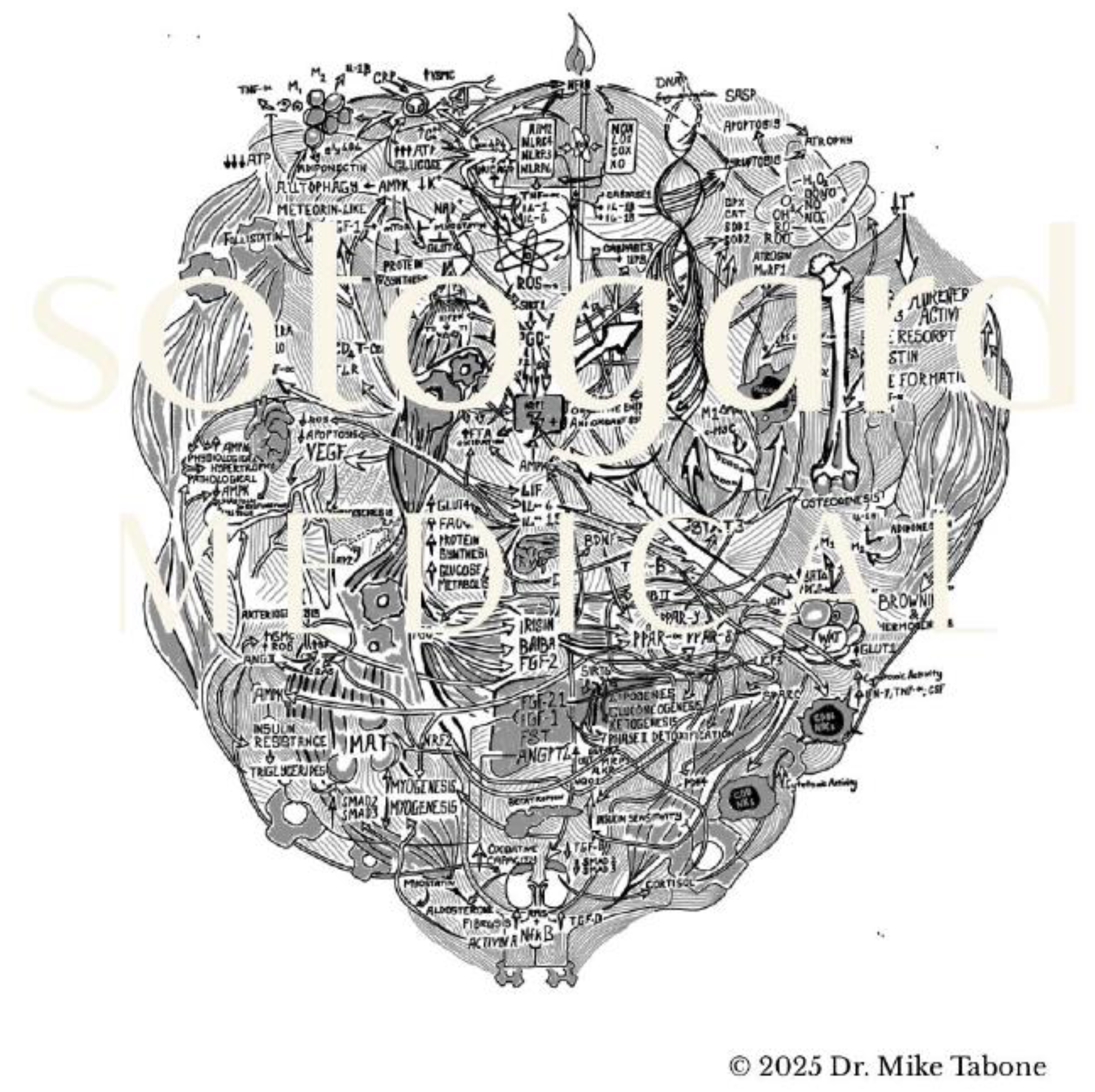
Figure 1.
Myokines: A Symphony of "Sarcosignalling".
Figure 1.
Myokines: A Symphony of "Sarcosignalling".
Artistic representation of the complex network of myokines and their relationships with cellular pathways, energy metabolism, inflammation, and tissue remodelling.
2. Materials & Methods
This review synthesizes evidence from peer-reviewed literature, including original research articles, systematic reviews, and meta-analyses indexed in PubMed, Scopus, and Web of Science. The focus was on studies addressing the molecular, cellular, and physiological roles of myokines in metabolic regulation, inflammation, and exercise adaptation. Emphasis was placed on human and translational animal studies published in the last two decades.
3. Results
3.1. Aging, Inflammation, and the Sarcopaenic State
Being alive entails a continuous "maintenance" burden of inflammation, which, in response to daily wear-and-tear, is physiological and reparative, assimilable to a low-burning flame governed by inflammasomes. These are central to the innate immune system, the body’s first line of defence against internal and external threats. Of particular interest to sarcopenia and metabolic syndrome is the nod-like receptor protein 3 (NLRP3) inflammasome, along with NLRP6, NLRC4, and AIM2.
Dysregulation of the NLRP3 inflammasome is implicated in many diseases and is a key regulator of skeletal muscle metabolism. Its activation leads to the maturation and secretion of pro-inflammatory cytokines IL-1β and IL-18, triggering inflammatory cascades observed in muscle atrophy and other myopathies.
This inflammatory phenotype, driven by inflammasomes, becomes pathological when excessively activated by environmental toxins, internal chemical messengers, altered microbiota, nutritional factors (trans/saturated fats, AGEs), and molecular patterns like PAMPs and DAMPs. These triggers activate pattern recognition receptors (PRRs), including NLRs, TLRs, and RLRs, leading to increased proinflammatory mediator expression [
7,
8,
9,
10,
17].
Chronic inflammation underlies many age-related diseases, such as osteoporosis, atherosclerosis, Alzheimer’s, Parkinson’s, and type 2 diabetes. Targeting these pathways is a promising strategy for age-related disorders. While it remains unclear whether the inflammatory phenotype and ROS production are features of healthy ageing or strictly pathological, evidence suggests that increased ROS accelerates the mutually reinforcing processes of ageing and inflammation-termed "inflammaging".
ROS are unstable, highly reactive molecules generated during redox reactions under physiological and pathological conditions. Major ROS include superoxide anion, hydroxyl radical, hydrogen peroxide, and hypochlorous acid, accounting for 1–2% of respiratory chain oxygen consumption. They are produced by enzymes such as NADPH oxidases, xanthine oxidase, nitric oxide synthase, cyclooxygenases, and lipoxygenases. When not sufficiently buffered by antioxidant systems, ROS contribute to the pathophysiology of ageing, sarcopenia, and metabolic syndrome [
18,
19,
20].
3.1.1. NLRP3, NF-κB, and TNF-α
NLRP3, NF-κB, and TNF-α are central mediators in the inflammatory processes that drive muscle atrophy and metabolic dysfunction. The NLRP3 inflammasome is activated by a range of stimuli, including excess ATP, glucose, reactive oxygen species (ROS), oxidized low-density lipoprotein (LDL), uric acid, and ionic imbalances such as calcium influx or potassium efflux, leading to caspase-1 activation and the maturation and secretion of pro-inflammatory cytokines IL-1β and IL-18 [
9,
21]
The activation of NLRP3 is closely linked to the transcription factor NF-κB, which upregulates the expression of tumour necrosis factor-alpha (TNF-α) and initiates a cascade central to sarcopenia, including muscle atrophy via the ubiquitin-proteasome system (UPS), muscle wasting through inflammatory signalling, and impaired muscle regeneration [
17,
22].
When activated in skeletal muscle, NF-κB stimulates the degradation of muscle proteins, enhances inflammation and fibrosis, and blocks the regeneration of myofibers following injury or atrophy [
23]. TNF-α, a key inflammatory cytokine, induces muscle protein loss through activation of the UPS and its main effector proteins, atrogin-1 (MAFbx) and muscle RING finger protein 1 (MuRF1), which promote ubiquitination and proteolysis, leading to skeletal muscle disintegration and atrophy [
24,
25,
26].
This process is further exacerbated by a self-reinforcing cascade in which the UPS and inflammatory cytokines activate NF-κB, which in turn activates NLRP3, while the resulting mitochondrial ROS and DNA fragmentation further stimulate both NLRP3 and NF-κB, perpetuating ongoing pathology [
8,
27].
Proinflammatory cytokines such as TNF-α, IL-1β, interferon-gamma (IFN-γ), and interleukin-6 (IL-6) contribute to muscle wasting, functional decline, and disease [
28,
29,
30,
31,
32].
NLRP3, NF-κB, and TNF-α play pivotal roles in the inflammatory cascade that adversely affects muscle metabolism through immunological and hormonal pathways. The NLRP3 inflammasome is activated by excess ATP, glucose, ROS, oxidized LDL, uric acid, and, under certain conditions, calcium influx or potassium efflux [
17]. One of the early steps in NLRP3 activation is the transcription of nuclear factor kappa B (NF-κB), which upregulates tumour necrosis factor-alpha (TNF-α) and initiates a triad of processes central to sarcopenia: muscle atrophy via the ubiquitin-proteasome system (UPS), muscle wasting through inflammatory signalling, and reduced regeneration of atrophied muscle [
9] NF-κB activation in skeletal muscle stimulates muscle protein degradation explicitly, enhances inflammation and fibrosis, and inhibits myofiber regeneration following injury or atrophy [
21]. Muscle atrophy can result from increased protein degradation, reduced synthesis, or both.
Generally, activation of the phosphatidylinositol 3-kinase (PI3K)/Akt pathway in response to loading and growth factors such as insulin and IGF-1 prevents skeletal muscle loss, whereas activation of NF-κB, activator protein-1 (AP-1), p53, FoxO, and p38 mitogen-activated protein kinase (MAPK) pathways leads to muscle atrophy [
21]. TNF-α induces caspase-1 activation and subsequent secretion of interleukin-1β (IL-1β) and interleukin-18 (IL-18), as well as activation of the UPS and its main effector proteins, atrogin-1 (MAFbx) and muscle RING finger protein 1 (MuRF1), which are central to sarcopenia [
22,
23,
24]. These proteins promote ubiquitination and proteolysis, leading to skeletal muscle protein breakdown, programmed pyroptosis, and subsequent muscle atrophy [
25,
26]
A self-reinforcing cascade perpetuates inflammasome activity in muscle atrophy, where the UPS and inflammatory cytokines activate NF-κB, which in turn activates NLRP3. The resulting damage generates more mitochondrial ROS and DNA fragmentation, both of which further induce NLRP3 and NF-κB, maintaining ongoing pathology [
8,
27]. Proinflammatory cytokines such as TNF- α, IL-1β, IFN-γ, and IL-6 contribute to skeletal muscle wasting, functional decline, and disease, with neutrophils involved in damage control and restoration of immune homeostasis, though their activity declines with age [
33].
3.1.2. IFN-γ, the Immune Response and Sarcopaenia
The mechanistic connection between IFN-γ signaling and skeletal muscle homeostasis is particularly important, as IFN-γ is involved in both regenerative and catabolic metabolism of muscle tissue, with acute rises following training or injury orchestrating tissue clearance before regeneration and chronic dysregulation contributing to impaired muscle repair in aging [
25,
33].
The generation of reactive oxygen species (ROS) increases with age, disease, and metabolic disturbances, including those arising from poor sleep, suboptimal nutrition, and exposure to toxins or radiation [
34]. Elevated oxidative stress plays a central role in the aetiology of metabolic syndrome, sarcopenia, and their complications, as excessive ROS burden, particularly when not adequately buffered by intrinsic or dietary antioxidants, drives the progression of metabolic syndrome and its sequelae, including diabetes and muscle wasting [
13,
35,
36]. In type 2 diabetes, persistent hyperglycemia is a prominent cause of increased ROS production through multiple biochemical pathways, which accelerates ageing, sarcopenia, and the weakening of endogenous antioxidant defences [
34,
37]. Inflammatory processes further augment ROS generation, and under physiological conditions, these are counteracted by anti-inflammatory and antioxidant systems. ROS and inflammation are interactive and mutually causative, though not completely mutually dependent, and are directly implicated in the pathogenesis of ageing, sarcopenia, and metabolic syndrome. Muscle fibre-specific apoptosis and TNF- α signalling in sarcopenia are attenuated by life-long calorie restriction [
37].
Thus, both in health and more so in disease, the state of being alive entails a continuous burden of ROS and inflammation, both of which can damage DNA, lipids, and proteins if their activity is not sufficiently controlled or their downstream effects not adequately contained by endogenous or exogenous buffers [
16].
IFN-γ exemplifies the pleiotropic nature of cytokines, being involved in both regenerative and catabolic muscle metabolism. Acute rises in IFN-γ post- training or injury facilitate the clearance of damaged tissue before regeneration, while chronic dysregulation impairs muscle regeneration in the elderly [
25,
38,
39]. Recent studies show that decreased counts of interferon- responsive macrophages (IFNRMs) in muscle after training or injury contribute to impaired regeneration with age, as these cells activate satellite cell proliferation via CXCL10 expression, which also declines with age [
40].
3.1.3. Inflammatory Cytokines and Hormonal Dysregulation
Inflammatory cytokines attenuate the effects of insulin-like growth factor 1 (IGF-1) and testosterone while augmenting glucocorticoid receptor activation, promoting aberrant lipid and glucose metabolism [
41,
42]. Differences in insulin signalling between type I and type II muscle fibres have been documented, with type I fibres more adept at glucose metabolism and expressing more GLUT4 receptors, while type II fibres accumulate more mitochondrial damage and are more vulnerable to ROS with age [
43,
44,
45]. Cortisol plays a central role in the pathophysiology of ageing, metabolic syndrome, and sarcopenia, exerting anti-inflammatory effects acutely but, when chronically elevated, leading to glucocorticoid resistance, decreased anti-inflammatory signalling, and enhanced inflammatory signalling [
46,
47]. Chronic cortisol elevation suppresses lipogenesis, gluconeogenesis, and ketogenesis while promoting insulin resistance, compensatory hyperinsulinemia, impaired mitochondrial biogenesis, and reduced oxidative capacity in skeletal muscle [
48].
Glucocorticoid signalling also stimulates Renin release through activation of the renin-angiotensin system (RAS) in vascular smooth muscle and bone and is itself stimulated by increased Renin in metabolic syndrome, type 2 diabetes, chronic kidney disease, and congestive heart failure [
49,
50]. The RAS inhibits IGF-1 signalling, downregulates protein synthesis, activates the UPS (with Ang II upregulating MuRF1 and Caspase3), and leads to mitochondrial dysfunction, sarcopenia, systolic hypertension, and upregulation of TGF-β, augmenting fibrosis [
51,
52,
53,
54].
3.1.4. Myostatin
The transforming growth factor-beta (TGF-β) family, including myostatin, plays a key role in muscle growth inhibition. Myostatin increases with age and declining muscle mass, is upregulated by AMPK, and inhibits muscle regeneration and protein synthesis via SMAD2/3 signalling, blocking AKT phosphorylation by insulin and IGF-1 and upregulating Atrogin1, promoting protein degradation. Myostatin also inhibits satellite cell proliferation and differentiation and is produced by both muscle and adipose tissue, impairing muscle growth via SMAD2/3/4 signalling and promoting insulin resistance. Its inhibition in animal studies improves insulin sensitivity and glucose tolerance [
55,
56,
57].
The myostatin signalling pathway is a crucial regulatory mechanism in muscle- organ crosstalk. Upon binding to its receptor complex, myostatin phosphorylates Smad2 and Smad3 transcription factors, which form a complex with Smad4 and translocate to the nucleus, directly activating atrophy-related genes and inhibiting protein synthesis pathways. Smad3 interacts with and inhibits MyoD, a key regulator of muscle differentiation, while the Smad2/3- Smad4 complex activates FoxO transcription factors, upregulating muscle- specific E3 ubiquitin ligases such as MAFbx/atrogin-1 and MuRF1, leading to proteasomal degradation of muscle proteins [
58]. Exercise-induced inhibition of myostatin signalling occurs through mechanisms including the induction of follistatin, a natural myostatin antagonist, and decorin, which binds myostatin and prevents receptor activation [
59,
60,
61,
62].
3.1.5. Leptin & Resistin
Adipokines such as leptin and resistin are bioactive mediators released by adipose tissue with systemic effects on metabolism and inflammation. Leptin acts as an adipostat, with levels reflecting energy stores and acute caloric intake, and also functions as a proinflammatory cytokine influencing energy homeostasis, feeding behaviour, and insulin resistance. Its expression is enhanced by overfeeding, glucose, insulin, glucocorticoids, estrogens, adiposity, TNF-α, IL-6, and LPS, and it stimulates IGF-1 activity, induces inflammation through STAT3 and JAK2, and activates monocytes and macrophages to produce TNF-α, IL-6, and IL-12 [
63,
64,
65,
66]. Resistin is a proinflammatory adipokine induced by inflammatory cytokines and LPS, acting via TNF-α to activate NF-κB, promote vascular smooth muscle cell migration, stimulate macrophages to produce IL-6 and TNF-α and enhance the uptake of oxidized LDL into macrophages, contributing to the atherogenic profile of metabolic syndrome [
67,
68,
69,
70].
3.1.6. Interleukin-6
Interleukin-6 (IL-6) plays a controversial role in metabolic syndrome, participating in both inflammatory cascades and mechanisms of insulin resistance and skeletal muscle atrophy, as well as in training adaptations. IL-6 is expressed in adipose tissue and correlates with obesity, potentially mediating insulin resistance and muscle atrophy through activation of SOCS3 and inhibition of IGF-1, with circulating IL-6 levels negatively correlated with IGF-I levels. Chronic elevation of IL-6 and STAT3 is involved in skeletal muscle atrophy, with the extent of muscle mass involved and duration of exertion influencing the magnitude of IL-6 response [
25,
71,
72,
73,
74,
75].
3.1.7. Fibroblast Growth Factor 2
Fibroblast growth factor 2 (FGF-2) is a myokine belonging to the TGF-β family with paradoxical effects in muscle, particularly concerning ageing and insulin resistance. FGF-2 suppresses secreted protein acidic and rich in cysteine (SPARC), a myokine involved in extracellular matrix adaptation, thereby promoting intramuscular adipose tissue (IMAT) deposition, but also plays a role in muscle regeneration by regulating angiogenesis and muscle satellite cell activation. The decline of SPARC with age contributes to muscle atrophy and insulin resistance [
76,
77]. The liver, central to systemic glucose homeostasis, is vulnerable to insulin resistance, which leads to metabolic-associated fatty liver disease (MAFLD) and is characterized by reduced SIRT6 and SIRT1 expression [
78,
79]. Elevated gamma-glutamyl transferase (GGT) levels correlate with mitochondrial distress and are strong predictors of diabetes and all-cause mortality [
80]. In metabolic syndrome, skeletal muscle atrophy is linked temporally and pathologically to insulin resistance, with a greater loss in the cross-sectional area observed in type II (fast-twitch) fibres, especially subtype IIB, compared to type I (slow-twitch) fibres [
44,
45,
81,
82].
Activation of the PI3K/Akt pathway in response to loading and growth factors such as insulin and IGF-1 prevents skeletal muscle loss, while activation of NF- κB, AP-1, p53, FoxO, and p38 MAPK pathways leads to muscle atrophy [
83].
Chronic mTORC1 activation, resulting from loss of inhibition, causes severe muscle atrophy and early death due to reduced autophagy, highlighting the importance of quality control mechanisms such as caloric restriction, which inhibits both inflammation and cancer via attenuation of IGF-1/PI3K/Akt/mTOR signalling and promotes activation of FoxO1, FoxO3, and Nrf2 transcription factors [
84,
85].
3.1.8. Current Understanding of Signalling Duality of Cytokines in Metabolic Health and Disease
Current understanding of cytokine signalling in metabolic health and disease reveals that physiological or pathological outcomes are rarely the result of a single factor but rather reflect the cumulative influence of numerous internal and external variables. Myokines, like cytokines, interact in multivariate, often nonlinear ways with metabolic and inflammatory pathways, making their effects highly context-dependent [
86]. This complexity is further heightened by the duality of cytokine signalling, where the same molecule can exert opposing effects depending on the biochemical environment. For example, proinflammatory cytokines typically have negative charges with isoelectric points below 7.4, while anti-inflammatory cytokines are often positively charged, affecting their biodistribution, tissue adhesion, and receptor interactions and, thus, their activity in different tissue microenvironments [
87]. During inflammation, local pH-dependent changes can alter cytokine charge and function, contributing to their context-specific effects [
88].
Receptor system morphology adds another layer of complexity, as the end effect of cytokine signalling depends on receptor distribution and form. For instance, IL-6 signalling through membrane-bound versus soluble receptors activates different downstream cascades and exercise-induced IL-6 from muscle acts through mechanisms distinct from IL-6 produced by immune cells during inflammation [
89,
90]. The internal environment’s extracellular matrix composition, oxygen tension, metabolic state, and the presence of other signalling molecules also shape cytokine actions. IFN-γ, for example, promotes muscle regeneration after exercise but contributes to atrophy during infection [
91].
Temporal dynamics are crucial, as acute, transient cytokine signalling mediates adaptive responses, whereas chronic elevation is typically pathological, influenced by receptor desensitization, cellular adaptation, and feedback mechanisms [
92]. Cytokines never act in isolation but interact with endocrine, paracrine, and autocrine mediators and other signalling pathways, enabling specificity and flexibility in biological responses. From an evolutionary perspective, cytokine duality may represent an adaptation for effective, self- regulated immune responses, allowing challenge-response without loss of homeostasis [
93]. This duality implies that therapeutic interventions targeting cytokine systems should aim for context-specific modulation rather than simple inhibition or stimulation and that integrative, multifaceted interventions are required to create the internal environment for optimal signalling and health outcomes [
94].
3.2. Physical Training and the Strength State
A fundamental axiom of a strong metabolic state is energy efficiency, which translates to effective blood glucose control and is ultimately dependent on efficient glucose uptake, glycolysis, gluconeogenesis, and mitochondrial health processes underpinned by the health of skeletal muscle [
36]. Skeletal muscle is highly plastic and adaptable, with its structural and metabolic homeostasis hinging on the balance between anabolic and catabolic pathways, specifically muscle protein synthesis versus breakdown. Anabolic processes are mediated primarily through the IGF-1/PI3K/Akt signalling pathway, which activates mTOR, a central regulator of protein synthesis and muscle growth [
83,
95].
However, optimal metabolic health is not achieved solely through anabolic growth; catabolic processes, including autophagy and protein turnover, are equally important for tissue quality control and longevity [
85]. Activation of mTORC1 promotes muscle hypertrophy in the short term, but chronic activation, particularly in the absence of adequate autophagy, leads to muscle atrophy, sarcopenia, and reduced lifespan [
96]. Cellular distress signals such as low ATP, hypoxia, or DNA damage activate AMPK, which inhibits mTORC1 and promotes catabolic processes, ensuring cellular quality control [
97,
98]. mTORC2, in contrast, supports cell survival and growth by inhibiting protein breakdown through modulation of transcription factors such as FoxO1/3a and GSK-3β [
99,
100]. Caloric restriction exemplifies this balance, attenuating IGF- 1/PI3K/Akt/mTOR signalling, activating FoxO and Nrf2 transcription factors, and promoting anti-inflammatory and anti-cancer effects [
101].
Striking a balance between anabolic growth and catabolic degeneration is key to reversing metabolic disease and optimizing longevity. Building and maintaining muscle tissue is foundational, especially since most individuals with metabolic syndrome lack sufficient skeletal muscle mass to serve as a metabolic moderator [
102]. The science of movement is, therefore, central to metabolic regulation, with skeletal muscle contraction being the primary driver of relevant mechanical and metabolic adaptations. The type and combination of muscle contractions- concentrated, eccentric, and isometric- determine the nature of the training adaptation.
The physiological burden of ROS and inflammation does not disappear with a strong, active metabolic state; instead, it is modulated so that biological responses remain physiological rather than pathological. This phenomenon is explained by hormesis, where a controlled, transient increase in low levels of a stressor (such as ROS from exercise) induces beneficial adaptations. At the same time, excessive or prolonged exposure leads to damage [
103,
104]. Early research demonstrated that moderate exercise-induced ROS production is essential for skeletal muscle adaptation, whereas high levels of exhaustive exercise cause muscle damage and diminish physiological benefits [
105,
106,
107,
108,
109,
110,
111,
112,
113]. The hormetic response to exercise-induced ROS is often depicted as a bell- shaped curve, though some evidence suggests that prolonged, high-intensity exercise may still confer health benefits without tissue damage, provided adequate recovery and lifestyle interventions are in place [
19,
114,
115,
116,
117,
118].
Standardization of exercise intensity, duration, frequency, and volume remains a challenge, leading to variability and arbitrariness in research and clinical recommendations. The safety of high-volume and high-intensity exercise is questioned in cases such as repeated exhaustive endurance exercise, which can generate ROS beyond the hormetic dose, precipitating arrhythmias or rhabdomyolysis if not buffered by appropriate nutrition and recovery [
119,
120,
121,
122,
123,
124,
125,
126,
127,
128,
129]
Therefore, absolutist statements about exercise prescription should be avoided, and recommendations should be individualized. Physical exercise, regardless of type, intensity, Or volume generally confers health benefits by mediating systemic anti-inflammatory responses and improving antioxidant capacity [
111,
130]
3.2.1. Skeletal Muscle Structure, Satellite Cells, and Regeneration
Skeletal muscle is a multinucleated, postmitotic tissue originating from embryonic mesoderm, with muscle stem cells (satellite cells) residing between the basal lamina and plasma membrane of myofibers. These satellite cells are central to muscle remodelling in response to mechanical work, retaining the capacity for regeneration throughout life [
131]. The pleiotropic benefits of exercise stem from both metabolic and anatomical adaptations, which are mutually reinforcing: metabolic changes enhance structural remodelling, and increased muscle mass and quality further optimize metabolic function [
132].
Structurally, muscle satellite cells (MSCs) are the site and source of muscle tissue growth. Muscle growth occurs primarily through hypertrophy, where an increase in myofibrils per muscle fibre leads to the greater cross-sectional area of individual fibres and, secondarily, the whole muscle. Hyperplasia, or an increase in muscle fibre number, may contribute minimally to muscle growth beyond the early postnatal stage [
133,
134,
135,
136,
137]. Following physical exercise, especially resistance training, quiescent MSCs are recruited in response to hormetic distress, proliferate to form myoblasts, and undergo controlled proliferation and differentiation before fusing with existing myofibers, thus regenerating muscle tissue and contributing to hypertrophy [
131,
138,
139].
The myogenic program is orchestrated by transcription factors such as paired box transcription factor 7 (Pax7), which is highly expressed in quiescent MSCs. Transformation into committed myoblasts depends on myogenic regulatory factors (MRFs), primarily MyoD during proliferation, with terminal differentiation initiated by upregulation of MRF4 and myogenin, leading to myotube formation and maturation [
140]. Myoblasts can also return to quiescence and self-renewal through the influence of Sprouty1, Notch receptors 1–3, and FoxO3 [
141]. Muscle remodelling in response to exercise shares features with the regenerative processes following injury, with macrophages orchestrating the inflammatory response and tissue regeneration. Macrophages engulf cell debris via efferocytosis, marking the transition from the proinflammatory to the recovery phase, and subsequently organize tissue repair, angiogenesis, and extracellular matrix remodelling [
142].
The STAT3 signalling pathway plays important roles in both muscle regeneration after exercise and in inflammation and its sequelae, with effects that are likely dose- or duration-dependent. In the acute phase following exercise, STAT3 phosphorylation initiates a cascade that encourages regeneration by promoting myoblast proliferation and discouraging apoptosis while also suppressing cytokine generation. In contrast, chronic elevations in STAT3 signalling contribute to muscle atrophy via mediators including IL-6, interferon-gamma, TNF-α, and TGF-β1 Mammalian target of rapamycin regulates miRNA-1 and follistatin in skeletal myogenesis [
95,
131,
143,
144,
145,
146,
147].
During exercise, energy expenditure increases dramatically, resulting in a corresponding increase in electron transport chain activity and related ROS production, which induces metabolic regulators such as peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) and members of the SIRTUIN family of histone deacetylases [
16,
148,
149]. SIRT1 and SIRT3 are the primary sirtuins involved in skeletal muscle mitochondrial metabolism. SIRT1 is an active regulator of muscle repair and hypertrophy, inhibiting p53-mediated apoptosis and directing FOXO transcription activity with regard to genes involved in cell cycle arrest, DNA repair, and oxidative stress resistance. SIRT1 is upregulated by caloric restriction and mechanical stretch stimuli to skeletal muscle via FoxO3a and early growth response factor 1 (Egr1) through the augmentation of AMPK and NAD+ levels [
150,
151,
152]. AMPK inhibits mTOR and induces autophagy, fatty acid oxidation, and GLUT4 upregulation in myocytes [
153,
154,
155]. SIRT1 also induces cardiomyocyte survival, neuroprotection, hepatic gluconeogenesis, decreases adipogenesis, and stimulates insulin secretion via repression of uncoupling protein 2 (UCP2) [
156]. SIRT1 exerts a range of effects on muscle metabolism through activation of PGC-1α, stimulating satellite cell proliferation, increasing myonuclear number, and enhancing nitric oxide production [
157,
158].
3.2.2. PGC-1α & PPARs
PGC-1α is induced in skeletal muscle and brown adipose tissue by cold, physical training, and β-adrenergic activity and aids in the activation of peroxisome proliferator-activated receptors (PPARs), especially PPAR-α, PPAR- δ, and PPAR-γ.
Fatty acids and their derivatives are natural ligands for peroxisome proliferator-activated receptors (PPARs), which play a central role in lipid homeostasis regulation [
159,
160]. PPAR-α exerts dose-dependent effects, with normal activation benefiting lipid metabolism but overactivation leading to glucose dysregulation and insulin resistance. PPAR-δ is the predominant isoform in skeletal muscle and has beneficial effects on lipid metabolism, glucose uptake, and insulin sensitivity [
161]. The link between fatty acid oxidation and PPAR-α was established when it was shown that the peroxisomal acyl-coenzyme A oxidase gene, involved in peroxisomal fatty acid β-oxidation, is regulated by PPAR-α, and numerous genes involved in hepatic fatty acid catabolism are induced by peroxisome proliferators and PPAR-α [
162]. PPAR-γ is expressed in skeletal muscle and liver, though at much lower levels than in adipocytes. It enhances fatty acid oxidation and glucose metabolism and is inhibited by TNF-α [
162,
163,
164]. PPAR-γ is highly expressed in macrophages, including foam cells in atheromatous lesions, and regulates cholesterol influx and efflux, contributing to the anti-atherosclerotic effects of PPAR-γ agonists [
165]. PPAR-γ agonists lower blood pressure in diabetic patients and hypertensive animal models, though the antihypertensive mechanism is not fully understood. PPAR-γ is the target for the antidiabetic actions of the glitazone class of drugs [
166].
PGC-1α acts as a master regulator of metabolic adaptation to exercise by transducing biological stimuli into specific metabolic strategies, including the induction of mitochondrial biogenesis through nuclear respiratory factor 1 (NRF1) and the regulation of metabolism via SIRT3 activation [
167,
168,
169]. PGC- 1α augments oxidative metabolism enhances ROS removal promotes β- oxidation of fatty acids, stimulates gluconeogenesis in the liver, and induces the cleavage of irisin from FNDC5, which contributes to adaptive thermogenesis in brown adipose tissue via upregulation of UCP1 [
148,
170,
171,
172] In skeletal muscle, PGC-1α also mediates fibre-type switching from type II to type I fibres through upregulation of hypoxia-inducible factor 2 alpha (HIF2α), and SIRT3 regulates MnSOD activity, contributing to antioxidant defence [
173,
174,
175]. PGC-1α, SIRT1 and SIRT3 expression are higher in type I fibres than in type II fibres, reflecting greater oxidative capacity [
158]. SIRT6 is involved in liver health, with its levels in hepatocytes regulating adipose tissue deposition, hepatic inflammation, and systemic glucose homeostasis [
79,
176].
Both muscle contraction and PGC-1α activate antioxidant response elements (ARE) via nuclear respiratory factor 2 (NRF2), the master regulator of antioxidant enzymes and cellular resilience, mediating hormesis in response to biomechanical and nutritional stimuli [
177,
178,
179]. NRF2 upregulates catalase and glutathione reductase activity, downregulates oxidative stress, enhances xenobiotic metabolism and excretion, promotes autophagy, and suppresses NF-κB and TGF-β signalling, which are linked to tissue repair, ageing, and carcinogenesis [
103,
180,
181,
182,
183]. In parallel with muscle remodelling, vascular remodelling in response to exercise increases oxygen and nutrient delivery and waste removal, with increased blood flow promoting angiogenesis through vasodilation and upregulation of VEGF and eNOS. Exercise increases endothelial NAD+ and SIRT1, activating VEGF-associated angiogenesis [
181].
Both VEGF and FGF-2 transiently increase after acute exercise, mediating vascular remodelling and pro-angiogenic adaptations in muscle, with VEGF supporting angiogenesis and FGF-2 contributing to arteriogenesis and the maintenance of mature vessels [
184,
185,
186].
3.2.3. Myokines
Myokines are signalling mediators released by muscle contractions that are at least partially responsible for the anti-inflammatory effects of physical exercise and enable autocrine, paracrine, and endocrine communication with surrounding tissues and distant organs such as adipose tissue, liver, bone, and brain [
15,
86]. ATP synthesis is rapidly activated through substrate utilization during exercise, and myokine release may be an adaptive mechanism to increased energy demand in contracting muscle [
187]. Skeletal muscle is capable of producing over 650 different myokines, but only about 5% have a defined biological function. Aging is associated with decreased secretion of beneficial myokines, including apelin, decorin, β-aminoisobutyric acid (BAIBA), sesterin, SPARC, IL-15, and irisin, and these myokines are critical regulators of age-related pathologies such as diabetes, muscle atrophy, and chronic inflammation. Serum from patients with type 2 diabetes contains reduced levels of beneficial myokines such as irisin, IL-13, and FSTL-1, and myokines from insulin-resistant myotubes impair β-cell function, proliferation and survival, indicating that muscle-to-pancreas cross-talk regulates insulin secretion [
188].
3.2.4. β-Amino Isobutyric Acid (BAIBA)
β-amino isobutyric Acid (BAIBA) is another myokine involved in the induction of mitochondrial free fatty acid (FFA) oxidation and improvements in insulin signalling and confers protection against inflammation through AMPK-PPAR dependent mechanisms, through which pathway (in a non-adrenergic manner) it also induces the thermogenic program in white adipose tissue.
When given to mice in drinking water for 14 days, BAIBA fails to increase the expression of thermogenic genes, including UCP-1, CIDEA, PGC-1α, and cytochrome c, in the PPARα null mice. Therefore, these results indicate that BAIBA increases the expression of the browning gene program through a specific PPARα-dependent mechanism. Together, these results indicate that BAIBA increases hepatic fatty acid oxidation gene expression through a PPARα dependent mechanism. BAIBA, IRISIN, Fibroblast Growth Factor 2 (FGF-2), and IGF-1 exert paracrine effects at the level of bone and fat tissue, effecting beneficial adaptations in fat and bone metabolism, providing separate avenues for bone mass density optimization from the more popular mechanoreceptor response to biomechanical stressors in physical exercise [
189,
190,
191]
3.2.5. Interleukin-6
Interleukin-6 (IL-6) is one of the most well-documented myokines and was indeed the first myokine found to be secreted into the bloodstream in response to muscle contraction. IL-6 increases exponentially with the duration of exercise and the volume of muscle mass engaged, likely acting as an energy sensor [
90]. Unlike the IL-6 response seen with inflammasome activation, exercise-induced IL-6 increases in the absence of muscle damage or preceding TNF-α elevation [
192]. Exercise-induced IL-6 enhances insulin-stimulated glucose uptake, activates AMPK (thereby increasing fat oxidation and GLUT4 translocation), enhances lipolysis, and promotes browning of white adipose tissue via UCP1. It also mediates the anti-inflammatory effects of exercise by inhibiting the production of proinflammatory cytokines such as TNF-α and IL- 1β and by stimulating anti-inflammatory cytokines including IL-1Ra and IL-10 [
102,
111,
193]. The interplay between IL-6 and other cytokines during exercise represents a complex regulatory network distinct from inflammatory IL-6 signalling. Exercise-induced IL-6 production in skeletal muscle occurs through calcium-dependent and glycogen-sensitive pathways, with p38 MAPK playing a central role in transcriptional activation. Upon release, IL-6 binds to a membrane-bound receptor complexed with gp130, activating JAK1 and STAT3 signalling, resulting in enhanced glucose uptake and fatty acid oxidation while also inhibiting TNF-α and stimulating anti-inflammatory cytokines [
194]. IL-6 is also involved in muscle regeneration after injury, with factors from the TGF-β family, IGF-I/II, FGF-2, FGF-6, HGF, TNF-α, and IL-6 all contributing to the restoration of normal muscle architecture [
138].
The role of IL-6 in the regenerative phase, along with the myokine leukaemia inhibitory factor (LIF), is to induce the JAK1/STAT1/STAT3 pathway, promoting myoblast proliferation while preventing premature differentiation [
195]. LIF is constitutively expressed at low levels in type I muscle fibres and has been shown to stimulate glucose uptake, inhibit adipocyte differentiation, and participate in hypertrophic adaptations [
196,
197,
198]. Conversely, IL-6 also promotes leptin mRNA expression and inhibits adiponectin mRNA expression, suggesting that exercise may impact serum leptin and adiponectin levels by decreasing IL-6 [
71,
72,
199].
3.2.6. Interleukin-15
Interleukin-15 (IL-15) confers multiple metabolic benefits, promoting the assembly of contractile proteins, enhancing mitochondrial biogenesis through PPAR-dependent mechanisms in skeletal muscle, and stimulating adiponectin secretion. IL-15 promotes muscle growth and glucose uptake, enhances mitochondrial activity, and exerts anti-oxidative effects while stimulating adiponectin secretion. Improved oxidative metabolism in skeletal muscle of rodents with high circulating IL-15 is likely due to PPAR activation by IL-15, as demonstrated by increased PPAR mRNA expression in muscle following IL-15 treatment [
200]. IL-15 was initially identified as a T-cell growth factor but also participates in neutrophil phagocytosis and macrophage differentiation and activates CD56 NK cells, increasing IFN-γ, GM-CSF, cytotoxic activity, and antibody-dependent cytotoxicity. IL-15 activates the JAK3/STAT3 signalling pathway, improving insulin sensitivity and activating PPAR-δ to enhance oxidative metabolism in skeletal muscle. Exercise-induced IL-15 secretion acts in an autocrine/paracrine fashion to activate PPAR, improving skeletal muscle oxidative metabolism, endurance capacity, and whole-body energy expenditure while also mobilizing fat from adipose tissue and improving insulin sensitivity [
201,
202].
3.2.7. Secreted Protein Acidic and Rich in Cysteine
SPARC is a myokine involved in the regenerative phase of muscle repair, known to increase human islet insulin secretion and play an active role in skeletal muscle remodelling. It is upregulated during muscle development and regeneration, and its exercise-induced expression has been proposed as a molecular tool to optimize exercise therapy and reduce intramuscular adipose tissue (IMAT) and adipocyte differentiation, with the skeletal muscle phenotype expressed after training shown to be SPARC-dependent in animal studies [
203,
204,
205,
206]. At the molecular level, SPARC signals primarily through integrin receptors, particularly integrin α5β1, activating focal adhesion kinase (FAK) and downstream MAPK signalling. In adipose tissue, SPARC inhibits adipogenesis by disrupting preadipocyte differentiation through inhibition of transcription factors C/EBPβ and PPARγ, reducing IMAT accumulation and improving muscle quality and insulin sensitivity. SPARC also enhances insulin secretion in pancreatic β-cells via calcium-dependent mechanisms and interacts with collagens and growth factors to facilitate proper extracellular matrix assembly and prevent fibrosis during muscle adaptation to exercise.
SPARC expression decreases with age and sedentary behaviour but is restored by resistance exercise training [
207,
208].
3.2.8. Follistatin
Follistatin, a TGF-β family member released after exercise, prevents SMAD2/SMAD3 signalling by binding and neutralizing myostatin in the circulation, thereby enhancing myoblast proliferation and myotube growth [
209]. Decorin is a multifunctional myokine synthesized and secreted by skeletal muscle, especially in response to resistance exercise. It binds myostatin directly, immobilizing it in the extracellular matrix and preventing its inhibitory action on muscle growth. By suppressing myostatin-mediated SMAD2/3 signalling, decorin promotes muscle hypertrophy, myoblast proliferation, and myotube growth, upregulates pro-myogenic factors like Mighty and Myod1, and reduces muscle-specific ubiquitin ligases involved in atrophic pathways [
59,
60,
61]. Decorin expression increases approximately 24 hours post-exercise, suggesting a crucial role in recovery and adaptation rather than the immediate post-training period. It is also involved in collagen formation and stabilization, possesses anti-inflammatory properties, and increases insulin content and secretion in pancreatic islet cells, establishing a muscle-pancreas signalling axis [
190].
3.2.9. Meteorin-Like
Meteorin-like (Metrnl) is a myokine expressed by macrophages, barrier tissues, and skeletal muscle. Exercise-induced Metrnl increases fat oxidation in both skeletal muscle and adipose tissue, controls inflammation in adipose tissue (meta-inflammation), and regulates muscle regeneration. Production of Metrnl during exercise is associated with NLRP3 inflammasome suppression in animal studies, and recombinant Metrnl improves muscle regeneration in ageing humans [
210,
211]. Metrnl also enhances β-cell function by promoting mitochondrial biogenesis and reducing endoplasmic reticulum stress via STAT3 activation and inhibits NLRP3 inflammasome activation by promoting an M2 macrophage phenotype through STAT6 signalling, linking exercise-induced myokines to reduced inflammation [
210,
211].
3.2.10. Brain-Derived Neurotrophic Factor
Brain-derived neurotrophic factor (BDNF) is an emerging myokine of interest, potentially stimulating glucose uptake and lipid metabolism. Increased BDNF levels are documented after exercise, and its role as a myokine is likely upregulated directly through skeletal muscle contraction, possibly via the PGC-1α/FNDC5/irisin pathway, suggesting a muscle-brain axis benefiting both metabolic and cognitive health [
212].
3.2.11. Insulin-Like Growth Factor 1
Insulin-like growth factor 1 (IGF-1), synthesized in the liver in response to growth hormone and produced locally in skeletal muscle after training, induces muscle growth via the AKT/mTOR pathway, promotes muscle regeneration by upregulating MRF4, and enhances force-generating capacity. IGF-1 signaling also restores SPARC expression [
213].
3.2.12. Adiponectin
Adiponectin, an adipokine released in response to skeletal muscle contraction, has anti-inflammatory, antidiabetic, and anti-atherogenic properties. It stimulates glucose uptake and fat oxidation, correlates positively with insulin sensitivity and negatively with adiposity, and modulates appetite-regulating pathways. Adiponectin inhibits TNF-α production in macrophages and stimulates IL-10, promoting the differentiation of anti-inflammatory M2 macrophages [
214,
215,
216]
3.2.13. Myokine Modulation of Insulin Sensitivity, Inflammasome Activity, and Bone Metabolism
The pancreatic effects of myokines are a critical aspect of their metabolic regulatory functions. Skeletal muscle-derived factors significantly influence pancreatic β-cell function and insulin secretion. Conditioned media from cultured myotubes have shown that myokines from healthy skeletal muscle enhance glucose-stimulated insulin secretion (GSIS), while myokines from insulin-resistant muscle impair this process, primarily via the p38 MAPK pathway in β-cells [
11]. Specifically, IL-6 from contracting muscle improves β- cell function by activating glucagon-like peptide-1 (GLP-1) production in L cells and directly stimulating pancreatic α-cells to secrete GLP-1, which in turn enhances insulin secretion [
217]. Irisin protects pancreatic β-cells against high glucose and lipid-induced apoptosis through activation of AMPK pathways, while meteorin-like (Metrnl) improves β-cell function by enhancing mitochondrial biogenesis and reducing endoplasmic reticulum stress through STAT3 activation [
218].
Myokines also modulate inflammatory responses, particularly through interactions with the NLRP3 inflammasome, a key mediator of age-related chronic inflammation. Irisin inhibits NLRP3 activation in adipose tissue macrophages by suppressing ROS production and promoting mitochondrial integrity. IL-15, upregulated during resistance exercise, suppresses NLRP3 activation in multiple tissues by enhancing mitochondrial function and reducing cellular stress. Meteorin-like (Metrnl) inhibits NLRP3 inflammasome activation by promoting an M2 macrophage phenotype via STAT6 signalling, and the IL-6 family member ciliary neurotrophic factor (CNTF) exerts anti- inflammatory effects in part by inhibiting NLRP3 assembly. These interactions provide a molecular framework by which exercise-induced myokines counteract chronic inflammation associated with metabolic dysfunction [
72,
185,
202,
219,
220,
221]
Myokine-mediated muscle-bone interactions are another critical aspect of exercise-induced metabolic adaptation. Several myokines, including IL-6, IL-15, irisin, and SPARC, directly influence bone remodelling. Irisin binds to integrin receptors on osteocytes, activating p38 MAPK and ERK pathways to enhance osteoblast differentiation and mineral deposition. IL-15 promotes osteoblast differentiation and inhibits osteoclastogenesis by modulating the RANKL/OPG ratio, shifting bone metabolism toward formation. Many myokine effects on bone converge on the Wnt/β-catenin signalling pathway, a master regulator of osteoblast differentiation. Resistance exercise, which produces greater ground reaction forces and muscle tension than aerobic exercise, elicits a more robust myokine-mediated osteogenic response, explaining the superior effects of RET on bone mineral density [
189,
200,
222,
223,
224]
3.2.14. General Effects of Physical Training on Myokine Expression
Both resistance exercise training (RET) and endurance training (ET) exert profound effects on the myokine profile, though with distinct patterns that reflect their different physiological demands and adaptations. Resistance training preferentially activates pathways that promote muscle protein synthesis, satellite cell proliferation, and hypertrophy while simultaneously suppressing catabolic signals.
Endurance training predominantly enhances metabolic flexibility, mitochondrial function, and oxidative capacity through complementary myokine signalling. The optimal approach for most individuals, particularly those with metabolic dysfunction, likely involves combining both modalities to capitalize on their unique and synergistic effects on the myokine profile [
226].
The intensity, duration, frequency, and type of exercise emerge as critical variables that determine the specific myokine response. Moderate to high- intensity training appears particularly effective at stimulating beneficial myokine profiles, though the appropriate intensity must be individualized based on fitness level, health status, and specific therapeutic goals. Exercise prescriptions should be tailored not just to improve conventional markers of fitness but to optimize the myokine-mediated metabolic benefits [
225].
The AMPK-PGC-1α-myokine axis represents a central pathway through which exercise exerts its metabolic benefits. This signalling cascade coordinates the expression and release of multiple myokines, including irisin, IL-6, and BAIBA, which collectively improve glucose homeostasis, enhance fat metabolism, and reduce inflammatory signalling. The ROS-NRF2-antioxidant response pathway provides another critical mechanism through which exercise-induced hormetic stress triggers protective adaptations against oxidative damage and metabolic dysfunction [
148].
3.2.15. Resistance Training and Myokine Expression
Different types of exercise trigger distinct patterns of myokine release, contributing to the specific metabolic and physiological adaptations seen with various training modalities. Resistance exercise training (RET) produces a potent stimulus for myokine secretion, with patterns distinct from those elicited by endurance training (ET). RET at moderate to high intensities (50– 80% 1RM) is a powerful modulator of the myokine profile, activating signalling cascades such as AMPK and mTOR, which are critical for the production of key myokines involved in metabolic regulation [
225,
226].
IL-15 shows a more robust response to RET compared to ET, with plasma IL-15 protein increasing acutely after resistance exercise, while high-volume endurance exercise produces minimal changes in circulating IL-15 levels. This differential response is likely related to the preferential recruitment of type II muscle fibres during RET. The acute increase in IL-15 after RET correlates with improvements in muscle protein synthesis and insulin sensitivity via JAK3/STAT3 signalling [
201]. Chronic RET of moderate to high intensity (8–12 weeks) significantly upregulates irisin production, with the intensity threshold being critical, as low-intensity resistance exercise does not elicit comparable responses. Myostatin expression is effectively suppressed by moderate or higher intensity RET (50–80% 1RM), but not by low-intensity protocols, and this suppression is facilitated by increased follistatin and decorin production, both of which are natural myostatin antagonists [
62,
227].
Decorin levels rise approximately 24 hours after RET, indicating a role in recovery and adaptation. SPARC, another myokine involved in extracellular matrix remodelling, increases acutely after RET and may contribute to long- term structural adaptations with chronic training [
76]. RET has been shown to depress NLRP3 inflammasome activation, with chronic programs longer than 8 weeks associated with decreased circulating levels of proinflammatory cytokines, including TNF-α, inflammatory IL-6, and IFN-γ [
228] The metabolic benefits of RET are intensity-dependent, with high-intensity resistance interval training producing superior effects on myokine profiles compared to lower intensity protocols, and myokine release rates proportional to the intensity and muscle volume recruited during training [
225].
3.2.16. Endurance Training and Myokine Expression
Endurance exercise training (ET) elicits a distinct myokine response profile compared to RET, with the duration of exercise and muscle mass (tissue volume) engagement being primary determinants of the response seen with the ET training adaptation. IL-6, the most extensively studied myokine, increases exponentially in response to endurance exercise duration, with elevations up to 100-fold during prolonged activity. Unlike inflammatory IL-6 production, exercise-induced IL-6 from endurance activity occurs without preceding TNF-α elevation and exerts different downstream effects [
90]. The IL-6 response to ET activates AMP-activated protein kinase (AMPK), enhances fat oxidation, upregulates GLUT4 translocation, and mediates anti- inflammatory effects by inhibiting proinflammatory cytokines and stimulating anti-inflammatory mediators such as IL-10 and IL-1Ra, creating an anti- inflammatory environment that improves insulin sensitivity and metabolic health [
193,
194].
BAIBA is another myokine upregulated by ET, with circulating levels increasing significantly after both acute and chronic endurance training. Three weeks of voluntary running is sufficient to elevate plasma concentrations in animal models, and in humans, 20 weeks of submaximal aerobic exercise increases BAIBA, which induces mitochondrial fatty acid oxidation and thermogenesis in white adipose tissue via PPARα-dependent mechanisms [
229]. FGF21 signalling also adapts to ET, with moderate to high-intensity training increasing FGF21 sensitivity, acute increases in serum levels, and chronic training leading to decreased baseline levels, suggesting enhanced tissue responsiveness over time. Exercise-induced FGF21 expression is regulated by AMPK and PPARα activation, with the unfolded protein response contributing during intense exercise [
230].
Irisin shows robust responses to endurance exercise, with aerobic exercise eliciting larger increases in circulating irisin than resistance exercise, especially up to 60 minutes post-exercise. This difference diminishes at later time points, indicating distinct temporal patterns between modalities. Higher volume and moderate to high-intensity aerobic exercise are most effective for stimulating irisin release [
231]. The anti-inflammatory effects of regular moderate- intensity ET are well documented, with programs of 12 or more weeks significantly reducing NLRP3 inflammasome activation and NF-κB signalling, contributing to the systemic anti-inflammatory profile and metabolic benefits
[
232]. Time-course analyses reveal that various myokines exhibit distinct temporal expression patterns after ET, with some, such as IL-6 and SPARC, peaking immediately post-exercise and others showing delayed responses, highlighting the importance of timing in evaluating myokine responses [
225].
4. Conclusions
The intricate network of myokine signalling represents a fundamental mechanism through which skeletal muscle communicates with distant organs to coordinate metabolic adaptations. The evidence presented in this review demonstrates that myokines function as critical chemical messengers and mediators that translate mechanical stimuli into biochemical signals, influencing glucose metabolism, lipid oxidation, inflammation, and tissue remodelling processes. These molecular pathways provide a scientific foundation for understanding how physical exercise produces its remarkable systemic health benefits.
As our understanding of myokine biology continues to evolve, the potential for developing exercise mimetics or myokine-based therapies represents an exciting frontier in metabolic medicine. However, the complex, coordinated, and context-dependent nature of exercise-induced myokine responses at local and systemic levels suggests that physical activity in the form of combined resistance and endurance training remains the most comprehensive, realistic, and applicable intervention for optimizing this system. Future research should focus on articulating the specific effects of different exercise protocols on myokine expression profiles and how these can be leveraged to address individual metabolic needs.
In conclusion, the intricate biochemistry of myokine signalling provides the molecular framework that explains how "exercise is medicine." Through these muscle-derived messengers, physical activity creates a systemic environment that counters metabolic dysfunction, reduces inappropriate inflammation, and enhances cellular energetics. The remarkable plasticity of skeletal muscle and its secretome offers a powerful target for lifestyle interventions aimed at preventing and treating metabolic disorders and age-related functional decline.
Author Contributions
This review was conceptualised and written by the author. The infographic (
Figure 1) was conceptualised and designed by the author. All authors have read and agreed to the published version of the manuscript.
Funding
This review was primarily funded by Sotogard Medical, with secondary funding provided by PharmaMT Ltd, MKPharma Ltd, and ProHealth Ltd.
Conflicts of Interest and Ethics Statements
The author declares no conflict of interest. No human or animal subjects were involved in this review.
References
- Prasun, P. Mitochondrial dysfunction in metabolic syndrome. Biochim Biophys Acta Mol Basis Dis. 2020;1866(10):165838. [CrossRef]
- Akintola AA, van Heemst D. Insulin, aging, and the brain: mechanisms and implications. Front Endocrinol (Lausanne). 2015;6:13. [CrossRef]
- Brown, K. Aging: the mitochondrial connection. J Clin Exp Pathol. 2012;S4(01):1–5. [CrossRef]
- Roubenoff, R. Catabolism of aging: is it an inflammatory process? Curr Opin Clin Nutr Metab Care. 2003;6(3):295–9.
- Harman, D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956;11(3):298–300. [CrossRef]
- Bonomini F, Rodella LF, Rezzani R. Metabolic syndrome, aging and involvement of oxidative stress. Aging Dis. 2015;6(2):109–20. [CrossRef]
- Antuña E, Cachán-Vega C, Bermejo-Millo JC, Potes Y, Caballero B, Vega-Naredo I, et al. Inflammaging: implications in sarcopenia. Int J Mol Sci. 2022;23(23):15039. [CrossRef]
- Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17(2):179–89. [CrossRef]
- Harijith A, Ebenezer DL, Natarajan V. Reactive oxygen species at the crossroads of inflammasome and inflammation. Front Physiol. 2014;5:352. [CrossRef]
- Artemyeva OV, Gankovskaya LV. Inflammaging as the basis of age-associated diseases. Med Immunol (Russ). 2020;22:419–32.
- Pedersen L, Hojman P. Muscle-to-organ cross talk mediated by myokines. Adipocyte. 2012;1(3):164–7.
- Iizuka K, Machida T, Hirafuji M. Skeletal muscle is an endocrine organ. J Pharmacol Sci. 2014;125(2):125–31. [CrossRef]
- Kwon JH, Moon KM, Min KW. Exercise-induced myokines can explain the importance of physical activity in the elderly: an overview. Healthcare (Basel). 2020;8(4):378. [CrossRef]
- Pedersen BK, Febbraio MA. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev. 2008;88(4):1379–406. [CrossRef]
- Austin S, St-Pierre J. PGC1α and mitochondrial metabolism—emerging concepts and relevance in ageing and neurodegenerative disorders. J Cell Sci. 2012;125(Pt 21):4963–71. [CrossRef]
- Afonina IS, Zhong Z, Karin M, Beyaert R. Limiting inflammation—the negative regulation of NF-κB and the NLRP3 inflammasome. Nat Immunol. 2017;18(8):861–9. [CrossRef]
- Kelley N, Jeltema D, Duan Y, He Y. The NLRP3 inflammasome: an overview of mechanisms of activation and regulation. Int J Mol Sci. 2019;20(13):3328. [CrossRef]
- Roberts CK, Sindhu KK. Oxidative stress and metabolic syndrome. Life Sci. 2009;84(21–22):705–12. [CrossRef]
- Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organ J. 2012;5(1):9–19. [CrossRef]
- Liu Y, Wang D, Li T, Yang F, Li Z, Bai X, et al. The role of NLRP3 inflammasome in inflammation-related skeletal muscle atrophy. Front Immunol. 2022;13:889188.
- Bodine SC, Latres E, Baumhueter S, Lai VKM, Nunez L, Clarke BA, et al. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science. 2001;294(5547):1704–8. [CrossRef]
- Li YP, Lecker SH, Chen Y, Waddell ID, Goldberg AL, Reid MB. TNF-α increases ubiquitin-conjugating activity in skeletal muscle by up-regulating UbcH2/E2 20k. FASEB J. 2003;17(9):1048–57.
- Gomes MD, Lecker SH, Jagoe RT, Navon A, Goldberg AL. Atrogin-1, a muscle-specific F-box protein highly expressed during muscle atrophy. Proc Natl Acad Sci U S A. 2001;98(25):14440–5. [CrossRef]
- Späte U, Schulze PC. Proinflammatory cytokines and skeletal muscle. Curr Opin Clin Nutr Metab Care. 2004;7(3):265–9.
- Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes. 2002;51(10):2944–50. [CrossRef]
- Li YP, Schwartz RJ. TNF-α regulates early differentiation of C2C12 myoblasts in an autocrine fashion. FASEB J. 2001;15(8):1413–5. [CrossRef]
- Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17(2):179–89. [CrossRef]
- Emery P, Keystone E, Tony HP, Cantagrel A, Van Vollenhoven R, Sanchez A, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis. 2008;67(11):1516–23. [CrossRef]
- Meroni PL, Valesini G. Tumour necrosis factor α antagonists in the treatment of rheumatoid arthritis: an immunological perspective. BioDrugs. 2014;28(2):143–59.
- Mitoma H, Horiuchi T, Tsukamoto H, Ueda N. Molecular mechanisms of action of anti-TNF-α agents—comparison among therapeutic TNF-α antagonists. Cytokine. 2018;101:56–63. [CrossRef]
- Phillips T, Leeuwenburgh C. Muscle fiber specific apoptosis and TNF-alpha signaling in sarcopenia are attenuated by life-long calorie restriction. FASEB J. 2005;19(6):668–70. [CrossRef]
- Schaap LA, Pluijm SMF, Deeg DJH, Harris TB, Kritchevsky SB, Newman AB, et al. Higher inflammatory marker levels in older persons: associations with 5-year change in muscle mass and muscle strength. J Gerontol A Biol Sci Med Sci. 2009;64(11):1183–9. [CrossRef]
- Wang Y, Wehling-Henricks M, Samengo G, Tidball JG. Increases of M2a macrophages and fibrosis in aging muscle are influenced by bone marrow aging and negatively regulated by muscle-derived nitric oxide. Aging Cell. 2015;14(4):678–88. [CrossRef]
- Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK. Reactive oxygen species in metabolic and inflammatory signaling. Circ Res. 2018;122(6):877–902. [CrossRef]
- Bhatti JS, Bhatti GK, Reddy PH. Mitochondrial dysfunction and oxidative stress in metabolic disorders—a step towards mitochondria based therapeutic strategies. Biochim Biophys Acta Mol Basis Dis. 2017;1863(5):1066–77. [CrossRef]
- Lacy F, O’Connor DT, Schmid-Schönbein GW. Plasma hydrogen peroxide production in hypertensives and normotensive subjects at genetic risk of hypertension. J Hypertens. 1998;16(3):291–303.
- Phillips T, Leeuwenburgh C. Muscle fiber specific apoptosis and TNF-alpha signaling in sarcopenia are attenuated by life-long calorie restriction. FASEB J. 2005;19(6):668–70. [CrossRef]
- Trenerry MK, Carey KA, Ward AC, Farnfield MM, Cameron-Smith D. Exercise-induced activation of STAT3 signaling is increased with age. Rejuvenation Res. 2008;11(4):717–24. [CrossRef]
- Trenerry MK, Carey KA, Ward AC, Cameron-Smith D. STAT3 signaling is activated in human skeletal muscle following acute resistance exercise. J Appl Physiol. 2007;102(4):1483–9. [CrossRef]
- Brochu-Gaudreau K, Rehfeldt C, Blouin R, Bordignon V, Murphy BD, Palin MF. Adiponectin action from head to toe. Endocrine. 2010;37(1):11–32.
- Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging and Body Composition (Health ABC) study. Am J Clin Nutr. 2008;87(1):150–5. [CrossRef]
- Dela F, Mikines KJ, Von Linstow M, Secher NH, Galbo H. Effect of training on insulin-mediated glucose uptake in human muscle. Am J Physiol. 1992;263(6 Pt 1):E1134–43. [CrossRef]
- Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–64. [CrossRef]
- Short KR, Bigelow ML, Kahl J, Singh R, Coenen-Schimke J, Raghavakaimal S, Nair KS. Decline in skeletal muscle mitochondrial function with aging in humans. Proc Natl Acad Sci U S A. 2005;102(15):5618–23. [CrossRef]
- Herold MJ, McPherson KG, Reichardt HM. Glucocorticoids in T cell apoptosis and function. Cell Mol Life Sci. 2006;63(1):60–72.
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21(1):55–89. [CrossRef]
- Lambillotte C, Gilon P, Henquin JC. Direct glucocorticoid inhibition of insulin secretion: an in vitro study of dexamethasone effects in mouse islets. J Clin Invest. 1997;99(3):414–23. [CrossRef]
- Paul M, Mehr AP, Kreutz R. Physiology of local renin-angiotensin systems. Physiol Rev. 2006;86(3):747–803. [CrossRef]
- Schmieder RE, Hilgers KF, Schlaich MP, Schmidt BM. Renin-angiotensin system and cardiovascular risk. Lancet. 2007;369(9568):1208–19.
- Kim S, Iwao H. Molecular and cellular mechanisms of angiotensin II-mediated cardiovascular and renal diseases. Pharmacol Rev. 2000;52(1):11–34.
- Kim S, Iwao H. Molecular and cellular mechanisms of angiotensin II-mediated cardiovascular and renal diseases. Pharmacol Rev. 2000;52(1):11–34.
- Haidet AM, Rizo L, Handy C, Umapathi P, Eagle A, Shilling C, et al. Long-term enhancement of skeletal muscle mass and strength by single gene administration of myostatin inhibitors. Proc Natl Acad Sci U S A. 2008;105(11):4318–22. [CrossRef]
- Huh, JY. The role of exercise-induced myokines in regulating metabolism. Arch Pharm Res. 2018;41(1):14–29.
- McPherron AC, Lawler AM, Lee SJ. Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature. 1997;387(6628):83–90. [CrossRef]
- Sharma M, McFarlane C, Kambadur R, Kukreti H, Bonala S, Srinivasan S. Myostatin: expanding horizons. IUBMB Life. 2015;67(8):589–600. [CrossRef]
- Guo T, Jou W, Chanturiya T, Portas J, Gavrilova O, McPherron AC. Myostatin inhibition in muscle, but not adipose tissue, decreases fat mass and improves insulin sensitivity. PLoS One. 2009;4(3):e4937. [CrossRef]
- Kim JS, Cross JM, Bamman MM. Impact of resistance loading on myostatin expression and cell cycle regulation in young and older men and women. Am J Physiol Endocrinol Metab. 2005;288(6):E1110–9. [CrossRef]
- Rodgers BD, Garikipati DK. Clinical, agricultural, and evolutionary biology of myostatin: a comparative review. Endocr Rev. 2008;29(5):513–34. [CrossRef]
- Weber IT, Harrison RW, Iozzo RV. Model structure of decorin and implications for collagen fibrillogenesis. J Biol Chem. 1996;271(50):31767–70. [CrossRef]
- Brandan E, Fuentes ME, Andrade W. The proteoglycan decorin is synthesized and secreted by differentiated myotubes. Eur J Cell Biol. 1991;55(2):192–200.
- Gubbiotti MA, Neill T, Frey H, Schaefer L, Iozzo RV. Decorin is an autophagy-inducible proteoglycan and is required for proper in vivo autophagy. Matrix Biol. 2015;48:14–25.
- Relizani K, Mouisel E, Giannesini B, Hourdé C, Patel K, Morales Gonzalez S, et al. Blockade of ActRIIB signaling triggers muscle hypertrophy and muscle strength gain in adult and aged mice. Skelet Muscle. 2014;4:34.
- Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372(6505):425–32. [CrossRef]
- Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395(6704):763–70. [CrossRef]
- Fain JN, Bahouth SW, Madan AK. Leptin and the interleukins. Vitam Horm. 2005;71:237–76.
- Jamaluddin MS, Weakley SM, Yao Q, Chen C. Resistin: functional roles and therapeutic considerations for cardiovascular disease. Br J Pharmacol. 2012;165(3):622–32. [CrossRef]
- Jung HS, Park KH, Cho YM, Chung SS, Cho HJ, Cho SY, et al. Resistin is secreted from macrophages in atheromas and promotes atherosclerosis. Cardiovasc Res. 2006;69(1):76–85. [CrossRef]
- Xu W, Yu L, Zhou W, Luo M. Resistin increases lipid accumulation and CD36 expression in human macrophages. Biochem Biophys Res Commun. 2006;351(2):376–82. [CrossRef]
- Lee TS, Lin CY, Tsai JY, Wu YL, Su KH, Lu KY, et al. Resistin increases lipid accumulation by affecting class A scavenger receptor, CD36 and ATP-binding cassette transporter-A1 in macrophages. Life Sci. 2009;84(3–4):97–104. [CrossRef]
- Wallenius V, Wallenius K, Ahren B, et al. Interleukin-6-deficient mice develop mature-onset obesity. Nat Med. 2002;8(1):75–9. [CrossRef]
- Matthews VB, Allen TL, Risis S, Chan MHS, Henstridge DC, Watson N, et al. Interleukin-6-deficient mice develop hepatic inflammation and systemic insulin resistance. Diabetologia. 2010;53(11):2431–41.
- Kwon H, Pessin JE. Adipokines mediate inflammation and insulin resistance. Front Endocrinol (Lausanne). 2013;4:71. [CrossRef]
- Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP. The pathophysiologic roles of interleukin-6 in human disease. Ann Intern Med. 1998;128(2):127–37. [CrossRef]
- Pedersen, BK. Muscular interleukin-6 and its role as an energy sensor. Med Sci Sports Exerc. 2012;44(3):392–6.
- Ghanemi A, Yoshioka M, St-Amand J. Secreted protein acidic and rich in cysteine as an exercise-induced gene: towards novel molecular therapies for immobilization-related muscle atrophy in elderly patients. Genes (Basel). 2022;13(6):1014. [CrossRef]
- Ghanemi A, Melouane A, Yoshioka M, St-Amand J. Exercise training of secreted protein acidic and rich in cysteine (Sparc) KO mice suggests that exercise-induced muscle phenotype changes are SPARC-dependent. Appl Sci. 2020;10(24):9108. [CrossRef]
- Zhong X, Huang M, Kim HG, Zhang Y, Chowdhury K, Cai W, et al. SIRT6 protects against liver fibrosis by deacetylation and suppression of SMAD3 in hepatic stellate cells. Cell Mol Gastroenterol Hepatol. 2020;10(2):341–56. [CrossRef]
- Khan D, Ara T, Ravi V, Rajagopal R, Tandon H, Parvathy J, et al. SIRT6 transcriptionally regulates fatty acid transport by suppressing PPARγ. Cell Rep. 2021;35(9):109193. [CrossRef]
- Lee DH, Ha MH, Kim JH, Christiani DC, Gross MD, Steffes M, et al. Gamma-glutamyltransferase and diabetes—a 4 year follow-up study. Diabetologia. 2003;46(3):359–64.
- Lexell J, Taylor CC, Sjöström M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J Neurol Sci. 1988;84(2–3):275–94. [CrossRef]
- Andersen JL, Schjerling P, Andersen LL, Dela F. Resistance training and insulin action in humans: effects of de-training. J Physiol. 2003;551(3):1049–58. [CrossRef]
- Schiaffino S, Dyar KA, Ciciliot S, Blaauw B, Sandri M. Mechanisms regulating skeletal muscle growth and atrophy. FEBS J. 2013;280(17):4294–314. [CrossRef]
- Komatsu T, Park S, Hayashi H, Mori R, Yamaza H, Shimokawa I. Mechanisms of calorie restriction: a review of genes required for the life-extending and tumor-inhibiting effects of calorie restriction. Nutrients. 2019;11(12):3068. [CrossRef]
- Komatsu M, Waguri S, Chiba T, Murata S, Iwata JI, Tanida I, et al. Loss of autophagy in the central nervous system causes neurodegeneration in mice. Nature. 2006;441(7095):880–4. [CrossRef]
- Pedersen BK, Febbraio MA. Muscles, exercise and obesity: Skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8(8):457–65. [CrossRef]
- Messina JM, Luo M, Hossan MS, Gadelrab HA, Yang X, John A, et al. Unveiling Cytokine Charge Disparity as a Potential Mechanism for Immune Regulation. Cytokine Growth Factor Rev. 2023;77:1–10. https://pmc.ncbi.nlm.nih.gov/articles/PMC11923798/.
- Kato Y, Ozawa S, Miyamoto C, Maehata Y, Suzuki A, Maeda T, et al. Acidic extracellular microenvironment and cancer. Cancer Cell Int. 2013;13(1):89. [CrossRef]
- Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta Mol Cell Res. 2011;1813(5):878–88. [CrossRef]
- Pedersen BK, Steensberg A, Fischer C, Keller C, Keller P, Plomgaard P, et al. Searching for the exercise factor: Is IL-6 a candidate? J Muscle Res Cell Motil. 2003;24(2–3):113–9.
- Tidball, JG. Regulation of muscle growth and regeneration by the immune system. Nat Rev Immunol. 2017;17(3):165–78. [CrossRef]
- Dinarello, CA. Historical insights into cytokines. Eur J Immunol. 2007;37(Suppl 1):S34–45. [CrossRef]
- Medzhitov, R. Origin and physiological roles of inflammation. Nature. 2008;454(7203):428–35. [CrossRef]
- O’Shea J, Paul WE. Mechanisms underlying lineage commitment and plasticity of helper CD4+ T cells. Science. 2010;327(5969):1098–102. [CrossRef]
- Guadagnin E, Mázala D, Chen YW. STAT3 in Skeletal Muscle Function and Disorders. Int J Mol Sci. 2018;19(8):2265. [CrossRef]
- Risson V, Mazelin L, Roceri M, Sanchez H, Moncollin V, Corneloup C, et al. Muscle inactivation of mTOR causes metabolic and dystrophin defects leading to severe myopathy. J Cell Biol. 2009;187(6):859–74. [CrossRef]
- Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS, et al. AMPK Phosphorylation of Raptor Mediates a Metabolic Checkpoint. Mol Cell. 2008;30(2):214–26. [CrossRef]
- Inoki K, Zhu T, Guan KL. TSC2 Mediates Cellular Energy Response to Control Cell Growth and Survival. Cell. 2003;115(5):577–90. [CrossRef]
- Dos DS, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, et al. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol. 2004;14(14):1296–302. [CrossRef]
- Saxton RA, Sabatini DM. mTOR Signaling in Growth, Metabolism, and Disease. Cell. 2017;168(6):960–76. [CrossRef]
- Komatsu M, Waguri S, Ueno T, Iwata J, Murata S, Tanida I, et al. Impairment of starvation-induced and constitutive autophagy in Atg7-deficient mice. J Cell Biol. 2005;169(3):425–34. [CrossRef]
- Pedersen, BK. Muscles and their myokines. J Exp Biol. 2011;214(Pt 2):337–46. [CrossRef]
- Calabrese, EJ. Hormetic mechanisms. Crit Rev Toxicol. 2013;43(7):580–606. [CrossRef]
- Ji LL, Kang C, Zhang Y. Exercise-induced hormesis and skeletal muscle health. Free Radic Biol Med. 2016;98:113–22. [CrossRef]
- Ji LL, Gomez-Cabrera MC, Vina J. Role of nuclear factor κB and mitogen-activated protein kinase signaling in exercise-induced antioxidant enzyme adaptation. Appl Physiol Nutr Metab. 2007;32(5):930–5. [CrossRef]
- Gudowska-Sawczuk M, Mroczko B. The Role of Nuclear Factor Kappa B (NF-κB) in Development and Treatment of COVID-19: Review. Int J Mol Sci. 2022;23(10):5283.
- Bąska P, Norbury LJ. The Role of Nuclear Factor Kappa B (NF-κB) in the Immune Response against Parasites. Pathogens. 2022;11(7):796. [CrossRef]
- Pfeffer, LM. The role of nuclear factor κb in the interferon response. J Interferon Cytokine Res. 2011;31(7):553–9. [CrossRef]
- Powers SK, Duarte J, Kavazis AN, Talbert EE. Reactive oxygen species are signalling molecules for skeletal muscle adaptation. Exp Physiol. 2010;95(1):1–9. [CrossRef]
- Radak Z, Chung HY, Goto S. Systemic adaptation to oxidative challenge induced by regular exercise. Free Radic Biol Med. 2008;44(2):153–9. [CrossRef]
- Steinbacher P, Eckl P. Impact of oxidative stress on exercising skeletal muscle. Biomolecules. 2015;5(2):356–77. [CrossRef]
- Gurd BJ, Perry CGR, Heigenhauser GJF, Spriet LL, Bonen A. High-intensity interval training increases SIRT1 activity in human skeletal muscle. Appl Physiol Nutr Metab. 2010;35(3):350–7. [CrossRef]
- Cassidy S, Thoma C, Houghton D, Trenell MI. High-intensity interval training: a review of its impact on glucose control and cardiometabolic health. Diabetologia. 2017;60(1):7–23. [CrossRef]
- Powers SK, Smuder AJ, Criswell DS. Mechanistic links between oxidative stress and disuse muscle atrophy. Antioxid Redox Signal. 2011;15(9):2519–28. [CrossRef]
- Yue F, Cheng Y, Breschi A, Vierstra J, Wu W, Ryba T, et al. A comparative encyclopedia of DNA elements in the mouse genome. Nature. 2014;515(7527):355–64. [CrossRef]
- Campos JC, Gomes KMS, Ferreira JCB. Impact of exercise training on redox signaling in cardiovascular diseases. Food Chem Toxicol. 2013;62:107–19. [CrossRef]
- Thirupathi A, Wang M, Lin JK, Fekete G, István B, Baker JS, et al. Effect of Different Exercise Modalities on Oxidative Stress: A Systematic Review. Biomed Res Int. 2021;2021:1947928. [CrossRef]
- Niki, E. Oxidative stress and antioxidants: Distress or eustress? Arch Biochem Biophys. 2016;595:19–24. [CrossRef]
- Sinert R, Kohl L, Rainone T, Scalea T. Exercise-Induced Rhabdomyolysis. Ann Emerg Med. 1994;23(6):1301–6.
- Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: An evaluation of 475 hospitalized patients. Medicine (Baltimore). 2005;84(6):377–85. [CrossRef]
- Scalco RS, Snoeck M, Quinlivan R, Treves S, Laforét P, Jungbluth H, et al. Exertional rhabdomyolysis: physiological response or manifestation of an underlying myopathy? BMJ Open Sport Exerc Med. 2016;2(1):e000151. [CrossRef]
- Furman, J. When exercise causes exertional rhabdomyolysis. J Am Acad Physician Assist. 2015;28(4):38–43.
- Adhikari P, Hari A, Morel L, Bueno Y. Exertional Rhabdomyolysis After CrossFit Exercise. Cureus. 2021;13(1):e12638. [CrossRef]
- Rath P, Fichadiya H, Elkattawy S, Jesani S, Messalti M, Fichadiya H, et al. Acute Compartment Syndrome in the Setting of Weight Loss Supplements and Exercise-Induced Rhabdomyolysis. Eur J Case Rep Intern Med. 2022;9(3):003073.
- Aalborg C, Rød-Larsen C, Leiro I, Aasebø W. An increase in the number of admitted patients with exercise-induced rhabdomyolysis. Tidsskr Nor Laegeforen. 2016;136(18):1556–8. [CrossRef]
- Al Badi A, Al Rasbi S, Alalawi AM. Exercise-Induced Rhabdomyolysis: A Case Report and Literature Review. Cureus. 2020;12(3):e7237. [CrossRef]
- Kim J, Lee J, Kim S, Ryu HY, Cha KS, Sung DJ. Exercise-induced rhabdomyolysis mechanisms and prevention: A literature review. J Sport Health Sci. 2016;5(3):324–33. [CrossRef]
- Wilborn CD, Taylor LW, Greenwood M, Kreider RB, Willoughby DS. Effects of different intensities of resistance exercise on regulators of myogenesis. J Strength Cond Res. 2009;23(8):2179–87.
- Thirupathi A, Wang M, Lin JK, Fekete G, István B, Baker JS, et al. Effect of Different Exercise Modalities on Oxidative Stress: A Systematic Review. Biomed Res Int. 2021;2021:1947928. [CrossRef]
- Ji LL, Gomez-Cabrera MC, Vina J. Exercise and hormesis: Activation of cellular antioxidant signaling pathway. Ann N Y Acad Sci. 2006;1067:425–35. [CrossRef]
- Sun Y, Ge Y, Drnevich J, Zhao Y, Band M, Chen J. Mammalian target of rapamycin regulates miRNA-1 and follistatin in skeletal myogenesis. J Cell Biol. 2010;189(7):1157–69. [CrossRef]
- Phillips, SM. A brief review of critical processes in exercise-induced muscular hypertrophy. Sports Med. 2014;44(Suppl 1):S71–7. [CrossRef]
- Pearson, AM. Muscle growth and exercise. Crit Rev Food Sci Nutr. 1990;29(3):167–96. [CrossRef]
- McCall GE, Byrnes WC, Dickinson A, Pattany PM, Fleck SJ. Muscle fiber hypertrophy, hyperplasia, and capillary density in college men after resistance training. J Appl Physiol (1985). 1996;81(5):2004–12. [CrossRef]
- Kraemer WJ, Duncan ND, Volek JS. Resistance Training and Elite Athletes: Adaptations and Program Considerations. J Orthop Sports Phys Ther. 1998;28(2):110–9. [CrossRef]
- Kraemer WJ, Ratamess NA. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. 2004;36(4):674–88. [CrossRef]
- Schoenfeld, BJ. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. 2010;24(10):2857–72. [CrossRef]
- Chargé SBP, Rudnicki MA. Cellular and Molecular Regulation of Muscle Regeneration. Physiol Rev. 2004;84(1):209–38. [CrossRef]
- Seale P, Sabourin LA, Girgis-Gabardo A, Mansouri A, Gruss P, Rudnicki MA. Pax7 is required for the specification of myogenic satellite cells. Cell. 2000;102(6):777–86. [CrossRef]
- Zammit PS, Golding JP, Nagata Y, Hudon V, Partridge TA, Beauchamp JR. Muscle satellite cells adopt divergent fates: A mechanism for self-renewal? J Cell Biol. 2004;166(3):347–57. [CrossRef]
- Shea KL, Xiang W, LaPorta VS, Licht JD, Keller C, Basson MA, et al. Sprouty1 regulates reversible quiescence of a self-renewing adult muscle stem cell pool during regeneration. Cell Stem Cell. 2010;6(2):117–29. [CrossRef]
- Tidball JG, Villalta SA. Regulatory interactions between muscle and the immune system during muscle regeneration. Am J Physiol Regul Integr Comp Physiol. 2010;298(5):R1173–87. [CrossRef]
- Chin ER, Olson EN, Richardson JA, Yang Q, Humphries C, Shelton JM, et al. A calcineurin-dependent transcriptional pathway controls skeletal muscle fiber type. Genes Dev. 1998;12(16):2499–509. [CrossRef]
- O’Shea JJ, Gadina M, Schreiber RD. Cytokine signaling in 2002: New surprises in the Jak/Stat pathway. Cell. 2002;109(Suppl):S121–31. [CrossRef]
- Zimmers TA, Fishel ML, Bonetto A. STAT3 in the systemic inflammation of cancer cachexia. Semin Cell Dev Biol. 2016;54:28–41. [CrossRef]
- Handschin C, Spiegelman BM. The role of exercise and PGC1α in inflammation and chronic disease. Nature. 2008;454(7203):463–9. [CrossRef]
- Di Meo S, Iossa S, Venditti P. Skeletal muscle insulin resistance: Role of mitochondria and other ROS sources. J Endocrinol. 2017;233(1):R15–42.
- Chen D, Bruno J, Easlon E, Lin SJ, Cheng HL, Alt FW, et al. Tissue-specific regulation of SIRT1 by calorie restriction. Genes Dev. 2008;22(13):1753–7. [CrossRef]
- Lamb DA, Moore JH, Mesquita PHC, Smith MA, Vann CG, Osburn SC, et al. Resistance training increases muscle NAD+ and NADH concentrations as well as NAMPT protein levels and global sirtuin activity in middle-aged, overweight, untrained individuals. Aging (Albany NY). 2020;12(10):9447–60. [CrossRef]
- Herzig S, Shaw RJ. AMPK: guardian of metabolism and mitochondrial homeostasis. Nat Rev Mol Cell Biol. 2018;19(2):121–35. [CrossRef]
- Lin SC, Hardie DG. AMPK: Sensing Glucose as well as Cellular Energy Status. Cell Metab. 2018;27(2):299–313.
- Lamb DA, Moore JH, Mesquita PHC, Smith MA, Vann CG, Osburn SC, et al. Resistance training increases muscle NAD+ and NADH concentrations as well as NAMPT protein levels and global sirtuin activity in middle-aged, overweight, untrained individuals. Aging (Albany NY). 2020;12(10):9447–60. [CrossRef]
- Herzig S, Shaw RJ. AMPK: guardian of metabolism and mitochondrial homeostasis. Nat Rev Mol Cell Biol. 2018;19(2):121–35. [CrossRef]
- Lin SC, Hardie DG. AMPK: Sensing Glucose as well as Cellular Energy Status. Cell Metab. 2018;27(2):299–313.
- Hardie DG, Ross FA, Hawley SA. AMPK: A nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol. 2012;13(4):251–62. [CrossRef]
- Zhang Y, Yang X, Bian F, Wu P, Xing S, Xu G, et al. TNF-α promotes early atherosclerosis by increasing transcytosis of LDL across endothelial cells: Crosstalk between NF-κB and PPAR-γ. J Mol Cell Cardiol. 2014;72:85–94. [CrossRef]
- Bordone L, Motta MC, Picard F, Robinson A, Jhala US, Apfeld J, et al. Sirt1 regulates insulin secretion by repressing UCP2 in pancreatic β cells. PLoS Biol. 2006;4(2):e31. [CrossRef]
- Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, et al. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1α. Cell. 2006;127(6):1109–22. [CrossRef]
- Gurd BJ, Yoshida Y, McFarlan JT, Holloway GP, Moyes CD, Heigenhauser GJF, et al. Nuclear SIRT1 activity, but not protein content, regulates mitochondrial biogenesis in rat and human skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2011;301(1):R67–75. [CrossRef]
- Kersten S, Rakhshandehroo M, Knoch B, Müller M. Peroxisome proliferator-activated receptor alpha target genes. PPAR Res. 2010;2010:612089. [CrossRef]
- Desvergne B, Wahli W. Peroxisome Proliferator-Activated Receptors: Nuclear Control of Metabolism. Endocr Rev. 1999;20(5):649–88. [CrossRef]
- Wang YX, Lee CH, Tiep S, Yu RT, Ham J, Kang H, et al. Peroxisome-proliferator-activated receptor δ activates fat metabolism to prevent obesity. Cell. 2003;113(2):159–70. [CrossRef]
- Issemann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990;347(6294):645–50. [CrossRef]
- Grimble, RF. Inflammatory status and insulin resistance. Curr Opin Clin Nutr Metab Care. 2002;5(5):551–9. [CrossRef]
- Kang K, Reilly SM, Karabacak V, Gangl MR, Fitzgerald K, Hatano B, et al. Adipocyte-derived Th2 cytokines and myeloid PPARδ regulate macrophage polarization and insulin sensitivity. Cell Metab. 2008;7(6):485–95. [CrossRef]
- Tontonoz P, Nagy L, Alvarez JGA, Thomazy VA, Evans RM. PPARγ promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell. 1998;93(2):241–52. [CrossRef]
- Lehmann JM, Moore LB, Smith-Oliver TA, Wilkison WO, Willson TM, Kliewer SA. An antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor γ (PPARγ). J Biol Chem. 1995;270(22):12953–6. [CrossRef]
- Herzig S, Long F, Jhala US, Hedrick S, Quinn R, Bauer A, et al. CREB regulates hepatic gluconeogenesis through the coactivator PGC-1. Nature. 2001;413(6852):179–83. [CrossRef]
- Valle I, Álvarez-Barrientos A, Arza E, Lamas S, Monsalve M. PGC-1α regulates the mitochondrial antioxidant defense system in vascular endothelial cells. Cardiovasc Res. 2005;66(3):562–73. [CrossRef]
- St-Pierre J, Drori S, Uldry M, Silvaggi JM, Rhee J, Jäger S, et al. Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell. 2006;127(2):397–408. [CrossRef]
- Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, et al. Transcriptional co-activator PGC-1α drives the formation of slow-twitch muscle fibres. Nature. 2002;418(6899):797–801. [CrossRef]
- Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481(7382):463–8. [CrossRef]
- Puigserver P, Wu Z, Park CW, Graves R, Wright M, Spiegelman BM. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell. 1998;92(6):829–39. [CrossRef]
- Shen Y, Wu Q, Shi J, Zhou S. Regulation of SIRT3 on mitochondrial functions and oxidative stress in Parkinson’s disease. Biomed Pharmacother. 2020;132:110928. [CrossRef]
- Pardo PS, Boriek AM. The physiological roles of Sirt1 in skeletal muscle. Aging (Albany NY). 2011;3(4):430–7. [CrossRef]
- Tao R, Coleman MC, Pennington JD, Ozden O, Park SH, Jiang H, et al. Sirt3-mediated deacetylation of evolutionarily conserved lysine 122 regulates MnSOD activity in response to stress. Mol Cell. 2010;40(6):893–904. [CrossRef]
- Nagai K, Matsushita T, Matsuzaki T, Takayama K, Matsumoto T, Kuroda R, et al. Depletion of SIRT6 causes cellular senescence, DNA damage, and telomere dysfunction in human chondrocytes. Osteoarthritis Cartilage. 2015;23(8):1412–20. [CrossRef]
- Nguyen T, Nioi P, Pickett CB. The Nrf2-Antioxidant Response Element Signaling Pathway and Its Activation by Oxidative Stress. J Biol Chem. 2009;284(20):13291–5. [CrossRef]
- Owuor ED, Kong ANT. Antioxidants and oxidants regulated signal transduction pathways. Biochem Pharmacol. 2002;64(5–6):765–70.
- Shih AY, Imbeault S, Barakauskas V, Erb H, Jiang L, Li P, et al. Induction of the Nrf2-driven antioxidant response confers neuroprotection during mitochondrial stress in vivo. J Biol Chem. 2005;280(24):22925–36.
- Calabrese EJ, Kozumbo WJ. The hormetic dose-response mechanism: Nrf2 activation. Pharmacol Res. 2021;167:105526. [CrossRef]
- Nguyen T, Sherratt PJ, Pickett CB. Regulatory Mechanisms Controlling Gene Expression Mediated by the Antioxidant Response Element. Annu Rev Pharmacol Toxicol. 2003;43:233–60. [CrossRef]
- Vomhof-DeKrey EE, Picklo MJ. The Nrf2-antioxidant response element pathway: a target for regulating energy metabolism. J Nutr Biochem. 2012;23(10):1201–6. [CrossRef]
- Done AJ, Traustadóttir T. Nrf2 mediates redox adaptations to exercise. Redox Biol. 2016;10:191–9. [CrossRef]
- Brutsaert TD, Gavin TP, Fu Z, Breen EC, Tang K, Mathieu-Costello O, et al. Regional differences in expression of VEGF mRNA in rat gastrocnemius following 1 hr exercise or electrical stimulation. BMC Physiol. 2002;2:8. [CrossRef]
- Alizadeh, H. Myokine-mediated exercise effects: the role of myokine meteorin-like hormone (Metrnl). Growth Factors. 2022;39(1–2):1–9.
- Severinsen MCK, Pedersen BK. Muscle–Organ Crosstalk: The Emerging Roles of Myokines. Endocr Rev. 2020;41(4):594–609. [CrossRef]
- Gaitanos GC, Williams C, Boobis LH, Brooks S. Human muscle metabolism during intermittent maximal exercise. J Appl Physiol. 1993;75(2):712–9. [CrossRef]
- Raschke S, Eckel J. Adipo-Myokines: Two sides of the same coin—Mediators of inflammation and mediators of exercise. Mediators Inflamm. 2013;2013:320724. [CrossRef]
- Kitase Y, Vallejo JA, Gutheil W, Vemula H, Jähn K, Yi J, et al. β-aminoisobutyric Acid, L-BAIBA, Is a Muscle-Derived Osteocyte Survival Factor. Cell Rep. 2018;22(6):1531–44.
- Morales FE, Forsse JS, Andre TL, McKinley-Barnard SK, Hwang PS, Anthony IG, et al. BAIBA Does Not Regulate UCP-3 Expression in Human Skeletal Muscle as a Response to Aerobic Exercise. J Am Coll Nutr. 2017;36(3):200–9.
- Fischer, CP. Interleukin-6 in acute exercise and training: what is the biological relevance? Exerc Immunol Rev. 2006;12:6–33. https://pubmed.ncbi.nlm.nih.gov/17201070/. 1720. [Google Scholar]
- Wolsk E, Mygind H, Grøndahl TS, Pedersen BK, Van Hall G. IL-6 selectively stimulates fat metabolism in human skeletal muscle. Am J Physiol Endocrinol Metab. 2010;299(5):E832–40. [CrossRef]
- Hoene M, Weigert C. The role of interleukin-6 in insulin resistance, body fat distribution and energy balance. Obes Rev. 2008;9(1):20–9.
- Muñoz-Cánoves P, Scheele C, Pedersen BK, Serrano AL. Interleukin-6 myokine signaling in skeletal muscle: a double-edged sword? FEBS J. 2013;280(17):4131–48. [CrossRef]
- Broholm C, Laye MJ, Brandt C, Vadalasetty R, Pilegaard H, Pedersen BK, et al. LIF is a contraction-induced myokine stimulating human myocyte proliferation. J Appl Physiol. 2011;111(1):251–9. [CrossRef]
- Spangenburg EE, Booth FW. Leukemia inhibitory factor restores the hypertrophic response to increased loading in the LIF(-/-) mouse. Cytokine. 2006;34(3–4):125–30. [CrossRef]
- Nadeau L, Patten DA, Caron A, Garneau L, Pinault-Masson E, Foretz M, et al. IL-15 improves skeletal muscle oxidative metabolism and glucose uptake in association with increased respiratory chain supercomplex formation and AMPK pathway activation. Biochim Biophys Acta Gen Subj. 2019;1863(2):317–30. [CrossRef]
- Quinn LS, Anderson BG, Strait-Bodey L, Stroud AM, Argilés JM. Interleukin-15 stimulates C2 skeletal myoblast differentiation. Biochem Biophys Res Commun. 2002;297(1):83–8.
- Rinnov A, Yfanti C, Nielsen S, Åkerström TCA, Peijs L, Zankari A, et al. Endurance training enhances skeletal muscle interleukin-15 in human male subjects. Endocrine. 2014;45(2):271–8.
- Pistilli EE, Quinn LS. From anabolic to oxidative: Reconsidering the roles of IL-15 and IL-15Rα in skeletal muscle. Exerc Sport Sci Rev. 2013;41(2):96–104.
- Ghanemi A, Yoshioka M, St-Amand J. Secreted protein acidic and rich in cysteine as a molecular physiological and pathological biomarker. Biomolecules. 2021;11(11):1628. [CrossRef]
- Nie J, Sage EH. SPARC functions as an inhibitor of adipogenesis. J Cell Commun Signal. 2009;3(3–4):239–46. [CrossRef]
- Termine JD, Kleinman HK, Whitson SW, Conn KM, McGarvey ML, Martin GR. Osteonectin, a bone-specific protein linking mineral to collagen. Cell. 1981;26(1 Pt 1):99–105. [CrossRef]
- Gomarasca M, Banfi G, Lombardi G. Myokines: The endocrine coupling of skeletal muscle and bone. Adv Clin Chem. 2020;94:155–218.
- Son JS, Chae SA, Testroet ED, Du M, Jun H. Exercise-induced myokines: a brief review of controversial issues of this decade. Expert Rev Endocrinol Metab. 2018;13(1):51–8.
- Lee SJ, McPherron AC. Regulation of myostatin activity and muscle growth. Proc Natl Acad Sci U S A. 2001;98(16):9306–11. [CrossRef]
- Chung HS, Hwang SY, Choi JH, Lee HJ, Kim NH, Yoo HJ, et al. Implications of circulating Meteorin-like (Metrnl) level in human subjects with type 2 diabetes. Diabetes Res Clin Pract. 2018;136:100–7. [CrossRef]
- Rao RR, Long JZ, White JP, Svensson KJ, Lou J, Lokurkar I, et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell. 2014;157(6):1279–91. [CrossRef]
- Wrann CD, White JP, Salogiannnis J, Laznik-Bogoslavski D, Wu J, Ma D, et al. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 2013;18(5):649–59. [CrossRef]
- Philippou A, Maridaki M, Halapas A, Koutsilieris M. The role of the insulin-like growth factor 1 (IGF-1) in skeletal muscle physiology. In Vivo. 2007;21(1):45–54.
- Takemura Y, Ouchi N, Shibata R, Aprahamian T, Kirber MT, Summer RS, et al. Adiponectin modulates inflammatory reactions via calreticulin receptor-dependent clearance of early apoptotic bodies. J Clin Invest. 2007;117(2):375–86. [CrossRef]
- Medoff BD, Okamoto Y, Leyton P, Weng M, Sandall BP, Raher MJ, et al. Adiponectin deficiency increases allergic airway inflammation and pulmonary vascular remodeling. Am J Respir Cell Mol Biol. 2009;41(4):397–406.
- Pang J, Rhodes DH, Pini M, Akasheh RT, Castellanos KJ, Cabay RJ, et al. Increased Adiposity, Dysregulated Glucose Metabolism and Systemic Inflammation in Galectin-3 KO Mice. PLoS One. 2013;8(2):e57915. [CrossRef]
- Ellingsgaard H, Hauselmann I, Schuler B, Habib AM, Baggio LL, Meier DT, et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat Med. 2011;17(11):1481–9. [CrossRef]
- Deng J, Zhang N, Chen F, Yang C, Ning H, Xiao C, et al. Irisin ameliorates high glucose-induced cardiomyocytes injury via AMPK/mTOR signal pathway. Cell Biol Int. 2020;44(11):2334–43. [CrossRef]
- Mazur-Bialy AI, Pocheć E, Zarawski M. Anti-inflammatory properties of irisin, mediator of physical activity, are connected with TLR4/Myd88 signaling pathway activation. Int J Mol Sci. 2017;18(4):701. [CrossRef]
- Ushach I, Arrevillaga-Boni G, Heller GN, Pone E, Hernandez-Ruiz M, Catalan-Dibene J, et al. Meteorin-like/Meteorin-β Is a Novel Immunoregulatory Cytokine Associated with Inflammation. J Immunol. 2018;201(12):3669–76. [CrossRef]
- Rose-John, S. Interleukin-6 family cytokines. Cold Spring Harb Perspect Biol. 2018;10(2):a028415. [CrossRef]
- Frost, HM. Bone “mass” and the “mechanostat”: A proposal. Anat Rec. 1987;219(1):1–9. [CrossRef]
- Tanianskii DA, Jarzebska N, Birkenfeld AL, O’Sullivan JF, Rodionov RN. Beta-aminoisobutyric acid as a novel regulator of carbohydrate and lipid metabolism. Nutrients. 2019;11(3):524. [CrossRef]
- Colaianni G, Cuscito C, Mongelli T, Oranger A, Mori G, Brunetti G, et al. Irisin enhances osteoblast differentiation in vitro. Int J Endocrinol. 2014;2014:902186. [CrossRef]
- Damas F, Phillips SM, Libardi CA, Vechin FC, Lixandrão ME, Jannig PR, et al. Resistance training-induced changes in integrated myofibrillar protein synthesis are related to hypertrophy only after attenuation of muscle damage. J Physiol. 2016;594(18):5209–22. [CrossRef]
- Egan B, Zierath JR. Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab. 2013;17(2):162–84. [CrossRef]
- Huh JY, Siopi A, Mougios V, Park KH, Mantzoros CS. Irisin in response to exercise in humans with and without metabolic syndrome. J Clin Endocrinol Metab. 2015;100(3):E453–7. [CrossRef]
- Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–15. [CrossRef]
- Egan B, Zierath JR. Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab. 2013;17(2):162–84. [CrossRef]
- Huh JY, Siopi A, Mougios V, Park KH, Mantzoros CS. Irisin in response to exercise in humans with and without metabolic syndrome. J Clin Endocrinol Metab. 2015;100(3):E453–7. [CrossRef]
- Lira FS, Rosa JC, Yamashita AS, Koyama CH, Batista ML, Seelaender M. Endurance training induces depot-specific changes in IL-10/TNF-α ratio in rat adipose tissue. Cytokine. 2009;45(2):80–5. [CrossRef]
- Roberts LD, Boström P, O’Sullivan JF, Schinzel RT, Lewis GD, Dejam A, et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell Metab. 2014;19(1):96–108. [CrossRef]
- Cuevas-Ramos D, Mehta R, Aguilar-Salinas CA. Fibroblast growth factor 21 and browning of white adipose tissue. Front Physiol. 2019;10:37. [CrossRef]
- Huh JY, Siopi A, Mougios V, Park KH, Mantzoros CS. Irisin in response to exercise in humans with and without metabolic syndrome. J Clin Endocrinol Metab. 2015;100(3):E453–7. [CrossRef]
- Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–15. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).