Submitted:
13 August 2025
Posted:
17 August 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Patient Selection
Data Collection
Review of Medical Records and Examination
Sensory Testing
COMQ-12 Questionnaire
Audiometry
Middle Ear Impedance Testing
Distortion-Product Otoacoustic Emissions (DPOAE)
Ultrasound Examination
Non-Invasive Assessment of Mastoid Function
Results
Characteristics of patients undergoing mastoidectomy
COMQ-12 questionnaire
| Median (IQR) | Mean (st. dev.) |
min.; max. | ||||||
| Q | TM | C | TM | C | TM | C | U | p |
| 1 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,2 (0,61) | 0,0 (0,0) | 0; 3 | 0; 0 | 467,0 | 0,34 |
| 2 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,07 (0,37) | 0,0 (0,0) | 0; 2 | 0; 0 | 464,0 | 0,3 |
| 3 | 0,0 (Q1: 0,0; Q3: 1,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,5 (1,01) | 0,0 (0,0) | 0; 4 | 0; 0 | 352,0 | 0,002 |
| 4 | 0,0 (Q1: 0,0; Q3: 2,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,93 (1,26) | 0,0 (0,0) | 0; 4 | 0; 0 | 288,0 | <0,001 |
| 5 | 0,0 (Q1: 0,0; Q3: 0,25) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,33 (0,71) | 0,0 (0,0) | 0; 3 | 0; 0 | 368,0 | 0,004 |
| 6 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,27 (0,69) | 0,0 (0,0) | 0; 3 | 0; 0 | 400,0 | 0,017 |
| 7 | 0,0 (Q1: 0,0; Q3: 1,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,47 (0,90) | 0,0 (0,0) | 0; 3 | 0; 0 | 352,0 | 0,002 |
| 8 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (0,0) | 0,0 (0,0) | 0; 0 | 0; 0 | 480,0 | 1 |
| 9 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,07 (0,37) | 0,0 (0,0) | 0; 2 | 0; 0 | 464,0 | 0,3 |
| 10 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,2 (0,76) | 0,0 (0,0) | 0; 3 | 0; 0 | 448,0 | 0,14 |
| 11 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,07 (0,36) | 0,0 (0,0) | 0; 2 | 0; 0 | 464,0 | 0,3 |
| 12 | 0,0 (Q1: 0,0; Q3: 0,0) | 0,0 (Q1: 0,0; Q3: 0,0) | 0,2 (0,48) | 0,0 (0,0) | 0; 2 | 0; 0 | 450,0 | 0,17 |
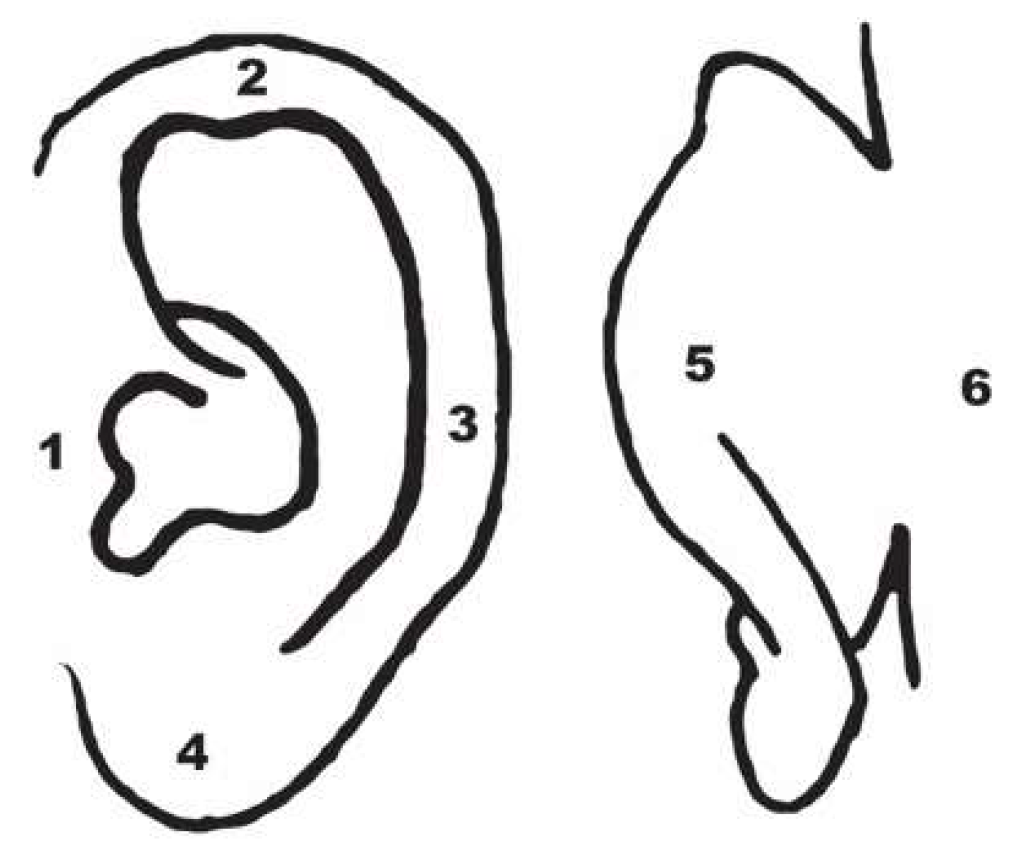
Tactile sensitivity testing of the auricle
Otomicroscopic examination
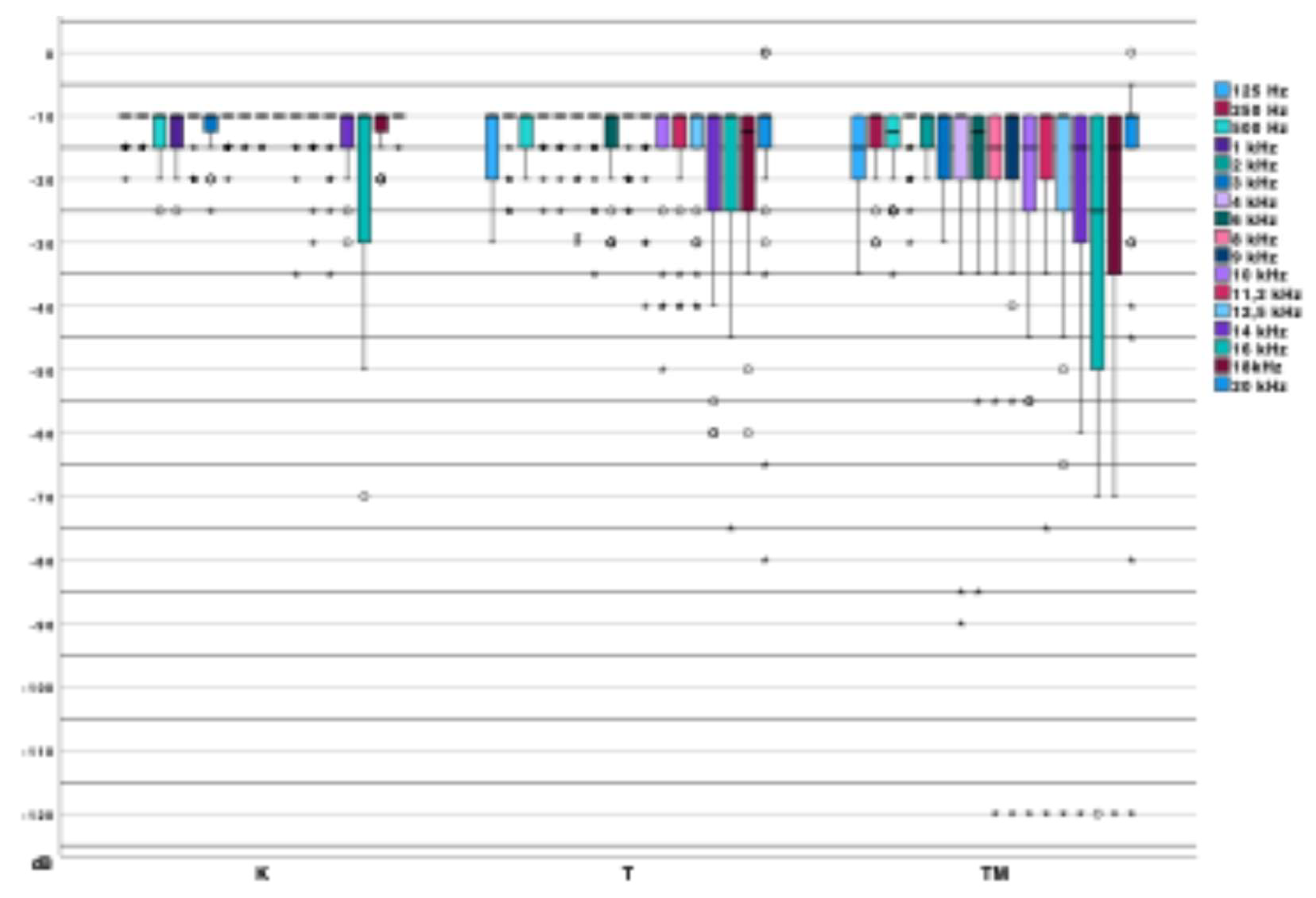
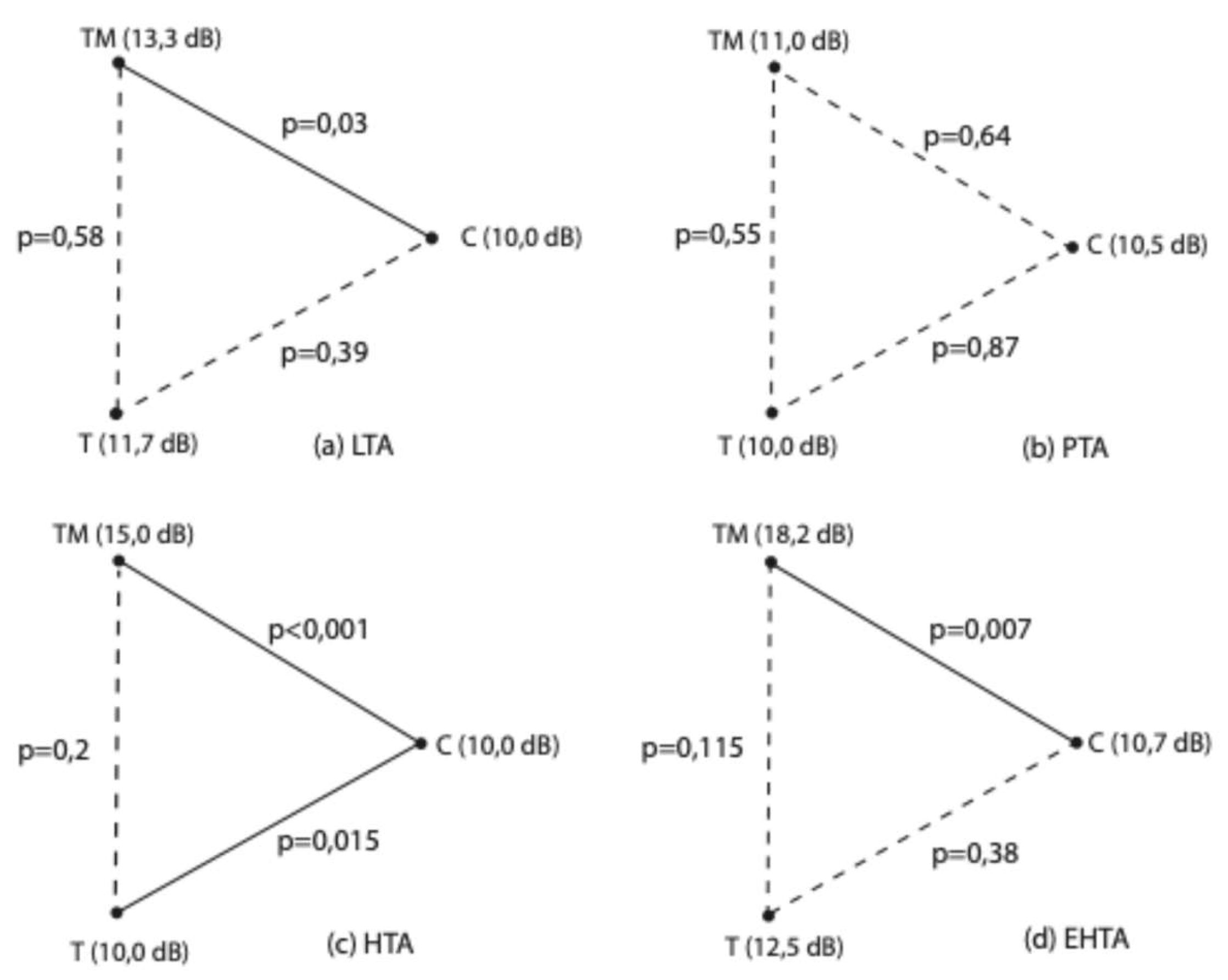
Extended high-frequency pure-tone audiometry
| C | T | TM | χ2 | p | ||
| LTA (dB) | Median (IQR) | 10,0 (Q1: 10,0; Q3: 11,66) |
11,66 (Q1: 10,0; Q3: 13,75) |
13,3 (Q1: 10,0; Q3: 18,33) |
8,06 | 0,018 |
| Min. | 10,0 | 10,0 | 10,0 | |||
| Max. | 16,67 | 25,0 | 31,7 | |||
| PTA (dB) | Median (IQR) | 10,5 (Q1: 10,0; Q3: 12,75) |
10 (Q1: 10,0; Q3: 12,25) |
11,0 (Q1: 10,0; Q3: 15,5) |
2,27 | 0,32 |
| Min. | 10,0 | 10,0 | 10,0 | |||
| Max. | 19,0 | 21,8 | 35,0 | |||
| HTA (dB) | Median (IQR) | 10 (Q1: 10,0; Q3: 10) |
10 ,0 (Q1: 10,0; Q3: 13,33) |
15,0 (Q1: 10,0; Q3: 19,17) |
21,7 | < 0,001 |
| Min. | 10,0 | 10,0 | 10,0 | |||
| Max. | 13,33 | 30,0 | 108,3 | |||
| EHTA (dB) | Median (IQR) | 10,71 (Q1: 10,0; Q3: 14,29) |
12,5 (Q1: 10,0; Q3: 19,82) |
18,2 (Q1: 10,0; Q3: 25,71) |
9,3 | 0,01 |
| Min. | 7,11 | 9,3 | 8,6 | |||
| Max. | 25,0 | 43,6 | 120 |
Middle ear impedance testing
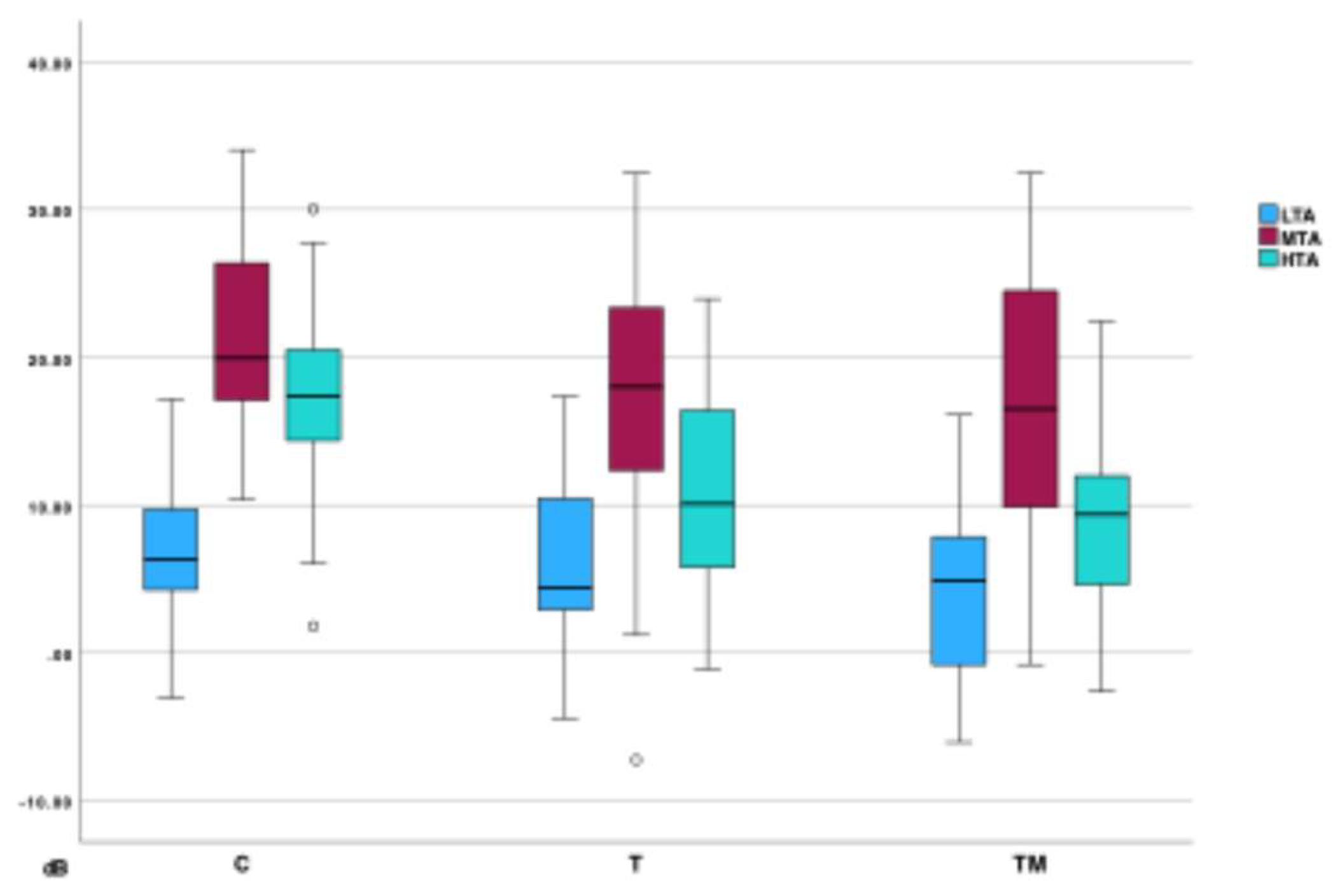
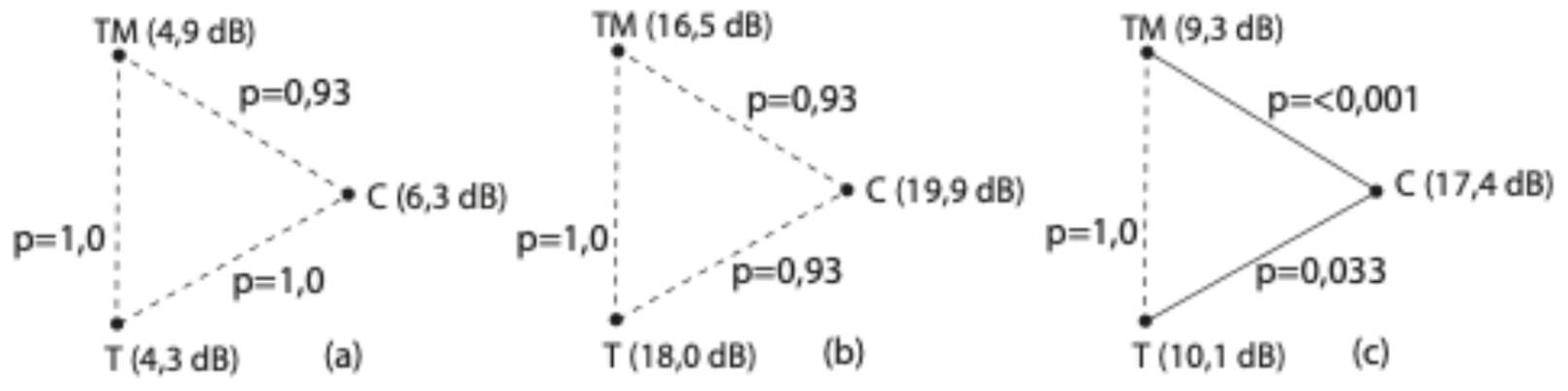
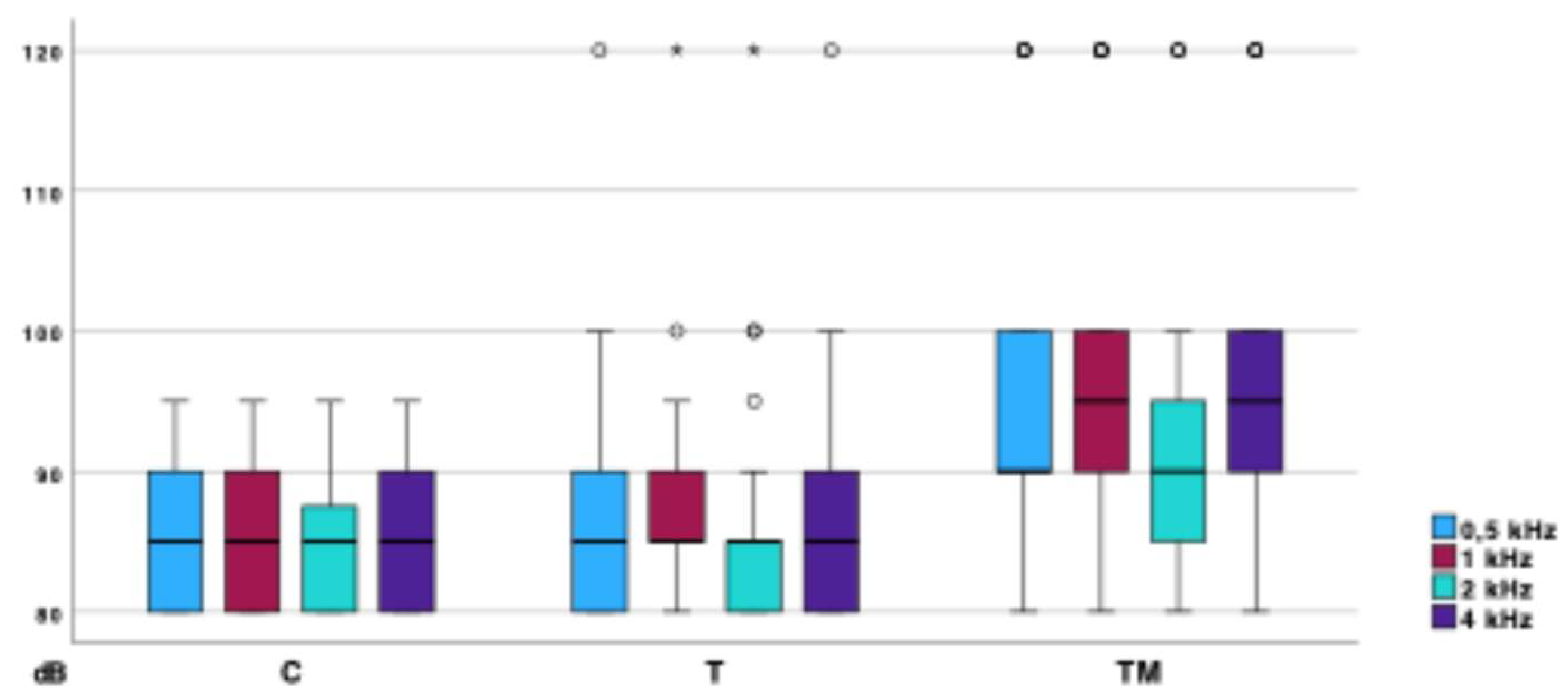
Distortion product otoacoustic emissions (DPOAE)
| Group C | Group T | Group TM | χ2 | p | ||
| LTA (dB) | Median (IQR) | 6,3 (Q1: 4,09; Q3: 9,76) |
4,38 (Q1: 2,8; Q3: 10,55) |
4,86 (Q1: -0,97; Q3: 8,35) |
0,76 | 0,68 |
| Min. | -3,05 | -4,45 | -6,05 | |||
| Max. | 17,15 | 17,35 | 16,10 | |||
| MTA (dB) | Median (IQR) | 19,93 (Q1: 10,38; Q3: 26,49) |
18,0 (Q1: 11,78; Q3: 23,61) |
16,51 (Q1: 9,83; Q3: 24,71) |
3,06 | 0,216 |
| Min. | 10,38 | -7,25 | -0,8 | |||
| Max. | 34,03 | 32,45 | 31,47 | |||
| HTA (dB) | Median (IQR) | 17,39 (Q1: 14,29; Q3: 20,58) |
10 ,08 (Q1: 5,48; Q3: 16,56) |
9,36 (Q1: 3,99; Q3: 12,24) |
20,23 | < 0,001 |
| Min. | 1,8 | -1,1 | -2,62 | |||
| Max. | 30,02 | 23,95 | 12,24 |
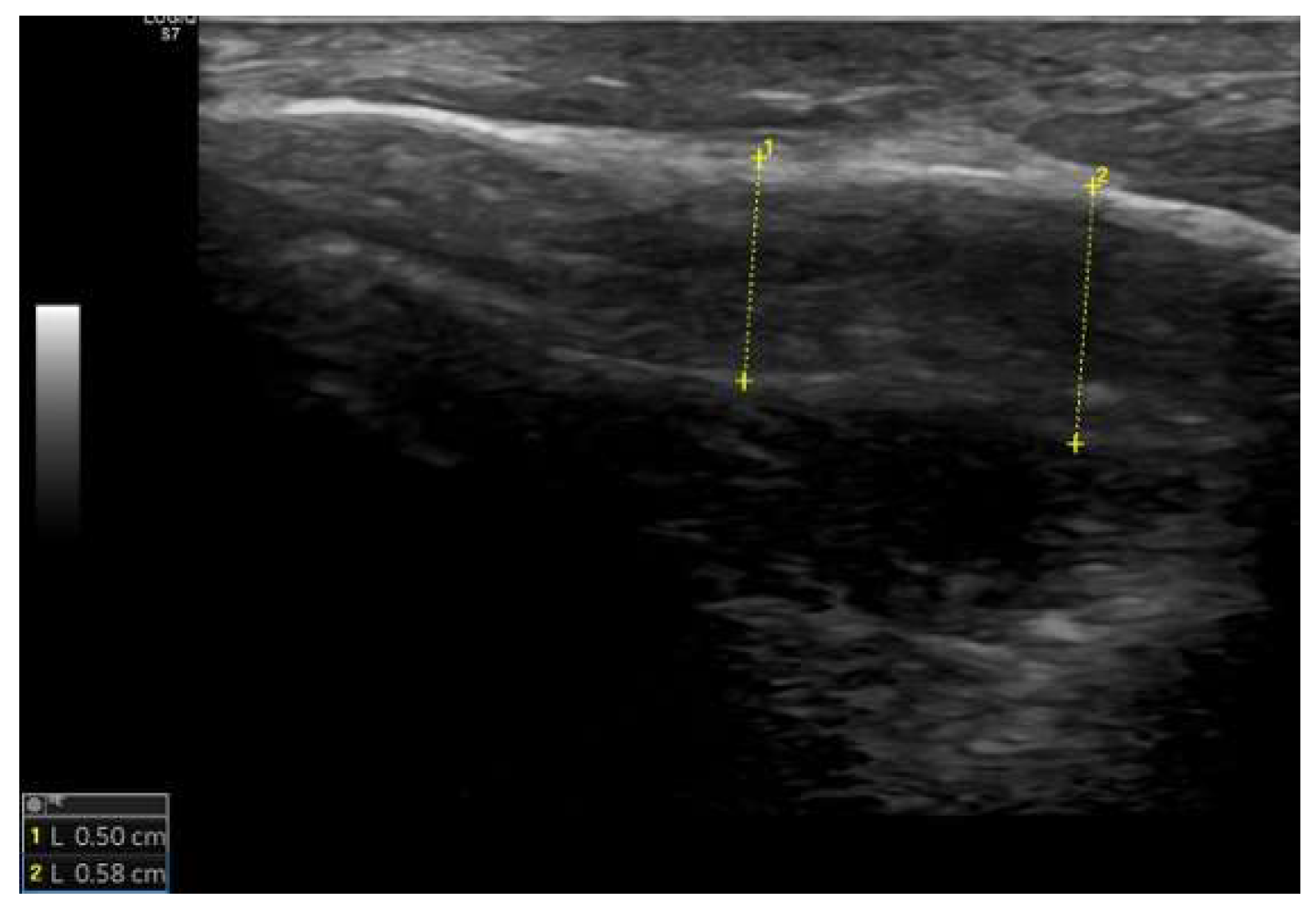
Ultrasound examination of the mastoid
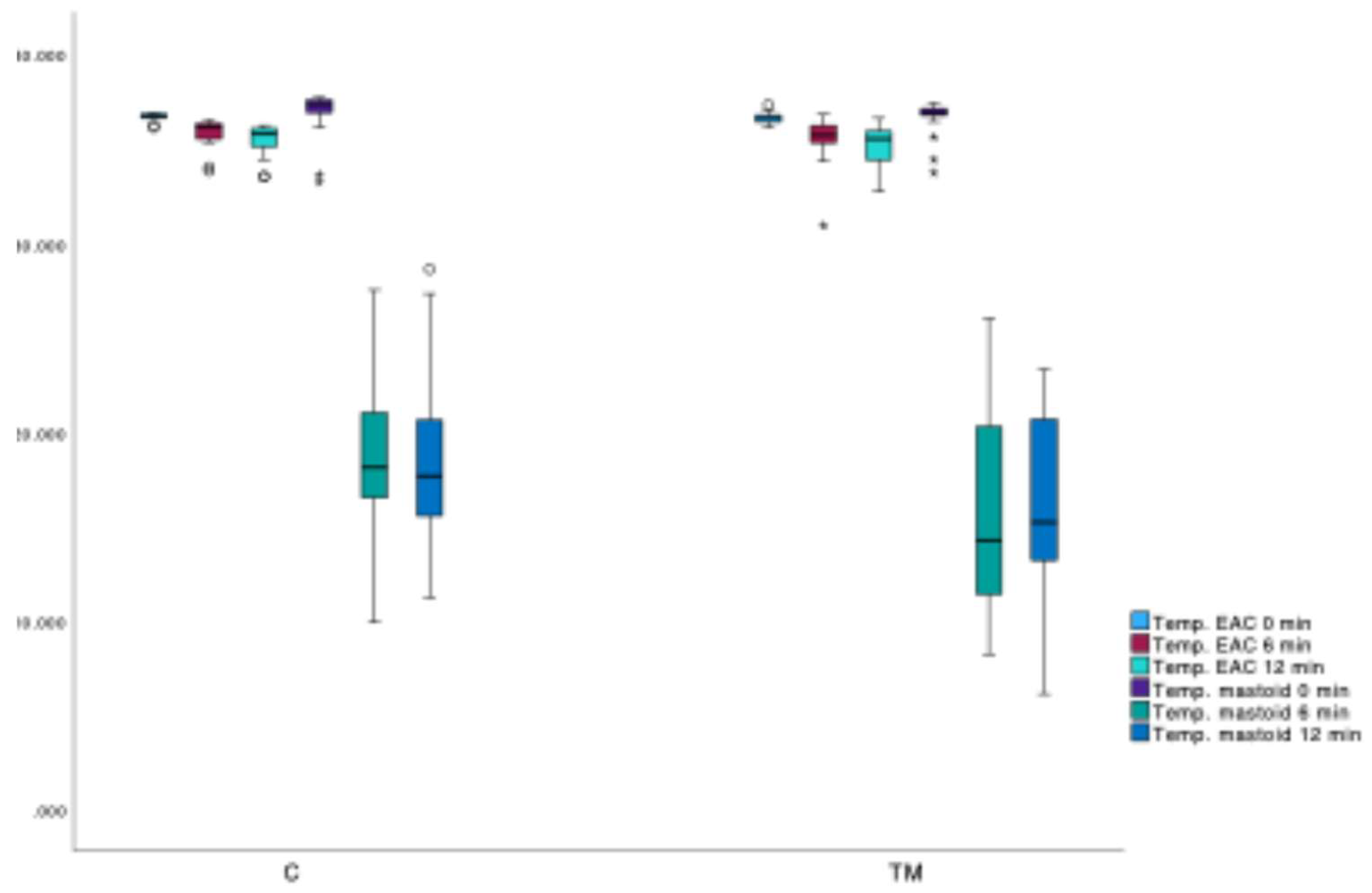
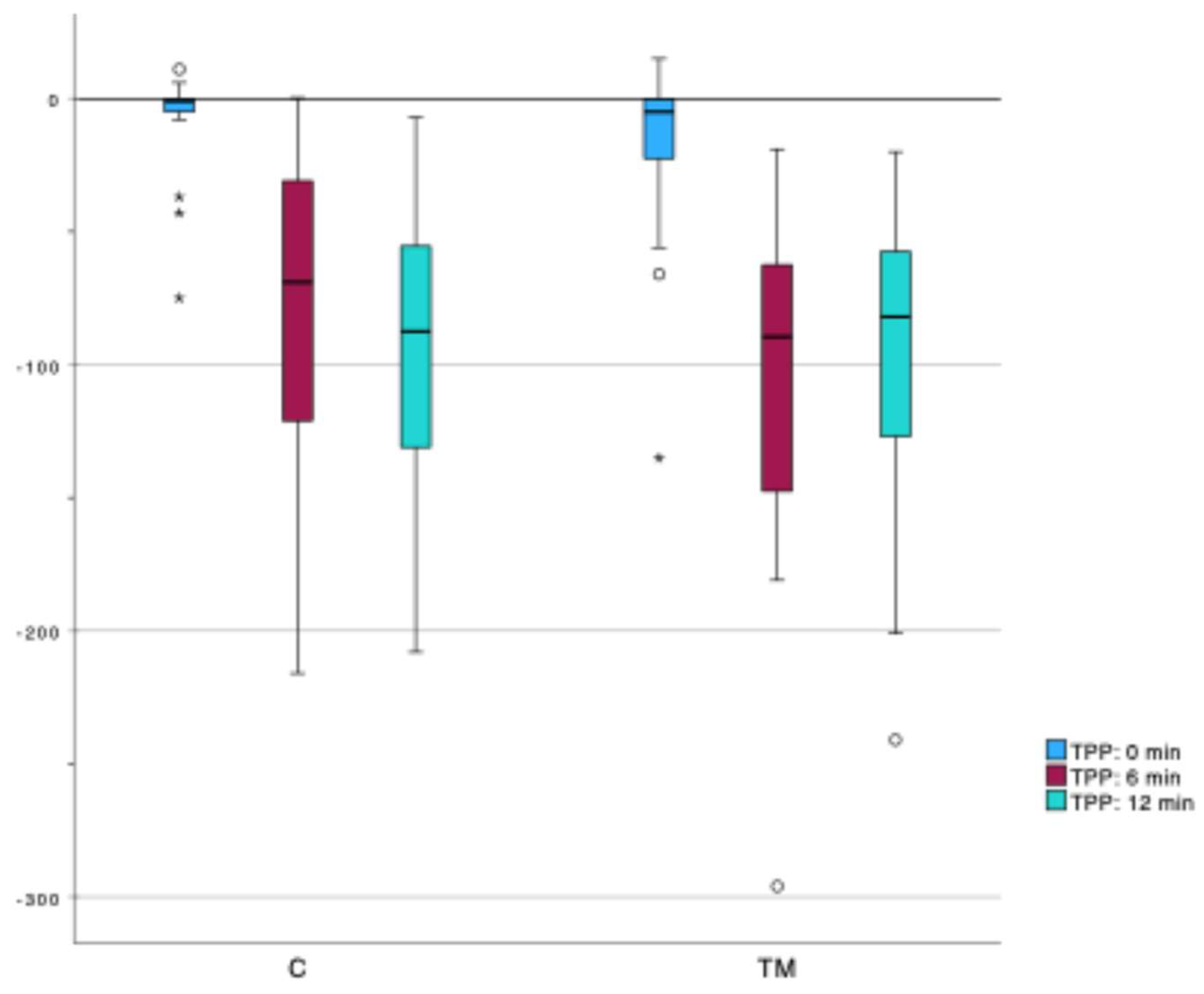
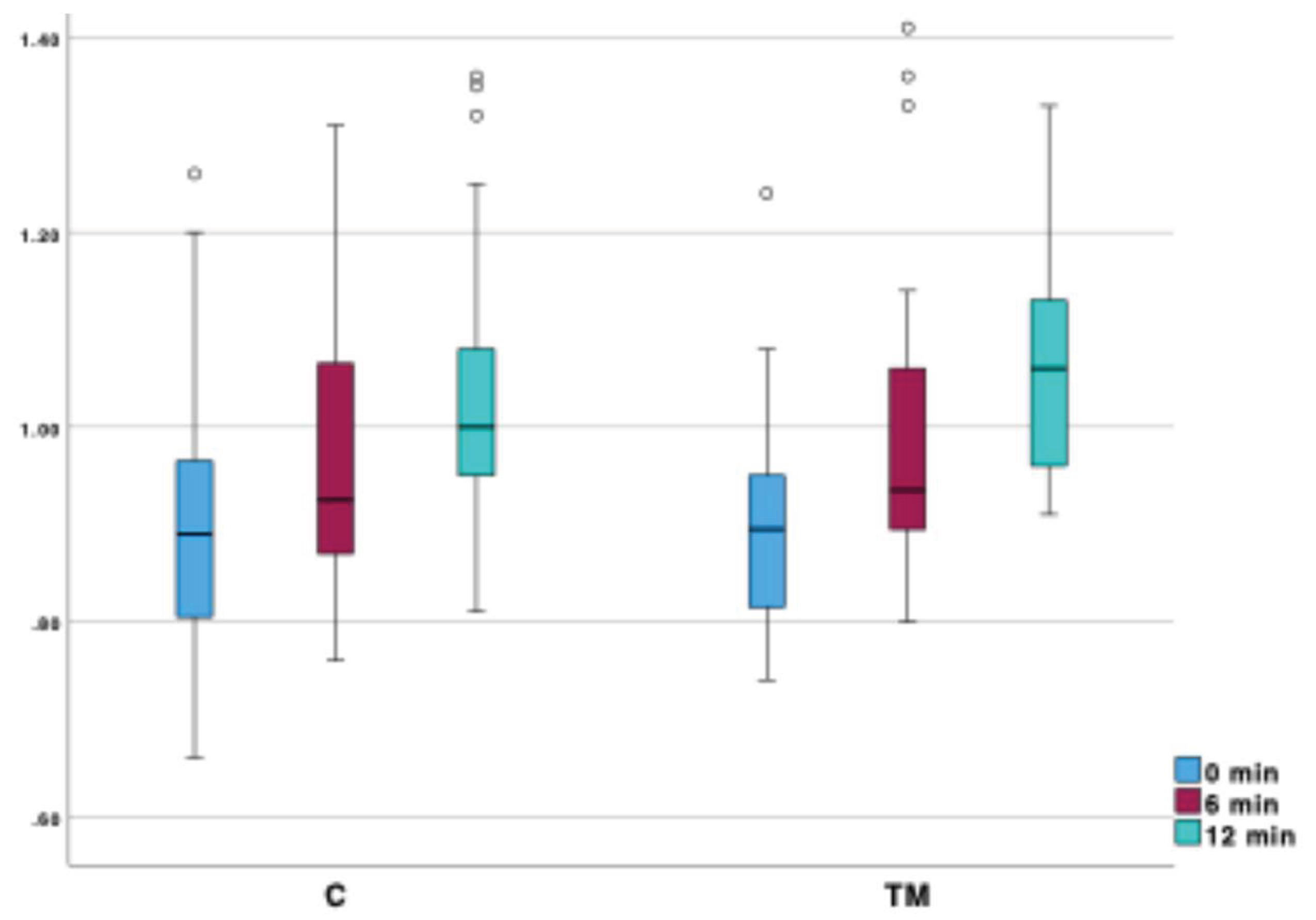
Mastoid function testing
| 0 min | 6 min | 12 min | |||||
| C | TM | C | TM | C | TM | ||
| TC (°C) | Median (IQR) | 36,7 (Q1: 36,6; Q3: 36,8) |
36,6 (Q1: 36,4; Q3: 36,7) |
36,1 (Q1: 35,5; Q3: 36,3) |
35,8 (Q1: 35,3; Q3: 36,2) |
35,75 (Q1: 35,1; Q3: 36,1) |
35,5 (Q1: 34,4; Q3: 35,9) |
| Min. | 36,1 | 36,1 | 36,1 | 35,3 | 33,5 | 32,7 | |
| Max. | 36,9 | 37,3 | 36,9 | 36,2 | 36,2 | 36,6 | |
| TM (°C) | Median (IQR) | 37,3 (Q1: 36,9; Q3: 37,6) |
36,9 (Q1: 36,8; Q3: 37,1) |
18,1 (Q1: 16,5; Q3: 21,3) |
14,8 (Q1: 11,9; Q3: 20,3) |
17,65 (Q1: 15,4; Q3: 20,9) |
15,2 (Q1: 13,2; Q3: 20,7) |
| Min. | 33,2 | 33,7 | 9,9 | 8,2 | 11,2 | 6,1 | |
| Max. | 37,7 | 37,4 | 27,5 | 26,0 | 28,6 | 23,3 | |
| VORg | Median (IQR) | 0,89 (Q1: 0,80; Q3: 0,96) |
0,88 (Q1: 0,54; Q3: 1,24) |
0,93 (Q1: 0,86; Q3: 1,06) |
0,93 (Q1: 0,90; Q3: 1,06) |
1,00 (Q1: 0,95; Q3: 1,08) |
1,06 (Q1: 0,95; Q3: 1,13) |
| Min. | 0,66 | 0,81 | 0,76 | 0,80 | 0,81 | 0,91 | |
| Max. | 1,26 | 0,95 | 1,31 | 1,41 | 1,36 | 1,33 | |
| TPP (daPa) | Median (IQR) | -1,0 (Q1: -5; Q3: 0) |
-5,0 (Q1: -23; Q3: 0) |
-69,0 (Q1: -124; Q3: -31) |
-89,5 (Q1: -65,3; Q3: -144,3) |
-87,5 (Q1: -133; Q3: -53,8) |
-82,0 (Q1: -130,5; Q3: -51,3) |
| Min. | -75 | -135 | -216 | -296 | -208 | -241 | |
| Max. | 11 | 15 | 0 | -19 | -7 | -20 | |
| Group C | Group TM | U | p | |
| TM 0 min (°C) | 37,3 (Q1: 36,9; Q3: 37,6) |
36,9 (Q1: 36,8; Q3: 37,1) | 260 | 0,002 |
| TM 6 min (°C) | 18,1 (Q1: 16,5; Q3: 21,3) |
14,8 (Q1: 11,9; Q3: 20,3) | 317,5 | 0,022 |
| TM 12 min (°C) | 17,65 (Q1: 15,4; Q3: 20,9) |
15,2 (Q1: 13,2; Q3: 20,7) | 302 | 0,030 |
| TC 0 min (°C) | 36,7 (Q1: 36,6; Q3: 36,8) |
36,6 (Q1: 36,4; Q3: 36,7) | 323 | 0,025 |
| TC 6 min (°C) | 36,1 (Q1: 35,5; Q3: 36,3) |
35,8 (Q1: 35,3; Q3: 36,2) | 395 | 0,230 |
| TC 12 min (°C) | 35,75 (Q1: 35,1; Q3: 36,1) |
35,5 (Q1: 34,4; Q3: 35,9) | 359,5 | 0,189 |
| Δ TM (0–6 min) (%) |
-106,6 (Q1: -126; Q3: -76) |
-146,2 (Q1: -212; Q3: -82) |
330 | 0,035 |
| Δ TM (6–12 min) (%) |
1,1 (Q1: -24,3; Q3: 10,4) |
2,9 (Q1: 14,2; Q3: -12,8) |
409,5 | 0,568 |
| Δ TM (0–12 min) (%) |
-103,6 (Q1: -141,7; Q3: -79,1) |
-141,6 (Q1: -176,4; Q3: -79,8) |
313 | 0,045 |
| Δ TC (0–6 min) (%) | -1,66 (Q1: -3,3; Q3: -1,37) |
-1,8 (Q1: -3,6; Q3: -1,1) |
462 | 0,8 |
| Δ TC (6–12 min) (%) | -1,11 (Q1: -1,42; Q3: -0,83) |
-1,13 (Q1: -0,13; Q3: -1,9) |
436 | 0,859 |
| Δ TC (0–12 min) (%) | -2,78 (Q1: -4,7; Q3: -2,01) |
-2,7 (Q1: -5,5; Q3: -2,2) |
423 | 0,711 |
| VORg (0 min) | 0,89 (Q1: 0,80; Q3: 0,96) |
0,88 (Q1: 0,54; Q3: 1,24) |
450,5 | 0,677 |
| VORg (6 min) | 0,93 (Q1: 0,86; Q3: 1,06) |
0,93 (Q1: 0,90; Q3: 1,06) |
453 | 0,703 |
| VORg (12 min) | 1,00 (Q1: 0,95; Q3: 1,08) |
1,06 (Q1: 0,95; Q3: 1,13) |
377 | 0,292 |
| TPP (0 min) (daPa) | -1,0 (Q1: -5; Q3: 0) |
-5,0 (Q1: -23; Q3: 0) |
342,5 | 0,051 |
| TPP (6 min) (daPa) | -69,0 (Q1: -124; Q3: -31) |
-89,5 (Q1: -65,3; Q3: -144,3) |
357 | 0,083 |
| TPP (12 min) (daPa) | -87,5 (Q1: -133; Q3: -53,8) |
-82,0 (Q1: -130,5; Q3: -51,3) |
442 | 0,929 |
| Δ VORg (0–6 min) | 0,06 (Q1: 0,032; Q3: 0,08) |
0,085 (Q1: 0,03; Q3: 0,12) |
378 | 0,152 |
| Δ VORg (6–12 min) | 0,045 (Q1: 0,023; Q3: 0,11) |
0,055 (Q1: 0,22; Q3: 0,11) |
386 | 0,357 |
| Δ VORg (0–12 min) | 0,10 (Q1: 0,09; Q3: 0,013) |
0,14 (Q1: 0,10; Q3: 0,18) |
304 | 0,033 |
| Δ TPP (0–6 min) (daPa) | -66,5 (Q1: -113,5; Q3: -27,8) |
-72,5 (Q1: -127,8; Q3: -50) |
403,5 | 0,281 |
| Δ TPP (6–12 min) (daPa) | -21 (Q1: -33; Q3: -22,8) |
-4 (Q1: -35; Q3: 45,3) |
339,5 | 0,108 |
| Δ TPP (0–12min) (daPa) | -87 (Q1: -121; Q3: -51,5) |
-71,5 (Q1: -101,8; Q3: -39,3) |
388,5 | 0,378 |
Discussion
Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AM | Acute mastoiditis |
| AOM | Acute otitis media |
| COMQ-12 | Chronic Otitis Media Questionnaire 12 |
| daPa | Deka pascal |
| DPOAE | Distortion-Product Otoacoustic Emissions |
| K | Kelvin |
| m | Meter |
| TPP | tympanometric peak pressure |
| VORg | vestibulo-ocular reflex gain |
| vHIT | video head impulse test |
| W | Watt |
References
- Luntz, M.; Brodsky, A.; Nusem, S.; Kronenberg, J.; Keren, G.; Migirov, L.; et al. Acute mastoiditis--the antibiotic era: a multicenter study. International journal of pediatric otorhinolaryngology. 2001, 57, 1–9. [Google Scholar] [CrossRef]
- Zanetti, D.; Nassif, N. Indications for surgery in acute mastoiditis and their complications in children. International Journal of Pediatric Otorhinolaryngology. 2006, 70, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Kværner, K.J.; Bentdal, Y.; Karevold, G. Acute mastoiditis in Norway: No evidence for an increase. International Journal of Pediatric Otorhinolaryngology. 2007, 71, 1579–1583. [Google Scholar] [CrossRef] [PubMed]
- Psarommatis, I.M.; Voudouris, C.; Douros, K.; Giannakopoulos, P.; Bairamis, T.; Carabinos, C. Algorithmic management of pediatric acute mastoiditis. International Journal of Pediatric Otorhinolaryngology. 2012, 76, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Pang, L.H.Y.; Barakate, M.S.; Havas, T.E. Mastoiditis in a paediatric population: A review of 11 years experience in management. International Journal of Pediatric Otorhinolaryngology. 2009, 73, 1520–1524. [Google Scholar] [CrossRef]
- Lin, H.W.; Shargorodsky, J.; Gopen, Q. Clinical Strategies for the Management of Acute Mastoiditis in the Pediatric Population. Clinical Pediatrics. 2010, 49, 110–115. [Google Scholar] [CrossRef]
- Hullegie, S.; Venekamp, R.P.; Van Dongen, T.M.A.; Hay, A.D.; Moore, M.V.; Little, P.; et al. Prevalence and Antimicrobial Resistance of Bacteria in Children with Acute Otitis Media and Ear Discharge: A Systematic Review. Pediatric Infectious Disease Journal. 2021, 40, 756–762. [Google Scholar] [CrossRef]
- Geva, A.; Oestreicher-Kedem, Y.; Fishman, G.; Landsberg, R.; DeRowe, A. Conservative management of acute mastoiditis in children. International journal of pediatric otorhinolaryngology. 2008, 72, 629–634. [Google Scholar] [CrossRef]
- Chesney, J.; Black, A.; Choo, D. What is the best practice for acute mastoiditis in children? The Laryngoscope. 2014, 124, 1057–1058. [Google Scholar] [CrossRef]
- Bakhos, D.; Trijolet, J.-P.; Morinière, S.; Pondaven, S.; Al zahrani, M.; Lescanne, E. Conservative Management of Acute Mastoiditis in Children. Archives of Otolaryngology–Head & Neck Surgery. 2011, 137, 346. [Google Scholar] [CrossRef]
- Psarommatis, I.; Giannakopoulos, P.; Theodorou, E.; Voudouris, C.; Carabinos, C.; Tsakanikos, M. Mastoid subperiosteal abscess in children: drainage or mastoidectomy? The Journal of Laryngology & Otology. 2012, 126, 1204–1208. [Google Scholar] [CrossRef]
- Andersen, S.A.W.; Mikkelsen, P.T.; Konge, L.; Cayé-Thomasen, P.; Sørensen, M.S. Cognitive load in distributed and massed practice in virtual reality mastoidectomy simulation. The Laryngoscope. 2016, 126, E74-9. [Google Scholar] [CrossRef] [PubMed]
- Attlmayr, B.; Zaman, S.; Scott, J.; Derbyshire, S.G.; Clarke, R.W.; De, S. Paediatric acute mastoiditis, then and now: Is it more of a problem now? Journal of Laryngology and Otology. 2015, 129, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Glynn, F.; Osman, L.; Colreavy, M.; Rowley, H.; Dwyer, T.P.O.; Blayney, A. Acute mastoiditis in children: presentation and long term consequences. The Journal of Laryngology & Otology. 2008, 122, 233–237. [Google Scholar] [CrossRef]
- Guillén-Lozada, E.; Bartolomé-Benito, M.; Moreno-Juara, Á. Surgical management of mastoiditis with intratemporal and intracranial complications in children. Outcome, complications, and predictive factors. International journal of pediatric otorhinolaryngology [Internet]. 2023 [cited 2024 Apr 2]. Available from: https://pubmed.ncbi.nlm.nih.gov/37352591/.
- Harley, E.H.; Sdralis, T.; Berkowitz, R.G. Acute mastoiditis in children: a 12-year retrospective study. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1997, 116, 26–30. [Google Scholar] [CrossRef]
- Petersen, C.G.; Ovesen, T.; Pedersen, C.B. Acute mastoidectomy in a Danish county from 1977 to 1997--operative findings and long-term results. Acta oto-laryngologica Supplementum. 2000, 543, 122–126. [Google Scholar] [CrossRef]
- Enoksson, F.; Groth, A.; Hultcrantz, M.; Stalfors, J.; Stenfeldt, K.; Hermansson, A. Subperiosteal abscesses in acute mastoiditis in 115 Swedish children. International Journal of Pediatric Otorhinolaryngology. 2015, 79. [Google Scholar] [CrossRef]
- Tos, M.; Poulsen, G. Attic Retractions Following Secretory Otitis. Acta Oto-Laryngologica. 1980, 89, 479–486. [Google Scholar] [CrossRef]
- Sade, J.; Berco, E. Atelectasis and Secretory Otitis Media. 1976, 85, 66–72. [CrossRef]
- Kang, H.S.; Ahn, S.K.; Jeon, S.Y.; Hur, D.G.; Kim, J.P.; Park, J.J.; et al. Sensation recovery of auricle following chronic ear surgery by retroauricular incision. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2012, 269, 101–106. [Google Scholar] [CrossRef]
- Phillips, J.S.; Haggard, M.; Yung, M. A new health-related quality of life measure for active chronic otitis media (COMQ-12): Development and initial validation. Otology and Neurotology. 2014, 35, 454–458. [Google Scholar] [CrossRef]
- Vozel, D.; Steiner, N.; Božanić Urbančič, N.; Mladenov, D.; Battelino, S. Slovenian Cross-Cultural Adaptation and Validation of Health-Related Quality of Life Measures for Chronic Otitis Media (COMQ-12), Vertigo (DHI, NVI) and TINNITUS (THI). Zdravstveno varstvo. 2020, 59, 120–127. [Google Scholar] [CrossRef]
- Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. AmericanAcademy of Otolaryngology-Head and Neck Surgery Ffoundation, Inc. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1995, 113, 186–187. [CrossRef]
- Magnuson, B. Functions of the mastoid cell system: auto-regulation of temperature and gas pressure. The Journal of Laryngology & Otology. 2003, 117, 99–103. [Google Scholar] [CrossRef]
- Fooken Jensen, P.V.; Gaihede, M. Congestion of mastoid mucosa and influence on middle ear pressure - Effect of retroauricular injection of adrenaline. Hearing research. 2016, 340, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Cros, O.; Borga, M.; Pauwels, E.; Dirckx, J.J.J.; Gaihede, M. Micro-channels in the mastoid anatomy. Indications of a separate blood supply of the air cell system mucosa by micro-CT scanning. Hearing research. 2013, 301, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Kadir, A.; Hayashi, N.; Takamoto, M. Direct influence of temperature on the semicircular canal receptor. Journal of vestibular research : equilibrium & orientation. 1998, 8, 169–173. [Google Scholar]
- Smolders, J.W.T.; Klinke, R. Effects of temperature on the properties of primary auditory fibres of the spectacled caiman,Caiman crocodilus (L.). Journal of Comparative Physiology A. 1984, 155, 19–30. [Google Scholar] [CrossRef]
- Whitehead, M.L.; Wilson, J.P.; Baker, R.J. The Effects of Temperature on Otoacoustic Emission Tuning Properties. Auditory Frequency Selectivity [Internet]. Boston, MA: Springer US; 1986 [cited 2021 Sept 20]. p. 39. Available from: http://link.springer.com/10.1007/978-1-4613-2247-4_5.
- Ferber-Viart, C.; Savourey, G.; Garcia, C.; Duclaux, R.; Bittel, J.; Collet, J. Influence of hyperthermia on cochlear micromechanical properties in humans. Hearing research. 1995, 91, 202–207. [Google Scholar] [CrossRef]
- Zenner, H.P.; Zimmermann, U. Caloric evoked motile responses of mammalian vestibular sensory cells. Acta oto-laryngologica. 1995, 115, 484–487. [Google Scholar] [CrossRef]
- Ohtani, M.; Yamashita, T.; Amano, H.; Kubo, N.; Kumazawa, T. Thermal influence on intracellular calcium concentration in vestibular hair cells isolated from the guinea pig. A preliminary report. Acta oto-laryngologica Supplementum. 1993, 500, 46–49. [Google Scholar] [CrossRef]
- Hood, J.D. Evidence of direct thermal action upon the vestibular receptors in the caloric test. A re-interpretation of the data of Coats and Smith. Acta Otolaryngol. 1989, 107, 161–165. [Google Scholar] [CrossRef]
- Feldmann, A.; Wili, P.; Maquer, G.; Zysset, P. The thermal conductivity of cortical and cancellous bone. European cells & materials. 2018, 35, 25–33. [Google Scholar] [CrossRef]
- Xu, F.; Lu, T.J.; Seffen, K.A.; Ng, E.Y.K. Mathematical modeling of skin bioheat transfer. Applied Mechanics Reviews. 2009, 62, 1–35. [Google Scholar] [CrossRef]
- Rojas-Altamirano, G.; Vargas, R.O.; Escandón, J.P.; Mil-Martínez, R.; Rojas-Montero, A. Calculation of Effective Thermal Conductivity for Human Skin Using the Fractal Monte Carlo Method. Micromachines [Internet]. 2022 [cited 2024 Sept 17];Available from: /pmc/articles/PMC8953946/. [CrossRef] [PubMed Central]
- Ni, Y.; Sha, Y.; Dai, P.; Li, H. Quantitative morphology of facial nerve based on three-dimensional reconstruction of temporal bone. Otolaryngology–Head and Neck Surgery. 2008, 138, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Merati, M.; Kazemi, M.A.; Dabiri, S.; Kouhi, A. Radiologic evaluation of the mastoid segment of the facial nerve tract in the intact temporal bone. Surg Radiol Anat. 2021, 43, 145–151. [Google Scholar] [CrossRef]
- Mahboubi, H.; Wu, E.C.; Jahanbakhshi, R.; Coale, K.; Rothholtz, V.S.; Zardouz, S.; et al. A novel method to determine standardized anatomic dimensions of the osseous external auditory canal. Otol Neurotol. 2012, 33, 715–720. [Google Scholar] [CrossRef]
- Palva, T.; Virtanen, H.; Mäkinen, J. Acute and latent mastoiditis in children. J Laryngol Otol. 1985, 99, 127–136. [Google Scholar] [CrossRef]
- Van Zuijlen, D.A.; Schilder, A.G.M.; Van Balen, F.A.M.; Hoes, A.W. National differences in incidence of acute mastoiditis: relationship to prescribing patterns of antibiotics for acute otitis media? The Pediatric infectious disease journal. 2001, 20, 140–144. [Google Scholar] [CrossRef]
- Bento, R.F.; Fonseca ACde, O. A brief history of mastoidectomy. International archives of otorhinolaryngology. 2013, 17, 168–178. [Google Scholar] [CrossRef]
- Bartov, N.; Lahav, Y.; Lahav, G.; Zloczower, E.; Katzenell, U.; Halperin, D.; et al. Management of Acute Mastoiditis With Immediate Needle Aspiration for Subperiosteal Abscess. Otology & Neurotology. 2019, 40, e612-8. [Google Scholar] [CrossRef]
- Spratley, J.; Silveira, H.; Alvarez, I.; Pais-Clemente, M. Acute mastoiditis in children: review of the current status. International journal of pediatric otorhinolaryngology. 2000, 56, 33–40. [Google Scholar] [CrossRef]
- Cohen-Kerem, R.; Uri, N.; Rennert, H.; Peled, N.; Greenberg, E.; Efrat, M. Acute mastoiditis in children: is surgical treatment necessary? The Journal of laryngology and otology. 1999, 113, 1081–1085. [Google Scholar] [CrossRef]
- Palva, T.; Ramsay, H. Incudal Folds and Epitympanic Aeration. Otology & Neurotology [Internet]. 1996. Available from: https://journals.lww.com/otology-neurotology/fulltext/1996/09000/incudal_folds_and_epitympanic_aeration.4.aspx.
- Groth, A.; Enoksson, F.; Hultcrantz, M.; Stalfors, J.; Stenfeldt, K.; Hermansson, A. Acute mastoiditis in children aged 0-16 years--a national study of 678 cases in Sweden comparing different age groups. International journal of pediatric otorhinolaryngology. 2012, 76, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Woo, J.H.; Cho, S.; Oh, H.W.; Joo, H.; Baik, H.J. Risk Factors for Perioperative Respiratory Adverse Events in Children with Recent Upper Respiratory Tract Infection: A Single-Center-Based Retrospective Study. Therapeutics and Clinical Risk Management. 2020, 16, 1227. [Google Scholar] [CrossRef] [PubMed]
- Groth, A.; Enoksson, F.; Stalfors, J.; Stenfeldt, K.; Hultcrantz, M.; Hermansson, A. Recurrent acute mastoiditis – a retrospective national study in Sweden. Acta Oto-Laryngologica. 2012, 132, 1275–1281. [Google Scholar] [CrossRef] [PubMed]
- Schwam, Z.G.; Michaelides, E.; Kuo, P.; Hajek, M.A.; Judson, B.L.; Schutt, C. Thirty-day morbidity and mortality following otologic/neurotologic surgery: Analysis of the national surgical quality improvement program. Laryngoscope. 2018, 128, 1431–1437. [Google Scholar] [CrossRef]
- Prinsley, P. An audit of “dead ear” after ear surgery. J Laryngol Otol. 2013, 127, 1177–1183. [Google Scholar] [CrossRef]
- Tait, A.R.; Malviya, S.; Voepel-Lewis, T.; Munro, H.M.; Seiwert, M.; Pandit, U.A. Risk factors for perioperative adverse respiratory events in children with upper respiratory tract infections. Anesthesiology. 2001, 95, 299–306. [Google Scholar] [CrossRef]
- Michel, F.; Vacher, T.; Julien-Marsollier, F.; Dadure, C.; Aubineau, J.-V.; Lejus, C.; et al. Peri-operative respiratory adverse events in children with upper respiratory tract infections allowed to proceed with anaesthesia: A French national cohort study. Eur J Anaesthesiol. 2018, 35, 919–928. [Google Scholar] [CrossRef]
- Yin, X.; Strömberg, A.-K.; Duan, M. Evaluation of the noise generated by otological electrical drills and suction during cadaver surgery. Acta Otolaryngol. 2011, 131, 1132–1135. [Google Scholar] [CrossRef]
- Michaelides, E.M.; Kartush, J.M. Implications of sound levels generated by otologic devices. Otolaryngol Head Neck Surg. 2001, 125, 361–363. [Google Scholar] [CrossRef]
- Maccà, I.; Scapellato, M.L.; Carrieri, M.; Maso, S.; Trevisan, A.; Bartolucci, G.B. High-frequency hearing thresholds: effects of age, occupational ultrasound and noise exposure. Int Arch Occup Environ Health. 2015, 88, 197–211. [Google Scholar] [CrossRef]
- Stenfelt, S.; Goode, R.L. Transmission properties of bone conducted sound: measurements in cadaver heads. J Acoust Soc Am. 2005, 118, 2373–2391. [Google Scholar] [CrossRef]
- Abtahi, S.H.; Fazel, A.; Rogha, M.; Nilforoush, M.; Solooki, R. Effect of drill-induced noise on hearing in non-operated ear. Adv Biomed Res. 2016, 5, 87. [Google Scholar] [CrossRef] [PubMed]
- Frampton, S.J.; Pringle, M. Cutaneous sensory deficit following post-auricular incision. The Journal of Laryngology & Otology. 2011, 125, 1014–1019. [Google Scholar] [CrossRef]
- Vakharia, S.D.; Gupta, S.R. Sensation Loss of Auricle Following Ear Surgery by Post-auricular Incision: Our Experience. Indian Journal of Otolaryngology and Head & Neck Surgery. 2022, 74, 120. [Google Scholar] [CrossRef]
- Zloczower, E.; Tsur, N.; Hershkovich, S.; Fink, N.; Marom, T. Efficacy of Oral Steroids for Acute Acoustic Trauma. Audiol Neurootol. 2022, 27, 312–320. [Google Scholar] [CrossRef]
- Cayé-Thomasen, P.; Hermansson, A.; Tos, M.; Prellner, K. Bone modeling dynamics in acute otitis media. The Laryngoscope. 1999, 109, 723–729. [Google Scholar] [CrossRef]
- Swarts, J.D.; Cullen Doyle, B.M.; Alper, C.M.; Doyle, W.J. Surface area-volume relationships for the mastoid air cell system and tympanum in adult humans: Implications for mastoid function. Acta oto-laryngologica. 2010, 130, 1230–1236. [Google Scholar] [CrossRef]
- Gaihede, M. Middle ear volume and pressure effects on tympanometric middle ear pressure determination: model experiments with special reference to secretory otitis media. Auris Nasus Larynx. 2000, 27, 231–239. [Google Scholar] [CrossRef]
- Cros, O.; Knutsson, H.; Andersson, M.; Pawels, E.; Borga, M.; Gaihede, M. Determination of the mastoid surface area and volume based on micro-CT scanning of human temporal bones. Geometrical parameters depend on scanning resolutions. Hearing Research. 2016, 340. [Google Scholar] [CrossRef]
- Lima, M.A.R.; Farage, L.; Cury, M.C.L.; Júnior, F.B. Mastoid surface area-to-volume ratios in adult brazilian individuals. Braz J Otorhinolaryngol. 2013, 79, 446–453. [Google Scholar] [CrossRef]
- Kwon, O.J.; Sung, J.M.; Jung, H.K.; Kim, C.W. Postoperative Mastoid Aeration Following Canal Wall Up Mastoidectomy according to Preoperative Middle Ear Disease: Analysis of Temporal Bone Computed Tomography Scans. J Audiol Otol. 2017, 21, 140–145. [Google Scholar] [CrossRef]
- Kaneko, K.; Kanemaru, S.; Kanai, R.; Atsushi, Y. Regeneration of Mastoid Air Cells in Vivo Using Autologous Cortical Bone. Surgical Science. 2012, 2012, 514–517. [Google Scholar] [CrossRef]
| Median (IQR) | Mean (st. dev.) | |||||||
| TM | T | C | TM | T | C | χ2 | p | |
| Atrophy | 0,0 (Q1: 0,0; Q3: 1,0) | 0,0 (Q1: 0,0; Q3: 1,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,6 (0,68) | 0,4 (0,56) | 0,0 (0,0) | 19,06 | < 0,001 |
| Thickening and scarring | 0,0 (Q1: 0,0; Q3: 1,0) |
0,0 (Q1: 0,0; Q3: 1,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,27 (0,69) | 0,27 (0,69) | 0,0 (0,0) | 5,98 | 0,5 |
| Myringosclerosis | 0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,63 (0,89) |
0,63 (0,89) |
0,0 (0,0) | 17,32 | < 0,001 |
| Myringitis | 0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,03 (0,18) | 0,03 (0,18) | 0,0 (0,0) | 1,09 | 0,58 |
| Retraction (Toš) | 0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,43 (0,68) | 0,3 (0,54) | 0,0 (0,0) | 12,36 | 0,002 |
| Retraction (Sadé) | 0,0 (Q1: 0,0; Q3: 1,0) |
0,0 (Q1: 0,0; Q3: 1,0) |
0,0 (Q1: 0,0; Q3: 0,0) |
0,1 (0,4) | 0,1 (0,4) | 0,0 (0,0) | 2,18 | 0,336 |
| Group C | Group TM | U | p | ||
| Skin thickness (mm) | Median (IQR) | 3,73 (Q1: 3,6; Q3: 3,93) |
3,7 (Q1: 3,59; Q3: 3,89) |
477,0 | 0,929 |
| Min. | 3,0 | 3,3 | |||
| Max. | 4,7 | 4,3 | |||
| Cortical bone thickness (mm) | Median (IQR) | 5,71 (Q1: 5,2; Q3: 6,36) |
5,77 (Q1: 5,2; Q3: 6,42) |
444,0 | 0,976 |
| Min. | 4,13 | 1,93 | |||
| Max. | 7,97 | 7,97 | |||
| Min. | 1,8 | -2,62 | |||
| Max. | 30,02 | 12,24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





