1. Introduction
Gastrointestinal endoscopic procedures are an indispensable part of modern gastroenterology practice. In addition to conventional endoscopic procedures such as esophagogastroduodenoscopy (EGD) and colonoscopy, advanced endoscopic techniques including endoscopic retrograde cholangiopancreatography (ERCP), endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), and peroral endoscopic myotomy (POEM) are also frequently performed in gastroenterology practice. However, the high volume of these procedures places gastroenterologists under significant physical stress. In particular, repetitive overuse during procedures such as colonoscopy, EGD, and ERCP , awkward posture, prolonged standing can lead to various musculoskeletal disorders.
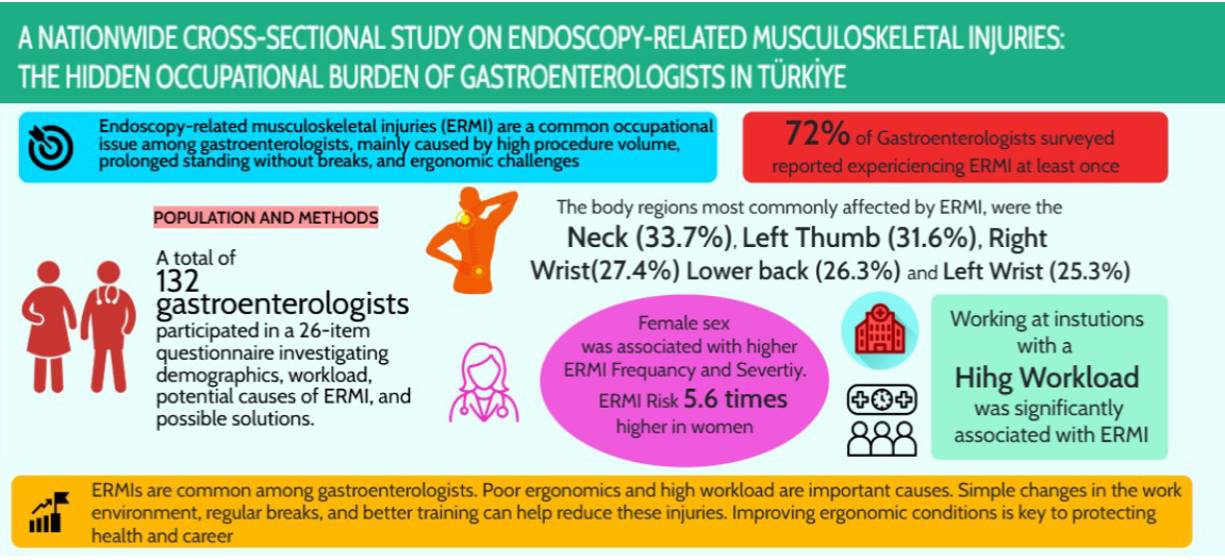
The prevalence of endoscopy-related musculoskeletal injuries (ERMI) among gastroenterologists has been reported to range between 37% to 89%[
1,
2]. Underlying causes of these injuries include increased procedure volume, prolonged procedure durations, the ergonomic design of endoscopic equipment, and modifiable environmental factors in the endoscopy unit such as monitor and bed height [
3].
Although various studies have been conducted on this subject in countries such as the United States[
3,
4,
5,
6,
7], Korea[
8], Japann[
9,
10] , Germany [
11] and Portugal [
12]; but systematic data on this subject are limited in Turkey. According to data from Türkiye in 2022, approximately 1.5 million upper gastrointestinal endoscopies and 850,000 lower gastrointestinal endoscopies were performed [
13].
The prevalence, risk factors, and occupational impact of ERMI among gastroenterologists have not been adequately investigated. This study aims to determine the prevalence of ERMI among gastroenterologists in Türkiye, to identify associated risk factors, and to evaluate their impact on professional practice.
2. Materials and Methods
2.1. Survey Administration
This cross-sectional survey study was conducted to evaluate the prevalence and characteristics of ERMI among gastroenterologists performing endoscopic procedures. The survey study was conducted from March to June 2025. The electronic survey was sent to 1,100 Turkish Gastroenterology Association (TGA) physician members and to 253 gastroenterology fellows still in training. At least 6 months of endoscopy practice was required for participation. The survey was sent to TGA members via e-mail and SMS through the association, while gastroenterology fellows received it via SMS and WhatsApp messages. For participants who did not respond, a follow-up reminder email and message were sent two weeks after the initial contact. A total of 132 gastroenterologists who completed the survey in full were included in the study. Informed consent was implied by response to the survey. No financial compensation was given for participation. The study protocol was approved by the Ethics Committee of Gazi University.
2.2. Survey Instrument
A 26-item survey was developed through internal discussions among team members and based on a review of the literature [
4,
7,
9,
11,
12,
14], particularly studies related to ergonomics in gastroenterological endoscopy. The electronic survey was created using Google Forms and distributed to participants via e-mail and SMS.
Basic demographic information including age, sex, height, and weight was collected. Participants were asked about their affiliated institution and their professional experience. To assess workload, participants were asked about the types of procedures they performed, the total number of endoscopic procedures they performed per week and their average working hours. In addition, participants were asked questions related to ERMI, including the number of injuries, affected joints, severity of the injuries, contributing factors, and strategies used to manage or prevent them.
2.3. Statistical Analysis
All data were arranged, processed, and analyzed with SPSS v.26. Descriptive statistics were presented as frequencies and percentages for categorical variables, and as mean ± standard deviation for continuous variables. The Chi-square test or Fisher’s exact test was used for comparisons between groups for categorical variables. For comparisons of continuous variables between two groups, the Student’s t-test or the Mann-Whitney U test was applied. Pearson or Spearman correlation tests were used to identify variables showing a linear relationship with the severity of injury. Logistic regression analysis was performed to identify factors associated with injury, using the Forward LR method. A p-value of <0.05 was considered statistically significant.
3. Results
Of the 1,100 gastroenterologists who are members of the Turkish Gastroenterology Association (TGA) and were invited to participate, 96 (representing approximately 9% of the total membership) completed the survey. Additionally, 36 out of 253 gastroenterology fellows (representing approximately 14% of the total fellows) responded, a total 132 gastroenterologists. Among these participants, 29 (22%) were female.
The mean age of the participants was 43.6 years, and the mean professional experience among the gastroenterologists was 11 years. A total of 121 participants (91.7%) were right-hand dominant. Of the participants, 36 (27.3%) were fellows currently undergoing training. The majority of gastroenterologists (79.8%) were worked at public institutions (including state universities, city hospitals, training and research hospitals, and government hospitals).
In the workload assessment, 60 participants (43.3%) reported performing more than 60 endoscopic procedures per week. A total of 125 gastroenterologists (94.7%) regularly performed EGD and colonoscopy. Among the endoscopists, 74 (56.1%) performed ERCP, 36 (27.3%) performed EUS, and 24 (18.2%) performed advanced procedures such as ESD, EMR, or POEM. A total of 19 participants (14.4%) reported working more than 40 hours per week. Additionally, 76 gastroenterologists (57.6%) preferred to hold the endoscope with the umbilical cord inside the forearm during procedures.
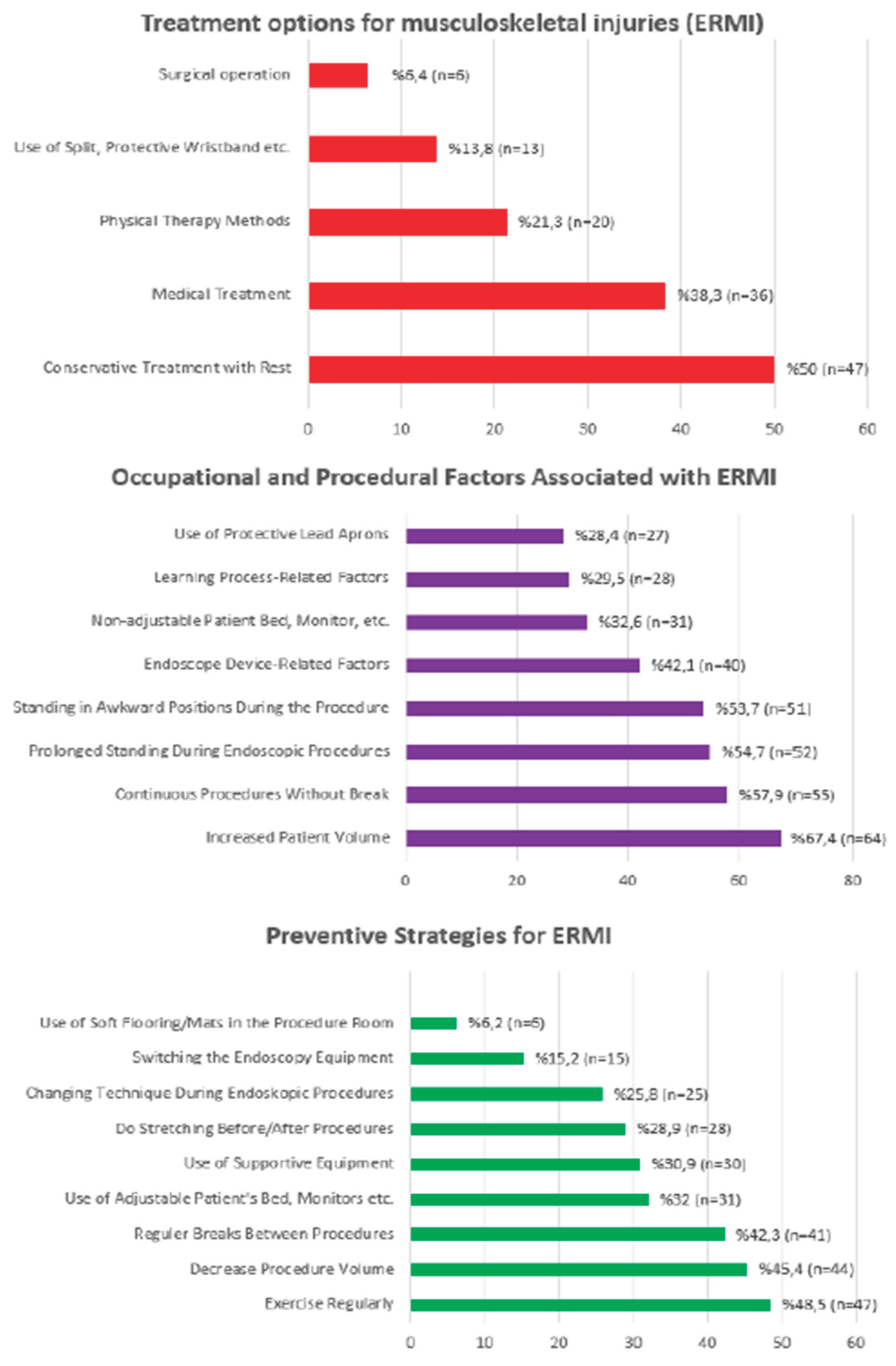
Ninety-five gastroenterologists (72%) reported experiencing at least one ERMI during their professional careers, while 28 (21.2%) reported experiencing work loss due to these injuries. Half of those who experienced ERMI recovered with conservative treatment with rest and medical treatment, while 6 gastroenterologists required surgical intervention.
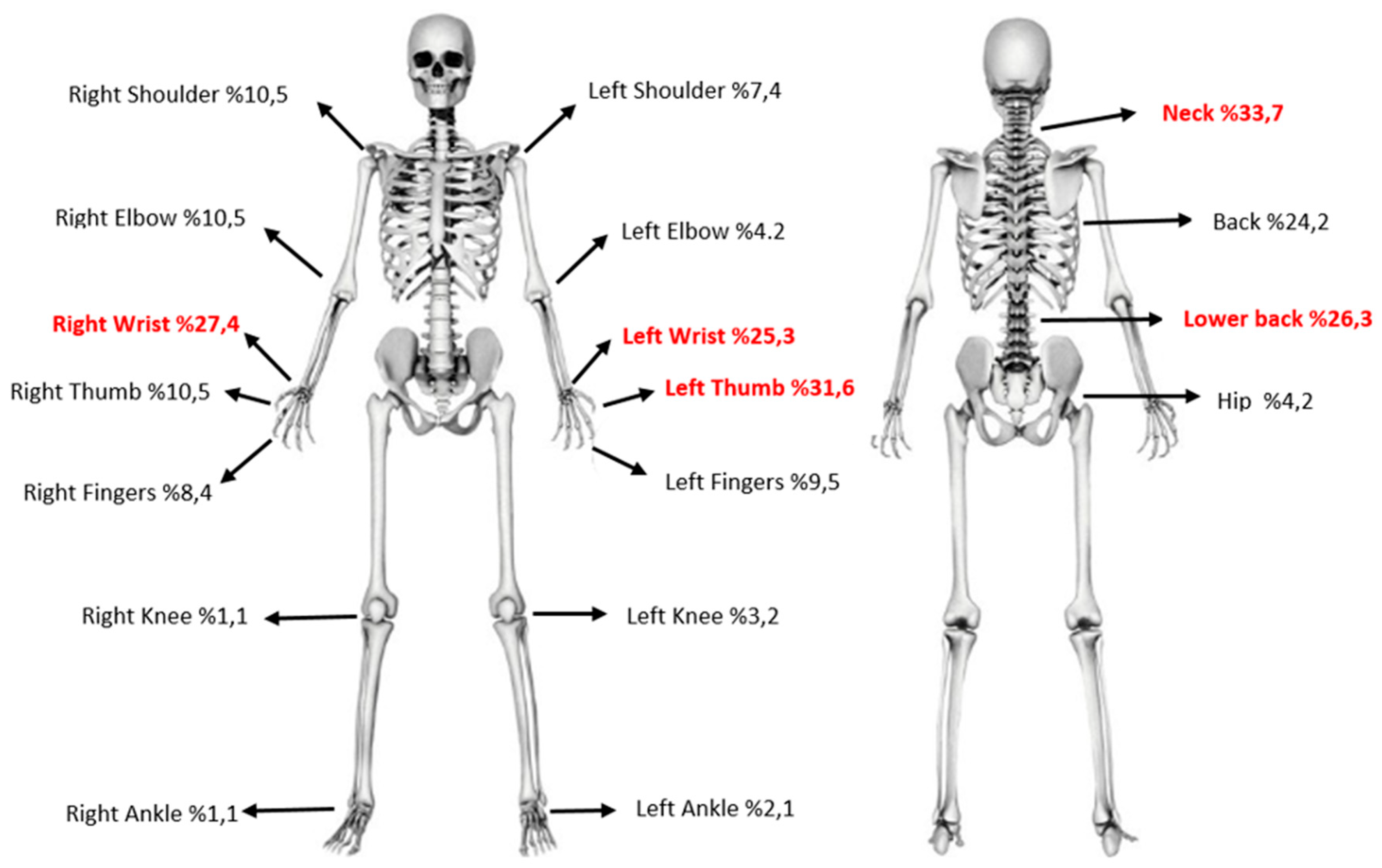
The most frequently injured body region was the neck ( 33.7%), followed by the left thumb (31.6%), right wrist (27.4%), lower back (%26.3), left wrist (25.3%) and back (%24.2) (
Figure 1). Among those who experienced injuries, 63.2% had injuries in multiple joints.
In the assessment of factors causing ERMI, the prominent reasons were increased patient volume, continuous procedures without break, prolonged standing during endoscopic procedures, and standing in awkward positions during the procedures.
To reduce or prevent ERMI, prominent solution strategies include engaging in regular exercise, decrease precedure volume, and taking regular breaks between procedures. The causes, treatment, and preventive strategies of ERMI are presented in
Figure 2.
A statistically significantly higher proportion of female gastroenterologists (89.7%) reported ERMI compared to their male (67.0%) counterparts (p=0.013). In addition, a statistically significant difference was found in the prevalence of ERMI according to the type of institution where the gastroenterologists worked (p=0.047). There was a statistically significant association between the total number of endoscopic procedures performed per week and the presence of ERMI (p=0.038). There was no statistically significant difference in the prevalence of ERMI with respect to dominant hand, glove/hand size, clinical experience, type of endoscopic procedure, total weekly working hours, or endoscope hold technique. The demographic and professional characteristics of the study population and comparison of variables between endoscopists with and without ERMI are summarized in
Table 1.
When participants were asked to rate the severity of their injury using the Visual Analog Score (VAS) from 1 to 10, the average VAS score was found to be 4.76/10. This rate was 7.31 in female gastroenterologists and 3.80 in male, statistically significant difference between genders in injury severity (p = 0.013). There was also a significant difference in injury severity according to glove size (p = 0.001). No statistically significant differences in injury severity were found for other variables (see
Table 2).
In the correlation analysis for the factors affecting the severity of injury; a negative, moderate and statistically significant relationship was found between the severity of injury and height, weight and glove size (p<0,001 for all variable). On the other hand, a positive, weak and statistically significant relationship was found between injury severity and the total number of endoscopic procedures per week (p=0.027). No statistically significant relationship was found between injury severity and other variables (p>0.05) ( see
Table 3).
Logistic regression analyses using the ‘Backward method’ assessing potential factors that increase the likelihood of EMRI showed that female gender increases the likelihood of injury by 5.640 times, while performed ERCP increases the likelihood of injury by 2.685 times. No significant associations were found for the other variables included in the model ( see
Table 4).
A detailed evaluation of the most commonly affected joints due to ERMI and potential associated variables is presented in
Table 5. Sex was found to be significantly associated with back, lower back, and right wrist injuries. Moreover total weekly number of ERCP procedures was found to be significantly associated with neck and left wrist injuries. Hand size was associated with neck and right wrist injuries. Similarly, the total weekly number of ESD/EMR/POEM procedures was associated with right wrist injuries.
4. Discussion
Endoscopic devices, which have a wide range of applications in modern medicine [
15], are an indispensable part of diagnostic and therapeutic procedures in gastroenterology practice. In a Japanese study, endoscopists reported spending a median of 25 hours per week on endoscopic procedures indicating that gastroenterologists devote well approximately 50 % of their clinical practice to endoscopy [
16]. According to data from Türkiye in 2022, approximately 1.5 million upper gastrointestinal endoscopies and 850,000 lower gastrointestinal endoscopies were performed [
13]. The increased patient volume and the develop of novel endoscopic treatment modalities have made ERMI a major occupational concern among gastroenterologists. For over 30 years, numerous studies have been conducted on injuries related to endoscopic procedures [
17]. In this study, the prevalence of ERMI and associated risk factors among gastrointestinal endoscopists were evaluated. Our findings are largely consistent with the existing literature and offer some novel contributions.
4.1. Prevalence of ERMI and Sex-Based Differences
In our study, ERMI was observed in 72% of endoscopists, which is consistent with the previously reported prevalence range of 37% to 89% in the literature[
1,
2].Only 22% of the participants were female. emale gender was found to be significantly associated with both higher frequency and greater severity of injury. Logistic regression analysis revealed that being female increased the risk of developing ERMI by 5.6 times. In the Austin et al. study, female sex was the only factor associated with a higher reported injury rate [
6]. Several studies have reported that female endoscopists are more prone to musculoskeletal injuries compared to their male counterparts [
2,
3,
18,
19,
20]. This difference may be explained by anthropometric and ergonomic factors. Female generally have shorter height, lower body weight, and less muscle mass, which may lead to
physically disadvantages during procedures [
3]. In our study, female participants were also found to have smaller glove sizes. In the 2024 systematic review by Bessone et al. [
15], it is emphasized that female endoscopists face greater challenges and are more prone to microtraumas, particularly due to equipment mismatch. This suggests a potential ergonomic mismatch, as endoscopic equipment is often designed using a one-size-fits-all approach, which may not adequately accommodate female gastroenterologists. Additionally, some studies have suggested that female endoscopists tend to perform procedures more carefully and meticulously, which may lead to prolonged static postures and increased musculoskeletal strain. This indicates that both procedural habits and physiological factors may together contribute to the higher risk of ERMI among female [
3].
All of these findings highlight that ignoring gender-based ergonomic needs may result in a significant occupational burden. Considering the increasing number of female gastroenterologists, the development of gender-sensitive ergonomic equipment, personalized training programs, workplace modifications, and individual exercise regimens aimed at improving muscle mass have become essential requirements.
4.2. Types of Injuries and Affected Joints
Technical insufficiencies during the learning process may increase stress on the musculoskeletal system of endoscopists. Improper handling techniques, prolonged maintenance of poor posture, and non-ergonomic habits often lead to excessive loading on various joints. Over time, this may result in the development of musculoskeletal injuries due to repetitive microtrauma, overuse, and prolonged standing. Repetitive movements, particularly involving the wrist, shoulder, and lower back, contribute significantly to biomechanical strain and the occurrence of ERMI [
6,
7,
8,
17].
In our study, 95 (72%) gastroenterologists reported experiencing at least one ERMI during their professional careers. The most frequently injured body regions were the neck (33.7%), followed by the left thumb (31.6%), right wrist (27.4%), lower back (26.3%), left wrist (25.3%), and back (24.2%). Among the participants, 33 gastroenterologists (36.8%) reported ERMI in a single joint, 19 (20.0%) in two joints, 22 (23.2%) in three joints, 13 (13.7%) in four joints, and 6 individuals (6.3%) had involvement of five or more joints. The upper limbs and thumbs are mainly strained from holding the endoscope, while the neck and back are affected by awkward positions during procedures and focusing on the monitor. In the past two decades, numerous studies conducted in various countries have consistently reported that the most commonly affected joints in ERMI cases are the neck, back, lower back, left thumb, right and left wrists, and shoulders [
4,
7,
9,
11,
12,
16,
18,
21,
22,
23]. In a 2025 meta-analysis of 30 studies published by Oliveira et al. [
20] the most commonly affected joints were the hand-wrist, thumbs, neck, back and lower back. In our study, however, shoulder involvement was observed less frequently. The other commonly affected joints in our study were consistent with those reported in the literature.
It was noted that most injuries were concentrated in the spine and hands. These findings suggest that prolonged procedures, combined with awkward postures and non-adjustable bed or monitor heights, may contribute to excessive stress on the spine. Additionally, the weight of the endoscopic equipment, forceful maneuvers, repetitive hand motions, and overuse during procedures likely result in increased mechanical load and microtrauma in the hands and wrists, contributing to injuries in these regions. Particularly in female, smaller glove size may contribute to hand, wrist, and finger injuries [
3].
In a detailed analysis of the joints most frequently affected by ERMI and their associated factors, gender was significantly associated with injuries to the back, lower back, and right wrist. Additionally, the total number of ERCP procedures performed per week was significantly associated with neck and left wrist injuries. Similarly, the weekly number of ESD/EMR/POEM procedures was associated with right wrist injuries. Hand size was also found to be associated with neck and right wrist injuries. In the study by Bhat et al. [
3], female gender was found to be associated with wrist injuries, while in the study by Suhail et al. [
19], it was associated with neck and back injuries. Our findings were consistent with these reports in the literature. In a study by Campbell et al.[
5] involving gastroenterologists performing ERCP, the most common ERMI sites were the neck, lower back, and wrist, with cases of De Quervain’s tenosynovitis reported. As expected, the study demonstrated that the incidence of injuries increased with a higher number of procedures. In a study by Han et al.[
24] involving advanced third-space (ESD/EMR/POEM) endoscopists from 10 different countries, the prevalence of ERMI was reported as 69%. The most commonly affected joints were the shoulders, back, neck, and wrists. However, no significant association was found between procedural volume and the occurrence of ERMI.
4.3. Workload and Institutional Factors in ERMI
High procedural volume and increased clinical workload have long been considered important risk factors for ERMI. According to 2021 data, it is estimated that in 2019, over 22 million endoscopic procedures were performed in adults in the United States, including approximately 7.5 million EGDs and 13.8 million colonoscopies [
25]. For Turkey, according to 2022 data, approximately 1.5 million upper gastrointestinal endoscopies and 850,000 lower gastrointestinal endoscopies were performed [
13]. This high procedural volume imposes a significant workload burden on gastroenterologists. In our study, it was found that 45.5% of gastroenterologists in Turkey perform more than 60 procedures per week, and approximately 30% spend 17 to 24 hours weekly on endoscopic procedures. This clearly demonstrates the substantial workload burden faced by these specialists. A total of 125 gastroenterologists (94.7%) regularly performed EGD and colonoscopy. Among the endoscopists, 74 (56.1%) performed ERCP, and 24 (18.2%) performed advanced procedures such as ESD, EMR, or POEM. In our study, logistic regression analysis revealed that performing ERCP was associated with a 2.6-fold increased risk of developing ERMI. ERCP is a more complex procedure than standard endoscopy, and it may carry a higher risk of ERMI due to longer procedural duration, the use of lead aprons and protective equipment, and the need for less comfortable or awkward working positions [
5].
The majority of gastroenterologists in our study worked at public institutions (such as state universities, city hospitals, training and research hospitals, and government hospitals) where patient volume and demand for endoscopic procedures are generally higher. Most studies indicate a clear association between high procedural volume and the occurrence of ERMI. Several studies have consistently demonstrated a significant association between high procedural workload and the development of ERMI. In a 2015 study by Ridtitid et al.[
7] performing >20 procedures per week or spending >16 hours on endoscopic tasks was associated with a higher prevalence of ERMI. Similarly, a study conducted in Japan by Matsuzaki et al.[
16] also found that performing >20 procedures or spending >16 hours per week on endoscopy significantly increased the risk of ERMI. More recently, in a 2022 study by Bessone et al.[
2], working more than 15 hours or performing over 15 procedures per week was also found to be significantly associated with ERMI.
High procedure volume makes it difficult for endoscopists to maintain proper ergonomic posture, while working under time pressure can lead to technical errors and impaired body mechanics. In addition, the lack of adequate rest periods between procedures increases physical strain, contributing to microtrauma, muscle fatigue and ergonomic overload, and consequently increasing the risk of ERMI.
4.4. Causes, Treatment and Prevention of ERMI
Endoscopy-related musculoskeletal injuries may result not only from the physical demands of endoscopic procedures, such as repetitive movements, prolonged standing, and awkward postures but also from individual factors like small hand size, low muscle mass, and lack of regular exercise. Furthermore, there are numerous modifiable and adjustable environmental factors as well. In our study, the prominent reasons were increased patient volume, procedures that continued without a break, prolonged standing during endoscopic procedures and inappropriate positions during procedures.
Conservative treatments; such as pharmacologic therapy, massage, physical therapy, rest, splinting, steroid injections, and alternative approaches like acupuncture or chiropractic care are commonly utilized in the management of ERMI [
4]. Endoscopy-related musculoskeletal injuries (ERMI) are primarily managed through conservative strategies, as shown in our findings where 50% of affected gastroenterologists reported using rest-based conservative treatment, and 38.3% relied on medical therapies, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or analgesics, Physical therapy was used by 21.3%, often including posture correction, muscle strengthening, and stretching programs. Supportive measures such as wrist splints or protective bands were less commonly utilized (13.8%) ,while 6 gastroenterologists required surgical intervention. Furthermore, 28 participants (21.2%) reported work loss due to these injuries. These results are consistent with previous literature emphasizing that early, non-surgical management is often sufficient in the majority of ERMI cases.
Another important factor contributing to ERMI is the challenge encountered during the learning process. Gaining access to endoscopic equipment without adequate theoretical and practical training may lead to improper or incorrect usage, which in turn increases the risk of musculoskeletal injuries. In addition, the lack of regular breaks between procedures or the failure to perform stretching exercises before and after endoscopic interventions may also contribute to an increased susceptibility to musculoskeletal injuries. If modifiable factors such as improper endoscopic techniques and incorrect positioning of equipment (e.g., bed, monitor) in the procedure room are not corrected, injuries may recurrence and become chronicity. therefore, the equipment in the processing room needs to be redesigned in the most optimal way, Both ergonomic modifications in the procedure room and structured ergonomics training have been emphasized in the literature as essential strategies to reduce musculoskeletal injury risk among endoscopists [
15,
20]. In the study by Suhail et al., the majority of trainers recommended incorporating ergonomics education into endoscopy training programs [
19].
In our study, the most frequently reported factor associated with musculoskeletal injuries was increased patient and procedural volume. Consequently, one of the most commonly adopted strategies among participants was to limit the number of endoscopic procedures. Similarly, several studies in the literature have reported that reducing procedure volume is often the first strategy preferred by endoscopists to mitigate injury risk [
2,
7,
11,
20]. However, this approach is not always feasible, especially in institutions such as public hospitals where patient demand is high.
5. Conclusions
This nationwide cross-sectional study highlights a high prevalence of ERMI among gastroenterologists in Türkiye. The most frequently affected joints were the neck, thumb, and wrists, with increased procedural volume, female sex, small glove size, and institutional workload identified as key contributing factors. Our findings are largely consistent with previous literature and emphasize the multifactorial nature of ERMI, involving ergonomic, anthropometric, and occupational variables. Addressing these injuries requires a comprehensive approach, including procedure room modifications, ergonomics-focused training during endoscopy education, reguler breaks, and institution-level support. With the growing number of procedures and female professionals in the field, ergonomic standardization and gender-sensitive equipment design should be prioritized to prevent long-term disability and ensure career sustainability. The findings are expected to contribute to the development of ergonomic training programs and effective preventive strategies.
Author Contributions
Conceptualization, H.K.; methodology, H.K.; formal analysis, H.K G.K and A.K; investigation, H.K, E.C, B.D, D.K.;; data curation, H.K and K.M.; writing—original draft preparation, H.K.; writing—review and editing, H.K and G.K.; visualization, H:K.; supervision, G.K, A.K, K.M , M.K, M.C, T.K. ; project administration, G.K.; . All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Gazi University ( approval date: 25 February 2025).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors declare that they have no acknowledgments.
Conflicts of Interest
The authors declare no conflicts of interest
Abbreviations
The following abbreviations are used in this manuscript:
| ERMI |
Endoscopic procedures-related musculoskeletal injuries |
| EGD |
Esophagogastroduodenoscopy |
| ERCP |
Endoscopic retrograde cholangiopancreatography |
| EMR |
Endoscopic mucosal resection |
| ESD |
Endoscopic submucosal dissection |
| POEM |
Peroral endoscopic myotomy |
References
- Yung DE, Banfi T, Ciuti G, Arezzo A, Dario P, Koulaouzidis A. Musculoskeletal injuries in gastrointestinal endoscopists: A systematic review. Expert Rev Gastroenterol Hepatol [Internet]. 2017 [cited 2025 Jul 13];11(10):939–47. Available from: https://www.tandfonline.com/doi/abs/10.1080/17474124.2017.1356225. [CrossRef]
- Bessone V, Adamsen S. Gastrointestinal endoscopy and work-related injuries: an international survey. Endosc Int Open [Internet]. 2022 May [cited 2025 Jul 15];10(05):E562–9. Available from: http://www.thieme-connect.com/products/ejournals/html/10.1055/a-1789-0506. [CrossRef]
- Bhatt A, Patil P, Thosani NC. Endoscopy ergonomics: a survey-based study exploring gender differences. Gastrointest Endosc [Internet]. 2024 Jul 1 [cited 2025 Jul 13];100(1):17–26. Available from: https://pubmed.ncbi.nlm.nih.gov/38185181/. [CrossRef]
- Pawa S, Banerjee P, Kothari S, D’Souza SL, Martindale SL, Gaidos JKJ, et al. Are All Endoscopy-Related Musculoskeletal Injuries Created Equal? Results of a National Gender-Based Survey. Am J Gastroenterol [Internet]. 2021 Mar 1 [cited 2025 Jul 13];116(3):530–8. Available from: https://pubmed.ncbi.nlm.nih.gov/33560650/. [CrossRef]
- Campbell E V., Muniraj T, Aslanian HR, Laine L, Jamidar P. Musculoskeletal Pain Symptoms and Injuries Among Endoscopists Who Perform ERCP. Dig Dis Sci [Internet]. 2021 Jan 1 [cited 2025 Jul 13];66(1):56–62. Available from: https://pubmed.ncbi.nlm.nih.gov/32144599/. [CrossRef]
- Austin K, Schoenberger H, Sesto M, Gaumnitz E, Teo Broman A, Saha S. Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey. Dig Dis Sci [Internet]. 2019 Jun 15 [cited 2025 Jul 13];64(6):1439–47. Available from: https://pubmed.ncbi.nlm.nih.gov/30684073/. [CrossRef]
- Ridtitid W, Coté GA, Leung W, Buschbacher R, Lynch S, Fogel EL, et al. Prevalence and risk factors for musculoskeletal injuries related to endoscopy. Gastrointest Endosc [Internet]. 2015 Feb 1 [cited 2025 Jul 13];81(2):294-302.e4. Available from: https://www.giejournal.org/action/showFullText?pii=S0016510714019270. [CrossRef]
- Byun YH, Lee JH, Park MK, Song JH, Min BH, Chang DK, et al. Procedure-related musculoskeletal symptoms in gastrointestinal endoscopists in Korea. World J Gastroenterol [Internet]. 2008 Jul 21 [cited 2025 Jul 13];14(27):4359–64. Available from: https://pubmed.ncbi.nlm.nih.gov/18666326/. [CrossRef]
- Kuwabara T, Urabe Y, Hiyama T, Tanaka S, Shimomura T, Oko S, et al. Prevalence and impact of musculoskeletal pain in Japanese gastrointestinal endoscopists: A controlled study. World J Gastroenterol [Internet]. 2011 [cited 2025 Jul 15];17(11):1488. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3070024/.
- Ono S, Nakajima S, Owada S, Tomita N, Tsuda M, Yamada M, et al. A Survey on Endoscopy-Related Musculoskeletal Injuries in Japanese Endoscopists Focused on Injury Sites and Risk Factors. Dig Dis Sci [Internet]. 2025 [cited 2025 Jul 13]; Available from: https://pubmed.ncbi.nlm.nih.gov/40102344/. [CrossRef]
- Sturm N, Leukert J, Perkhofer L, Hann A, Wagner M, Mayer B, et al. The impact of endoscopic activity on musculoskeletal disorders of high-volume endoscopists in Germany. Sci Rep [Internet]. 2022 Dec 1 [cited 2025 Jul 13];12(1):1–12. Available from: https://www.nature.com/articles/s41598-022-12400-4. [CrossRef]
- Morais R, Vilas-Boas F, Pereira P, Lopes P, Simões C, Dantas E, et al. Prevalence, risk factors and global impact of musculoskeletal injuries among endoscopists: a nationwide European study. Endosc Int Open. 2020;08(04). [CrossRef]
- AKDOĞAN KAYHAN Meral, ÇETİNKAYA Erdinç, ÖTER Volkan, ÇOLAKOĞLU Muhsmmet Kadri, ER Sadettin, ERİŞMİŞ Betül, ÖZTÜRK Ömer,TERZİOĞLU Serdar Gökay UİS. Üst Ve Alt Gastrointestinal Sistem Endoskopisi Akılcı İstem Kılavuzu [Internet]. Ankara; 2024. Available from: https://ekutuphane.saglik.gov.tr/Yayin/668.
- Austin K, Schoenberger H, Sesto M, Gaumnitz E, Teo Broman A, Saha S. Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey. Dig Dis Sci [Internet]. 2019 Jun 15 [cited 2025 Jul 15];64(6):1439–47. Available from: https://link.springer.com/article/10.1007/s10620-019-5463-7. [CrossRef]
- Bessone V, Roppenecker DB, Adamsen S. Work-Related Musculoskeletal Injury Rates, Risk Factors, and Ergonomics in Different Endoscopic Specialties: A Review. Healthc 2024, Vol 12, Page 885 [Internet]. 2024 Apr 24 [cited 2025 Jul 14];12(9):885. Available from: https://www.mdpi.com/2227-9032/12/9/885/htm. [CrossRef]
- Ippei Matsuzaki A, Ebara T, Tsunemi M, Hatta Y, Yamamoto K, Baba A, et al. Effects of endoscopy-related procedure time on musculoskeletal disorders in Japanese endoscopists: a cross-sectional study. Endosc Int Open [Internet]. 2021 May [cited 2025 Jul 14];09(05):E674–83. Available from: http://www.thieme-connect.com/products/ejournals/html/10.1055/a-1352-3850. [CrossRef]
- Buschbacher R. Overuse syndromes among endoscopists. Endoscopy [Internet]. 1994 [cited 2025 Jul 15];26(6):539–44. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-2007-1009030. [CrossRef]
- Villa E, Attar B, Trick W, Kotwal V, Van Buren W. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc Int Open [Internet]. 2019 Jun [cited 2025 Jul 14];07(06):E808–12. Available from: http://www.thieme-connect.com/products/ejournals/html/10.1055/a-0811-5985. [CrossRef]
- Suhail FK, Luo Y, Williams K, Advani R, Campbell K, Dunleavy K, et al. Sex differences impact ergonomic endoscopic training for gastroenterology fellows. Gastrointest Endosc [Internet]. 2024 Feb 1 [cited 2025 Jul 15];99(2):146-154.e1. Available from: https://www.sciencedirect.com/science/article/pii/S0016510723029346?casa_token=yppAch31aOMAAAAA:q-u9cQs__nLZGDkD6NeB3B4cJ0xQuSbmWkhbPAhk6u82Oxd77G0RTCMFChgFig8fkS8NFISKUog.
- Oliveira R, Roseira J, Estevinho MM, Tavares de Sousa H, Rolanda C, Meining A, et al. Endoscopy-Related Musculoskeletal Injuries: A Systematic Review and Meta-Analysis on Prevalence, Risk Factors and Prevention. United Eur Gastroenterol J [Internet]. 2025 [cited 2025 Jul 14]; Available from: /doi/pdf/10.1002/ueg2.70042. [CrossRef]
- Byun YH, Lee JH, Park MK, Song JH, Min BH, Chang DK, et al. Procedure-related musculoskeletal symptoms in gastrointestinal endoscopists in Korea. World J Gastroenterol [Internet]. 2008 Jul 21 [cited 2025 Jul 15];14(27):4359. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2731189/. [CrossRef]
- Hansel SL, Crowell MD, Pardi DS, Bouras EP, DiBaise JK. Prevalence and impact of musculoskeletal injury among endoscopists: A controlled pilot study. J Clin Gastroenterol [Internet]. 2009 May [cited 2025 Jul 15];43(5):399–404. Available from: https://journals.lww.com/jcge/fulltext/2009/05000/prevalence_and_impact_of_musculoskeletal_injury.3.aspx. [CrossRef]
- Kamani L, Kalwar H. Ergonomic Injuries in Endoscopists and Their Risk Factors. Clin Endosc [Internet]. 2021 May 1 [cited 2025 Jul 15];54(3):356–62. Available from: https://synapse.koreamed.org/articles/1150966. [CrossRef]
- Han S, Hammad HT, Wagh MS. High prevalence of musculoskeletal symptoms and injuries in third space endoscopists: an international multicenter survey. Endosc Int Open [Internet]. 2020 Oct [cited 2025 Jul 15];08(10):E1481–6. Available from: http://www.thieme-connect.com/products/ejournals/html/10.1055/a-1236-3379.
- Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology [Internet]. 2022 Feb 1 [cited 2025 Jul 15];162(2):621–44. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0016508521036556. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).