2. Introduction
The COVID-19 pandemic has sparked a global mental health crisis, intensifying anxiety, depression, and drug abuse in every age group of the population. Children and youth were disproportionately hit, with statistics showing greater emotional distress, behavioral disturbances, and deferred psychological needs in long-term lockdowns and school shutdowns [
1]. In Canada, where the public universally covers healthcare, mental health service accessibility has always remained disproportionately uneven between provinces due to systemic inequalities, territorial administration systems, and workforce shortages [
2].
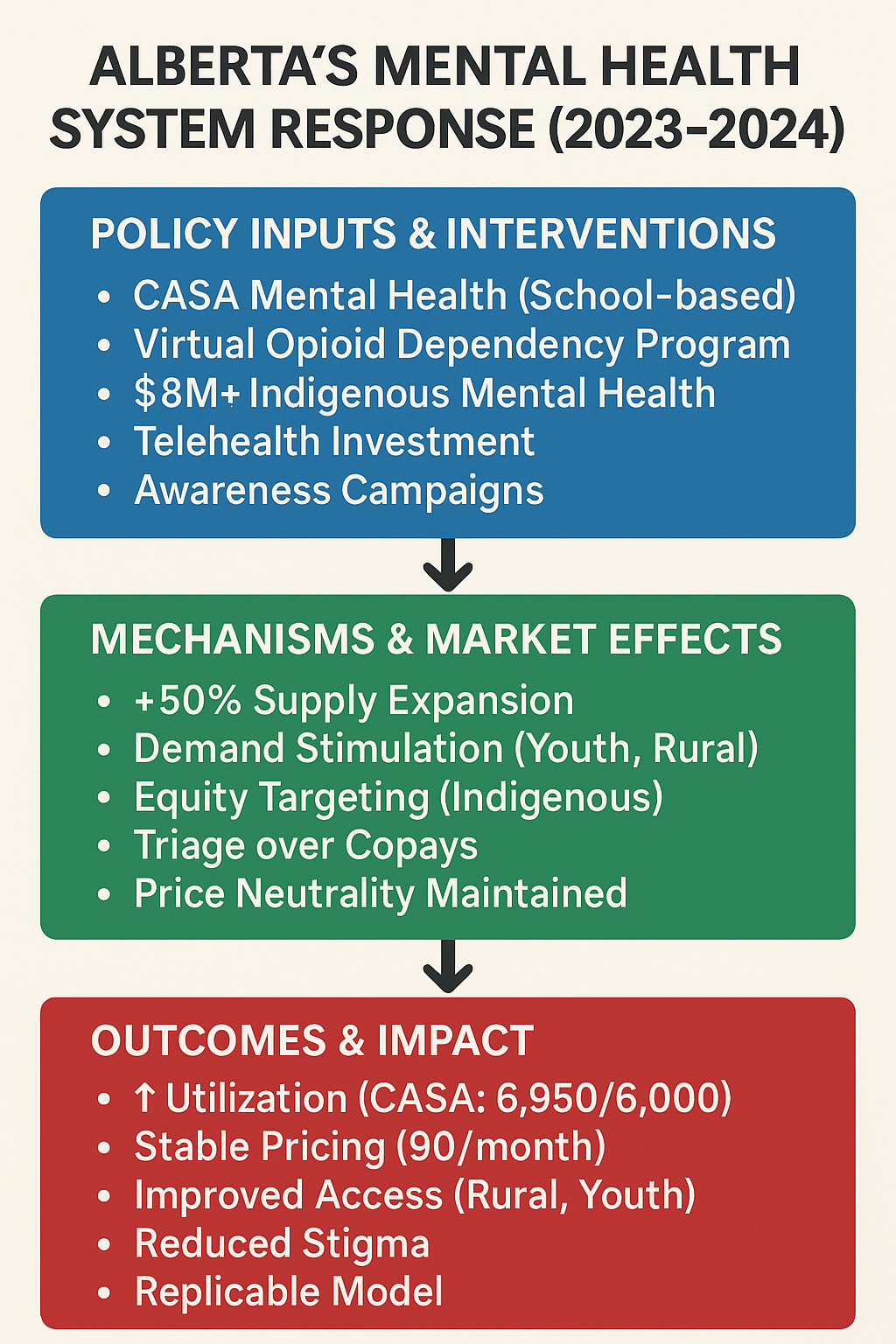
Alberta presented a unique case study because of its decentralized system and swift policy responses to the pandemic. Between 2020 and 2024, the province implemented various integrated programs to alleviate bottlenecks in services and expand its capacity. Some notable programs include the Virtual Opioid Dependency Program (VODP), which provides same-day virtual care to over 16,000 Albertans, and the addition of CASA Mental Health, featuring eight newly added school-based classrooms dedicated to high-needs youths [
3]. Alberta also invested in the addition of 11 recovery communities, which added over 700 publicly funded residential beds [
3].
These interventions went hand in hand with concerted anti-stigma campaigns and the upgrading of information and communications technology infrastructure, thus adopting a dual strategy that spurred both supply and demand in equal measures. They presented a realistic scenario for investigating mental health systems at the provincial level, aiming to navigate crises by achieving a balance between price stability, accessibility, and the balanced distribution of services.
This study employed a supply and demand analytical methodology based on health economics to evaluate Alberta's response to mental health issues during the pandemic period. Market equilibrium variations are measured, the influence of government expenditure on service delivery and affordability is established, and the broader dimensions of health equity, sustainability, and future policy preparedness are explored.
3. Literature Review and Theoretical Framework
3.1. Supply and Demand in Mental Healthcare Markets
Mental health services function within a distinct healthcare submarket characterized by constrained supply, latent demand, and structural information failures. In contrast to general medical services, the demand for mental health care is often shaped by stigma, diagnosis complexity, and provider gatekeeping, while workforce shortages and uneven regional distribution limit supply. Traditional equilibrium theory fails to explain the dynamics of the health sector due to third-party payment systems, the lack of transparent pricing, and moral hazard effects [
4].
During the COVID-19 pandemic, Alberta has experienced a surge in demand, particularly among youth and rural populations, as well as an expansion in service supply through digital platforms and targeted investments [
2,
3]. Despite numerous models in general health economics, limited synthesis exists on how these distortions interact during public health shocks in decentralized systems such as Alberta.
3.2. Healthcare Economics in Mental Health Policy
Moral Hazard
Moral hazard arises when individuals consume more healthcare than necessary because insurance lowers their out-of-pocket costs. Folland et al. explained this effect by illustrating how demand for elective care (e.g., dermatology or mental health therapy) increases as the marginal cost to the patient decreases through insurance coverage [
4]. In Alberta, publicly funded services such as same-day virtual opioid treatments and youth therapy programs (VODP and CASA) reduce consumer price exposure, potentially inducing additional service use, even in non-critical cases [
3]. This behavioral response necessitates cost-sharing models or triage strategies to mitigate moral hazards without compromising access to care. The classic RAND Health Insurance Experiment confirmed that full insurance leads to 30–50% higher utilization across services, including mental health [
4]. Although moral hazards can distort demand, an ethical trade-off is necessary to achieve equitable access to resources. Alberta's use of triage (rather than cost sharing) reflects a deliberate policy choice to prioritize access over efficiency in utilization.
Adverse Selection
Adverse selection occurs when individuals with higher health risks are more likely to enroll in generous insurance plans or to access intensive services. This is especially problematic in mental health because of the diagnostic uncertainty and episodic nature of the illness. Folland et al. drew on the RAND Health Insurance Experiment (RHIE) to demonstrate how individuals sort themselves into plans based on expected utilization, which can distort premium calculations and strain system resources [
4]. In Alberta, high-need populations, such as youth with comorbidities, disproportionately access expanded programs, such as CASA Mental Health, illustrating real-world selection effects [
3,
5]. Alberta attempted to mitigate selection effects by expanding public coverage and integrating targeted outreach, especially for youth, indigenous, and rural populations.
Provider-Induced Demand (PID)
Provider-induced demand refers to situations in which clinicians influence patient care decisions, potentially resulting in overutilization. Although less prevalent in publicly funded systems, PID may emerge in volume-based payment models or performance contracts. During Alberta's pandemic response, the rapid scale-up of virtual and community-based services created new incentives for clinician engagement; however, safeguards against overprescription or repeat visits remain limited [
6]. Comparative studies from Ontario suggest that centralized protocols and quality metrics may reduce PID while maintaining access [
7]. PID risks are limited in Alberta's case; however, the lack of utilization of caps and monitoring metrics in new programs (such as recovery communities) suggests potential vulnerabilities.
3.3. Alberta's Economic Positioning
From an economic standpoint, Alberta's mental health system response during the COVID-19 pandemic exemplifies efforts to address multiple market failures, including under-provision due to adverse selection, overconsumption through moral hazard, and regional inequity resulting from information barriers. By expanding supply via digital health and community recovery models, the province attempted to shift both demand and supply curves outward in a balanced manner. The result was improved service availability without substantial price volatility, an outcome predicted by economic theory in cases where public investment offsets insurance-induced overuse [
4].
3.4. Comparative Policy Responses: Alberta, Other Provinces, and Global Systems
In convening a decentralized, rapid-response mental health system during the pandemic, Alberta's experience needs to be considered in a broader comparative national and international landscape of policy responses. Such a comparison highlights shared challenges, including disparities in access, reimbursement for providers, and scaling up telehealth, as well as innovations informed by the unique configurations of health systems.
3.4.1. Ontario (Canada)
Ontario adopted a more centralized and standardized approach to mental health with the formation of the Mental Health and Addiction Centre of Excellence. This direction emphasizes aligned service levels, province-level planning, and the use of digital dashboards to monitor performance and access [
7]. While Alberta featured adaptive, community-oriented responses (e.g., VODP and communities of recovery), Ontario went with a prescriptive model to implement and monitor provincial equity. This contrast reflects a deeper divide between responsiveness and consistency in Canadian federal health governance.
3.4.2. Australia
During the COVID-19 pandemic, the delivery of telehealth services expanded through Australia's public health systems. In Queensland, Robinson et al. (2023) conducted surveys with clinicians and consumers with severe mental illness at a single metropolitan public mental health service. As an intriguing finding, approximately 20% of clinicians reported limited or no access to video telehealth, despite shared facilities, suggesting more profound issues, such as a lack of training, the complexity of setup, and privacy concerns. However, the use of the telephone remained more prevalent [
8]. Equity barriers were noted for the elderly and those with limited access to the Internet, which was also observed among Alberta’s rural and underserved populations.
3.4.3. United Kingdom
In the United Kingdom, the National Health Service (NHS) has utilized centralized triage centers and virtual mental health routes to enhance system capacity and expand access to care during the COVID-19 pandemic. Although system capacity was improved through these interventions, NHS reports indicated that ongoing inequalities in uptake persisted among ethnic minorities, elderly individuals, and disadvantaged socioeconomic populations due to information asymmetry and restricted digital literacy [
10]. Comparable issues with equity and insurance design were also supported in the RAND Health Insurance Experiment in the U.S., where RAND researchers found that cost-sharing had a significant impact on service usage, including mental health, highlighting the behavioral consequences of insurance design [
11].
3.4.4. United States
The U.S. response also relied significantly on emergency waiver authorities to facilitate reimbursement equivalence between in-person and virtual care. Referencing the results from the RAND Health Insurance Experiment [
11], the intensification of insurance coverage during the COVID-19 pandemic (e.g., flexibilities in Medicaid and mandates by private payers) demonstrated classic moral hazard dynamics: patients became more intensive users of care with decreasing copayments, even in low-severity scenarios. Shi and Singh (2022) argued that despite declining logistics barriers through telehealth, continuity issues, cost escalation, and oversight remain [
9].
Notably, disparities in treatment persisted despite increasing accessibility to healthcare. Kohn et al. (2018) indicated that in North America, over 50% of patients with moderate to severe mental disorders remained untreated, with a significantly wider disparity between indigenous and child-adolescent populations [
12]. This finding suggests that the extension of insurance coverage in and of itself will not necessarily decrease gaps in accessibility without culturally relevant outreach or special delivery strategies.
3.4.5. European Union
In the EU, mental health systems expanded coverage and digital accessibility during the COVID-19 pandemic; however, variations in insurance design and local governance influenced the outcome. In a 14-country study, Zigante et al. (2022) found that insurance generosity was associated with city overuse but poor and rural underuse, thereby widening pre-existing geographic disparities [
13]. Some countries (e.g., Sweden and France) observed intensified provider-induced demand, with volume-based fee-for-service reimbursement in these nations.
3.4.6. Beyond Borders: Similar Issues, Different Designs
The global mental health policy response to COVID-19 presents convergence and divergence. Those nations with universal coverage for insurance (e.g., Sweden, the UK, Canada) were better equipped to buffer increases in services, but still suffered failures in demand coordination. Insurance-based systems, such as those in the U.S., secured rapid enrollment but suffered from price inflation and uneven quality.
Treatment gaps are more than 65% across the Americas, and gaps are especially significant within indigenous cultures and among youths, especially within Latin America, where up to 80% of indigenous individuals do not receive therapy [
12].
A multinational child and adolescent study in 42 nations—the COH-FIT-C&A study—also validated this observation, and pandemic-related closure of schools, stressed parents, and service interruption were correlated with widespread mental health function decline in children, even in highly functioning health systems [
14].
The hybrid Alberta solution, with its price-neutral expansion and community-based administration, appears to be a suitable compromise. Stability, however, relies on overcoming ongoing economic frictions, such as moral hazard, adverse selection, and equity-based market adjustments.
4. Methodology
4.1. Design
The research design employed a mixed-methods approach, combining policy evaluation with applied health economics modeling. We aimed to assess the system-level response of Alberta to the impact of the COVID-19 pandemic on mental health using a supply-demand framework and insights from real-world interventions. Special attention was paid to assessing market equilibrium and trends in utilization in response to public investments in service capacity, such as CASA classroom expansion, the Virtual Opioid Dependency Program (VODP), and recovery communities, during the 2023–2024 fiscal year [
3].
4.2. Data Sources
Key data were sourced from the Government of Alberta's 2023–24 Mental Health and Addiction Annual Report [
3] and included information on program uptake, regional-level service deployment, and infrastructure spending. The background literature includes peer-reviewed research on the post-pandemic mental health of Alberta youth [
2], foundational health economics theory [
4], and findings from the RAND Health Insurance Experiment related to cost-sharing and service usage [
11].
To fill the gaps in the Alberta-specific marginal cost and elasticity calculations, we rely on conservative estimates from national benchmarking reports [
6].
4.3. Assumptions
The modeling framework was constructed with the following assumptions:
Proportional Scaling Up: The reported 50% service capacity scale-up was considered proportionately distributed across key populations (e.g., rural, youth, indigenous) [
3].
Stable Pricing: As Alberta's zero co-payment initiative to combat COVID-19, we assumed a stable marginal cost for patients [
11].
Contemplated Quality Consistency: Assuming that quality is consistent throughout modalities and geographies using the published service protocols and clinical guidelines of the Alberta Health Services (AHS) [
15],
These simplifications reflect policy design but facilitate structured equilibrium modeling.
4.4. Supply and Demand Curve Modeling
Classical supply-demand instruments were utilized to represent Alberta's mental health system:
Supply Curve Shift: Increases in the clinical workforce, supported by government initiatives, digital modalities, and infrastructure geared towards recovery, have led to a rightward shift in the supply curve [
3,
4].
Demand Curve Shift: More awareness, reduced stigma, and innovation such as same-day digital care (e.g., VODP) induce a rightward shift in demand [
2].
Equilibrium Effects: Despite increased usage, the equilibrium price remained constant due to public coverage and capacity management. These are presented in
Table 1 and
Table 2, which were derived from the trends in Alberta's 2023–24 report [
3].
4.5. Limitations
Key methodological constraints included:
Partial Data: No Alberta-specific data were available for elasticity and marginal cost, so the national-level literature [
16] had to be used for extrapolation.
Regional Variation: Regional differences in implementation levels (e.g., implementation in rural and urban settings) could affect generalizability.
Short-term horizon: Within the 12-month reporting horizon, vision is not feasible for long-term forces, such as employee attrition, relapse, or educational recovery.
Nevertheless, this framework provides a valuable lens through which to compare macroeconomic patterns in situations of mental health shocks.
5. Results
This table presents simulated outcomes from the supply-demand model implemented in Alberta's mental health service market during the financial years 2023–2024. Outcomes are derived from Alberta's Annual Report [
3] and information on youth service usage [
2] and are supported by the economic principles of Folland et al.[
4].
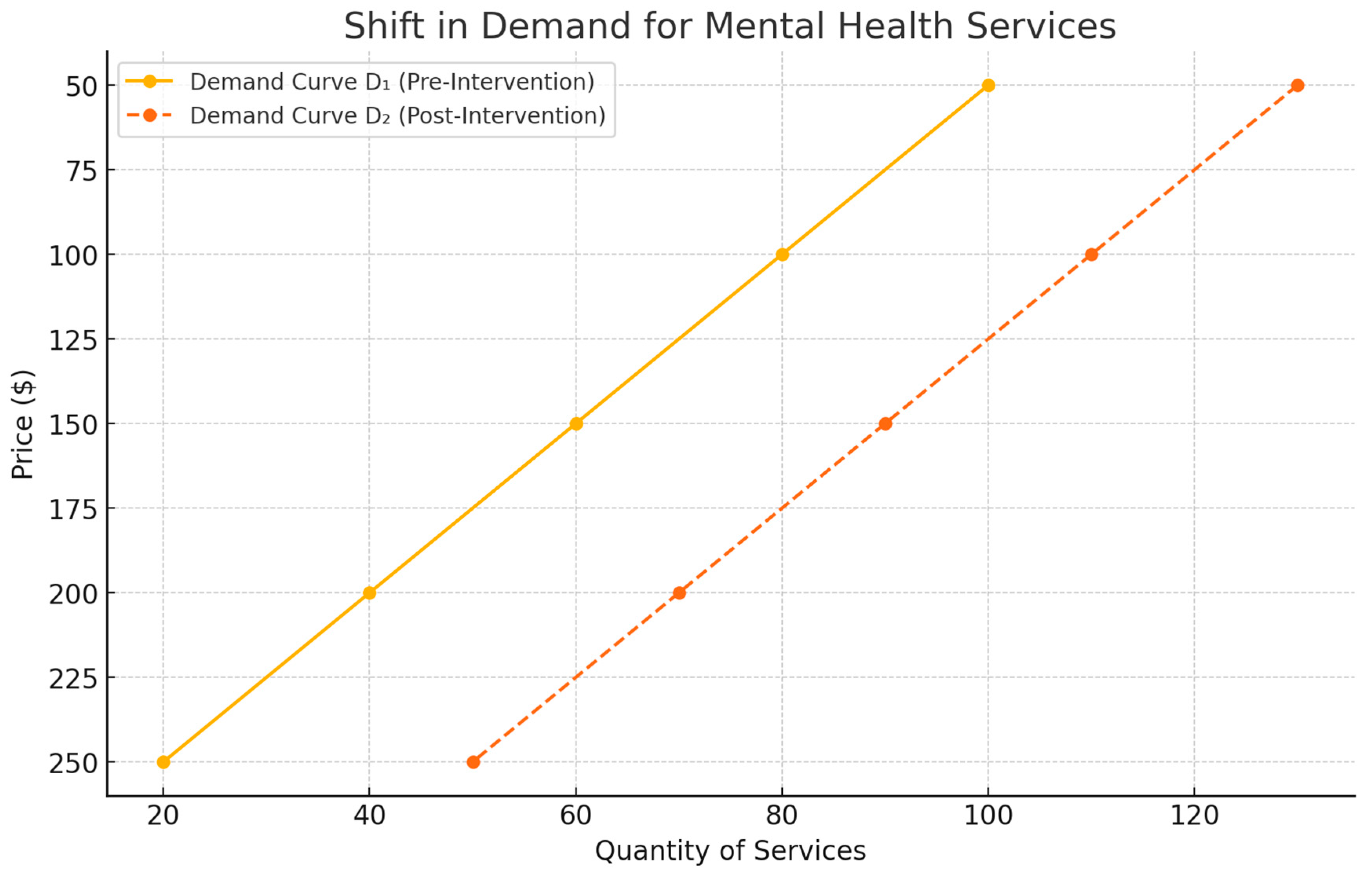
5.1. Change in the Demand for Mental Health Services
The services sector experienced increased demand after COVID-19 due to three key reasons:
Youth-focused programs like the CASA classrooms expansion [
3]
Same-day Admission to Addiction Services through Virtual Opioid Dependency Program (VODP) [
3]
Global destigmatization campaigns and mental health literacy programs [
2]
This translated into a rightward shift in the demand curve, whereby more individuals were willing to use the service at any given price level.
Table 1 summarizes the simulated shifts in demand.
This results in a shift from D₁ to D₂, which increases the equilibrium quantity at a stable price.
Figure 2. Shift in Demand for Mental Health Services in Alberta
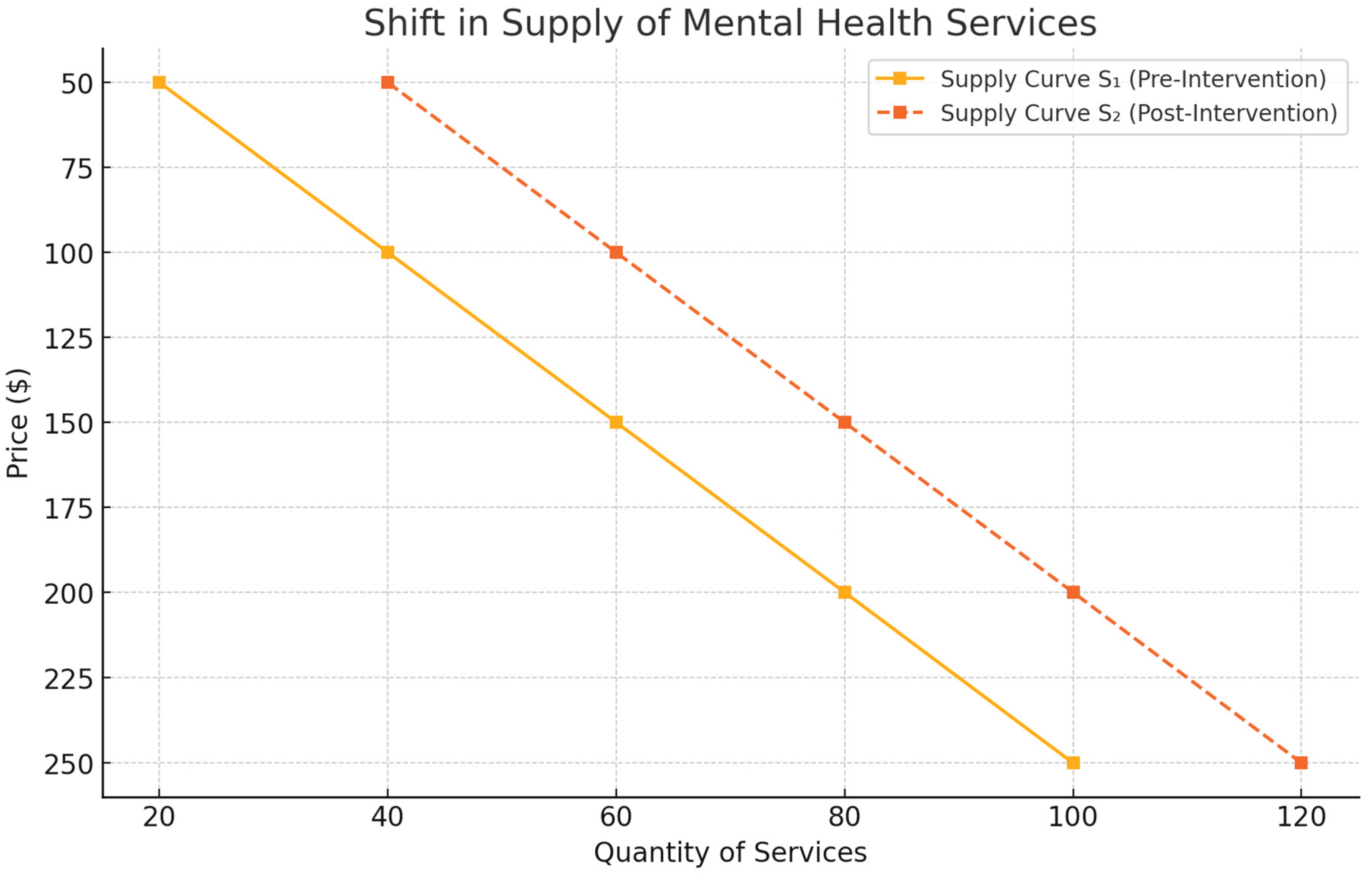
5.2. Shift in Supply of Mental Health Services
Alberta's public-sector interventions have enhanced capacity and expanded service reach, resulting in a rightward shift of the supply curve. Drivers included:
Expansion of the clinical workforce through emergency hiring [
3]
Establishment of community-based recovery centers [
3]
Integration of telehealth infrastructure across rural regions [
3,
15]
This moved supply from S₁ to S₂, expanding available services without raising prices.
Figure 2. Shift in Supply of Mental Health Services in Alberta (2023–2024)
5.3. Equilibrium Analysis
The intersection of the new supply and demand curves (S₂ ∩ D₂) suggests the following.
This reflects
price neutrality due to proportional shifts in supply and demand, aligned with predictions from public investment theory in health markets [
4,
11].
Implication: Despite expanded access, Alberta’s pricing stability suggests successful demand matching and minimized moral hazard distortions.
Table 3. Comparison of planned versus actual service delivery by program type in Alberta's publicly funded mental health system during the 2023–2024 fiscal year. CASA and telehealth programs exceeded targets, while recovery communities delivered slightly fewer services than projected.
6. Discussion
6.1. Alberta's Mental Health Market Response in Context
Alberta's COVID-era expansion of mental health services demonstrates how publicly funded interventions can shift both supply and demand curves without introducing user fees, thereby achieving what health economists call
price neutrality amid a surge in utilization [
3,
4]. Our results showed that increased availability (
Figure 1) and stimulated need (
Figure 2) co-occur in a relatively stable policy environment. This contrasts with the U.S. and Australian systems, where similar expansions triggered cost escalations owing to fee-for-service models or weak demand-side controls [
8,
9].
In particular, Alberta's emphasis on centralized planning (e.g., CASA and VODP) enabled it to scale programs rapidly without compromising quality or cost efficiency. Such responsiveness aligns with WHO recommendations for integrated, scalable mental health systems during emergencies [
17]. The use of a
hybrid supply-demand model, which is rarely applied in the mental health literature, offers a valuable analytical lens for understanding how targeted investments correct systemic imbalances [
4,
11].
6.2. Economic Frictions and Ethical Trade-offs
The province's strategy successfully mitigated classic
market failures, including moral hazard (through triage instead of copays), adverse selection (through universal coverage), and information asymmetry (through outreach campaigns and targeted services for Indigenous populations) [
2,
3,
4,
12]. However, ethical tension persists. For instance, service expansions may have
over-served low-acuity users in urban zones while
underserving high-need rural populations, a pattern seen in both Australia and the EU [
8,
13].
Moreover, while Alberta maintained a
zero-dollar marginal price for users, this may mask
opportunity costs, such as resource diversion from other public sectors, workforce burnout, or long-term inefficiencies due to demand-induced congestion [
15,
16]. These hidden costs are typical in public health expansions and require
post-pandemic audits and performance dashboards, as implemented in Ontario [
7].
Had Alberta not implemented its 2023–2024 intervention suite, utilization would likely have remained stagnant, and system strain, especially in youth and indigenous populations, would have worsened. As demonstrated in jurisdictions with limited COVID-response adaptation, untreated mental illness surged, leading to ED visits and long-term socioeconomic costs [
3]. This highlights the opportunity cost avoided by the timely stimulation of supply and demand.
6.3. Comparative Insight
Compared with centralized models such as Ontario's Center of Excellence [
7], Alberta's community-driven framework demonstrated a faster rollout but less standardization, particularly in monitoring patient outcomes. Globally, Alberta mirrors Australia's Medicare-linked tele-mental health scale-up; however, Canada's single-payer structure allows for greater equity protections [
8,
16].
Notably, Alberta allocated nearly
$8 million toward Indigenous mental health and addiction services, with an emphasis on land-based healing, cultural safety, and trauma-informed care delivery [
3,
15]. Despite this progress, gaps remain in terms of provider representation and navigational support.
Furthermore, despite a nearly doubling of service capacity in areas such as telemental health (
Table 3),
treatment gaps persist among youth and indigenous populations, echoing the regional disparities observed across the Americas and Europe [
12,
13]. This highlights the need for system responsiveness to be coupled with
targeted equity instruments, such as community-based navigator programs, culturally competent care, and outcome-linked reimbursements [
17].
6.4. Limitations and Policy Implications
While Alberta's fiscal data is relatively rich [
3,
15], limitations include:
Absence of real-time price elasticity estimates;
Lack of patient-reported outcomes; and
Single-year analysis frame.
Nonetheless, the province offers a compelling case study of how market dynamics can be shaped by non-price instruments, such as awareness campaigns, virtual access, and targeted public subsidies. Future studies should investigate cost-effectiveness and long-term utilization trends using patient-level longitudinal data.
7. Policy Implications and Recommendations
The findings of Alberta's COVID-19 mental health system response offer actionable insights into long-term policy development. The following recommendations reflect core systemic priorities:
Addressing Alberta's rural and regional workforce shortages requires a targeted investment in human capital. Strategic actions include the following.
Expanding mental health training programs with rural placement incentives;
Offering student loan forgiveness, relocation stipends, and retention bonuses;
Supporting continuous professional development and mental health specialization pathways.
By reinforcing frontline capacity in underserved areas, Alberta can reduce geographic inequities in service availability [
3,
15].
Telehealth proved instrumental during the pandemic, but now requires structural reinforcement.
Continued broadband expansion, particularly in northern and rural communities;
Standardized training for providers in virtual mental health delivery;
Patient-centered education to improve digital literacy and uptake.
These actions ensure equitable access and prevent digital exclusion from becoming a new social determinant of mental health [
2,
3,
8].
To maintain momentum post-COVID, Alberta must explore blended financing options:
Public-private partnerships (PPPs) can bring innovation, flexibility, and supplemental capital.
Integration of private telehealth firms into provincial frameworks may expand access without duplicating infrastructure;
Community-corporate collaborations can support recovery-oriented programming in non-clinical settings.
Sustainable funding mitigates reliance on short-term government stimuli and supports long-term scalability [
16].
The province's million-dollar investment in Indigenous mental health services is a promising start [
3,
15]. Further actions should include the following.
Co-designed programs rooted in traditional healing and trauma-informed care;
Expansion of Indigenous-led provider networks and training;
Meaningful consultation and shared governance with First Nations, Métis, and Inuit communities.
Proper cultural safety requires systems that not only accommodate but also center on Indigenous knowledge and perspectives.
Advanced analytics and integrated health data systems are critical for adaptive policy:
Use real-time dashboards to monitor access, equity, and outcome metrics;
Link service utilization data with demographic variables to fine-tune interventions;
Evaluate programs using cost-effectiveness and long-term return on investment models.
Data infrastructure enables policymakers to iterate quickly and transparently, thereby building trust with the public [
7,
15].
Sustained investment in population-targeted awareness campaigns will:
Normalize help-seeking behavior across age, gender, and cultural groups;
Reduce delays in intervention through early recognition and destigmatization;
Promote awareness of available services, including CASA, VODP, and community recovery programs.
Campaigns should be co-designed with stakeholders who have lived experience to maximize authenticity and impact [
1,
2].
8. Conclusion
Alberta's mental health response during the COVID-19 pandemic demonstrates how targeted public investment can stabilize service markets under crisis conditions. Programs such as CASA and VODP have expanded access while maintaining price neutrality, showing the effectiveness of combining supply- and demand-side interventions.
This case study contributes to the health economics literature by illustrating how policy tools such as telehealth infrastructure, workforce development, and public awareness correct market failures without imposing user costs. Alberta's model offers transferable insights into other jurisdictions that navigate mental health system challenges.
To sustain these gains, future efforts should focus on equity-driven expansion, stable funding mechanisms, and long-term workforce retention, particularly in rural and underserved communities. With strategic investment and data-driven oversight, Alberta is well positioned to lead the design of scalable and inclusive mental health systems.
9. Limitations and Future Research
Although this study offers valuable insights into Alberta's mental health system response during the COVID-19 crisis, it has several limitations.
9.1. Data Limitations
Our analysis relied heavily on publicly available government reports, particularly the 2023–2024 Alberta Mental Health and Addiction Annual Report [
3]. Although this source provides comprehensive administrative data, it lacks granularity in terms of the
Patient-level outcomes (e.g., satisfaction, clinical improvement);
Real-time utilization rates stratified by sociodemographic variables (e.g., age, income, and ethnicity)
Cost-effectiveness estimates across programs.
Additionally, key economic parameters such as the price elasticity of demand, marginal cost per service type, and long-term system savings were either unavailable or approximated using national-level proxies [
4,
16].
9.2. Generalizability
Although Alberta's decentralized, publicly funded model provides a unique case study, the findings may not be directly applicable to other provinces or countries.
Centralized governance (e.g., Ontario),
Mixed public-private systems (e.g., the United States),
Alternatively, differing insurance structures (e.g., EU member states).
Thus, the transferability of this model requires an adaptation based on contextual governance, fiscal capacity, and health infrastructure.
9.3. Equity Evaluation Gaps
Although the study emphasizes rural, youth, and indigenous access, the absence of disaggregated equity outcome data limits precise evaluation of the impact. For instance:
9.4. Short-Term Focus
The study focused on a single fiscal year (2023–2024), which restricts the longitudinal inference. Key unknowns include:
Whether service utilization trends are sustained after the crisis;
Whether initial investments generate long-term economic savings (e.g., reduced emergency room visits and improved employment outcomes)
The extent to which workforce expansions are retained or eroded over time.
9.5. Modeling Assumptions
Our supply–demand framework used theoretical economic models with simplified assumptions:
Price neutrality was inferred from the policy design (i.e., no co-payments), but it has not been empirically tested.
Uniform service quality was assumed across both rural and urban settings, although variations in delivery were likely to exist.
Triage effectiveness as a moral hazard control was assumed but not quantitatively verified.
Although reasonable for system-level modeling, these assumptions underscore the need for more rigorous empirical validation.
9.6. Future Research Directions
To address these limitations and guide future policymaking, we propose the following research avenues:
Longitudinal evaluations that calculate return on investment (ROI) for Alberta's interventions (e.g., VODP, CASA, and recovery communities) using patient-level data are essential to justify continued funding.
- 2.
Equity Audits and Disparity Mapping
Future studies should integrate geospatial and demographic data to track service gaps across rural, indigenous, and low-income populations. Equity dashboards, modeled after Ontario's Center of Excellence [
7], may enhance real-time tracking.
- 3.
Behavioral Outcomes Research
Mixed-methods studies that incorporate the perspectives of youth, families, and providers can effectively evaluate the social and psychological impact of key programs.
- 4.
Workforce Retention Studies
Investigating burnout, career longevity, and geographic mobility of newly recruited mental health workers can inform future labor policies and incentive schemes.
- 5.
Digital Access and Literacy
With the expansion of telehealth, studies should assess digital exclusion risks, particularly among seniors, low-income groups, and remote communities, to inform infrastructure planning and training programs that effectively address these risks.
- 6.
Comparative Provincial/International Policy Evaluation
Systematic comparisons with jurisdictions such as Ontario, Australia, and the UK could elucidate the best practices in crisis-responsive mental health system design.
Author Contributions
Conceptualization: Kola Adegoke, Abimbola Adegoke; Methodology: Deborah Dawodu, Ayoola Bayowa, Temitope Kayode; Investigation: Ayoola Bayowa, Deborah Dawodu, Akorede Adekoya; Writing – Original Draft: Kola Adegoke; Writing – Review & Editing: Abimbola Adegoke; Temitope Kayode; Mallika Singh; Visualization: Temitope Kayode; Ayoola Bayowa; Supervision: Abimbola Adegoke; Project Management: Kola Adegoke; Resources: Akorede Adekoya, Mallika Singh; Data Curation: Deborah Dawodu, Temitope Kayode, and Mallika Singh; The authors have all read and approved of the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgment
The authors gratefully acknowledge Dr. Adam Block, Ph.D., Associate Professor of Health Policy and Management at New York Medical College, for his expert guidance and encouragement. This manuscript originated as an academic assignment and was inspired by Dr. Block’s constructive feedback and mentorship. His insights significantly contributed to the expansion of the work into a broader research collaboration, enriching its analytical depth.
Ethical Statements
No ethical approval was required.
Data Availability Statement
No datasets were generated or analyzed during the current study.
Plain Language Summary (English)
During the COVID-19 pandemic, mental health needs in Alberta rose sharply. In response, the government expanded services through virtual care, youth programs, such as CASA, and recovery communities. This helped meet the rising demand without increasing costs. Our study demonstrates that Alberta effectively balances service access and affordability by investing in both supply and demand. Programs, especially those targeting rural areas, youth, and indigenous populations, have helped; however, some gaps remain. Alberta's approach offers valuable lessons for other regions: funding must be sustained, services must be culturally inclusive, and digital access must be improved to ensure fairness and equity.
Résumé en langage clair (Français):
endant la pandémie de COVID-19, les besoins en santé mentale ont fortement augmenté en Alberta. Le gouvernement a réagi en élargissant les services, notamment les soins virtuels, les programmes pour les jeunes (comme CASA) et les centres de rétablissement. Cela a permis de répondre à la demande sans augmenter les coûts. Notre étude montre qu'Alberta a bien équilibré l'accès aux soins et leur accessibilité financière. Les programmes ont particulièrement aidé les populations rurales, les jeunes et les communautés autochtones, même si des inégalités subsistent. L’approche de l’Alberta peut servir de modèle à d’autres régions : il faut un financement durable, des services inclusifs sur le plan culturel et un meilleur accès au numérique pour garantir l’équité.
Ethical Statement
This study did not involve human or animal subjects; therefore, ethical approval was not required.
Consent Statement
Not applicable, as the study does not involve individual participants.
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- Talarico, F. Impact of the COVID-19 Pandemic on Developmental Vulnerabilities and Mental Health: Implications for Children and Adolescents in Alberta Using an Evidence Synthesis Approach [PhD dissertation]. University of Alberta; 2024. Available from: https://era.library.ualberta.ca/items/a6203b55-8e11-4f25-8a3b-cd9174c9d544.
- Russell, M.J.; Urichuk, L.; Parker, N.; Agyapong, V.I.O. Youth mental health care use during the COVID-19 pandemic in Alberta, Canada: an interrupted time series, population-based study. Child Adolesc Psychiatry Ment Health. 2024. [CrossRef]
- Government of Alberta. 2023–24 Mental Health and Addiction Annual Report. Edmonton: Alberta Health; 2023. Available from: https://open.alberta.ca/dataset/610118c0-60ce-4ca1-9ef6-16fa703e46b7/resource/f43fcaad-bd2b-42e9-a7b4-657000baff95/download/mha-annual-report-2023-2024.pdf.
- Folland, S.; Goodman, A.C.; Stano, M.; Danagoulian, S. The economics of health and health care. 9th ed. Abingdon: Taylor & Francis; 2024. p. 275–309. Available from: https://doi.org/10.4324/9781003308409. [CrossRef]
- Talarico, F. Impact of the COVID-19 Pandemic on Developmental Vulnerabilities and Mental Health: Implications for Children and Adolescents in Alberta Using an Evidence Synthesis Approach [PhD dissertation]. University of Alberta; 2024. https://era.library.ualberta.ca/items/a6203b55-8e11-4f25-8a3b-cd9174c9d544.
- Tulchinsky, T.H.; Varavikova, E.A. Health technology, quality, law, and ethics. Public Health Reviews. 2014. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7171898/.
- Ontario Ministry of Health. Mental Health and Addictions Centre of Excellence: 2023 Operational Overview. Government of Ontario; 2023. Available from: https://www.ontario.ca/page/mental-health-and-addictions-centre-excellence.
- 8. Robinson, L.; Parsons, C.; Northwood, K.; Siskind, D.; McArdle, P. Patient and clinician experience of using telehealth during the COVID-19 pandemic in a public mental health service in Australia. Schizophr Bull Open. 2023;4(1):sgad016. [CrossRef]
- Shi, L.; Singh, D.A. Essentials of the US Health Care System. 6th ed. Burlington, MA: Jones & Bartlett Learning; 2022. Available from: Google Books.
- NHS Confederation. Mental Health Services and COVID-19: Policy and Practice Review. London: NHS Confederation; 2022. Available from: https://www.nhsconfed.org/publications/mental-health-services-and-covid-19.
-
Manning, W.G.; Newhouse, J.P.; Duan, N.; Keeler, E.B.; Benjamin, B.; Leibowitz, A.; et al.Health insurance and the demand for medical care: evidence from a randomized experiment. Santa Monica (CA): RAND Corporation; 1988. Report No.: R-3476-HHS. Available from: https://www.rand.org/content/dam/rand/pubs/reports/2005/R3476.pdf.
- Kohn, R.; Ali, A.A.; Puac-Polanco, V.; Figueroa, C.; López-Soto, V.; Morgan, K.; et al. Mental health in the Americas: an overview of the treatment gap. Rev Panam Salud Publica. 2018;42:e165. [CrossRef]
- Zigante, V.; Hodin, M.; Muir, T. Inequalities in access to mental health services across the EU: Evidence and policy responses. Brussels: European Commission; 2022.
- Solmi, M.; Estradé, A.; Thompson, T.; Agorastos, A.; Radua, J.; Cortese, S.; et al. Physical and mental health impact of COVID-19 on children, adolescents, and their families: The Collaborative Outcomes study on Health and Functioning during Infection Times - Children and Adolescents (COH-FIT-C&A). J Affect Disord. 2022;299:367–79. Available from: https://www.sciencedirect.com/science/article/pii/S0165032721010491.
- Alberta Health Services. 2022–2023 Annual Report. Edmonton: AHS; 2023 [cited 2025 Jul 25]. Available from: https://www.albertahealthservices.ca/assets/about/publications/ahs-pub-pr-2022-23-q4.pdf#page=41.
- Canadian Mental Health Association. Federal Plan for Universal Mental Health & Substance Use Health: Background Paper. Ottawa: CMHA; 2022 [cited 2025 Jul 25]. Available from: https://cmha.ca/wp-content/uploads/2022/11/AfMH-White-Paper-EN-FINAL.pdf.
- World Health Organization. Mental health preparedness and response for the COVID-19 pandemic. Geneva: WHO; 2020. Available from: https://apps.who.int/gb/ebwha/pdf_files/EB148/B148_20-en.pdf.
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–98. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).