1. Introduction
One of the most effective orthopaedic operations done today for individuals experiencing pain from a range of ailments is total knee arthroplasty (TKA). The knee joint is well exposed via the medial parapatellar approach. For complete knee replacement, the medial parapatellar approach has been the accepted method. Von Langenbeck described the medial parapatellar approach in 1878, however the optimal surgical method is still up for debate.
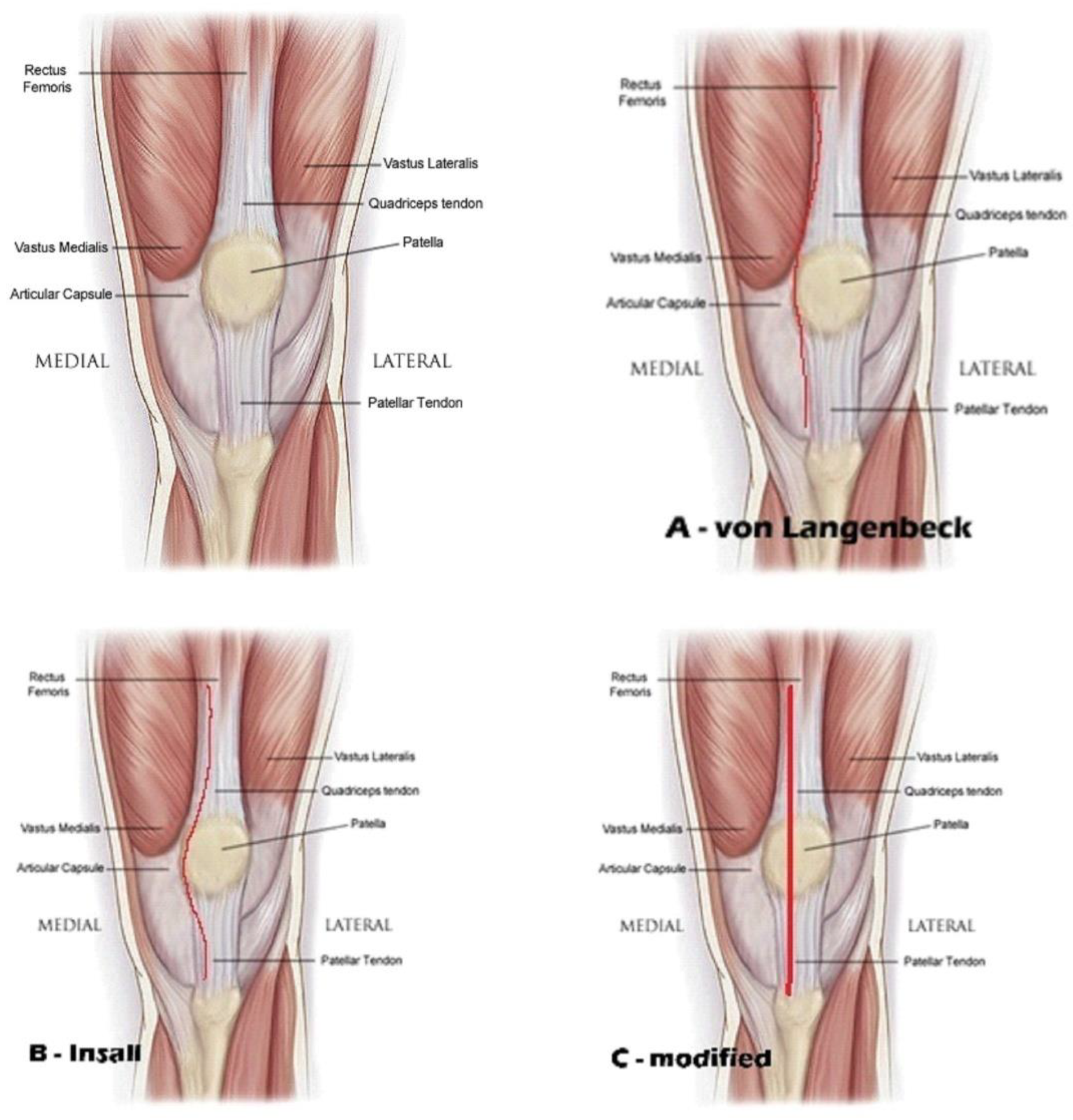
In order to reconstruct the medial joint capsule, von Langenbeck explained the procedure, which left a cuff of tissue on the patella and followed the medial boundary of the quadriceps tendon [
1]. One critique of this strategy was that it upset the quadriceps mechanism at the point where the quadriceps tendon and vastus medialis meet, which led to the patella being unstable.
A variant of this technique was reported by Insall in 1971, which entailed severing the quadriceps tendon at the junction of the medial third and lateral two-thirds [
2]. But the cuff that would be utilized for repair was blocked by the cut, which ran along the medial border of the patella.
Nevertheless, the method has been connected to instances of stress fractures, dislocation, subluxation, and patella fragmentation brought on by avascular necrosis (Mochizuki 1979; Moreland 1988) [
3,
4].
We modified this medial approach, by making an incision at the internal border of the quadriceps tendon leaving 3-4 mm on internal side, peeling from patella almost half of fibrous - tendinous part and continue on the patella tendon leaving 3-4 mm on internal side. We repair the medial joint capsule and the continuity of the extensor mechanism by two or three bone tunnels on the patella to reinsert the tendinous peeling from the patella, we name this - transtendinous approach of the extensor mechanism in TKA. (
Figure 1)
Figure 1.
Medial parapatellar arthrotomy A - von Langebeck B – Insall C - modified.
Figure 1.
Medial parapatellar arthrotomy A - von Langebeck B – Insall C - modified.
This medial technique is reproducible in primary and revision arthroplasty and could be used in early revisions as well, despite the recent development of minimally invasive techniques to lessen soft tissue damage and enable a speedy recovery [
5,
6]. The variations in the damage site demonstrate the biological mechanisms governing tendon injury and repair [
7].
2. Objectives
To establish the rate of complications and differences between the classical medial approach and the modified approach of the extensor mechanism in TKA.
3. Background
The global demand for knee replacement surgeries is increasing due to factors such as an ageing population, increased obesity, and knee traumatic disorders.
The number of primary knee arthroplasties performed worldwide is increasing from year to year, and so are the complicated cases with severe deformity of varus-valgus (more than 15 degrees), osteoporotic bone structure, or large preexisting defect. High load forces applied to the tibial component of a primary TKA may cause aseptic loosening and implant failure too soon. In these cases, a tibial stem added to the implant can dissipate the implant-bone stress levels reducing the risk of failure.
The incidence of peri-prosthetic joint infection (PJI) is high, and there is an increase in revisions.
We have tried to reduce complications in TKA in three directions. 1. The patelloplasty complications using the new approach. 2. To disperse stresses and increase implant stability in situations of severe deformity by adding a tibial stem extension. 3. Reducing the number of septic failures.
4. Methods
1. We tried to diminish the complications related to patelloplasty through this modified approach.
This study was carried out after 14 February 2017. After the approval from the hospital's institutional review board and the Hospital's Ethics Committee, the entire study begins. This study respect the principles set out in the Helsinki Declaration.
Since 2017, we have made changes to the traditional medial approach – and we named this the transtendinous approach of the extensor mechanism in TKA. The incision begins at the internal border of the quadriceps tendon, leaving 3–4 mm on the inside. It then peels off nearly half of the fibrous and tendinous portion of the patella and continues on the patella tendon, leaving 3–4 mm on the inside. We repair the medial joint capsule and the continuity of the extensor mechanism by two or three bone tunnels on the patella to reinsert the tendinous peeling from the patella.
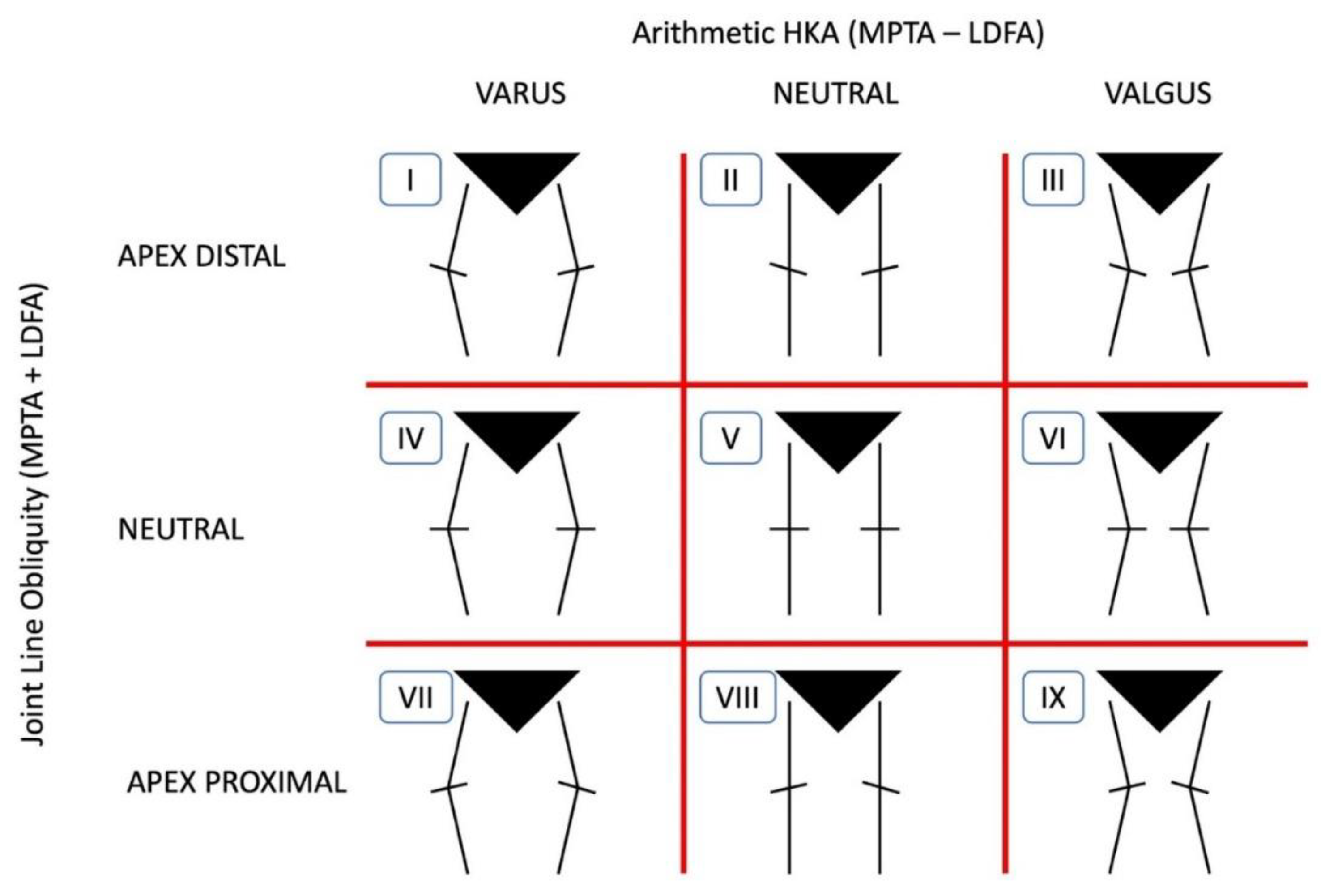
Figure 2.
- 9 types of knee phenotypes based on HKA and JLOA Mac Dessi, Bellemans JBJS 2021.
Figure 2.
- 9 types of knee phenotypes based on HKA and JLOA Mac Dessi, Bellemans JBJS 2021.
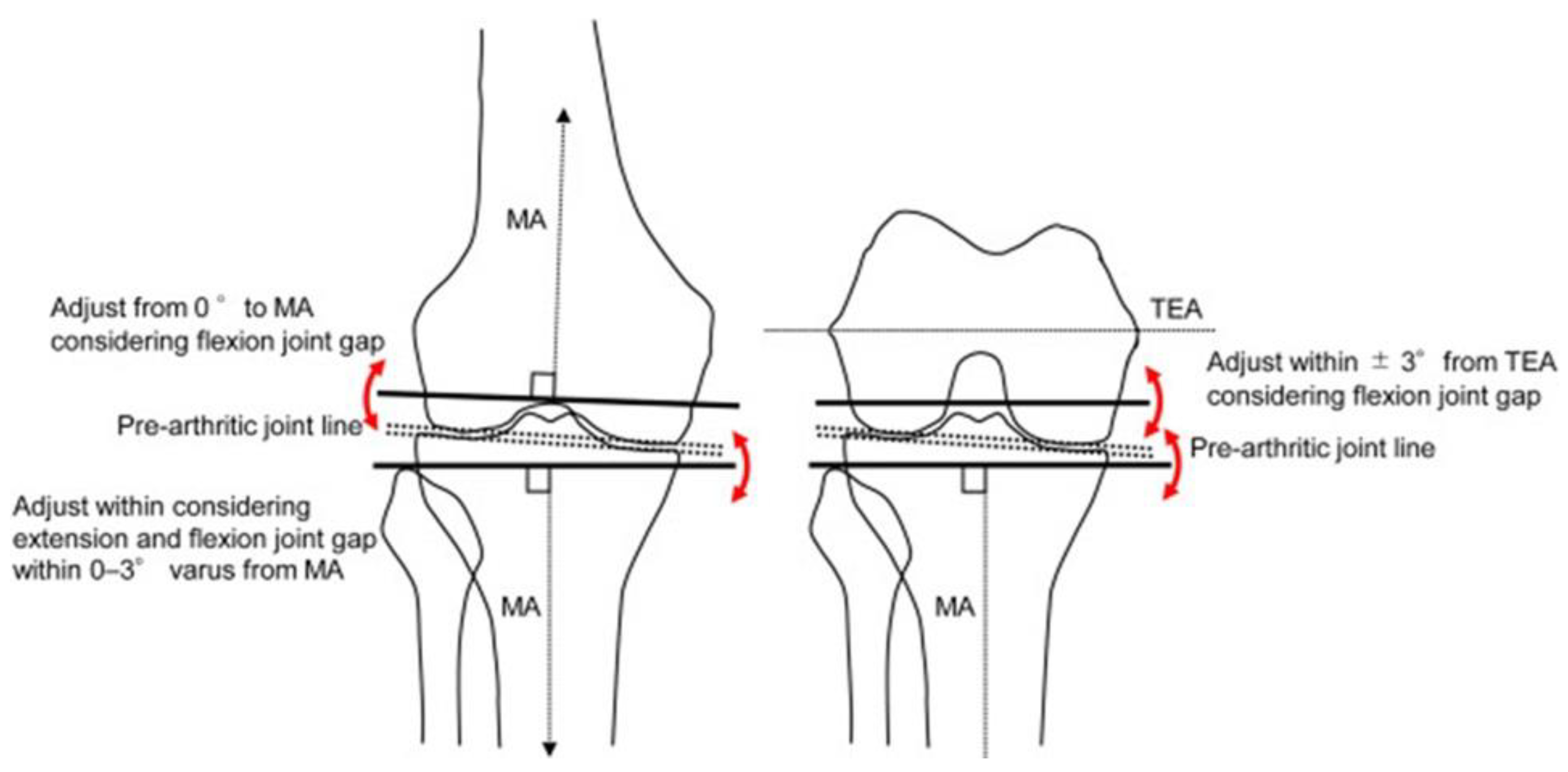
We denervate the patella instead of resurfacing it. We also do osteophyte resection instead of patelloplasty. The functional alignment was employed (
Figure 3). We envisioned the modified approach strategy with the goal of lowering patellar problems. For this reason, we contrasted our results using the modified approach with those of the other authors' publications.
The classification described by Mac Dessi et al. is well known regarding the constitutional knee phenotypes using the Coronal Plane Alignment of the Knee (CPAK) (
Figure 2) [
8].
Figure 3.
Functional alignment.
Figure 3.
Functional alignment.
2. In cases of severe deformity, a tibial stem extension is added to distribute the forces and improve the stability of the implants.
Since 2017, we have used this modified method on 706 TKA patients, including 302 females and 281 males. Their ages ranged from 45 to 78. Eighty of those 706 TKA cases had severe deformities, such as large preexisting defects, osteoporotic bone structure, or severe varus-valgus deviation. A tibial stem extension was added to the regular prosthesis to dissipate the stress levels, reducing the risk of failure in severe knee deformity.
Only 38 out of 80 tibial stem extension in primary TKA, had varus deformity, more than 15°, 25 had valgus deformity, 10 had severe osteoporosis, 4 rheumatoid arthritis with osteoporotic bone structure and 3 had previous proximal correction osteotomy or callus deformity. The same type of implants was used with or without tibial stem extension. Stem lengths varied from 80 mm to 140 mm.
The participants were assessed via the Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire, Visual Analogue Scale (VAS) and the Forgotten Joint Score (FJS) at their last follow-up visit, three years postoperatively.
3. To cut down on the frequency of catastrophic septic failures.
We tried to reduced the septic complications in TKA. The septic failure are devastating. The incidence of peri-prosthetic joint infection (PJI) varies from 0.3% to 2,7% in primary knee replacements, and it can reach 10% in revision procedures. Both surgical and patient characteristics, including age, body mass index (BMI), co-morbidities, and lifestyle, are associated with the likelihood of surgical site infection (SSI) and pressure soreness (PJI). Pre-operative patient bacterial decolonization, screening and prevention of anemia, peri-operative patient warming, skin antisepsis, povidone-iodine wound lavage, and antibacterial coated sutures are all important components of a multifaceted strategy to lower the risk of SSI in primary hip and knee arthroplasty. [
15,
16]
To reduce them, we adopt a protocol which includes the selection of patients, MSSA decolonisation, laminary flow, dedicated OR rooms, blood management, the use of tranexamic acid locally and i.v., tourniquets, clean surgery, a well-trained surgeon team, local administration of 1 g of vancomycin injected intraosseous, three-minute lavage with 3.5% povidone-iodine of primary TKA wounds prior to closure, and the use of active drainage.
Antibiotic prophylaxis: Cephalosporins, 1st generation (Cefazolin), and Vancomycin (for MRSA cases) – only 24 hours; in alergic cases Clindamycin 600 mg / 8 hours + cipro 400mg / 12 hours.
5. Results
We compared the results with other studies regarding the patellar complications in total knee arthroplasty.
Commonly observed complications of the patellofemoral joint are crepitation, subluxation, excessive wear, loosening, and persistent patient discomfort. These complications have been attributed to inadequate prosthetic design, fixation techniques, anatomic abnormalities, and surgical error [
9,
10,
11,
12,
13,
14].
We have operated on 706 TKAs on 583 patients, 302 females and 281 males. Their ages ranged from 45 to 78.
Eighty of those 706 TKA cases had severe deformities, such as large preexisting defects, osteoporotic bone structure, or severe varus-valgus deviation. The same type of implants was used with or without tibial stem extension. Stem lengths varied from 80 mm to 140 mm.
Patients using the medial modified approach have not experienced any avascular necrosis, stress fractures, or patellar dislocation or subluxation.
A radiographic evaluation revealed two cases of tibial implant loosening, in the lot with standard components. The average pain and function scores at the time of assessment were 85 and 83, respectively. On average, the range of motion was 110° at the last follow-up. Kaplan-Meier survivorship was 98.6% at 7 years. There were no significant differences in VAS score, WOMAC, FJS or OKS.
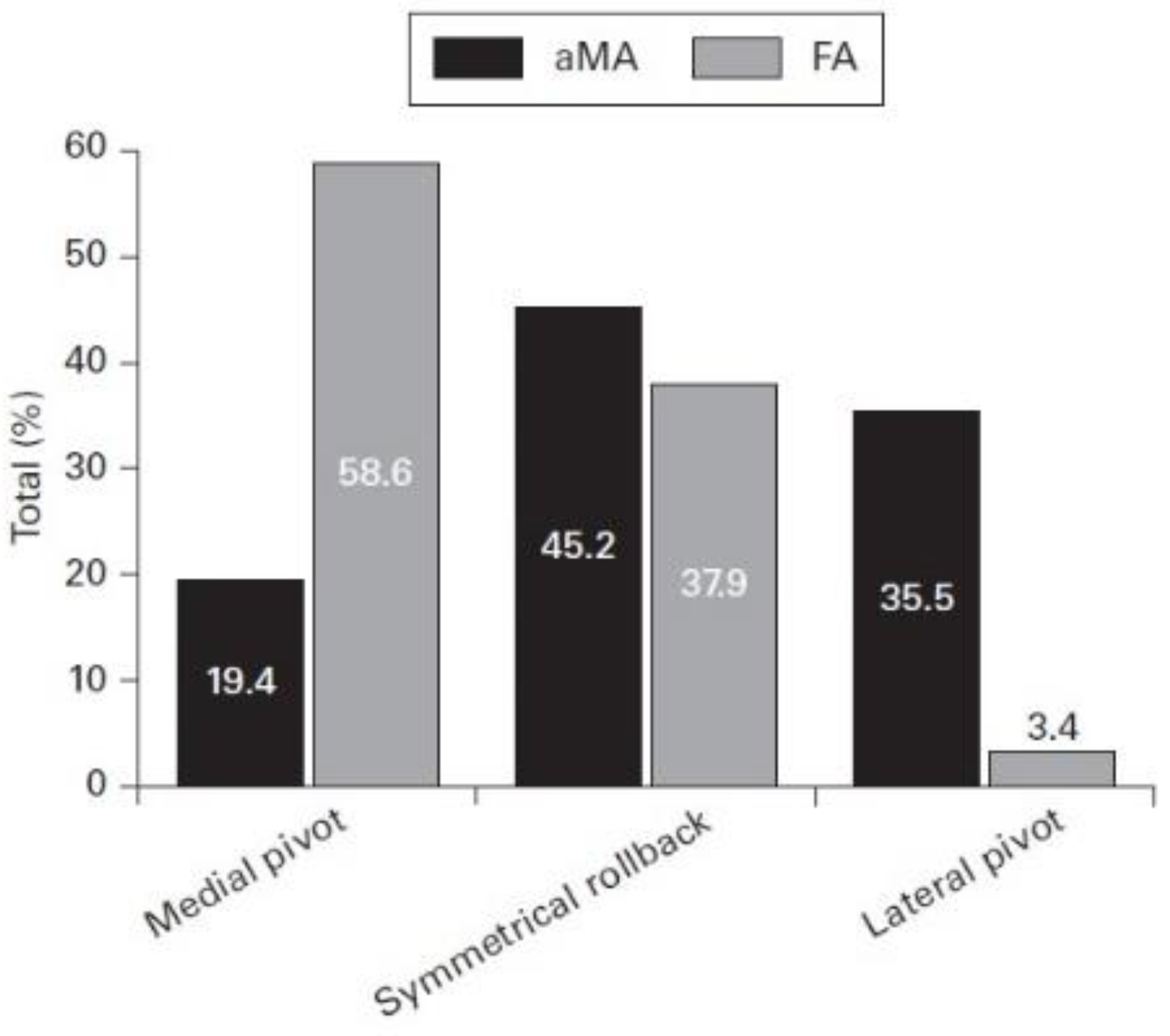
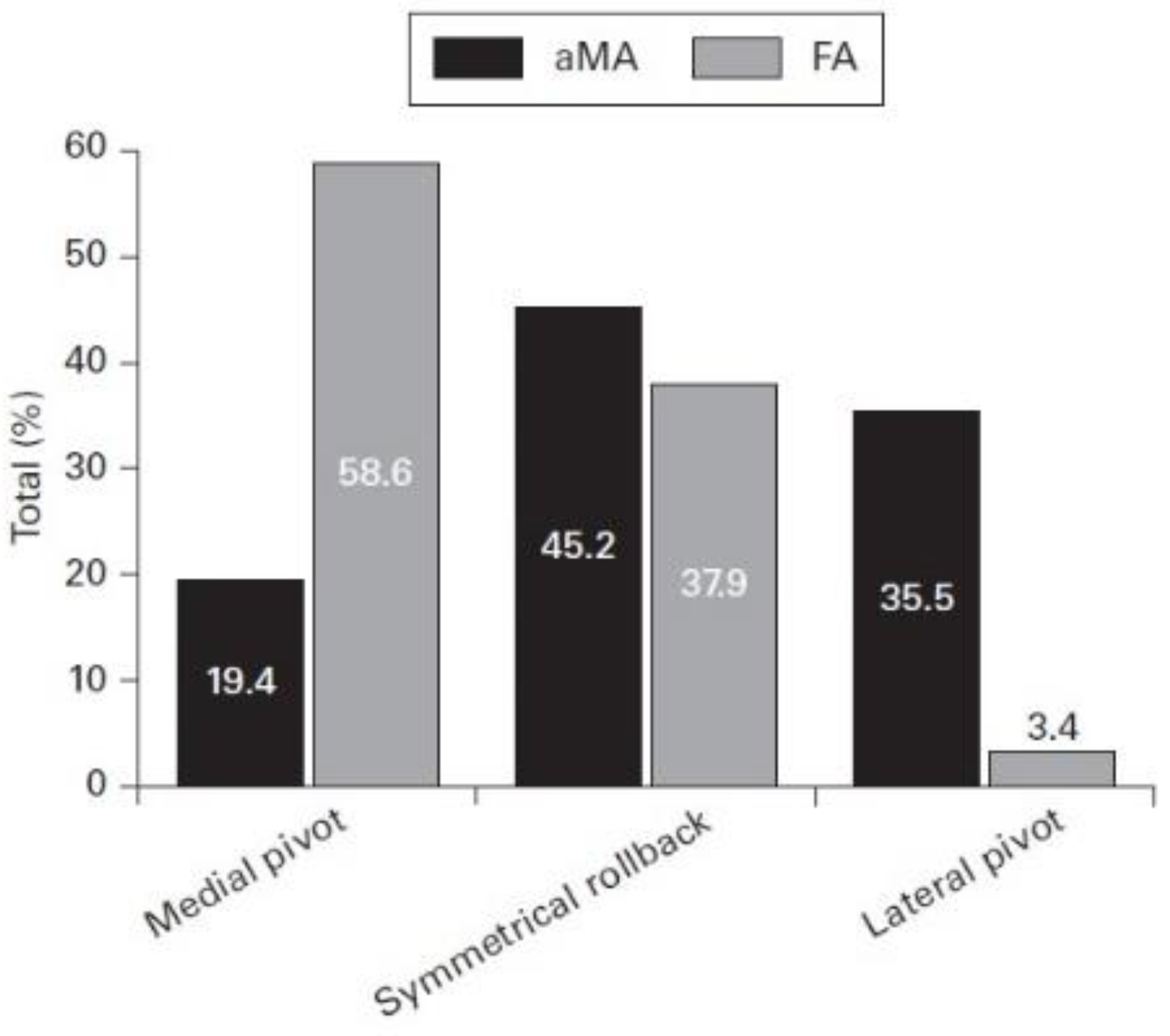
Other recent studies confirm the right choice of functional alignment. This study presents the biomechanical results of functional alignment (FA) in 29 cases, comparing with adjusted mechanical alignment (aMA) (n = 31) of 60 consecutive patients randomised to a robotically assisted TKA. Functional alignment (FA-TKA) produced a medial pivot in 58.6% of cases (17/29), symmetrical rollback in 37.9% (11/29), and a lateral pivot in 3.4% (1/29). In patients with an adjustment mechanical alignment (aMA-TKA), 19.4% (6/31) produced a medial pivot, 45.2% (14/31) had symmetrical rollback, and 35.5% (11/31) had a lateral pivot (p < 0.001, chi-squared test) [
17] (
Figure 4).
Figure 4.
Kinematic pattern by alignment group. aMA, adjusted mechanical alignment; FA, functional alignment.
Figure 4.
Kinematic pattern by alignment group. aMA, adjusted mechanical alignment; FA, functional alignment.
We illustrate here a primary case of TKA with valgus deformity on right knee, varus deformity on left knee - who necessitates the use of revision components with tibial stem extension with offset. (
Figure 5).
Figure 5.
Primary TKA with revision components tibial stem extension and offset, X-ray and clinical result.
Figure 5.
Primary TKA with revision components tibial stem extension and offset, X-ray and clinical result.
1. Another case with a 34° varum deformity that was treated by primary TKA with tibial stem extension is shown here. Intraoperative and postoperative X-rays are included (
Figure 6).
Figure 6.
X-rays taken during and after surgery show a significant deformity of 34° of varus that was corrected by a primary TKA with revision components.
Figure 6.
X-rays taken during and after surgery show a significant deformity of 34° of varus that was corrected by a primary TKA with revision components.
There were nine cases of sepsis. Our septic incidence was 1.27%, which was less than the 2.7% reported in other countries. [
15,
16]
Five of these needed an early septic revision at 15 – 24 days after surgery. Four cases necessitated two stages revisions. The technique makes the surgery easier in those septic situations, using the same soft tissue approach.
For the early revision cases treated by retention of implants with polyethylene insert change, antibiotic association was administered i.v. for 2 weeks followed by 10 weeks of oral antibiotics with antibiofilm activity. The mobile part of implants was changed.
The late cases revision necessitate a two-stage exchange, explantation debridement and a mobile spacer with antibiotics, followed by 2 weeks of i.v. antibiotic association without antibiofilm activity, implantation of a revision implant, followed by 2 weeks of i.v. antibiotic association without antibiofilm activity and finally 8 weeks of oral antibiotics with antibiofilm activity.
6. Discussions
We have tried to reduce complications in TKA in three directions. 1. The difficulties associated with patelloplasty with the modified method. 2. To disperse stresses and increase implant stability in situations of severe deformity, a tibial stem extension is inserted. 3. To lessen the frequency of catastrophic septic breakdowns.
We tried to reduce the complications related to patellar prosthetics through this approach.
The difference between the two surgical methods essentially concerns the patellar complications in TKA. The two procedures differ in that the patellar tendinous-fibrous tissue is peeled and then reinserted through bone tunnels. This approach is entirely through the tendinous-fibrous tissue, and the healing of that tissue is improved compared to the classical approach. A continuity of incision through the tendinous tissue of the quadriceps and patellar tissue confers the repair of that.
We repair the medial joint capsule and the continuity of the extensor mechanism by two or three bone tunnels on the patella to reinsert the tendinous peeling from the patella.
That is why we focused on studies that follow the complications of patellar prosthesis. Patellofemoral joint problems include loosening, excessive wear, subluxation, crepitation, and ongoing patient discomfort. These issues have been linked to surgical mistake, anatomic anomalies, poor fastening methods, and poor prosthetic design [9-13].
Obesity (body mass index >30 is associated with a 1.7-fold increase in fracture risk and a 6.3-fold increase in loosening risk), patellar thickness <18 mm, patellar tilting or subluxation, and valgus greater than 10° are risk factors for patellar complications [
14].
The risk of complications may be associated with surgery; when resurfacing is done, a thin patella raises the risk of fracture and osteonecrosis. Also, an asymmetric bone cut or lateral retinacular release could determine fracture, loosening, and pain. Femoral and/or tibial rotational malalignment increases the risk of patellar instability [
14].
Decisions to perform revision surgery for patello-femoral complications must be convincingly documented, with identification of the cause of the complication. When no cause is identified, non-operative treatment is the best option, given the uncertain outcomes of the various available surgical procedures [
10].
Additional research may be required in the future to compare the histological variations in healing between the two methods. Biomechanical variations were also discernible.
The number of primary knee arthroplasties performed worldwide is increasing from year to year, and so are the complicated cases with severe deformity of varus-valgus (more than 15 degrees), osteoporotic bone structure, or large preexisting defect. High load forces applied to the tibial component of a primary TKA may cause aseptic loosening and implant failure too soon. In these cases, a tibial stem added to the implant can dissipate the implant-bone stress levels, reducing the risk of failure.
To lower the risk of failure in difficult cases with severe deformity, a tibial stem extension was added to the standard prosthesis to distribute the stress levels. The tibial stem extension increases the stability of the implants.
Eighty of those 706 TKA cases had severe deformities, such as large preexisting defects, osteoporotic bone structure, or severe varus-valgus deviation. This modified approach permit us to correct also these severe diformities. The same type of implants was used with or without tibial stem extension. Stem lengths varied from 80 mm to 140 mm.
Radiographic evaluation reported 2 cases of tibial implant loosening in the lot with standard components. The average pain and function scores at the time of assessment were 85 and 83. Average range of motion was 110° at the latest follow-up, respectively. Kaplan-Meier survivorship was 98.6% at 7 years. No significant difference in VAS score, WOMAC, FJS, or OKS.
The preoperative planning is mandatory, but the final decision will be intraoperatively whether to use tibial stem extension or not in total knee arthroplasties with severe deformity. Tibial stem extension must be used in osteoporotic or large preexisting bone defects in severe varus-valgus deformities. The stem length and diameter must be precisely chosen carefully to diminish the failure rates. The clinical results support the use of stems in difficult primary total knee arthroplasties. To determine the diameter and length of the components' extensions that are most suited for the patient, more research might be needed in the future.
The septic failure are devastating. The incidence of peri-prosthetic joint infection (PJI) varies from 0.3% to 2,7% in primary knee replacements, and it can reach 10% in revision procedures. The risk of surgical site infection (SSI) and pressure soreness (PJI) is correlated with both surgery and patient variables, such as age, body mass index (BMI), co-morbidities, and lifestyle.
A comprehensive approach to reducing the risk of surgical site infections (SSI) in primary hip and knee replacements should include pre-operative patient bacterial decolonization, screening and prevention of anemia, peri-operative patient warming, skin antisepsis, povidone-iodine wound lavage, and antibacterial coated sutures. [15, 16]
To reduce them, we adopt a protocol which includes the selection of patients, MSSA decolonisation, laminary flow, dedicated OR rooms, blood management, the use of tranexamic acid locally and i.v., tourniquets, clean surgery, a well-trained surgeon team, local administration of 1 g of vancomycin injected intraosseous, three-minute lavage with 3.5% povidone-iodine of primary TKA wounds prior to closure, and the use of active drainage.
Antibiotic prophylaxis: Cephalosporins, 1st generation (Cefazolin), and Vancomycin (for MRSA cases) – only 24 hours; in alergic cases Clindamycin 600 mg / 8 hours + cipro 400mg / 12 hours.
7. Conclusions
This modified approach is reproducible, gives a large exposure and allows even the revisions through the same approach. The recovery is good due to the tendinous healing.
There were no differences between the modified and classical methods, but in our 706 TKA, there were no patellar complications. We have not experienced any avascular necrosis, stress fractures, or patellar dislocation or subluxation.
Preoperative planning is mandatory, but the final decision will be intraoperative to use or not use tibial stem extension in total knee arthroplasties with severe deformities. This modified approach is useful even in severe knee deformity allowing tibial stem extension. Tibial stem extension is recommended for severe deformities, osteoporotic conditions, and large pre-existing bone defects. The diameter and length of the stem must be selected to reduce the failure rate. The stem length and diameter must be precisely chosen carefully to diminish the failure rates. The clinical findings lend credence to using stems in challenging primary total knee replacements.
The clinical results support the use of stems in difficult primary total knee arthroplasties. To determine the diameter and length of the components' extensions that are most suited for the patient, more research might be needed in the future.
Our protocol that includes patient selection, MSSA decolonisation, laminar flow, dedicated operating rooms, blood management, administration of tranexamic acid locally and intravenously, tourniquets, clean surgery, a team of skilled surgeons, intraosseous injection of 1 g of vancomycin, lavage of primary TKA wounds with 3.5% povidone-iodine for 3 minutes before closure, and active drainage reduces septic failure in TKA.
Our septic incidence was 1.27%, which was less than the 2.7% reported in other countries. Using the same soft tissue approach, the procedure facilitates the surgery in certain sepsis circumstances.
8. Future Directions
Additional research may be required in the future to compare the histological variations in healing between the two methods. Biomechanical variations were also discernible.
Future studies could be necessary to determine the diameter and length of the component extensions most suited for the patient. Careful planning and selection are required to ensure that the stem has the proper diameter and length. particular to the patient's malformation.
Additional research may be required in the future to reduce the septic complications in TKA.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions. The following statements “Conceptualization, S.C., M.G. and Fl.G.; methodology, S.C.; software, Fl.G. and V.B.; validation, V.B. and Fl.G.; formal analysis, S.C.; investigation, V.B.; resources, S.C. and Fl.G.; data curation, S.C. and Fl.G.; writing—original draft preparation, S.C.; writing—review and editing, S.C.; visualization, S.C.; supervision, S.C.; project administration, S.C.; funding acquisition, S.C. All authors have read and agreed to the published version of the manuscript.” Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding
None of the authors received funding to realize this article. No funding was received for this article.
Institutional Review Board Statement
In this section, please add the Institutional Review Board Statement and approval number for studies involving humans or animals. Please note that the Editorial Office might ask you for further information. Please add “The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of NAME OF INSTITUTE (protocol code XXX and date of approval).” OR “Ethical review and approval were waived for this study, due to REASON (please provide a detailed justification).” OR “Not applicable.” for studies not involving humans or animals. You might also choose to exclude this statement if the study did not involve humans or animals.
Informed Consent Statement
“Informed consent was obtained from all subjects involved in the study.”. “Written informed consent has been obtained from the patient(s) to publish this paper.”.
Conflicts of Interest
Declare conflicts of interest or state “The authors declare no conflict of interest.”.
References
- Von Langenbeck, B. Zur resection des kniegellenks. Verhandlungen der Deutschen Gesellschaft fur Churg. 1878, 7, 23–30. [Google Scholar]
- Insall, J. A midline approach to the knee. J Bone Jt Surg Am Ed. 1971, 53, 1584–1586. [Google Scholar] [CrossRef]
- Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty Journal of Bone and Joint Surgery; American Edition 1979, 61, 879–83.
- Moreland, JR. Mechanisms of failure in total knee arthroplasty. Clinical Orthopaedics and Related Research 1988, 226, 49–64. [Google Scholar] [CrossRef]
- Khan RJK, Keogh A, Fick DP, Wood DJ. Surgical approaches in total knee arthroplasty Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No.: CD005329. [CrossRef]
- Ștefan Cristea, Vlad Predescu, Șerban Dragosloveanu, Ștefan Cuculici and Nicholas Mărăndici Surgical Approaches for Total Knee Arthroplasty Edited by Vaibhav Bagaria Arthroplasty - A Comprehensive Review USA, 2016 jan pag25 - 47 INTECH. [CrossRef]
- Natalie L. Leong, Jamie L. Kator, Thomas L. Clemens, Aaron James, Motomi Enamoto-Iwamoto, Jie Jiang Tendon and Ligament Healing and Current Approaches to Tendon and Ligament Regeneration Journal of Orthopaedic Research: Volume 38, Issue 1. [CrossRef]
- MacDessi, S. J. , Griffiths-Jones, W., Harris, I. A., Bellemans, J. & Chen, D. B. Coronal plane alignment of the knee (CPAK) classification. Bone Joint J. 2021, 103-b, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Kyung Ah Chun, Kenjirou Ohashi, D. Lee Bennett, and Georges Y. El-Khoury Patellar Fractures After Total Knee Replacement American Journal of Roentgenology, Musculoskeletal Imaging, Volume 185, Issue 3. [CrossRef]
- Sophie Putman, Florian Boureau, Julien Girard, Henri Migaud, Gilles Pasquier, Patellar complications after total knee arthroplasty Orthop Traumatol Surg Res. 2019, 105, S43–S51. [CrossRef]
- Hans-Peter W van Jonbergen, Ashvin V Boeddha, Jos J A M van Raaij Patient Satisfaction and Functional Outcomes Following Secondary Patellar Resurfacing Orthopedics 2016, 39, e850–e856. [CrossRef] [PubMed]
- Angelos Assiotis, Kendrick To, Rhidian Morgan-Jones, Ioannis P Pengas, Wasim Khan Patellar complications following total knee arthroplasty: a review of the current literature. EJOST 2019, 29, 1605–1615. [CrossRef] [PubMed]
- Leblanc, JM. Patellar complications in total knee arthroplasty. A literature review.Orthop Rev. 1989 Mar;18(3):296-304.
- Meding JB, Fish MD, Berend ME, Ritter MA, Keating EM. Predicting patellar failure after total knee arthroplasty.Clin Orthop Relat Res 2008, 466, 2769–74. [CrossRef]
- Philip, F. Dobson, Michael R. Reed EFORT Open Rev 2020, 5, 604–613, www.efortopenreviews.org. [Google Scholar] [CrossRef]
- Peter Sharkey Rothman Inst. Diagnosis and Prevention of Periprosthetic Joint Infections Evidence-Based Clinical Practice Guideline AAOS 2006.
- J. R. Manara, R. J. R. Manara, R. Steer, S. L. Whitehouse, D. Collopy, G. W. Clark Functional alignment restores native kinematics more consistently than mechanical axis alignment in total knee arthroplasty Bone Joint J 2025, 107-B, 423–431. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).