1. Introduction
Cataract is defined as a partial or complete clouding or opacification of the normally transparent lens of the eye or its surrounding capsule [
1]. While initially slow to progress and minimally disruptive, cataracts tends to worsen with age, particularly after the fourth or fifth decade, ultimately interfering with daily functioning [
2]. Cataracts are the leading cause of reversible visual impairment among the elderly worldwide, defined as individuals aged 65 and older [
1,
3]. Nearly half of people in their early 70s and almost all in their 90s develop clinically significant cataracts. According to the National Eye Institute, the overall prevalence of cataracts is 17.1%, with an estimated 38 million individuals expected to be affected by 2030 [
4]. In middle and low-income countries, cataracts account for 50% of all cases of blindness cases, compared to only 5% in high-income regions [
5].
Cataract surgery remains the most effective treatment, with high success rates and significant improvements in vision and quality of life. However, as global life expectancy increases, so does the demand for cataract surgery among older adults, along with the need to better understand and manage age-related surgical risks [
6]. Complications in elderly patients are a growing concern. Intraoperative risks include posterior capsule rupture, floppy iris syndrome, and iris or ciliary body injury [
1,
7]. Postoperative complications range from transient intraocular pressure elevation and corneal edema, to late issues such as posterior capsule opacification, cystoid macular edema, and retinal detachment [
1,
7,
8,
9,
10,
11]. Although uncommon with modern surgical techniques, these complications can significantly impact outcomes and patient quality of life.
Several ocular features have been associated with increased intraoperative risk, including small pupils, white cataracts, unstable capsular bags, and the absence of a red reflex [
12,
13,
14]. Early identification of these factors is essential for preventing complications and optimizing outcomes.
Ethnicity has also been shown to influence cataract prevalence, severity, and surgical outcomes. Disparities in access to care and postoperative results have been reported across ethnic groups [
15]. However, limited data exist on outcomes within multiethnic populations treated within the same healthcare system. A retrospective study conducted at Soroka University Medical Center, Israel (2009–2016), compared cataract surgery outcomes in late elderly patients (mean age 92.6 years) versus middle elderly patients (mean age 75.2 years), revealing more advanced cataracts and worse visual outcomes in the older group [
6]. To date, no similar studies have been carried out at Ziv Medical Center in Safed, which serves a diverse regional population representing various ethnicities from Northern Israel, highlighting the need for localized data to assess potential ethnic disparities in surgical outcomes.
The primary objective of this study is to examine and compare the demographic characteristics, clinical features, and postoperative outcomes of cataract surgery between Jewish and Arab populations in Northern Israel. Specifically, the study aims to assess the prevalence and incidence of postoperative complications and visual recovery within these groups. These findings are intended to provide valuable insights into the burden of cataracts on patients, caregivers, healthcare providers, and the broader health system. By identifying ethnicity-specific differences, this study aims to elucidate ethnicity-specific disparities to advance a nuanced understanding of the determinants influencing cataract surgery outcomes among diverse populations in Israel.
2. Materials and Methods
This single-center, retrospective cohort study underwent cataract surgery between January 1st, 2023 and December 31st, 2023. in the Department of Ophthalmology at Ziv Medical Center, Safed, Israel. Patient data were collected from the hospital’s electronic medical records (EMR) database, including demographic variables (age, sex and ethnicity), ocular and systemic comorbidities, cataract type classification (Nuclear sclerotic (NS), Cortical, and Posterior sub-capsular cataracts), as well as postoperative outcomes (incidence of intraoperative complications, postoperative ocular comorbidities, pre- and postoperative uncorrected (UCVA) and best-corrected distance visual acuity (BCVA)). Inclusion criteria required patients to have no history of prior ocular surgery, a pre-operative best-corrected visual acuity (BCVA) of 6/12 or worse. Exclusion criteria included age less than 60 years, evidence of corneal diseases (e.g., corneal dystrophies, ectasias), glaucoma, or retinal pathologies (e.g., Diabetic Retinopathy, Hypertensive Retinopathy, Retinal Detachment (RD), or Age-related macular degeneration (AMD)) and patients with less than one month of postoperative follow-up.
The patients included in this study represent the complete dataset of cataract surgeries performed during the study period with full available records (
Table 1). Patients were categorized into two ethnic groups, Jewish and Arab, and further stratified by age into three subgroups. This stratification enabled a more detailed comparative analysis of surgical outcomes across different demographic and age groups: early elderly (60–69 years), middle elderly (70–79 years) and late elderly (80–90 years and above 90 years).
Statistical Analysis:
Statistical analyses were conducted using IBM SPSS Statistics version 27 (IBM Corp., Armonk, NY, USA). Continuous variables were presented as means and standard deviations (SD), and categorical variables were summarized as frequencies and percentages. Differences in continuous variables between groups were assessed using the Mann–Whitney U test due to non-normal distributions. Categorical variables were compared using Pearson’s chi-square (χ²) test or Fisher’s exact test, as appropriate. All statistical tests were two-sided, and a p-value of <0.05 was considered statistically significant.
3. Results
The study included 251 patients who underwent cataract surgery in 2023, comprising 149 (59%) of Jewish ethnicity and 102 (41%) of Arab ethnicity.
The mean age in the Jewish group was 73.52 years (SD = 7.17), while the Arab group had a slightly higher mean age of 73.71 years (SD = 7.42). This difference was not statistically significant (p = 0.770). The standard deviation reflects a moderate variability in age for both groups. The standard error of the mean was marginally lower in the Jewish cohort (SEM = 0.587) compared to the Arab cohort (SEM = 0.735), suggesting a slightly more precise age estimate in the Jewish group.
Gender distribution was nearly identical between the groups: 50.3% female and 49.7% male in the Jewish cohort, compared to 50.0% female and 50.0% male in the Arab cohort (p = 0.960). These results indicate that potential differences in postoperative outcomes are unlikely to be influenced by confounding differences in age or gender between the groups.
To further explore the influence of age on surgical outcomes, patients were stratified into three groups: early elderly (60–69 years), middle elderly (70–79 years), and late elderly (≥80 years). Across both ethnic groups, a trend of reduced postoperative visual acuity improvement was observed with advancing age. The early elderly subgroup exhibited the greatest gain in visual acuity by postoperative day 30, particularly among Jewish patients. In contrast, the late elderly subgroup showed more modest visual recovery and a slightly higher rate of postoperative complications, including corneal edema and posterior capsular opacification. However, these differences did not reach statistical significance (p > 0.05). This trend may reflect increased ocular and systemic fragility with age, as well as a higher prevalence of dense cataracts and comorbid conditions in the older cohorts. While age alone was not an independent predictor of poor outcome in the multivariable model, it remains a relevant clinical consideration when evaluating prognosis and recovery expectations.
A comparison of systemic comorbidities between the Jewish and Arab populations revealed significant differences in the prevalence of certain conditions. Hypertension was more common in the Arab cohort (p = 0.038), as was diabetes mellitus (p = 0.004). In contrast, no significant differences were observed for chronic obstructive pulmonary disease (COPD) (p = 0.832) or hyperlipidemia (p = 0.197).
As shown in
Table 1, diabetes mellitus demonstrated a notably higher mean rank in the Arab group compared to the Jewish group (139.67 vs. 116.64), indicating a substantially greater prevalence. Although the prevalence of COPD was comparable between the groups, the overall burden of comorbidities appeared higher in the Arab population, with diabetes mellitus representing the most marked disparity. The use of mean ranks in this context reflects the relative distribution of comorbidity prevalence between the two groups.
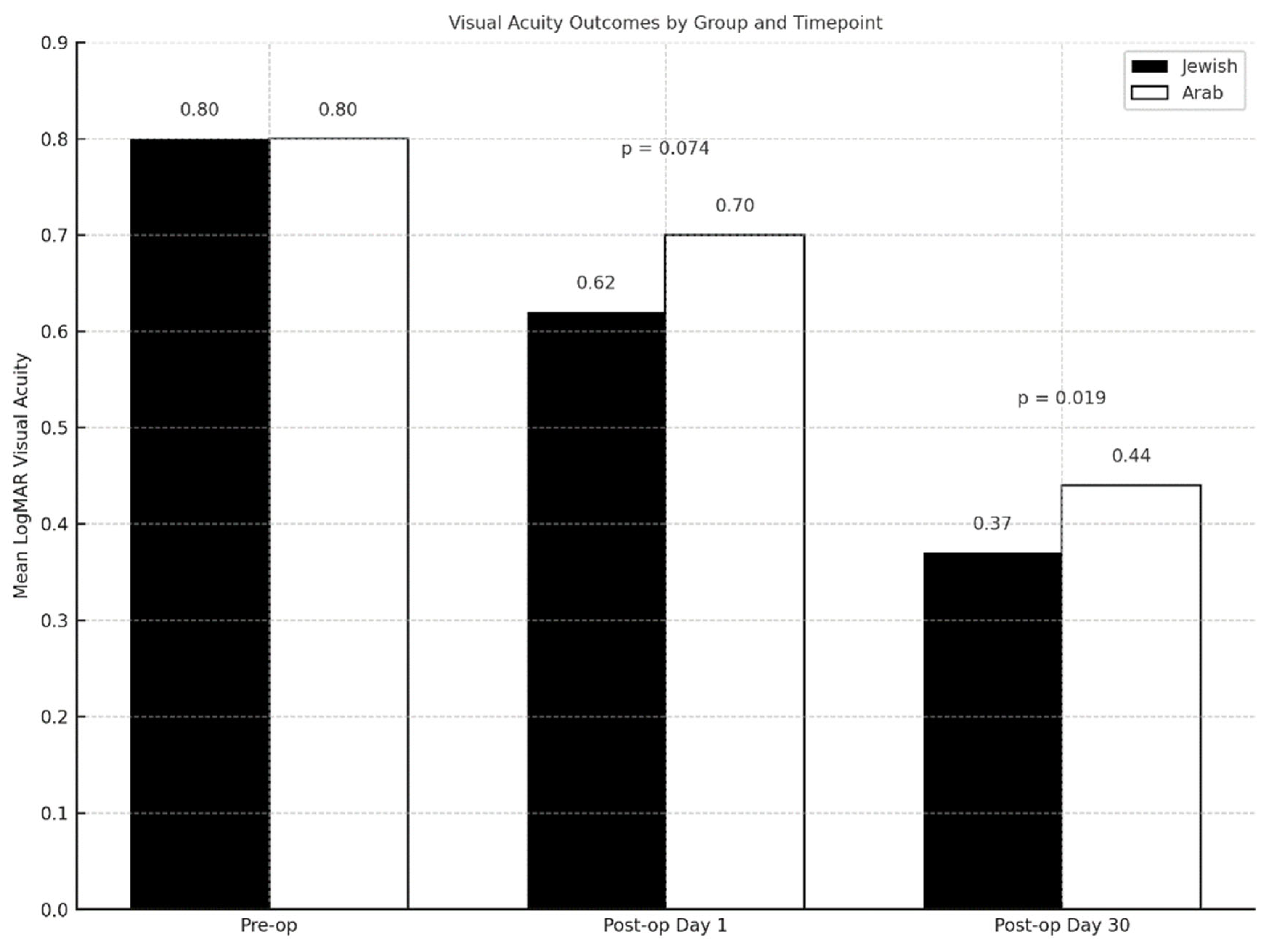
Visual acuity measurements were assessed at three time points: preoperatively, on postoperative day 1, and on postoperative day 30, to evaluate and compare visual outcomes between the Jewish and Arab patient groups (
Table 2).
Preoperative visual acuity was statistically comparable between groups, with both exhibiting a mean LogMAR of 0.80 (p = 0.989), indicating no significant baseline differences in ocular function. By postoperative day 1, a trend toward better visual acuity was observed in the Jewish group (mean LogMAR 0.62) compared to the Arab group (mean LogMAR 0.70), though the difference did not reach statistical significance (p = 0.074). However, by postoperative day 30, this difference became statistically significant: The Jewish group demonstrated a lower mean LogMAR of 0.37 versus 0.44 in the Arab group (p = 0.019), reflecting a superior visual improvement over time. These findings suggest that while both groups began with equivalent visual acuity and exhibited early postoperative gains, the Jewish population experienced a greater and more sustained improvement by the 30-day follow-up. The results highlight a potential disparity in long-term visual recovery, warranting further investigation into postoperative care adherence, access to follow-up, and broader systemic factors that may influence surgical outcomes across different population groups. (
Figure 1).
Significant differences were observed in the prevalence and severity of specific cataract types between the Jewish and Arab populations, as detailed in
Table 3. Posterior sub-capsular (PSC) cataracts were significantly more prevalent in the Arab group (50%), compared to the Jewish group (36.9%) (p = 0.043). In contrast, no significant differences were noted in the prevalence of cortical cataracts (p = 0.072) or nuclear sclerosis (p = 0.492) between both groups.
These results suggest that while posterior sub-capsular cataracts are more common among the Arab cohort, the occurrence of other cataract types remains comparable across the populations studied. The increased severity of cataracts observed in the Arab group highlights the need for further investigation into potential contributing factors such as genetic predispositions, environmental exposures, and disparities in healthcare access.
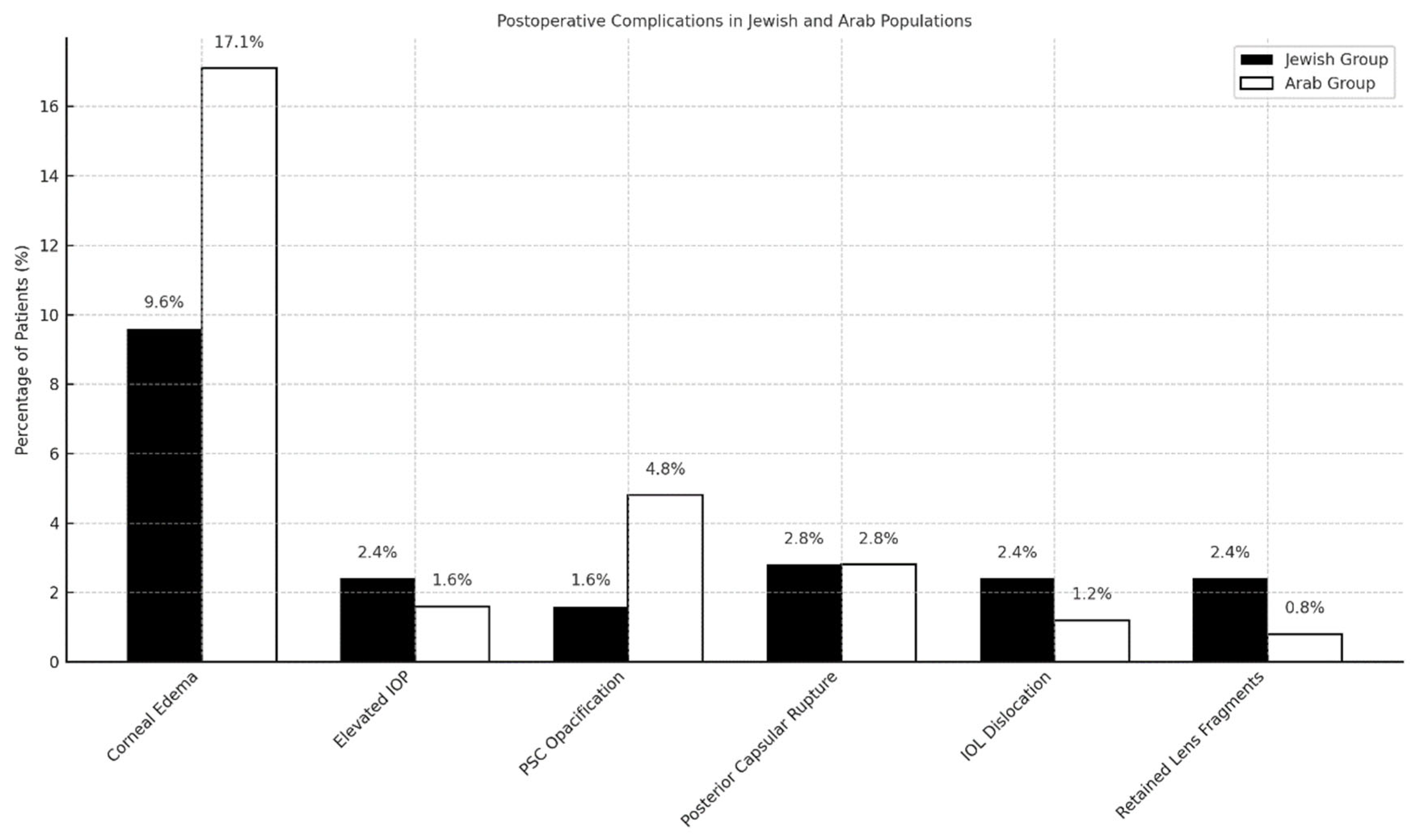
The incidence of postoperative complications following cataract surgery differed between the Jewish and Arab populations, as summarized in
Table 4.
In the Jewish cohort, 39% of patients experienced no postoperative complications, while 61% reported at least one complication. The most frequently observed complication was corneal edema occurring in 16.1% of cases, followed by elevated intraocular pressure (IOP) (4.0%), posterior capsular rupture (2.7%), intraocular lens (IOL) dislocation (4.7%), posterior capsular opacification (2.7%), and retained lens fragments (4.0%). In contrast, only 30.4% of patients in the Arab cohort experienced no complications, suggesting a higher overall complication rate in this group. Corneal edema was significantly more prevalent among Arab patients, affecting 42.2% compared to 16.1% in the Jewish cohort (p<0.001). Posterior capsular opacification was also more common among Arab patients (11.8% vs. 2.7%, p=0.0067). The rates of elevated IOP (3.9% vs. 4.0%), posterior capsular rupture (6.9% vs. 2.7%), IOL dislocation (2.9% vs. 4.7%), and retained lens fragments (2.0% vs. 4.0%) did not differ significantly between the two groups. These differences in complication profiles are illustrated in
Figure 2.
To statistically evaluate differences in postoperative complication rates between groups, a Mann–Whitney U test was conducted. This non-parametric test is appropriate for comparing two independent groups when the dependent variable is ordinal or non-normally distributed. Results demonstrated a significant difference: The Arab group had a higher mean rank (149.12) compared to the Jewish group (110.17), indicating a greater likelihood of postoperative complications. The sum of ranks was 15,210.5 for Arabs and 16,415.5 for Jews, from a total sample size of 251 patients. Although the U statistic was not explicitly reported, the marked difference in rank distributions suggests statistical significance.
Supporting this, a chi-square analysis of complication types yielded a p-value of < 0.001, confirming that the observed differences are unlikely due to chance. These results highlight a potential disparity in postoperative outcomes between the two populations, warranting further investigation into contributing factors such as comorbidities, healthcare access, or perioperative management protocols.
4. Discussion
This study highlights significant disparities in cataract surgery outcomes between Jewish and Arab elderly patients in northern Israel, despite both groups receiving care at the same tertiary hospital and ophthalmology department. While baseline demographics such as age and gender were comparable, key differences emerged in comorbid conditions, cataract severity, surgical outcomes, and postoperative complications.
Arab patients exhibited a higher prevalence of systemic comorbidities, particularly hypertension and diabetes mellitus conditions known to accelerate cataract formation and thus increase surgical complexity [
16]. These findings correspond with the greater proportion of posterior sub-capsular cataracts and higher cataract severity scores observed in this cohort, suggesting that disparities in general health status may lead into worse ophthalmologic profiles at the time of presentation.
Socioeconomic status likely contributed to the disparities observed in this study. As a known determinant of healthcare access and quality [
17], lower socioeconomic conditions in the Arab population may have led to delays in seeking care, resulting in more advanced cataract severity at presentation and a more complex postoperative course.
Postoperative visual outcomes further underscore these differences. While both cohorts had comparable baseline visual acuity, the Jewish group exhibited significantly greater visual improvement by postoperative day 30. Although the incidence of major intraoperative complications such as posterior capsular rupture and intraocular lens (IOL) dislocation was similar across groups, the Arab cohort experienced a higher rate of mild yet vision-affecting complications, particularly corneal edema and posterior capsular opacification (PCO).
A critical, yet often under-recognized, factor influencing postoperative recovery is patient compliance with the prescribed eye drop regimen. Adherence to topical corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), and antibiotic drops is essential for minimizing postoperative inflammation, preventing infection, and reducing the risk of vision compromising complications such as cystoid macular edema, persistent corneal edema, and PCO [
18]. Noncompliance may hinder optimal healing and could partially explain the increased incidence of minor postoperative complications observed in the Arab group. Ensuring consistent and timely use of these medications during the immediate postoperative period is therefore vital to realizing the full therapeutic potential of cataract surgery.
These complications may also be attributed to longer phacoemulsification times necessitated for denser, more mature cataracts [
19], which are more common in patients with delayed presentation. Although not immediately sight-threatening, such complications can prolong recovery and limit ultimate visual acuity outcomes [
19].
Despite both populations receiving care within the same institutional setting, patient-level and interpersonal factors likely contributed to these disparities. Language barriers and varying levels of health literacy may have impeded understanding of postoperative instructions, reducing adherence to prescribed drop regimens and follow-up visits. These communication challenges are especially consequential in postoperative care, where multiple medications with frequent dosing are required. Furthermore, cultural perceptions of surgery, reliance on family-based decision-making, and apprehension toward medical interventions more common in traditional communities may further delay care-seeking behavior and surgical acceptance [
20].
In addition, the experience level of the operating ophthalmologist is an important consideration in surgical outcomes, especially in complex or dense cataracts [
21]. Although all procedures were conducted within the same tertiary facility, variability in surgical expertise among staff and trainees likely existed. Denser cataracts, more frequently seen in the Arab cohort, often require advanced technical skill and longer surgical duration factors that elevate the risk of intra- and postoperative complications, particularly when surgeries are performed by less experienced surgeons [
22]. Allocating more complex cases to senior surgeons or enhancing supervision protocols may help mitigate such risks and improve outcomes in high-risk patients.
Timing of surgical intervention is also a critical determinant of outcomes. In this study, delayed presentation in the Arab cohort likely contributed to both higher cataract severity and greater complication rates. Contributing factors may include variability in referral patterns, limited access to primary or specialist eye care, and systemic barriers that hinder effective navigation of the healthcare system.
While this study focused primarily on clinical outcomes, a more comprehensive evaluation including long-term visual function and patient-reported quality-of-life metrics is essential to fully assess the impact of the observed disparities. Future research should adopt prospective designs and include larger, more diverse cohorts to further elucidate the multifactorial nature of cataract outcomes. Additionally, examining the influence of socioeconomic factors, cultural beliefs, eye drop adherence, and overall postoperative compliance may provide valuable insights for optimizing care in underserved populations.
Addressing these disparities requires a multifaceted approach. Early detection programs targeted at high-risk groups, culturally tailored patient education, and system-level interventions to improve postoperative adherence are imperative. In particular, enhancing compliance with postoperative eye drop regimens through patient counseling, simplified dosing strategies, and the provision of multilingual instructions may reduce preventable complications and support better recovery. Such efforts are essential to ensuring that the benefits of cataract surgery are equitably realized across all population groups, ultimately leading to improved visual outcomes and enhanced quality of life [
23].
This study has several important limitations. First, as a retrospective analysis, it is inherently subject to selection bias and restricted by the availability and completeness of clinical records. Additionally, potential confounding factors such as socioeconomic status, healthcare access, and adherence to postoperative care were not directly measured, yet may have significantly influenced the observed differences in outcomes. The single-center nature of the study also limits the generalizability of the findings to broader or more diverse populations. Moreover, the study did not account for differences in surgical technique, surgeon experience, or the timing of surgeries (e.g., morning vs. afternoon sessions). These factors could impact patient outcomes and introduce systematic variability. For instance, surgeon fatigue or fluctuating performance throughout the day might influence complication rates or recovery trajectories, particularly in high-volume settings. Without accounting for these operational nuances, the true sources of disparity in outcomes may be only partially captured.
The findings highlight the need for targeted strategies to reduce disparities in cataract surgery outcomes especially among populations with a greater burden of comorbidities such as diabetes mellitus and hypertension. Early identification and management of these conditions in high-risk groups may improve preoperative visual status and enhance surgical prognosis.
Optimizing postoperative care is also critical. Interventions that promote health literacy, improve patient education, and support adherence to medication and follow-up schedules could meaningfully reduce complications and promote better visual recovery. Tailored patient navigation services or culturally sensitive care models may help bridge gaps in access and adherence, particularly in underserved communities.
Further research is needed to better understand the multifactorial nature of postoperative disparities. Prospective, multicenter studies with larger and more diverse cohorts could validate and extend these findings. Future investigations should examine the influence of surgeon-related factors (e.g., experience, volume, fatigue) and structural determinants of health, including socioeconomic status, transportation availability, education level, and health beliefs.
Additionally, studies focusing on cultural practices, patient-provider communication, and trust in the healthcare system may provide deeper insight into behavioral and systemic contributors to differential outcomes. A comprehensive approach addressing both clinical and contextual determinants is essential for ensuring equitable cataract surgery outcomes across ethnic and socio-economic groups.
5. Conclusions
This study highlights significant disparities between Jewish and Arab populations in northern Israel with respect to cataract severity, associated comorbidities, and postoperative outcomes. Despite similar age and gender distributions, the Arab cohort demonstrated a higher prevalence of hypertension and diabetes mellitus conditions that were linked to increased cataract severity and a higher incidence of postoperative complications. In contrast, the Jewish cohort exhibited superior postoperative visual acuity and fewer complications, suggesting that systemic health factors, healthcare access, and potential variations in adherence to postoperative protocols may play a significant role in these outcomes. These findings emphasize the need for targeted interventions to address health disparities, including early screening and management of comorbidities such as hypertension and diabetes, as well as improvements in postoperative care and patient education. Future research should focus on exploring the underlying mechanisms contributing to these disparities, with the goal of optimizing cataract management and improving surgical results across diverse patient populations.
Author Contributions
D. Njudat, S. Boqaaiya, O. Chassid, Y. Cohen: study conception and design as well as data acquisition, data analysis, and drafting of the manuscript Y. Cohen, S. Boqaaiya, W. Srour: data acquirement and statistical analysis K.Beiruti Wiegler: critical manuscript revision.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted -in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (0086-23-ZIV) at Ziv Medical Center, Israel(date: 11.01.2024).
Informed Consent Statement
Patient consent was waived by the institutional review board due to the anonymized nature of data collection and the retrospective analysis of data.
Data Availability Statement
Full data is available following a formal request and in compliance with state regulations.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moshirfar, M.; Milner, D.; Patel, B. Cataract surgery. StatPearls. 2023. [Google Scholar]
- Nizami, A.A.; Gurnani, B.; Gulani, A.C. Cataract. In StatPearls [Internet]; StatPearls Publishing: 2024.
- Hashemi, H.; Pakzad, R.; Yekta, A.; Aghamirsalim, M.; Pakbin, M.; Ramin, S.; Khabazkhoob, M. Global and regional prevalence of age-related cataract: a comprehensive systematic review and meta-analysis. Eye 2020, 34, 1357–1370. [Google Scholar] [CrossRef] [PubMed]
- Terveen, D.; Berdahl, J.; Dhariwal, M.; Meng, Q. Real-World Cataract Surgery Complications and Secondary Interventions Incidence Rates: An Analysis of US Medicare Claims Database. Journal of Ophthalmology 2022, 2022, 8653476. [Google Scholar] [CrossRef] [PubMed]
- Mencucci, R.; Stefanini, S.; Favuzza, E.; Cennamo, M.; De Vitto, C.; Mossello, E. Beyond vision: Cataract and health status in old age, a narrative review. Frontiers in medicine 2023, 10, 1110383. [Google Scholar] [CrossRef] [PubMed]
- Nussinovitch, H.; Tsumi, E.; Tuuminen, R.; Malyugin, B.; Lior, Y.; Naidorf Rosenblatt, H.; Boyko, M.; Achiron, A.; Knyazer, B. Cataract surgery in very old patients: a case-control study. Journal of clinical medicine 2021, 10, 4658. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef] [PubMed]
- Althiabi, S.; Aljbreen, A.J.; Alshutily, A.; Althwiny, F.A.; Aljbreen, A. Postoperative endophthalmitis after cataract surgery: an update. Cureus 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Durr, G.M.; Ahmed, I.I.K. Intraocular lens complications: decentration, uveitis–glaucoma–hyphema syndrome, opacification, and refractive surprises. Ophthalmology 2021, 128, e186–e194. [Google Scholar] [CrossRef] [PubMed]
- Hong, A.R.; Sheybani, A.; Huang, A.J. Intraoperative management of posterior capsular rupture. Current opinion in ophthalmology 2015, 26, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Mencucci, R.; Vignapiano, R.; Rubino, P.; Favuzza, E.; Cantera, E.; Aragona, P.; Rolando, M. Iatrogenic dry eye disease: dealing with the conundrum of post-cataract discomfort. A PICASSO board narrative review. Ophthalmology and Therapy 2021, 10, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Grimfors, M.; Lundström, M.; Höijer, J.; Kugelberg, M. Intraoperative difficulties, complications and self-assessed visual function in cataract surgery. Acta Ophthalmologica 2018, 96, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Seyedian, M.A.; Mohammadpour, M. Small pupil and cataract surgery. Current opinion in ophthalmology 2015, 26, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Weber, C.H.; Cionni, R.J. All about capsular tension rings. Current opinion in ophthalmology 2015, 26, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Elam, A.R.; Tseng, V.L.; Rodriguez, T.M.; Mike, E.V.; Warren, A.K.; Coleman, A.L.; Aguwa, U.; Alabiad, C.; Briceno, C.; Capo, H. Disparities in vision health and eye care. Ophthalmology 2022, 129, e89–e113. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.R.; Koo, E.; Agrón, E.; Hallak, J.; Clemons, T.; Azar, D.; Sperduto, R.D.; Ferris III, F.L.; Chew, E.Y.; Group, A.-R.E.D.S. Risk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmology 2011, 118, 2113–2119. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Egerter, S.; Williams, D.R. The social determinants of health: coming of age. Annual review of public health 2011, 32, 381–398. [Google Scholar] [CrossRef] [PubMed]
- Nouraeinejad, A. Factors of noncompliance with prescribed eye drops in patients undergoing cataract surgery. The Journal of Medicine Access 2023, 7, 27550834231152341. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Singhal, D.; Nair, S.P.; Sahay, P.; Sreeshankar, S.; Maharana, P.K. Corneal edema after phacoemulsification. Indian journal of ophthalmology 2017, 65, 1381–1389. [Google Scholar] [CrossRef] [PubMed]
- Kiziltoprak, H.; Tekin, K.; Inanc, M.; Goker, Y.S. Cataract in diabetes mellitus. World journal of diabetes 2019, 10, 140. [Google Scholar] [CrossRef] [PubMed]
- Tsegaw, G.W.; Dea, Y.C.; Mengesha, M.M. Predictors of time to recovery from cataract surgery among cataract patients at Menelik II Comprehensive Specialized Hospital: a retrospective follow up study. BMC ophthalmology 2025, 25, 246. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, L.D.; Baltă, G.; Baltă, F.N. Investigation of risk factors predicting cataract surgery complications in patients with pseudoexfoliation syndrome: a systematic review. Journal of Clinical Medicine 2024, 13, 1824. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, G.A.; Borkar, D.S.; Borboli-Gerogiannis, S.; Greenstein, S.H.; Lorch, A.C.; Vasan, R.A.; Kloek, C.E. Optimization of cataract surgery follow-up: a standard set of questions can predict unexpected management changes at postoperative week one. PLoS One 2019, 14, e0221243. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).