1. Introduction
The aesthetics of the face have attracted patients since the dawn of humanity. Several techniques have been developed to achieve facial harmony and symmetry. Jaw advancement surgeries, fillers, and genioplasty have been employed in the lower third of the face with excellent outcomes and clear indications [
1].
Genioplasty is a well-established surgical procedure. Performed through osteotomies in the mental region of the mandible, this procedure involves separating the bone stumps and repositioning them in the necessary position, followed by a rigid fixation using plates and screws. This technique allows for advancement, setback, widening, narrowing, and increase or decrease in facial height [
2].
An alternative to genioplasty is the placement of anatomical facial prostheses, which increase the volume and contour of the chin region without requiring osteotomies [
3].
Finite element analysis (FEA) is commonly performed before in vitro and in vivo studies. In these studies, we can virtually simulate situations where forces are applied in different regions of the plates and evaluate the maximum stress and fatigue of the material [
4]. This technique helps guide future studies and assess the feasibility of the product [
5].
To revolutionize and improve this surgical approach, we developed an anatomical chin plate that enables multidirectional movement of the bone stumps, offering enhanced contour and anatomy to the facial aesthetic region. In this study, we compared a conventional chin plate (CP) with the new anatomical chin plate (ACP) using finite elements.
2. Materials and Methods
2.1. New Design
The ACP plate arose from the need to bring a greater aesthetic result to genioplasty, and bone advancement or setback is already well-established in both the literature and clinical practice. The aesthetic complement of the mentolabial sulcus in several patients often requires bone or fat grafts to obtain the desired aesthetic effect.
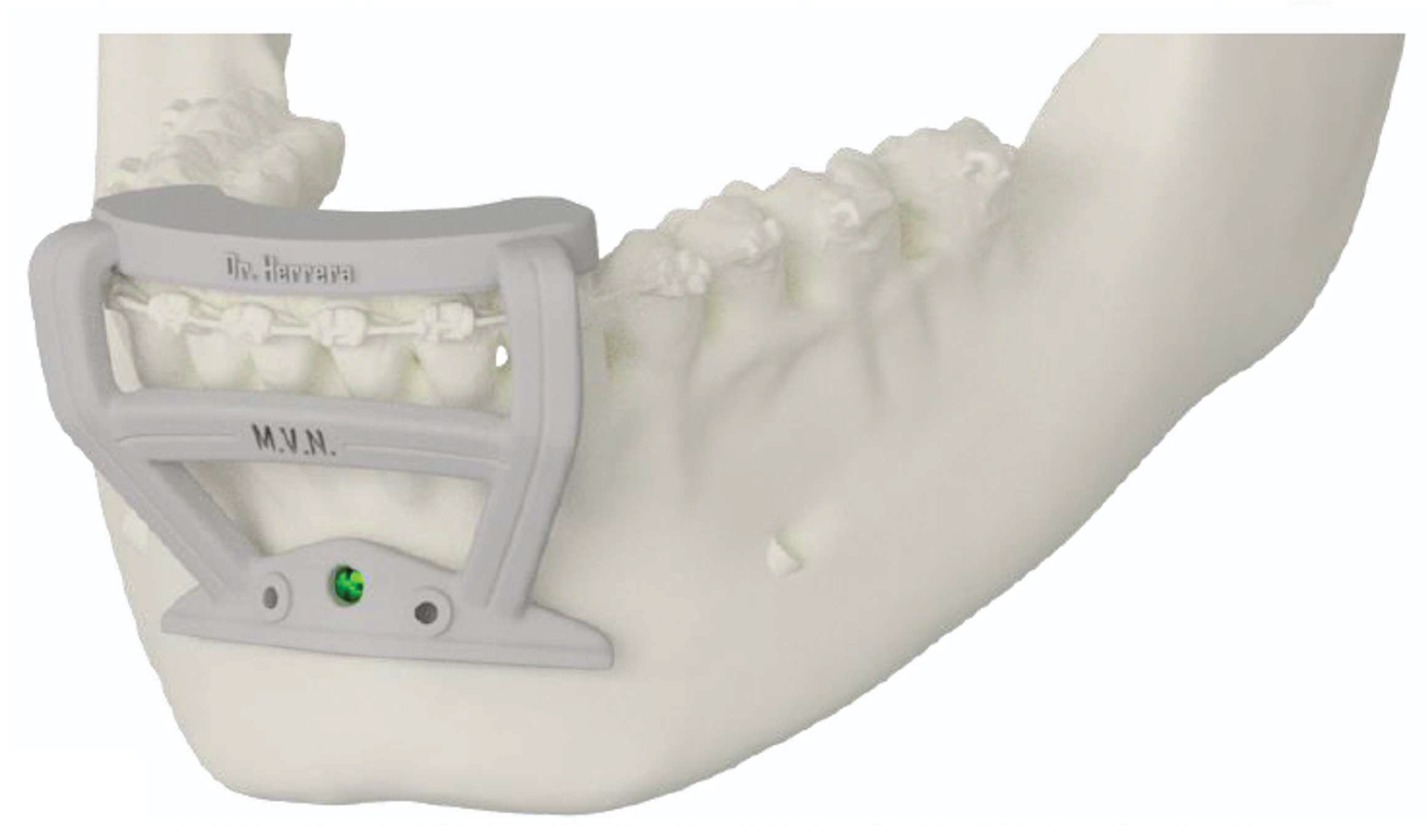
This new customized plate allows for precise planning of bone advancement or setback while maintaining the aesthetics of the mentolabial fold, which can be seen both in the profile and frontal analysis of the patient (
Figure 1).
To ensure the ACP fits accurately and achieves the planned aesthetic outcome, a guided osteotomy must be performed. A surgical guide is fabricated with high precision to match the planned osteotomy. This guide must be stabilized at both the top (occlusion of the lower teeth) and bottom using a screw (
Figure 2). The screw used to stabilize the guide also serves as a drilling guide for the placement of the ACP plate.
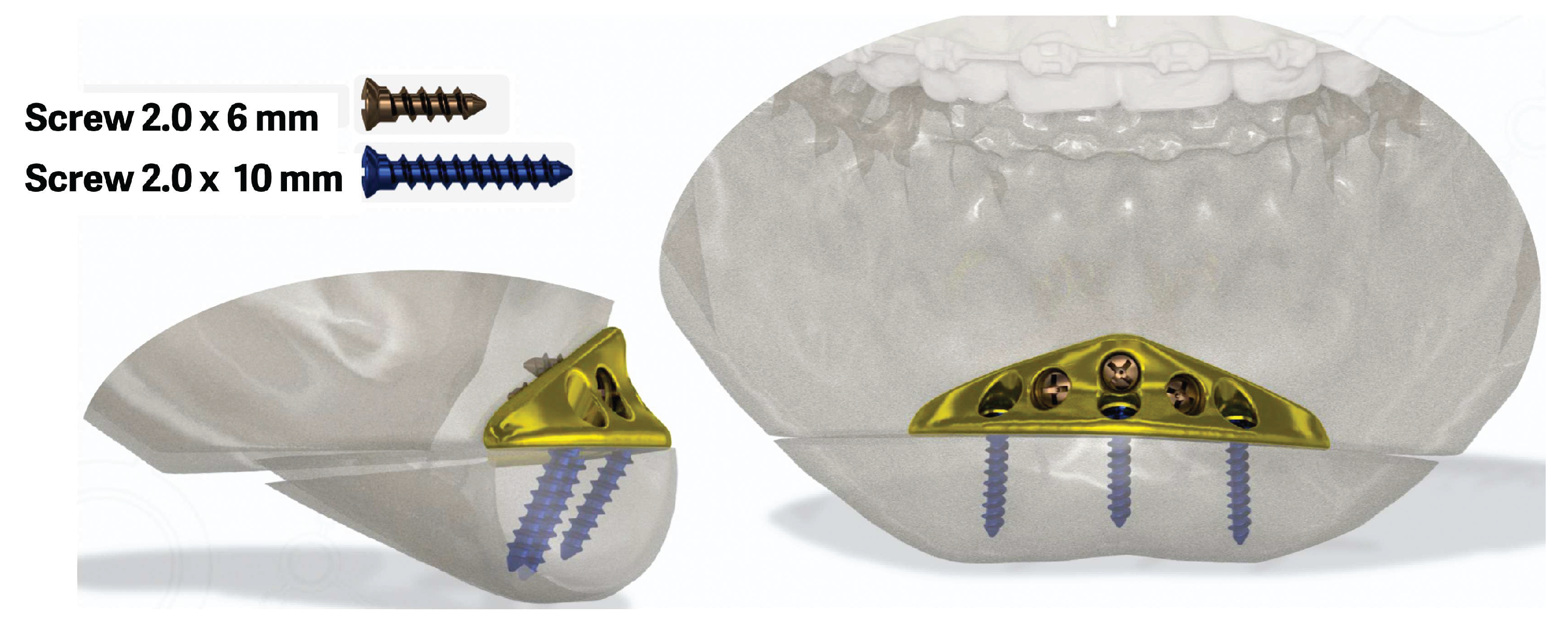
During planning the ACP plate, the required size of the screws and their relationship with the dental roots were carefully determined to avoid future complications (
Figure 3).
2.2. Modeling and Mechanical Analysis
The plates used in this study were modeled using Blender software version 3.x (Blender Foundation, 2025). Titanium Ti-6AI-4V plates were used, with an elastic modulus of 110 GPa, Poisson’s coefficient of 0.34, and a yield strength of 880 MPa. These three-dimensional models were imported into the ANSYS Mechanical Finite Element Analysis software (© 2024 ANSYS, Inc.).
To simulate muscle loading in the chin region, an oblique force vector with a modulus of 60 N was applied, oriented at 45° in the sagittal plane, directed inferoposteriorly. This direction corresponds to the muscular forces exerted primarily by the mental muscles and the anterior belly of the digastric during functional contraction.
Based on the functional anatomy of the mentalis and anterior belly of the digastric muscles, the resulting vector of muscle force acting on the chin can be represented by an oblique vector inclined at 45°, directed inferoposteriorly (i.e., downward and backward).
If we consider a total net force of 60 N, the vector at 45° has equal components in X and Y, as follows:
To evaluate the mechanical strength of the titanium plates used in genioplasty, three-dimensional FEA was performed using the von Mises equivalent stress criterion. This criterion was selected because it is widely accepted in the flow prediction of ductile materials such as Ti-6Al-4V.
The plate model was subjected to a vector force of 60 N applied at 45° in the sagittal plane, representing the combined traction of the mentalis muscles and anterior belly of the digastric. Boundary conditions were applied to simulate rigid fixation of the plate to the mandibular blocks using screws that were restricted to all translational degrees of freedom.
The mesh was composed of second-order tetrahedral elements, and the solution was applied until the numerical residuals converged. Von Mises stresses were calculated throughout the body of the plate to identify the regions of stress concentration. Results were expressed in megapascals (MPa) and presented on a continuous chromatic scale.
3. Results
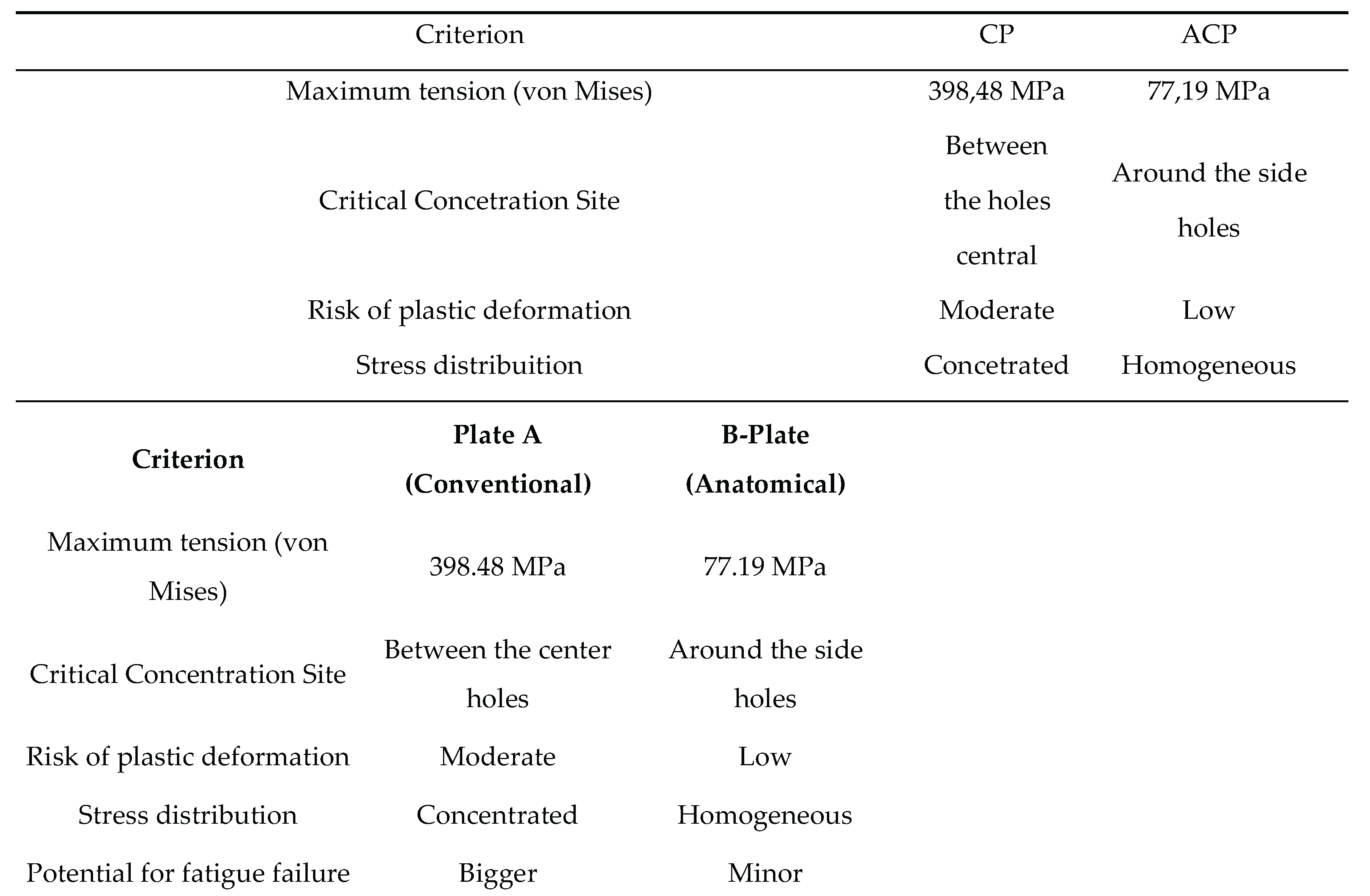
Two different configurations of titanium plates for genioplasty were analyzed with respect to the distribution of von Mises stresses under the same 60 N loading applied at 45°, simulating the combined vector action of the mentalis and anterior digastricus muscles. All models and their characteristics are summarized in
Table 1.
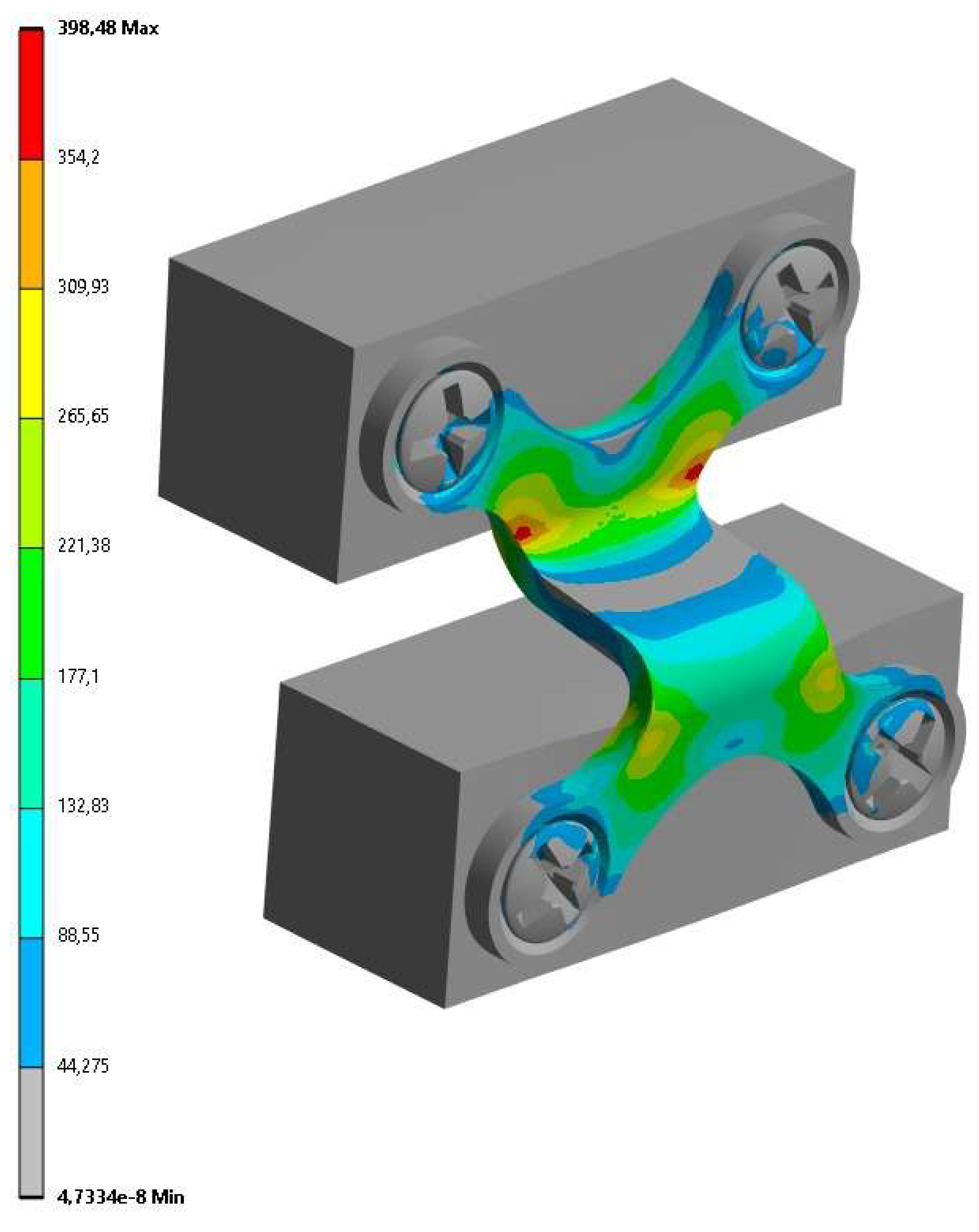
For the conventional plate (
Figure 4), the maximum recorded stress was 398.48 MPa, which was located in the central region of the plate between the fixing holes. The stress distribution was concentrated in the geometric transition areas and near the orifices, suggesting a possible failure starting point under the cyclic loading. Despite the concentration, the values remained below the yield strength of grade 5 titanium (880 MPa), indicating structural safety under an isolated loading.
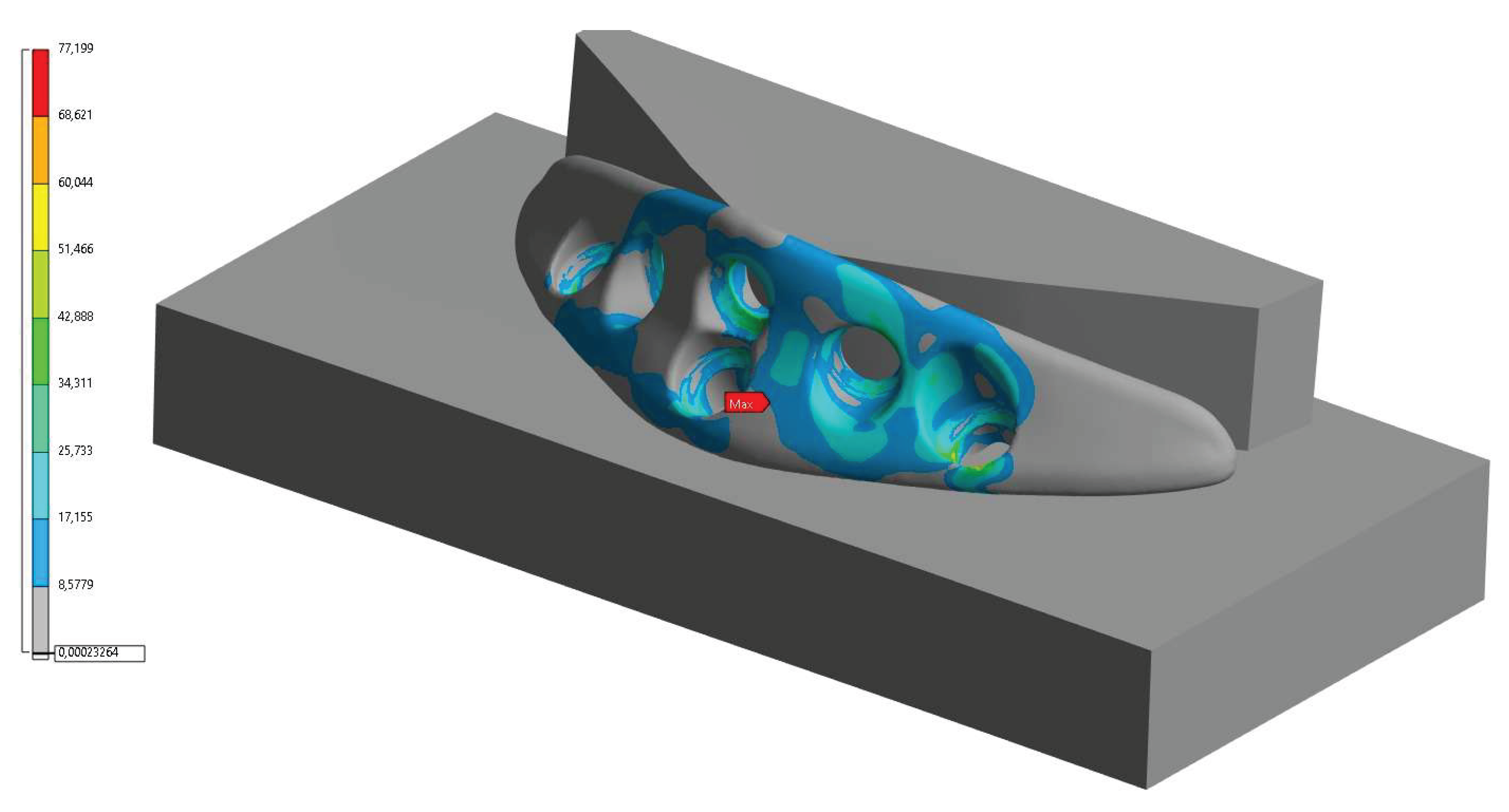
In contrast, for the ACP plate (
Figure 5), the maximum stress was 77.19 MPa, distributed around the fixation holes on the lateral portions of the implant. The stress distribution was more homogeneous, with a significant reduction in peak concentrations, particularly in the critical transition regions between the holes and edges. The results suggest that anatomical geometry favors a more efficient dispersion of the load, contributing to greater resistance to fatigue and a reduced risk of local failure.
4. Discussion
Genioplasty is a surgical procedure that modifies the size, shape, and position of the chin in all directions {2}. When we combined genioplasty with internal fixation, regardless of the fixation type, the procedure proved to be stable regardless of movement (advance or retreat) when evaluating recurrence in hard and soft tissues [
6].
In terms of aesthetics, genioplasty, when compared to chin implants, provided more satisfaction in patients undergoing osteotomy and produced fewer complications [
3]. When we think about the osteotomy itself, a modification that has great acceptance is the Chin Wing [
7]. Because of its great extension in most cases, it becomes necessary to have extra fixations, which would be an excellent indication for the ACP plate due to its high degree of resistance. In cases of minimally invasive osteotomies with different shapes [
8], the ACP plate can be used to improve the quality of the soft tissue in the submental region.
We used finite elements as an accurate and cohesive method for evaluating the strength of a plate. It is known that the width, rather than the thickness, of a plate can influence the resistance, making the facts decisive for reducing the maximum stress under bending forces [
9]. This is in accordance with the shape of our ACP plate, which, because it is extended, has 11 less tensions than a conventional plate in addition to delivering the necessary aesthetics for the region.
When evaluating the stability of genioplasty, one of the main concerns is the stability of the bone stump in relation to the musculature inserted in the chin. This fixation method is effective in preventing recurrence [
5]. Initially, genioplasties were fixed with two bicortical screws; however, FEA has shown that a centrally located conventional plate produced more stability than two bicortical screws [
10]. Thus, the placement of a plate, in addition to being more stable, is an easier procedure, particularly in cases of indentation and chin asymmetry.
The ACP plate was slightly thicker than the conventional plate. Plate thickness can be an important factor influencing the yield threshold and plate deformation. Further studies using plates of different thicknesses should be conducted in the future.
Among the various osteotomy techniques, the T-osteotomy, which removes the central part of the chin, reduces the width, and provides a new contour, is considered one of the least stable and requires fixation with greater stability. A finite element study found that the optimal stability was achieved with either a 1.2 mm plate and five screws or a 0.9 mm plate and seven screws [
11]. This suggests that the new ACP plate, in addition to maintaining a thickness of 1.2 mm, also has six screws, which should be more than ideal to ensure perfect resistance to variations in T-osteotomy.
In advanced genioplasties, customized plates have demonstrated better distribution of strain stress and improved stabilization between the stem and segment [
12]. Another benefit of customized plates is the incorporation of nanoparticles such as graphene into their composition; these alloys have been shown to reduce the stress distribution between 5% and 25% in the critical zones of titanium plates [
13].
The thickness of the plate is a primary factor for stress distribution on the plates, promoting more resistance in advance [
14,
15]. The conventional plate has a thickness of 0.8 mm, whereas the customized ACP plate, at its smallest point, maintains a thickness of 1.2 mm, making it substantially more resistant to titanium fatigue.
5. Conclusions
The results indicate that the ACP plate model demonstrates superior mechanical performance compared to the CP plate, with significantly lower stress values and better load distribution across the structure. This suggests more favorable biomechanical behavior, especially in situations of cyclic or prolonged loading conditions, similar to the functional activities of the chin.
Further studies should be conducted, mainly on biomechanical models and loads, to evaluate the in vitro resistance of these new plates.
With the validation and clinical adoption of anatomical plates in genioplasty, the benefits of osteotomy and the contour of facial prostheses can be combined in a single, integrated technology for enhancing facial aesthetics.
Author Contributions
All authors contributed equally to the conceptualization, methodology, data analysis, validation, drafting, review, editing, and final approval of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no financial support for this study, authorship, or publication.
Institutional Review Board Statement
This study was conducted in accordance with the relevant laws and institutional guidelines and was approved by the Ethics Committee of São Leopoldo Mandic University (approval number: 43735621.5.0000.5374).
Informed Consent Statement
Not applicable
Data Availability Statement
The raw data supporting the conclusions of this study are available from the authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shokri T, Rosi-Schumacher M, Petrauskas L, Chan D, Ducic Y. Genioplasty and Mandibular Implants. Facial Plast Surg. 2021 Dec;37(6):709.
- Ferretti C, Reyneke JP. Genioplasty. Atlas Oral Maxillofac Surg Clin North Am. 2016 Mar;24(1):79–85.
- Tabrizi R, Behnia P, Kavianipour M, Behnia H. Osseous genioplasty versus chin implants: early complications and patient satisfaction. Int J Oral Maxillofac Surg. 2024 Feb;53(2):141–145.
- Choi AH, Ben-Nissan B, Conway RC. Three-dimensional modelling and finite element analysis of the human mandible during clenching. Aust Dent J. 2005 Mar;50(1):42–48.
- Stróżyk P, Bałchanowski J. Application of numerical simulation studies to determine dynamic loads acting on the human masticatory system during unilateral chewing of selected foods. Front Bioeng Biotechnol. 2023 May 11;11:993274.
- Kumar M, Singh RS, Singh G, Raj P, Gupta H, Kasrija R. Hard and soft tissue relapse after different genioplasty procedures: a scoping review. Cureus. 2023 Jul 6;15(7):e41478.
- Cordier G, Sigaux N, Rasteau S, Ibrahim B, Cresseaux P. Long-term stability of basilar mandible osteotomy: Chin Wing. J Stomatol Oral Maxillofac Surg. 2022 Jun;123(3):337–344.
- Leon NJ, Péres AJP, Requejo S, Goméz D, Barros HLM. Telescopic genioplasty: a new concept to reshape the chin. Advances in Oral and Maxillofacial Surgery. 2021 Oct;(4): 10076.
- Guerra RC, de Fátima Borim Pulino B, Salomão Júnior VF, Dos Santos Pereira R, Thieringer FM, Sacco R, Sader R, Vieira EH. Finite element analysis of low-profile reconstruction plates for atrophic mandibles: a comparison of novel 3D grid and conventional plate designs. Oral Maxillofac Surg. 2024 Jun;28(2):595–603.
- Gulsever S, Munevveroglu S, Hartomacioglu S, Guldiken IN, Uckan S. Comparison of screw and plate osteosynthesis in advancement genioplasty: a finite element analysis study. Eur Oral Res. 2025 Jan 5;59(1):40–45.
- Akkoyun EF, Pergel T. Finite element analysis of shape and thickness variations in patient-specific implants for T-shaped genioplasty. Med Oral Patol Oral Cir Bucal. 2025 Mar 23:27065.
- Ramos VF, Pinto LAPF, Basting RT. Force and deformation stresses in customized and non-customized plates during simulation of advancement genioplasty. J Craniomaxillofac Surg. 2017 Nov;45(11):1820–1827.
- Jindal P, Worcester F, Gupta A, Breedon P. Efficiency of nanoparticle reinforcement using finite element analysis of titanium alloy mandible plate. Proc Inst Mech Eng H. 2019 Mar;233(3):309–317.
- Tazh T, Khorramymehr S, Hassani K, Nikkhoo M. Finite element analysis of various fixation patterns in mandible bone fracture. Comput. Methods Biomech Biomed Engin. 2025 Mar 13:1–16.
- da Silveira MLM, de Oliveira Bueno ML, da Silva JSP, Germano AR. Biomechanical analysis in mandibular advancement and occlusal plane rotation with finite element analysis. Br J Oral Maxillofac Surg. 2021 Apr;59(3):362–367.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).