Submitted:
15 July 2025
Posted:
16 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
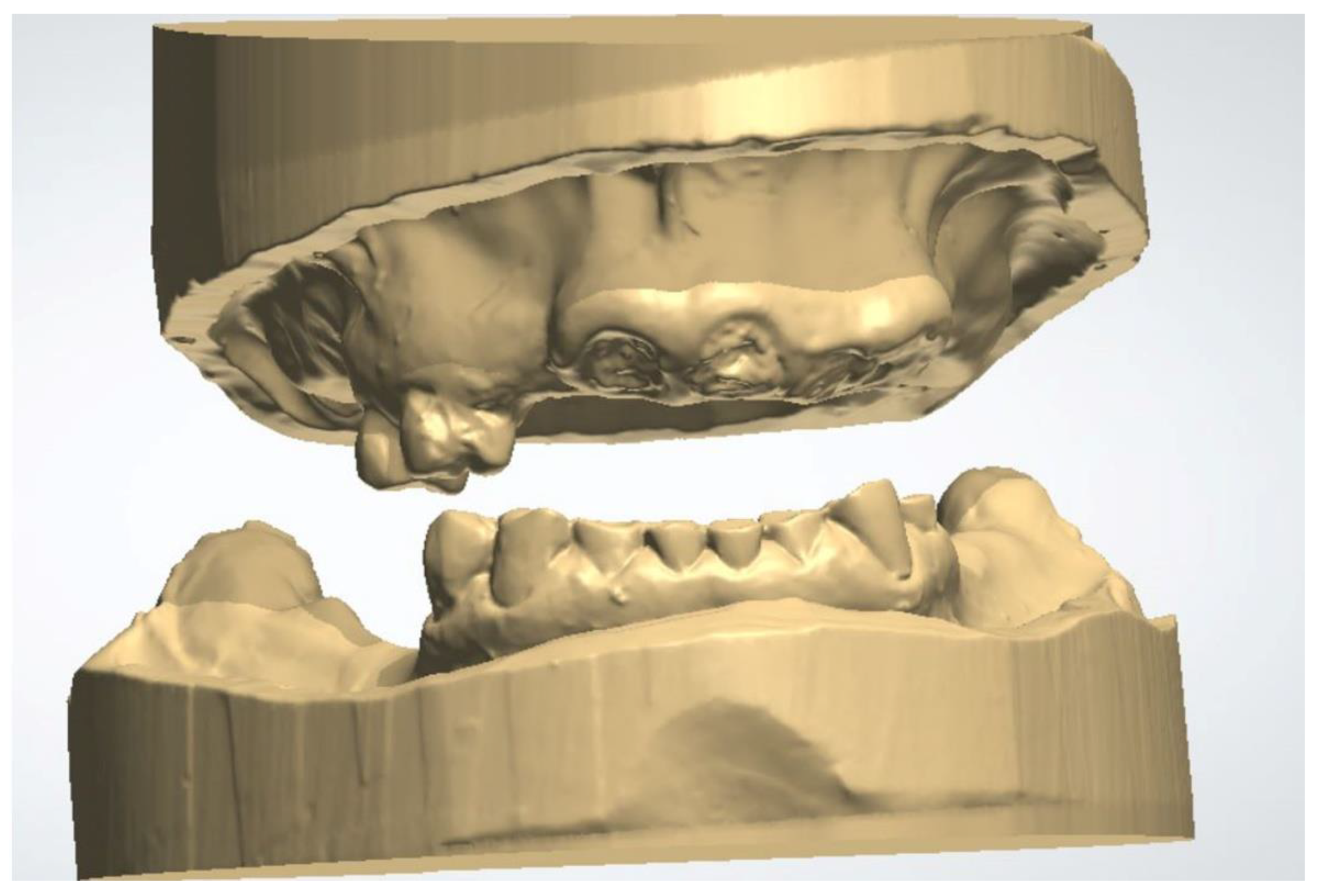
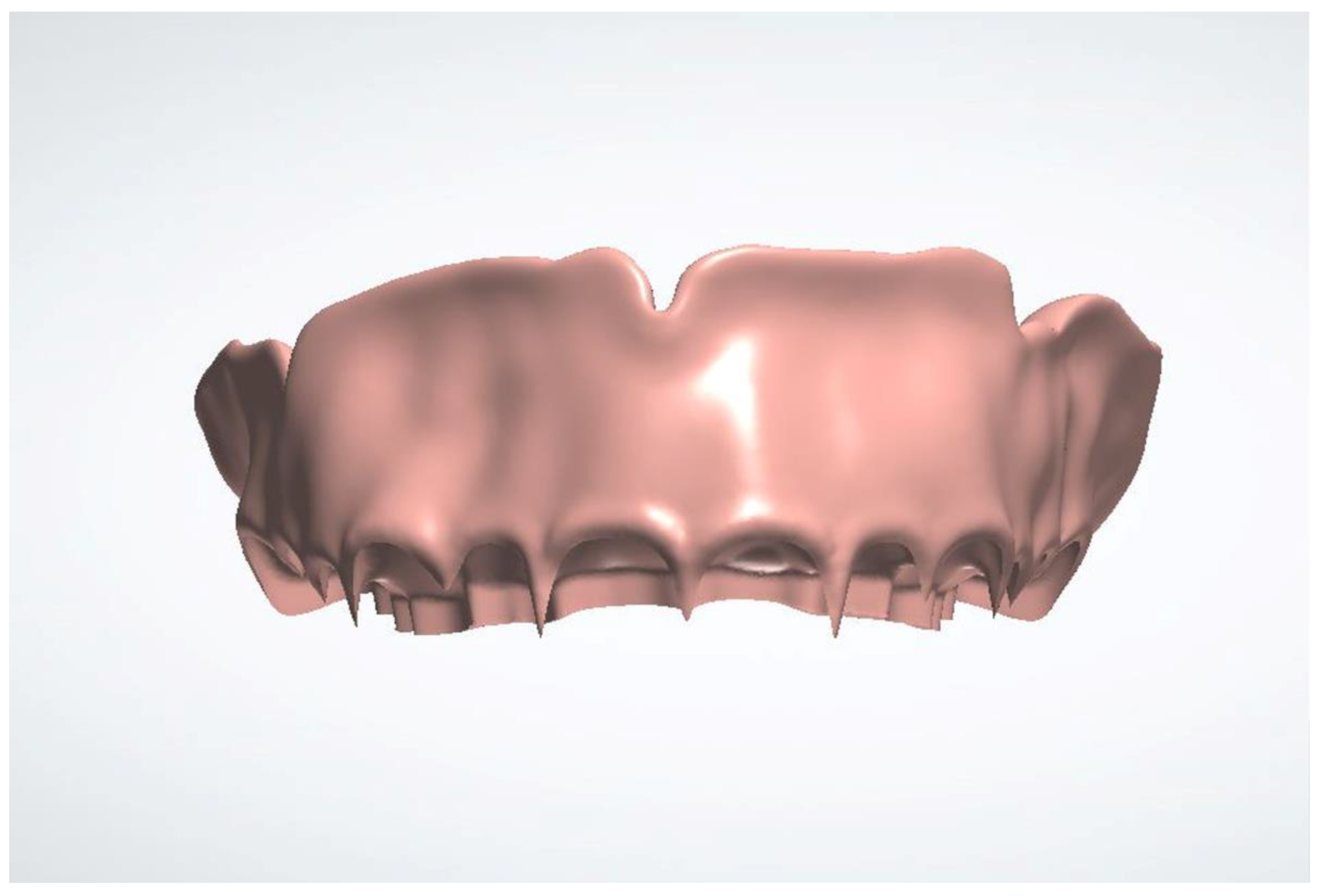
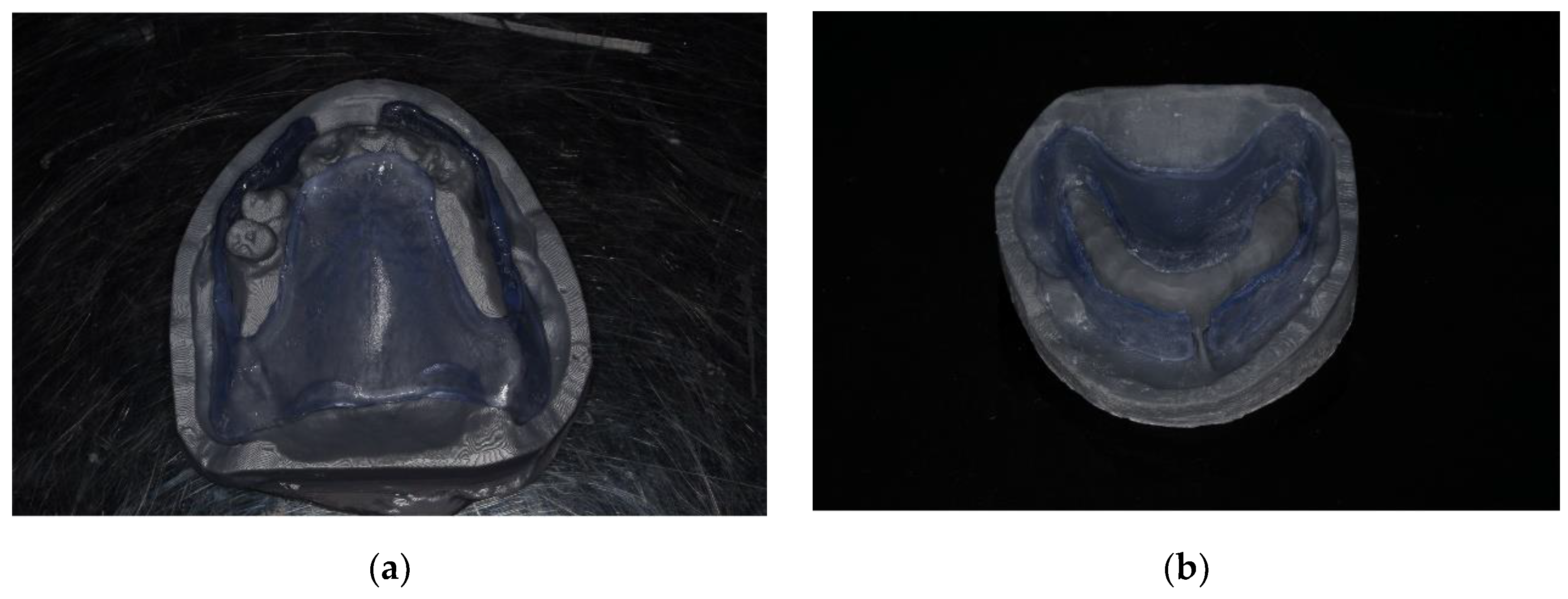
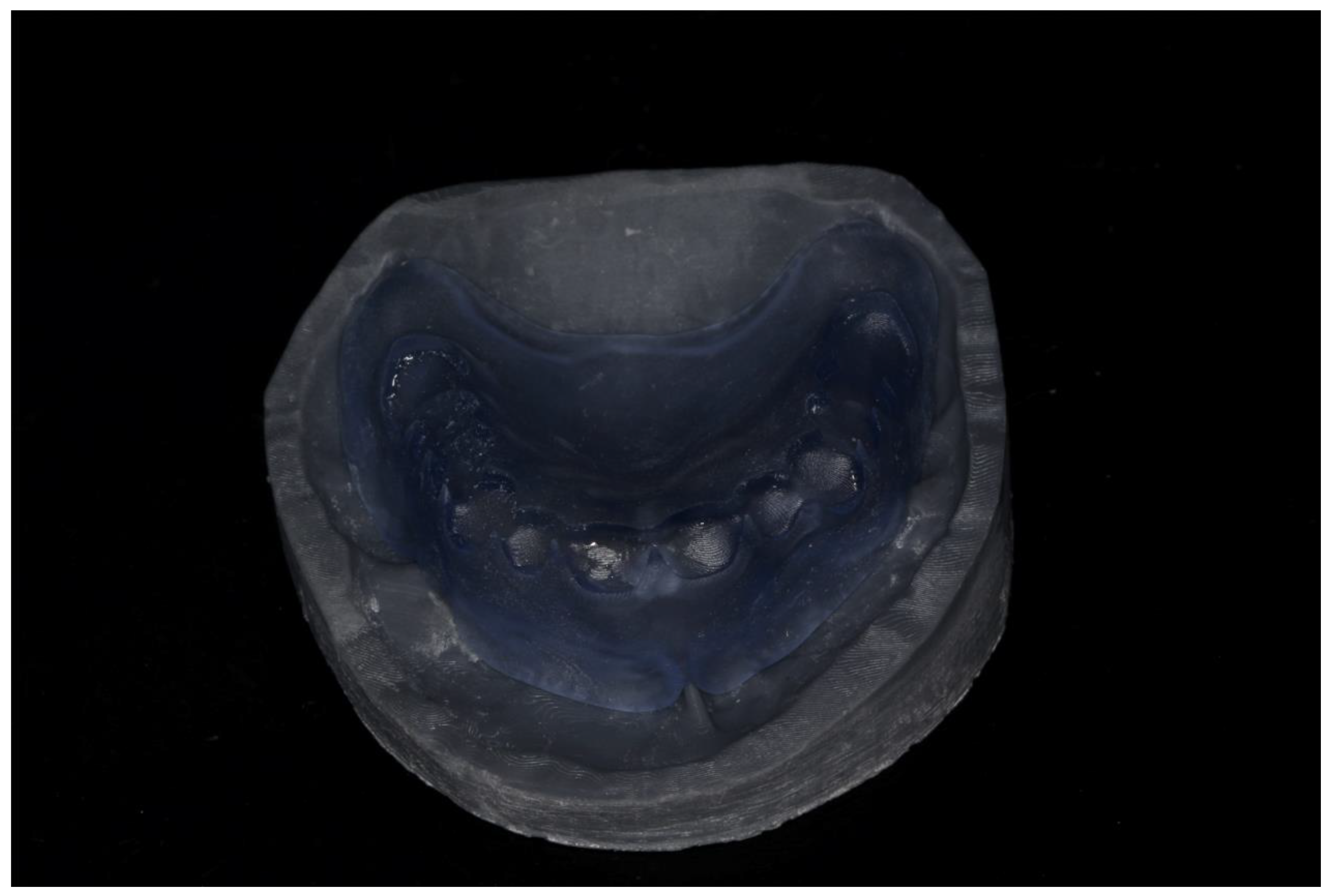
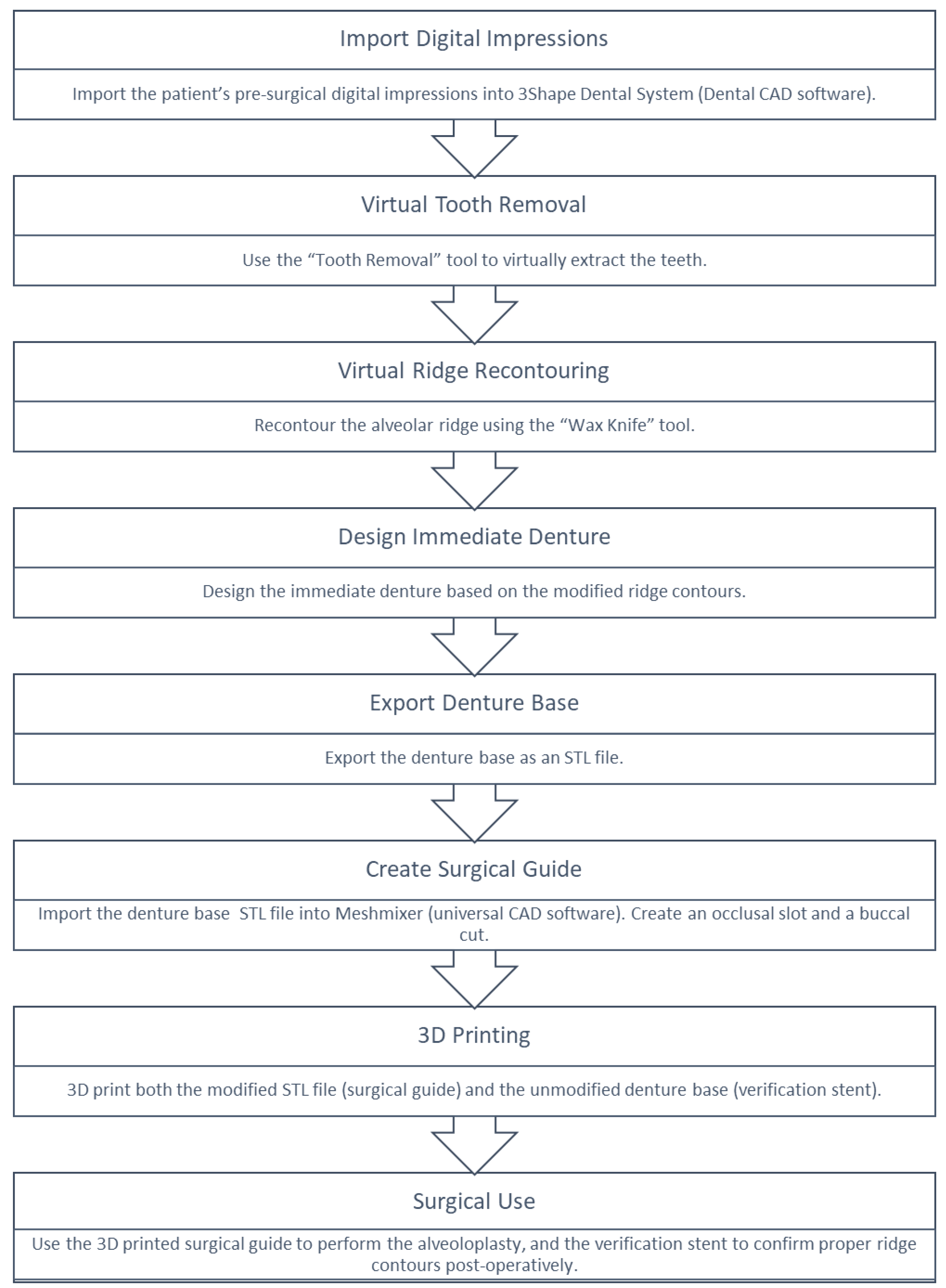
- Import the digital impressions of the patient’s pre-operative maxillary and mandibular arches into a dental CAD software (3Shape Dental System version DS2022-1 /2.22.1.0 or later; 3Shape A/S) for the fabrication of a complete denture (Figure 1). the digital impressions could either be direct intraoral scans, or laboratory scans of stone casts or analogue impressions.Figure 1. Pre-operative maxillary and mandibular digital impressions imported into 3Shaped Dental Manager.Figure 1. Pre-operative maxillary and mandibular digital impressions imported into 3Shaped Dental Manager.
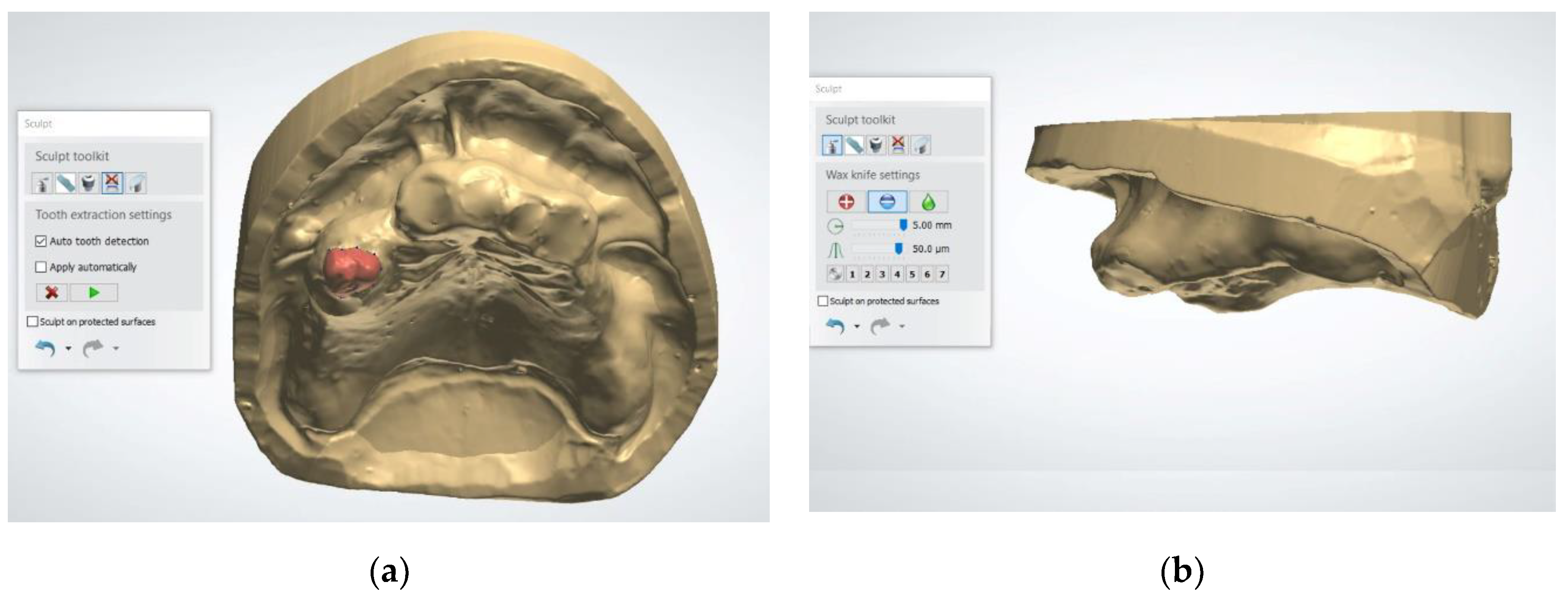
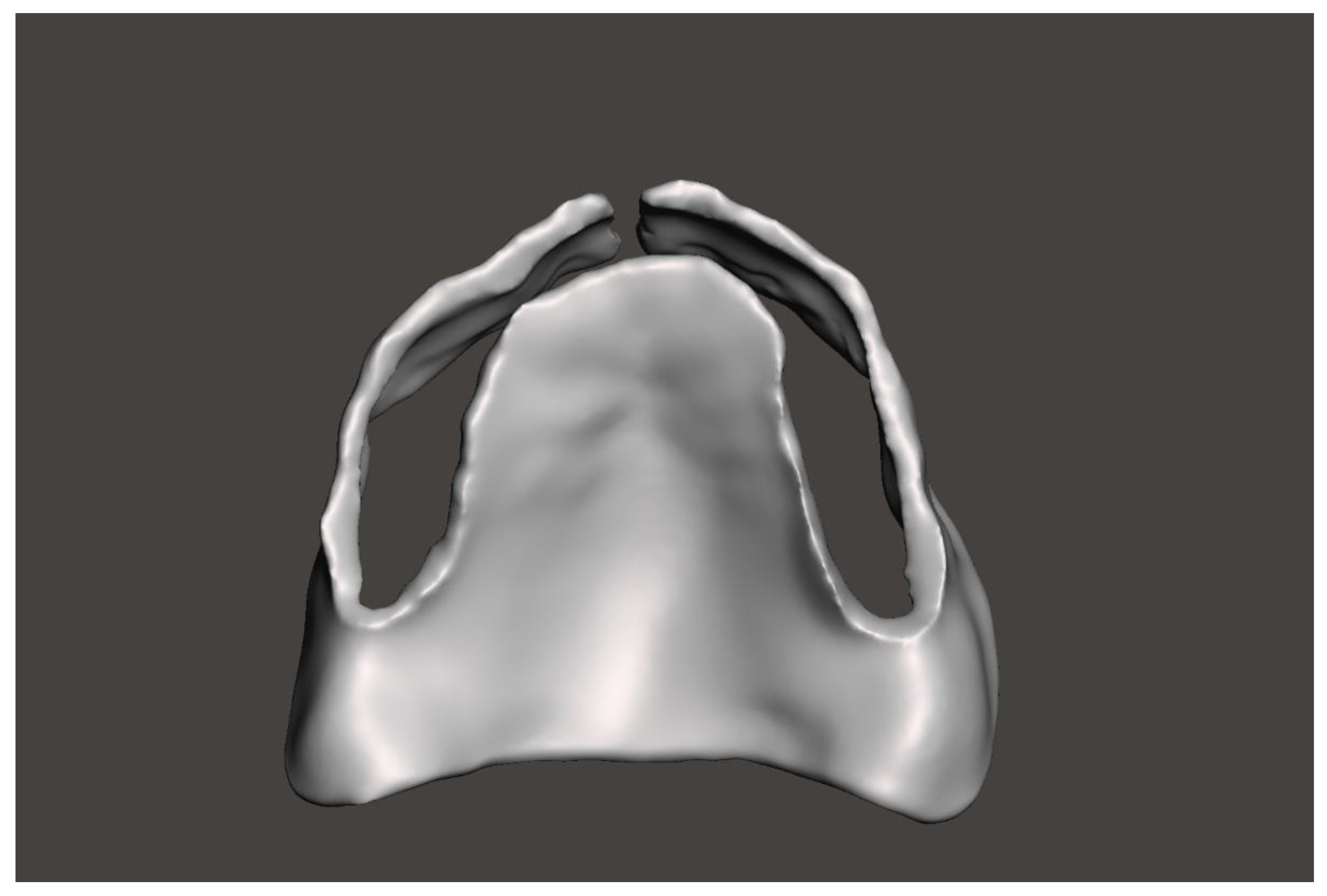
- Use the "Tooth Removal" tool to virtually extract the teeth, simulating the post-extraction ridge anatomy (Figure 2). This tool allows the user to define the long axis of each tooth and segment it from the digital cast. Once removed, the software automatically fills the socket area by generating a smooth surface over the extraction sites based on the contours of the adjacent gingiva. This virtual soft tissue approximation simulates the anticipated post-extraction ridge morphology. However, some bony projections may still remain visible after applying this tool. To ensure a more accurate and clinically appropriate representation of the post-extraction ridge, it is essential to carefully inspect the auto-generated model and manually refine the contours when necessary.Figure 2. Using the Tooth Removal Tool: (a) The tooth to be virtually extracted is selected; (b) The tooth is virtually extracted after selection.Figure 2. Using the Tooth Removal Tool: (a) The tooth to be virtually extracted is selected; (b) The tooth is virtually extracted after selection.
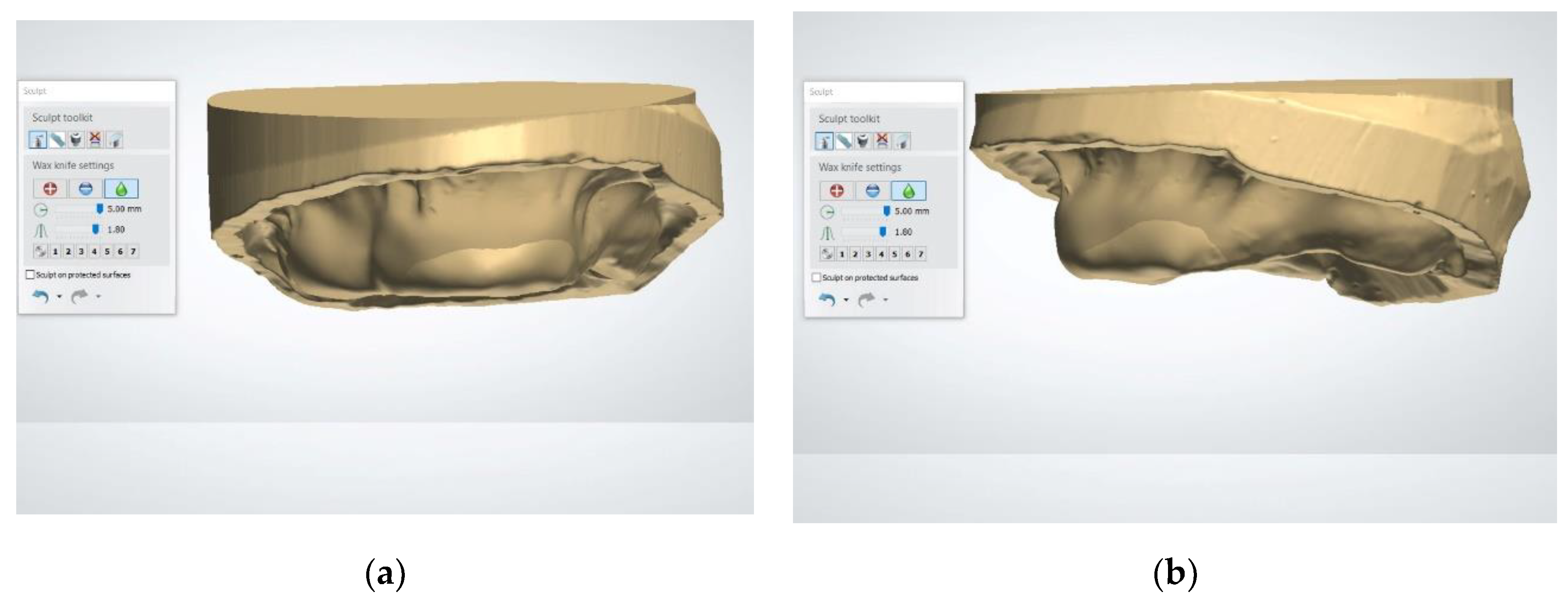
- Use the “Wax Knife” tool to digitally recontour the alveolar ridge. Create a smooth and contoured ridge surface, simulating the expected results of alveoloplasty (Figure 3). The Wax Knife tool offers two primary functions, remove and smooth, that allow for precise digital recontouring of the alveolar ridge. The remove function allows the user to selectively subtract excess material or virtual bony peaks that may protrude from the auto-generated surface, effectively mimicking surgical bone reduction. This is particularly helpful in areas where residual ridges appear irregular or sharp, which could interfere with prosthetic planning or guide stability. The smooth function, on the other hand, helps to blend and polish the surrounding areas by softening transitions and eliminating minor surface irregularities. This function is beneficial in creating a continuous, contoured ridge that mirrors the expected results of an alveoloplasty procedure. By alternating between the remove and smooth functions, clinicians can create a virtual ridge form that is both anatomically realistic and surgically feasible.Figure 3. The virtual alveolopasty procedure using the Wax Knife tool to remove the undercuts and irregular ridge contours: (a) Frontal view; (b) Lateral view.Figure 3. The virtual alveolopasty procedure using the Wax Knife tool to remove the undercuts and irregular ridge contours: (a) Frontal view; (b) Lateral view.
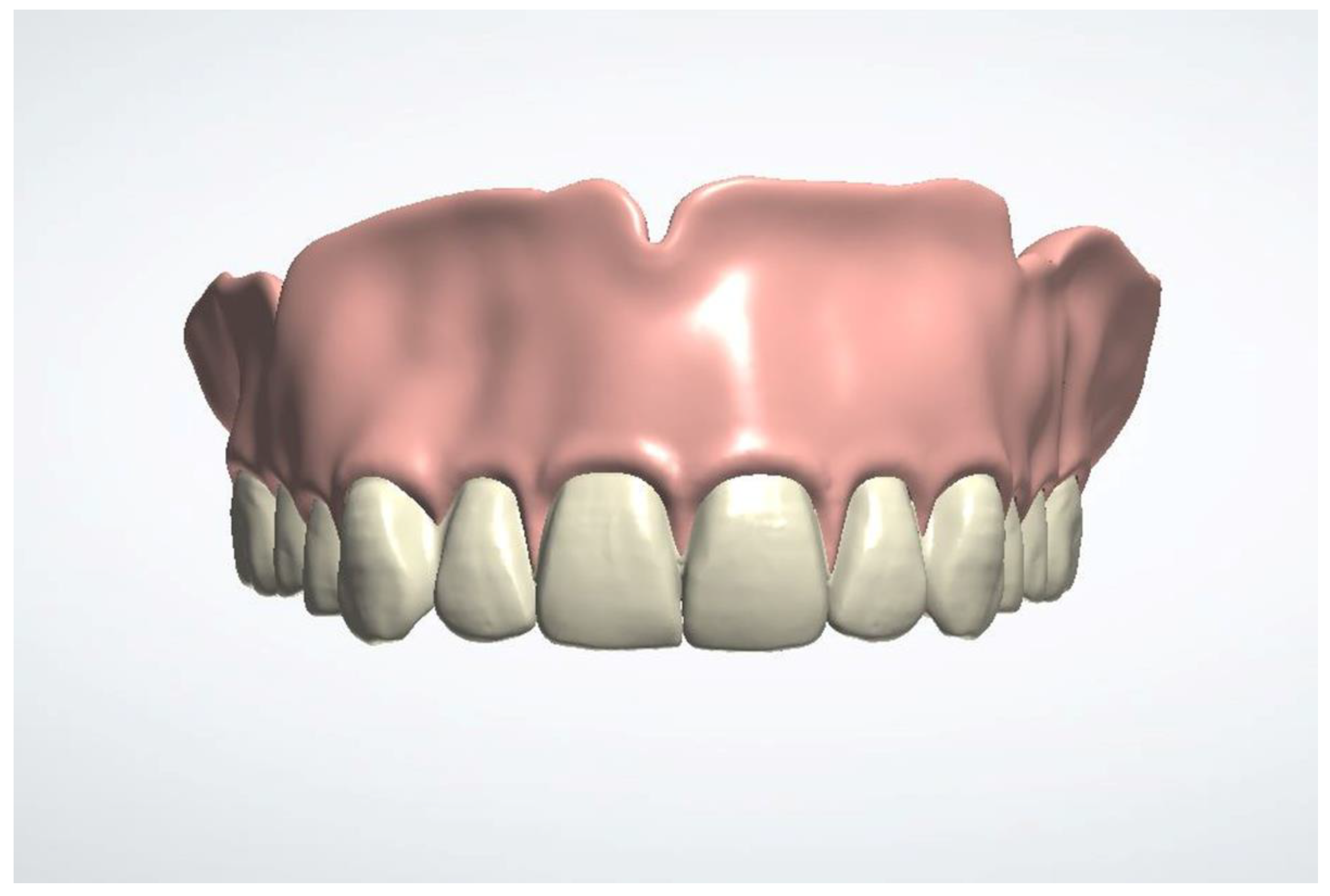
- Design the immediate denture (Figure 4). The recommended software settings for denture base design are as follows: use the natural wax template; set a 0.10 mm space between the denture base and the soft tissue; ensure a minimum thickness of 0.5 mm beneath the teeth; enable the "Remove Undercuts from Teeth Pockets" feature; and disable the "Drill Compensation of Teeth Pockets" option.Figure 4. The immediate denture is designed based of the new maxillary arch contours.
- Export the denture base in Standard triangle language (STL) format for modification (Figure 5).Figure 5. The denture base of the immediate denture design is segmented and exported in STL format.
- Import the STL file of the denture base into a universal CAD software (Meshmixer version 3.5; Autodesk). Create an occlusal slot to guide the surgical reduction. Add buccal cut to allow the seating of the guide during surgery. Use the buccal flange to guide and verify the buccal surgical reduction (Figure 6). Design these features using the following steps: First, use the “Select” tool to define the areas for the occlusal window and buccal slot. For the occlusal window, select the region corresponding to the teeth sockets on the denture base. For the buccal slot, extend the selection vertically from the midline of the occlusal window to the full depth of the denture base flange. Next, use the “Edit – Erase & Fill” tools to perform the initial cuts. Finally, smooth all transitions using the “Sculpt – Robust Smooth” tool, with a strength setting of 15–20%.Figure 6. The denture base of the immediate denture design is used to design the surgical guide using Autodesk Meshmixer. The surgical guide is designed with a buccal cut and occlusal slot. .Figure 6. The denture base of the immediate denture design is used to design the surgical guide using Autodesk Meshmixer. The surgical guide is designed with a buccal cut and occlusal slot. .
- Export the modified STL file for additive manufacturing (Pro 95s; Sprintray). Import it into the computer-aided manufacturing (CAM) software (RayWare software; version 2.8 or later; Sprintray). Select (NG Flex, Sprintray) as the material. Set the printing orientation at 30–45° with supports placed on non-critical surfaces. Use the following parameters on the 3D printer (Pro 95s; Sprintray): Layer Thickness: 100 microns, Support Density: 80%, Tip Size: 0.6 mm. Use a biocompatible flexible translucent material to fabricate the surgical guide (NG Flex, Sprintray) to allow the insertion underneath the undercut (Figure 7). Ensure the guide is free from defects and fits accurately. Fabricate a duplicate of the unmodified denture base STL file using the same settings and material to serve as verification stent.Figure 7. 3D-printed surgical guide: (a) Before adjustment, the flexibility of the selected material allows for the insertion of the guide underneath the undercut; (b) After adjustment, the width of the anterior slot is used to verify adequate buccal ridge augmentation.Figure 7. 3D-printed surgical guide: (a) Before adjustment, the flexibility of the selected material allows for the insertion of the guide underneath the undercut; (b) After adjustment, the width of the anterior slot is used to verify adequate buccal ridge augmentation.
- Use the verification stent to confirm proper ridge contours after alveoloplasty and before immediate denture placement (Figure 8).Figure 8. 3D-printed verification stent is used to verify the proper ridge contours. augmentation.
3. Results
4. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAD | Computer-aided design |
| CAM | Computer-aided manufacturing |
| STL | Standard triangle language |
| NG | Night guard |
| 3D | Three-dimensional |
References
- Dean, O.T. Surgery for the denture patient. J Am Dent Assoc 1936, 23, 2124–2128. [Google Scholar]
- Hillerup, S. Preprosthetic surgery in the elderly. J Prosthet Dent 1994, 72, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J Clin Med 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Nagata, K.; Fuchigami, K.; Hoshi, N.; Atsumi, M.; Kimoto, K.; Kawana, H. Accuracy of guided surgery using the silicon impression and digital impression method for the mandibular free end: a comparative study. Int J Implant Dent 2021, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Bourgoyne, J.R. Alveoloplasty in preparation for the immediate denture insertion. J Prosthet Dent 1951, 1, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Komagamine, Y.; Kanazawa, M.; Sasaki, Y.; Sato, Y.; Minakuchi, S. Prognoses of new complete dentures from the patient’s denture assessment of existing dentures. Clin Oral Investig 2017, 21, 1495–1501. [Google Scholar] [CrossRef] [PubMed]
- Hyde, T.P. Case report: differential pressure impressions for complete dentures. Eur J Prosthodont Restor Dent 2003, 11, 5–8. [Google Scholar] [PubMed]
- Kelly, E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent 1972, 27, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.W.; Walmsley, A.D. A review of prosthodontic management of fibrous ridges. Br Dent J 2005, 199, 715–741. [Google Scholar] [CrossRef] [PubMed]
- Meyer, I. Alveoloplasty—the oral surgeon’s point of view. Oral Surg Oral Med Oral Pathol 1966, 22, 441–455. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Schaefer, O.; Thompson, G.A.; Guentsch, A. Comparison of Accuracy and Reproducibility of Casts Made by Digital and Conventional Methods. J Prosthet Dent 2015, 113, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Shabestari, G.O.; Zeighami, S.; Samadi, M.J.; Shamshiri, A.R. Effect of Storage Time of Extended-Pour and Conventional Alginate Impressions on Dimensional Accuracy of Casts. J Dent (Tehran) 2014, 11, 655–664. [Google Scholar]
- Punj, A.; Bompolaki, D.; Garaicoa, J. Dental Impression Materials and Techniques. Dent Clin North Am 2017, 61, 779–796. [Google Scholar] [CrossRef] [PubMed]
- Puryer, J.; Forbes-Haley, C.; Blewitt, I. Dental Management of the ‘Gagging’ Patient: Challenges and Strategies. Int J Dent Health Sci 2015, 3, 423–431. [Google Scholar]
- Yildirim-Bicer, A.Z.; Akarslan, Z.Z. Influence of Gag Reflex on Removable Prosthetic Restoration Tolerance According to the Patient Section of the Short Form of the Gagging Problem Assessment Questionnaire. J Adv Prosthodont 2014, 6, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Stromeyer, S.; Wiedemeier, D.; Mehl, A.; Ender, A. Time Efficiency of Digitally and Conventionally Produced Single-Unit Restorations. Dent J (Basel) 2021, 9, 62. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J. Accuracy of Casts Produced from Conventional and Digital Workflows: A Qualitative and Quantitative Analyses. J Adv Prosthodont 2019, 11, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Mu, M.; Yan, J.; Han, B.; Ye, R.; Guo, G. 3D printing materials and 3D printed surgical devices in oral and maxillofacial surgery: design, workflow and effectiveness. Regen Biomater 2024, 11, rbae066. [Google Scholar] [CrossRef] [PubMed]
- Rouzé l’Alzit, F.; Cade, R.; Naveau, A.; Babilotte, J.; Meglioli, M.; Catros, S. Accuracy of commercial 3D printers for the fabrication of surgical guides in dental implantology. J Dent 2022, 117, 103909. [Google Scholar] [CrossRef] [PubMed]
- Garza-Cisneros, A.N.; García-Pérez, M.M.; Rodriguez-Guajardo, W.J.; Elizondo-Riojas, G.; Negreros-Osuna, A.A. Cost-effective Solution for Maxillofacial Reconstruction Surgery with Virtual Surgical Planning and 3D Printed Cutting Guides Reduces Operative Time. Plast Surg (Oakv) 2024, 32, 70–77. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, E.O.; Pellizzer, E.P.; Goiatto, M.C.; Margonar, R.; Rocha, E.P.; Freitas, A.C., Jr.; Anchieta, R.B. Computer-guided surgery in implantology: review of basic concepts. J Craniofac Surg 2010, 21, 1917–1921. [Google Scholar] [CrossRef] [PubMed]
- Sayed, M.E.; Alshehri, A.H.; Al-Makramani, B.M.A.; Al-Sanabani, F.; Shaabi, F.I.; Alsurayyie, F.H.; Ahmed, W.M.; Al-Mansour, H.; Jain, S. Accuracy of Master Casts Generated Using Conventional and Digital Impression Modalities: Part 1—The Half-Arch Dimension. Appl Sci 2021, 11, 12034. [Google Scholar] [CrossRef]
- Cao, R.; Zhang, S.; Li, L.; et al. Accuracy of intraoral scanning versus conventional impressions for partial edentulous patients with maxillary defects. Sci Rep 2023, 13, 16773. [Google Scholar] [CrossRef] [PubMed]
- Rekow, E.D. Digital dentistry: The new state of the art - Is it disruptive or destructive? Dent Mater 2020, 36, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Shibli, J.A.; Fortin, T. Digital dentistry: New materials and techniques. Int J Dent 2016, 2016, 5261247. [Google Scholar] [CrossRef] [PubMed]
- de Magalhães, A.A.; Santos, A.T. Advancements in Diagnostic Methods and Imaging Technologies in Dentistry: A Literature Review of Emerging Approaches. J Clin Med 2025, 14, 1277. [Google Scholar] [CrossRef] [PubMed]
- Suese, K. Progress in digital dentistry: The practical use of intraoral scanners. Dent Mater J 2020, 39, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Revilla-Leon, M.; Frazier, K.; Da Costa, J.B.; Kumar, P.; Duong, M.-L.; Khajotia, S.; Urquhart, O. Intraoral scanners: An American dental association clinical evaluators panel survey. J Am Dent Assoc 2021, 152, 669–670.e2. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.M.; Horst, J.A. The Effect of New Oral Care Technologies on the Need for Dentists in 2040. J Dent Educ 2017, 81, eS126–eS132. [Google Scholar] [CrossRef] [PubMed]
- Ohyama, H.; Duong, M.L.; Yancoskie, A.E.; Smiley, A.B.; Syed, A.Z.; Reddy, M.S.; Bencharit, S.; Smiley, A.Z. Challenges and Opportunities in Implementing Digital Technology in Dental Curriculum: A Review and Perspective. Cureus 2025, 17, e83272. [Google Scholar] [CrossRef] [PubMed]
- van der Zande, M.M.; Gorter, R.C.; Bruers, J.J.M.; Aartman, I.H.A.; Wismeijer, D. Dentists’ opinions on using digital technologies in dental practice. Community Dent Oral Epidemiol 2018, 46, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Sônego, M.V.; Neto, C.L.M.M.; Dos Santos, D.M.; Moreno, A.L.D.M.; Bertoz, A.P.D.M.; Goiato, M.C. Quality of Life, Satisfaction, Occlusal Force, and Halitosis after Direct and Indirect Relining of Inferior Complete Dentures. Eur J Dent 2022, 16, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Gauci, M.O. Patient-Specific Guides in Orthopedic Surgery. Orthop Traumatol Surg Res 2022, 108, 103154. [Google Scholar] [CrossRef] [PubMed]
- Mistry, R.; Pisulkar, S.K.; Borle, A.B.; Godbole, S.; Mandhane, R. Stability in complete dentures: an overview. IOSR J Dent Med Sci 2018, 17, 36–41. [Google Scholar]
- Jain, P.; Rathee, M. Stability in Mandibular Denture; StatPearls Publishing LLC: Treasure Island, FL, USA, 2020. [Google Scholar]
- Bessadet, M.; Drancourt, N.; El Osta, N. Time Efficiency and Cost Analysis between Digital and Conventional Workflows for the Fabrication of Fixed Dental Prostheses: A Systematic Review. J Prosthet Dent 2024, 133, 71–84. [Google Scholar] [CrossRef] [PubMed]
- van Noort, R. The future of dental devices is digital. Dent Mater 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Róth, I.; Hermann, P.; Vitai, V.; Rózsa, N.; Madléna, M.; Borbély, J. Comparison of the Learning Curve of Intraoral Scanning with Two Different Intraoral Scanners Based on Scanning Time. BMC Oral Health 2023, 23, 267. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S.M.; Chaturvedi, S.; Alahmari, M.A.; Alaleyani, A.M.; Alqahtani, A.A.; Sahal, A.A.; Salem, M. Digital Impression (Intraoral Scanners) and Factors Affecting Its Accuracy—An Insight into Knowledge and Awareness Amongst Graduates and Clinical Practitioners. BMC Oral Health 2024, 24, 1323. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



