Submitted:
07 July 2025
Posted:
08 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Measures
2.4. Procedure
2.5. Analysis
2.6. Reflexivity & Trustworthiness
3. Results
3.1. Participant Characteristics
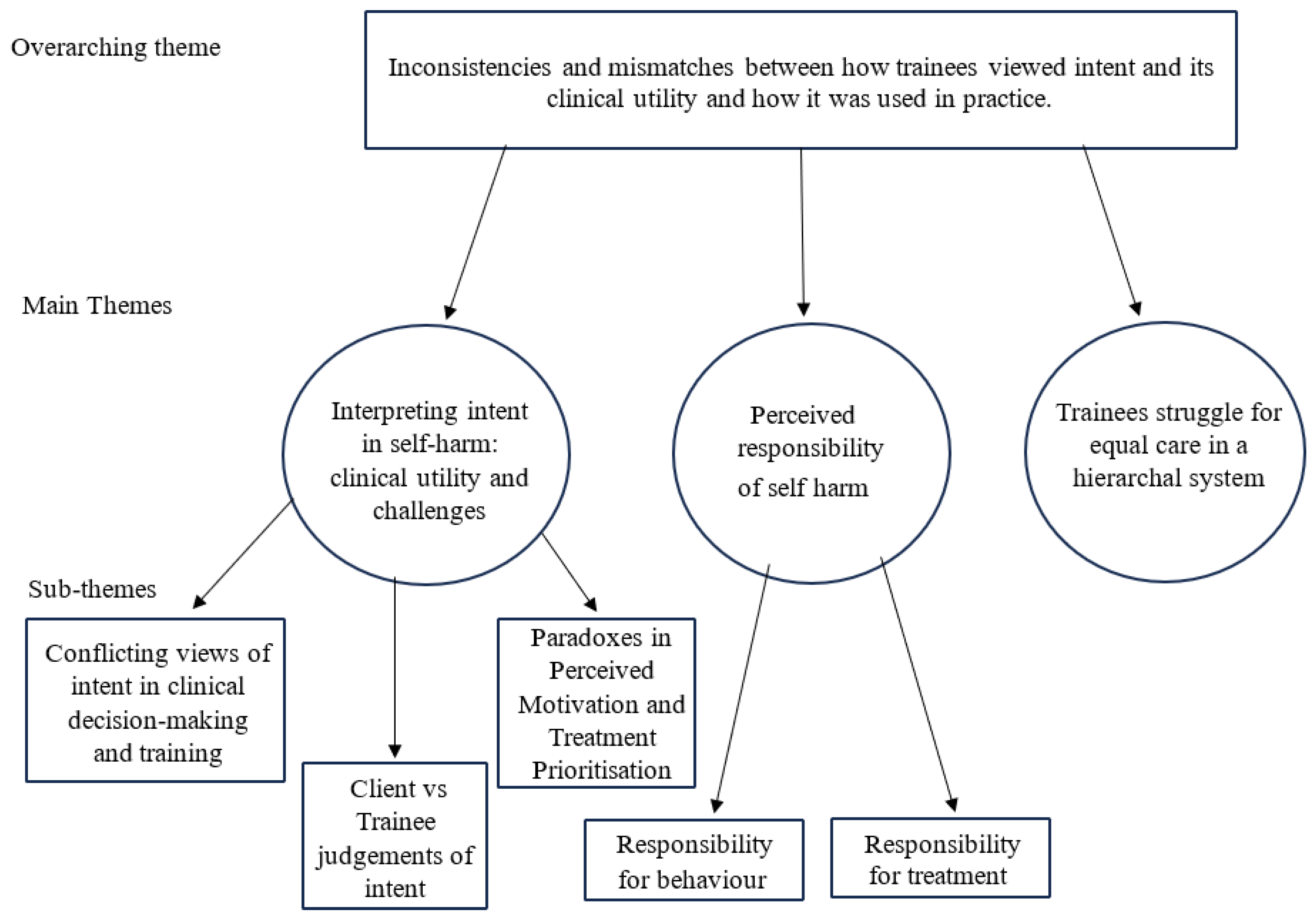
3.2. Thematic Analysis
3.2.1. Interpreting Intent in Self-Harm: Clinical Utility and Challenges
Conflicting Views of Intent in Clinical Decision-Making and Training
Client vs Trainee Judgements of Intent
Paradoxes in Perceived Motivation and Treatment Prioritization
3.2.2. Perceived Responsibility of Self-harm
Responsibility for Behaviour
Responsibility for Treatment
3.2.3. Trainees Struggle for Equal Care in a Hierarchical System
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- NICE. (2022). Self-harm: assessment, management and preventing recurrence. National Institute for Health and Care Excellence.
- Knipe, D. , et al. Self-harm and suicide in low- and middle-income countries. The Lancet Psychiatry 2022, 9, 97–109. [Google Scholar]
- McManus, S. , et al. (2016). Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014. NHS Digital.
- Link, B. G. , & Phelan, J. C. Conceptualizing stigma. Annual Review of Sociology 2001, 27, 363–385. [Google Scholar]
- Guerrero-Diaz, M. The stigma of self-harm: public perceptions and professional bias. Journal of Mental Health 2021, 30, 421–429. [Google Scholar]
- Lloyd, C. , Blazely, A., & Phillips, L. Stigma in self-injury: The views of young people who self-injure. Journal of Youth Studies 2018, 21, 620–635. [Google Scholar]
- Newton, B. , & Bale, C. Self-harm and stigma: A qualitative study of perceptions. Clinical Psychology Forum 2012, 233, 24–28. [Google Scholar]
- Brickell, T. A. , & McLean, C. Emerging issues and challenges for improving patient safety in mental health: A qualitative analysis of expert perspectives. Journal of Patient Safety 2011, 7, 39–44. [Google Scholar]
- Alonzo, D. , & Pratto, D. The stigma of self-injury among healthcare providers. Community Mental Health Journal 2021, 57, 1132–1139. [Google Scholar]
- Michall, C. , Tait, L., & Churchill, R. Stigma towards people who self-harm: attitudes of nurses in a UK mental health trust. Mental Health Practice 2017, 20, 28–35. [Google Scholar]
- Rees, N. , et al. Attitudes of healthcare staff towards people who self-harm. The British Journal of Psychiatry 2014, 205, 41–46. [Google Scholar]
- Rees, N. , et al. Staff attitudes towards people who self-harm: A multi-site evaluation. Journal of Psychiatric and Mental Health Nursing 2018, 25, 31–40. [Google Scholar]
- McGough, P. , et al. Emergency nurses' attitudes towards people who self-harm: An observational study. International Emergency Nursing 2022, 59, 101048. [Google Scholar]
- O’Keeffe, S. , et al. Patients' experiences of self-harm and stigma in healthcare settings. BMJ Open 2021, 11, e042763. [Google Scholar]
- Storey, P. , et al. Patients who present with self-harm: Clinical attitudes and stigma. British Journal of Psychiatry 2005, 187, 68–73. [Google Scholar]
- Akinola, M. , & Rayner, G. Stigma and self-harm: Service users' experiences. Journal of Mental Health 2022, 31, 345–352. [Google Scholar]
- Oliver, C. , et al. Understanding service users’ experiences of stigma following self-harm. Journal of Mental Health 2014, 23, 85–89. [Google Scholar]
- Masuku, N. The refusal of care for individuals who self-harm: A critical review. Nursing Ethics 2019, 26, 1041–1051. [Google Scholar]
- Rayner, G. , et al. Healthcare staff responses to people who self-harm: A mixed-method review. International Journal of Nursing Studies 2019, 98, 73–85. [Google Scholar]
- Taylor, T. L. Attitudes towards self-harm: An investigation of the views of healthcare professionals. Journal of Psychiatric and Mental Health Nursing 2009, 16, 60–65. [Google Scholar]
- Bergen, H. , et al. Neglecting psychological needs after self-harm: A qualitative study. Social Psychiatry and Psychiatric Epidemiology 2023, 58, 497–506. [Google Scholar]
- Chapman, A. L. , & Martin, E.R. Stigma and help-seeking for self-injury. Journal of Nervous and Mental Disease 2014, 202, 536–543. [Google Scholar]
- McManus, S. , et al. Prevalence, patterns, and correlates of self-harm: Findings from the Adult Psychiatric Morbidity Survey 2014. BJPsych Open 2019, 5, e90. [Google Scholar]
- Frost, M. , et al. Stigma and help-seeking behaviour for self-harm: A systematic review. BMJ Open 2015, 5, e007888. [Google Scholar]
- Halicka, J. , & Kiejna, A. Non-suicidal self-injury and suicide attempts: Different or similar phenomena? Psychiatria Polska 2015, 49, 751–764. [Google Scholar]
- Taylor, T. L. , et al. Functions of non-suicidal self-injury in young people: A systematic review. Clinical Child Psychology and Psychiatry 2018, 23, 578–593. [Google Scholar]
- Halicka, J. , & Kiejna, A. Suicidal behaviour and self-harm: Definitions and classification. Archives of Psychiatry and Psychotherapy 2018, 20, 7–14. [Google Scholar]
- Samari, E. , et al. Suicidal ideation in non-suicidal self-injury: A longitudinal study. Suicide and Life-Threatening Behavior 2020, 50, 1265–1273. [Google Scholar]
- Herzog, J. , et al. Suicidal ideation among adolescents engaging in non-suicidal self-injury: Prevalence and predictors. Journal of Affective Disorders 2022, 300, 15–22. [Google Scholar]
- Gouveia-Pereira, M. , et al. The continuum of self-harm intent: A narrative review. Clinical Psychology Review 2022, 90, 102107. [Google Scholar]
- Muehlenkamp, J.J. Self-injury and suicide behavior: A review for clinicians. Journal of Clinical Psychology 2014, 70, 279–291. [Google Scholar]
- Kapur, N. , et al. Classification of self-harm by intent: An ongoing debate. The Lancet Psychiatry 2013, 1, 4–5. [Google Scholar]
- Kar Ray, M. , et al. Clinical challenges in understanding changing suicidal intent. Psychiatric Bulletin 2020, 44, 112–117. [Google Scholar]
- Hawton, K. , et al. Assessment of suicide risk in self-harm patients. Psychological Medicine 2003, 33, 655–663. [Google Scholar]
- McGough, P. , et al. Emergency nurses and intent assessment: Barriers and priorities. Journal of Emergency Nursing 2021, 47, 739–747. [Google Scholar]
- Ogurin, D. , et al. Clinical importance of assessing self-harm intent. Archives of Suicide Research 2015, 19, 344–356. [Google Scholar]
- Butler, G. , & Malone, K. Non-suicidal self-injury vs suicide attempts in adolescents. Archives of Suicide Research 2013, 17, 197–210. [Google Scholar]
- Gardner, W. J. , et al. Differentiating self-harm: Intent and intervention. Crisis: The Journal of Crisis Intervention and Suicide Prevention 2021, 42, 231–239. [Google Scholar]
- Reynders, A. , et al. The impact of clinicians’ attitudes on self-harm care decisions. Suicide and Life-Threatening Behavior 2014, 44, 320–332. [Google Scholar]
- Corrigan, P.W. How stigma interferes with mental health care. American Psychologist 2003, 59, 614–625. [Google Scholar] [CrossRef]
- Smith, B. Controllability beliefs and stigma in self-harm. Journal of Mental Health 2016, 25, 224–230. [Google Scholar]
- Gale, M. , et al. Mental health professionals' perceptions of controllability of suicidal behaviour. Crisis 2016, 37, 294–300. [Google Scholar]
- Senf, B. , Maiwurm, D., & Fettel, D. Healthcare providers' attitudes towards suicidality in cancer patients. Palliative & Supportive Care 2022, 20, 12–18. [Google Scholar]
- Yue, Z. , et al. Psychiatric nurses' perceptions of non-suicidal self-injury: A qualitative study. International Journal of Mental Health Nursing 2024, 33, 89–98. [Google Scholar]
- Staniland, R. Perceived control and stigma in self-harm. Journal of Psychiatric and Mental Health Nursing 2021, 28, 784–791. [Google Scholar]
- Dawson, D. L. , et al. Stigma and self-harm in healthcare: A systematic review. British Journal of Clinical Psychology 2021, 60, 334–352. [Google Scholar]
- Malterud, K. , Siersma, V. D., & Guassora, A. D. Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research 2016, 26, 1753–1760. [Google Scholar] [CrossRef]
- Anderson, R. , Challenor, R., & Ford, T. Exploring healthcare professionals’ attitudes towards self-harm: The role of intent and stigma. Journal of Mental Health.
- Khan, M. , Roberts, R., & White, D. Understanding self-harm intent and stigma in clinical settings: A qualitative synthesis. International Journal of Mental Health Nursing 2021, 30, 123–132. [Google Scholar] [CrossRef]
- Owen, G. , Armstrong, M., & Johnstone, L. Perceived controllability of self-harm: A qualitative study with mental health practitioners. Psychology and Psychotherapy: Theory, Research and Practice 2017, 90, 80–95. [Google Scholar] [CrossRef]
- Eppich, W. , Gormley, G. , & Teunissen, P.W. Cross-pollination of clinical education and qualitative research: Transformative learning through dialogue. Academic Medicine 2019, 94, 507–511. [Google Scholar] [CrossRef]
- Braun, V. , & Clarke, V. Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- McEvoy, P. , & Richards, D. Critical realism: A way forward for evaluation research in nursing? Journal of Advanced Nursing 2003, 43, 411–420. [Google Scholar] [CrossRef]
- Koch, T. Establishing rigour in qualitative research: The decision trail. Journal of Advanced Nursing 2006, 53, 91–103. [Google Scholar] [CrossRef]
- O’Connor, R. C. , & Nock, M. K. The psychology of suicidal behaviour. The Lancet Psychiatry 2014, 1, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Cox, G. R. , Campbell, A., & Stallard, P. Risk factors for suicidal behavior in young people: A systematic review. Journal of Adolescence 2020, 84, 188–200. [Google Scholar] [CrossRef]
- Mughal, F. , McKenna, H., & Renfrew, M. J. False reassurance in mental health risk assessment: A qualitative study of trainee experiences. Journal of Clinical Psychology 2023, 79, 150–165. [Google Scholar] [CrossRef]
- Andersson, S. , Bakker, D., & Müller, V. Experiences of non-suicidal self-injury clients in mental health services: A qualitative analysis. Clinical Psychology Review 2024, 105, 102207. [Google Scholar]
- Shahwan, S. , Duhig, M., & Naicker, M. “We felt written off”: Client experiences of marginalization in self-harm care. Community Mental Health Journal 2022, 58, 630–640. [Google Scholar]
- Cully, G. , Corcoran, P., Leahy, D., Griffin, E., Dillon, C., Cassidy, E., Shiely, F., & Arensman, E. Method of self-harm and risk of self-harm repetition: findings from a national self-harm registry. Journal of Affective Disorders 2019, 246, 843–850. [Google Scholar] [CrossRef]
- McCabe, R. , Saeri, A., & Platz, E. Psychosocial interventions for suicidal behaviour in adults: A systematic review. BMJ Open 2018, 8, e024314. [Google Scholar]
- Mendez-Bustos, P. , Baca-Garcia, E., & Saiz-Ruiz, J. Psychological approaches to reducing suicide risk: A meta-analysis. Journal of Affective Disorders 2019, 243, 16–27. [Google Scholar] [CrossRef]
- Graney, J. , Simmons, M., & Bradley, C. The role of safety planning in suicide prevention: A review of implementation practices. Crisis 2020, 41, 96–104. [Google Scholar] [CrossRef]
- Nuji, N. , Venkatesan, S., & Saunders, D. Effectiveness of risk management strategies in clinical practice: A systematic review. Risk Management and Healthcare Policy 2021, 14, 37–48. [Google Scholar]
- Marchant, A. , Hawton, K., & Stewart, A. Self-harm in primary care: Patterns and predictors. British Journal of General Practice 2020, 70, e421–e428. [Google Scholar]
- Gibbs, L. , & Baker, H. Prioritising suicidal self-harm in clinical settings: A qualitative study. International Journal of Mental Health Nursing 2011, 20, 470–477. [Google Scholar] [CrossRef]
- Quinlivan, L. , Kannenberg, K., & Smith, J. Psychosocial assessments of self-cutting behaviour in adults. Social Psychiatry and Psychiatric Epidemiology 2022, 57, 521–530. [Google Scholar]
- Fortune, S. , Mulligan, M., & Stewart, L. Clinical prioritisation of self-harm in mental health services: Service-user perspectives. Journal of Mental Health 2021, 30, 19–27. [Google Scholar]
- Saunders, K. E. , Culpin, I., & John, A. Psychological distress in self-cutting adolescents. Journal of Child Psychology and Psychiatry 2012, 53, 113–121. [Google Scholar] [CrossRef]
- Perry, Y. , Hawton, K., & Lavender, T. Self-injury clinical outcomes: Why self-cutting may be underestimated. British Journal of Psychiatry 2020, 217, 519–524. [Google Scholar] [CrossRef]
- Whitlock, J. , Muehlenkamp, J., & Purington, A. Identification of self-injury: Role of clinician perceptions. Journal of Clinical Psychology 2013, 69, 982–992. [Google Scholar] [CrossRef]
- O’Connor, R. C. , & Kirtley, O. J. The lived experience of self-harm and clinician misinterpretation. Journal of Mental Health 2017, 26, 201–207. [Google Scholar]
- Garlow, S. J. , & Rosen, P. Clinician misalignment in self-harm care: An observational study. Psychiatric Services 2007, 58, 871–876. [Google Scholar]
- Allen, N. B. Self-harm, depression and autonomy: Understanding the link. Journal of Affective Disorders 2007, 100, 1–8. [Google Scholar] [CrossRef]
- Barr, D. , Leitner, B., & Thomas, S. Autonomy in self-harm and help-seeking: A qualitative study. Social Psychiatry and Psychiatric Epidemiology 2004, 39, 272–278. [Google Scholar]
- Rogers, M. L. , Gorday, E., & Joiner, T. E. Calculated suicidal behavior: Systematic review. Suicide and Life-Threatening Behavior 2021, 51, 234–247. [Google Scholar] [CrossRef]
- Paashaus, L. W. , Jansen, A., & Muris, P. Perceived control in self-harm: A cross-sectional study. BMC Psychiatry 2021, 21, 312. [Google Scholar]
- Lee, H. , & Hyun, M. H. Victim-perpetrator perspectives on intent: Self-harm analysis. Psychiatric Quarterly 2021, 92, 621–632. [Google Scholar]
- Floyd, J. Psychosocial dimensions of self-harm control: A review. Clinical Psychology Review 2019, 70, 95–108. [Google Scholar] [CrossRef]
- Fikke, L. R. , Jacobsen, N. H., & Helseth, S. Control beliefs in NSSI: A pilot study. Child and Adolescent Psychiatry and Mental Health 2011, 5, 28. [Google Scholar] [CrossRef]
- Jobes, D. A. , & Chalker, S.A. Fear of liability in suicide risk management: Implications for care. Journal of Psychiatric Practice 2019, 25, 35–44. [Google Scholar] [CrossRef]
- Bleich, S. , Ostroff, R., & Hammer, S. Professional anxiety and self-harm care: A phenomenological study. Journal of Psychiatric & Mental Health Nursing 2011, 18, 856–863. [Google Scholar] [CrossRef]
- Hoifodt, R. S. , & Talseth, A. G. Anxiety and accountability: Nurses’ experiences in acute care. Nursing Ethics 2006, 13, 588–600. [Google Scholar]
- Jobes, D. A. Managing clinician fear in suicide prevention: A clinical guide. Suicide and Life-Threatening Behavior 2020, 50, 30–46. [Google Scholar] [CrossRef]
- O’Keeffe, S. , Suzuki, M., Ryan, M. P., Hunter, J., & McCabe, R. Experiences of care for self-harm in the emergency department: Comparison of the perspectives of patients, carers and practitioners. BJPsych Open 2021, 7, e175. [Google Scholar] [CrossRef]
- Gamblin, D. , McNaughton, R., & Raby, N. (2024). Organisational barriers to targeted self-harm training. Journal of Health Services Research & Policy.
- Veresova, A. , Smith, P., & Martin, L. Training disparities in healthcare: System-level influences. Medical Education 2024, 58, 115–123. [Google Scholar] [CrossRef]
- Jahn, S. , Quinnet, J., & Ries, M. Resource constraints in mental health services: A UK perspective. Health Services Management Research 2016, 29, 145–153. [Google Scholar]
- Petrik, A. , Walker, N., & Molloy, D. Hierarchy and self-harm care: Staff perceptions. Journal of Psychiatric and Mental Health Nursing 2015, 22, 254–262. [Google Scholar] [CrossRef]
- Witt, A. , Bailey, K., & James, S. Systemic influences on mental health clinical decision-making. BMC Health Services Research 2023, 23, 12. [Google Scholar]
- Thexton, W. Clinical psychology training and preparation for multidisciplinary team working: a grounded theory model and the reframing of reflective practice (Doctoral dissertation, University of Birmingham).
- Leather, J. Z. , O'Connor, R. C., Quinlivan, L., Kapur, N., Campbell, S., & Armitage, C. J. Healthcare professionals’ implementation of national guidelines with clients who self-harm. Journal of psychiatric research 2020, 130, 405–411. [Google Scholar] [CrossRef]
- Woodford, R. , Spittal, M. J., Milner, A., McGill, K., Kapur, N., Pirkis, J., Mitchell, A., & Carter, G. Accuracy of clinician predictions of future self-harm: a systematic review and meta-analysis of predictive studies. Suicide and Life-Threatening Behavior 2019, 49, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Mulder, R. , Newton-Howes, G., & Coid, J. W. The futility of risk prediction in psychiatry. The British Journal of Psychiatry 2016, 209, 271–272. [Google Scholar] [CrossRef]
- Kool, N. , van Meijel, B., Koekkoek, B., van der Bijl, J., & Kerkhof, A. Improving communication and practical skills in working with inclients who self-harm: a pre-test/posttest study of the effects of a training programme. BMC psychiatry 2014, 14, 1–9. [Google Scholar]
- https://doi.org/10.1186/1471-244X-14-64. [CrossRef]
- Bellairs-Walsh, I. , Byrne, S. J., Bendall, S., Perry, Y., Krysinska, K., Lin, A., Michail, M., Lamblin, M., Li, T.Y., Hetrick, S., & Robinson, J. Working with young people at risk of suicidal behaviour and self-harm: A qualitative study of Australian General Practitioners’ perspectives. International journal of environmental research and public health 2021, 18, 12926. [Google Scholar] [CrossRef]
- Coppens, E. , Van Audenhove, C., Gusmão, R., Purebl, G., Székely, A., Maxwell, M., Koburger, N., Arensman, E., & Hegerl, U. Effectiveness of general practitioner training to improve suicide awareness and knowledge and skills towards depression. Journal of Affective Disorders 2017, 227, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Michail, M. , Tait, L., & Churchill, D. General practitioners' clinical expertise in managing suicidal young people: Implications for continued education. Primary Health Care Research and Development 2017, 18, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R. , Carson, J., & Houghton, T. Stigma towards non-suicidal self-harm: Evaluating a brief educational intervention. British Journal of Nursing 2019, 28, 307–312. [Google Scholar] [CrossRef]
- Karman, P. , Kool, N., Poslawsky, I.E., & Van Meijel, B. Nurses’ attitudes towards self-harm: a literature review. Journal of Psychiatric and Mental Health Nursing 2015, 22, 6575. [Google Scholar] [CrossRef]
- Parker, J. , & Davies, B. No blame no gain? From a no blame culture to a responsibility culture in medicine. Journal of Applied Philosophy 2020, 37, 646–660. [Google Scholar] [CrossRef]
- Belford, 2023 Belford, A. J. No blame policy is not no blame culture. bmj 2023, 383. [Google Scholar] [CrossRef]
- Pickard, H. , & Ward, L. (2013). Responsibility without blame: Philosophical reflections on clinical practice. In K. W. M. Fulford, and others (Eds.) The Oxford Handbook of Philosophy and Psychiatry. (pp. 1134–1152). Oxford Academic. [CrossRef]
- Østervang, C. , Touborg Lassen, A., Stenager, E., & Valdersdorf Jensen, M. Experiences of nursing care for patients who self-harm and suggestions for future practices: The perspectives of emergency care nurses. International Journal of Mental Health Nursing 2022, 31, 70–82. [Google Scholar] [CrossRef]
- Coulter, A. , Edwards, A., Elwyn, G., & Thomson, R. Implementing shared decision making in the UK. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen 2011, 105, 300–304. [Google Scholar] [CrossRef]
| Characteristic | N |
|---|---|
| Age M (SD) | 29.2 (8.02) |
| Gender | |
| Female | 14 |
| Non-binary | 1 |
| Ethnicity | |
| White | 15 |
| Programme | |
| DClinPsy1 | 5 |
| Mental Health Nursing | 3 |
| Medicine | 3 |
| TAPP2 | 2 |
| DCounPsy3 | 1 |
| NAP4 | 1 |
| Lived experience of self-harm | |
| Yes | 8 |
| No | 7 |
| Personally know someone who has self-harmed | |
| Yes, close family/friend | 12 |
| Yes, distant family/friend | 2 |
| No | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





