Submitted:
06 July 2025
Posted:
07 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measurement
2.2.1. Demographic Variable Questionnaire
2.2.2. Family Function Scale
2.2.3. Social Support Scale
2.2.4. Quality of Life Scale
2.2.5. Loneliness Scale
2.3. Data Collection and Analysis
2.3.1. Descriptive Statistics
2.3.2. Inferential Statistics
2.4. Ethical Considerations
3. Results
3.1. Study Sample Characteristics
3.2. Mediation Effect Analysis
3.2.1. Mediating Effect of Family Function, Social Support Satisfaction, and Quality of Life
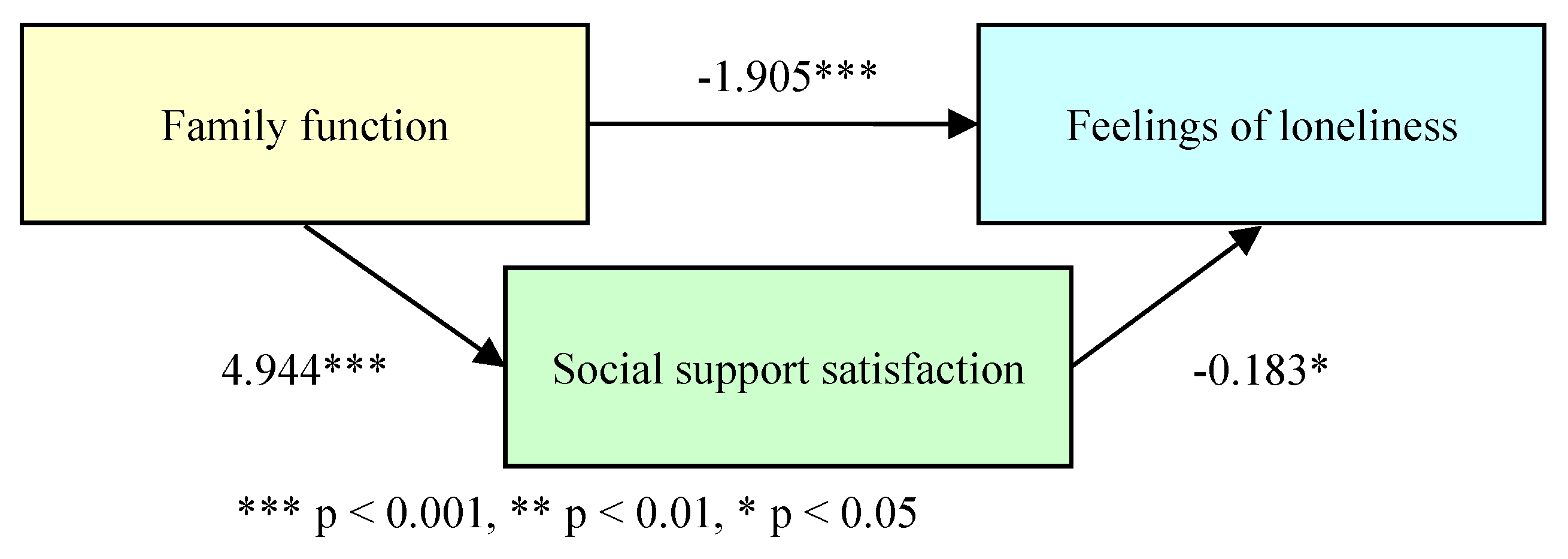
3.2.2. Mediating Effect of Family Function, Social Support Satisfaction, and Loneliness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The World Health Report: 2001 Mental health: New understanding, new hope; World Health Organization, 2001. https://iris.who. 1066.
- World Health Organization. Concepts in mental health; World Health Organization, 2022. https://www.who.
- Smilkstein, G. The physician and family function assessment. Family Systems Medicine. 1984, 2, 263–278. [Google Scholar] [CrossRef]
- Sawant, N. S.; Jethwani, K. S. Understanding family functioning and social support in unremitting schizophrenia: A study in India. Indian journal of psychiatry. 2010, 52, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Zhou Xiaozhen. The relationship between self-stigma, family function and disease prognosis in patients with mental illness; National Taiwan Normal University: Taipei, Taiwan, 2014; 28p. [Google Scholar]
- Farrel, E. L.; Feng, B.; Burleson, B. R. Supportive communication; In M., L. Knapp, M. L., Daly, J.A. (Eds.), Hand book of interpersonal communication (pp. 317–354). Thousand Oaks, CA: Sage, 2011. https://www.researchgate. 2833. [Google Scholar]
- Segrin, C.; Domschke, T. Social support, loneliness, recuperative processes, and their direct and indirect effects on health. Health communication. 2011, 26, 221–232. [Google Scholar] [CrossRef]
- Davidson, L.; Shahar, G.; Stayner, D. A.; Chinman, M. J.; Rakfeldt, J.; Tebes, J. K. Supported socialization for people with psychiatric disabilities: Lessons from a randomized controlled trial. Journal of Community Psychology. 2004, 32, 453–477. [Google Scholar] [CrossRef]
- Mueser, K. T.; Tarrier, N. Handbook of social functioning in schizophrenia; Allyn & Bacon, 1998. https://psycnet.apa. 1998. [Google Scholar]
- McCorkle, B. H.; Rogers, E. S.; Dunn, E. C.; Lyass, A.; Wan, Y. M. Increasing social support for individuals with serious mental illness: Evaluating the compeer model of intentional friendship. Community mental health journal. 2008, 44, 359–366. [Google Scholar] [CrossRef]
- Beels, C. C. Social support and schizophrenia. Schizophrenia Bulletin. 1981, 7, 58–72. [Google Scholar] [CrossRef]
- Buchanan, J. Social support and schizophrenia: a review of the literature. Archives of Psychiatric Nursing. 1995, 9, 68–76. [Google Scholar] [CrossRef]
- Gayer-Anderson, C.; Morgan, C. Social networks, support and early psychosis: a systematic review. Epidemiology and psychiatric sciences. 2013, 22, 131–146. [Google Scholar] [CrossRef]
- Cheng, J. J.; Kao, C.C. Quality of life of patients with mental illness and its measurement. Taiwan Psychiatry. 2005, 19, 179–191. https://www.airitilibrary. 1028. [Google Scholar]
- Dong, M.; Lu, L.; Zhang, L.; Zhang, Y. S.; Ng, C. H.; Ungvari, G. S.; Li, M.; Meng, X.; Xiang, Y. T. Quality of life in schizophrenia: A meta-analysis of comparative studies. Psychiatric Quarterly. 2019, 90, 519–532. [Google Scholar] [CrossRef]
- Desalegn, D.; Girma, S.; Abdeta, T. Quality of life and its association with psychiatric symptoms and socio-demographic characteristics among people with schizophrenia: A hospital-based cross-sectional study. Plos one. 2020, 15, e0229514. [Google Scholar] [CrossRef]
- Liao, H. Y.; Lee, Y.; Hsu, S. T.; Yen, C. F. Loneliness in patients with schizophrenia. Taiwanese Journal of Psychiatry. 2021, 35, 59–63. [Google Scholar] [CrossRef]
- Badcock, J. C.; Adery, L. H.; Park, S. Loneliness in psychosis: a practical review and critique for clinicians. Clinical Psychology: Science and Practice. 2020, 27, 1–13. [CrossRef]
- Fulford, D.; Mueser, K. T. The importance of understanding and addressing loneliness in psychotic disorders. Clinical Psychology: Science and Practice. 2020, 27, 1–3. [CrossRef]
- Brunt, D.; Hansson, L. The social networks of persons with severe mental illness in in-patient settings and supported community settings. Journal of Mental Health. 2002, 11, 611–621. [Google Scholar] [CrossRef]
- Goering, P.; Durbin, J.; Foster, R.; Boyles, S.; Babiak, T.; Lancee, B. Social networks of residents in supportive housing. Community Mental Health Journal. 1992, 28, 199–214. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, R. W.; Rollins, A. L.; Lehman, A. F. Social network correlates among people with psychiatric disabilities. Psychiatric Rehabilitation Journal. 2003, 26, 393–402. [Google Scholar] [CrossRef]
- Prince, J. D.; Oyo, A.; Mora, O.; Wyka, K.; Schonebaum, A. D. Loneliness among persons with severe mental illness. The Journal of nervous and mental disease. 2018, 206, 136–141. [Google Scholar] [CrossRef]
- Perese, E. F.; Wolf, M. Combating loneliness among persons with severe mental illness: social network interventions' characteristics, effectiveness, and applicability. Issues in mental health nursing. 2005, 26, 591–609. [Google Scholar] [CrossRef]
- Buzan, Tony. The Mind Map Book; Penguin Books, 2000. 2732.
- Smilkstein, G.; Ashworth, C.; Montano, D. Validity and reliability of the family APGAR as a test of family function J fam Pract. 1982, 15, 303–311. https://pubmed.ncbi.nlm.nih. 7097. [Google Scholar]
- Yang Zhengcheng. Research on Internet Addiction, Social Support and Life Adaptation of College Students; Tunghai University: Taichung, Taiwan, 2002. [Google Scholar]
- Huang Lilong. Related research on college students' self-esteem, social support and coping styles with love relationship conflicts; National Taichung University of Education: Taichung, Taiwan, 2012. [Google Scholar]
- Yao Kaiping. Introduction to the concept and measurement principles of health-related quality of life. Taiwan Medicine. 2002, 6, 183–192. [CrossRef]
- Ou Zhongming. Research on the quality of life and related factors of patients with schizophrenia - comparison with and without the use of home care; National Taipei University of Nursing and Health: Taipei, Taiwan, 2011. [Google Scholar]
- Development Team of the Taiwan Version of the World Health Organization Quality of Life Questionnaire. Introduction to the Development of the Taiwan Version of the World Health Organization Quality of Life Questionnaire. Chinese Journal of Public Health. 2000, 19, 315–324. [CrossRef]
- Russell, D.; Peplau, L. A.; Cutrona, C. E. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980, 39, 472–480. /: https. [CrossRef]
- Xie Mingjun. Research on the relationship between loneliness, social support and happiness among college students; National Taiwan Normal University: Taipei, Taiwan, 2015. [Google Scholar]
- Arnautovska, U.; Trott, M.; Vitangcol, K. J.; Milton, A.; Brown, E.; Warren, N.; Leucht, S.; Firth, J.; Siskind, D. Efficacy of User Self-Led and Human-Supported Digital Health Interventions for People with Schizophrenia: A Systematic Review and Meta-Analysis. Schizophrenia Bulletin. 2024, sbae143. [Google Scholar] [CrossRef]
- Yu, Y. H.; Peng, M. M.; Bai, X.; Luo, W.; Yang, X.; Li, J.; Liu, B.; Thornicroft, G.; Chan, C. L. W.; Ran, M. S. Schizophrenia, social support, caregiving burden and household poverty in rural China. Social Psychiatry and Psychiatric Epidemiology. 2020, 55, 1571–1580. [Google Scholar] [CrossRef]
- El-Monshed, A.; Amr, M. Association between perceived social support and recovery among patients with schizophrenia. International Journal of Africa Nursing Sciences. 2020, 13, 100236. [Google Scholar] [CrossRef]
- World Health Organization. Comprehensive Mental Health Action Plan 2013–2030; World Health Organization, 2021. https://www.who. 9789.
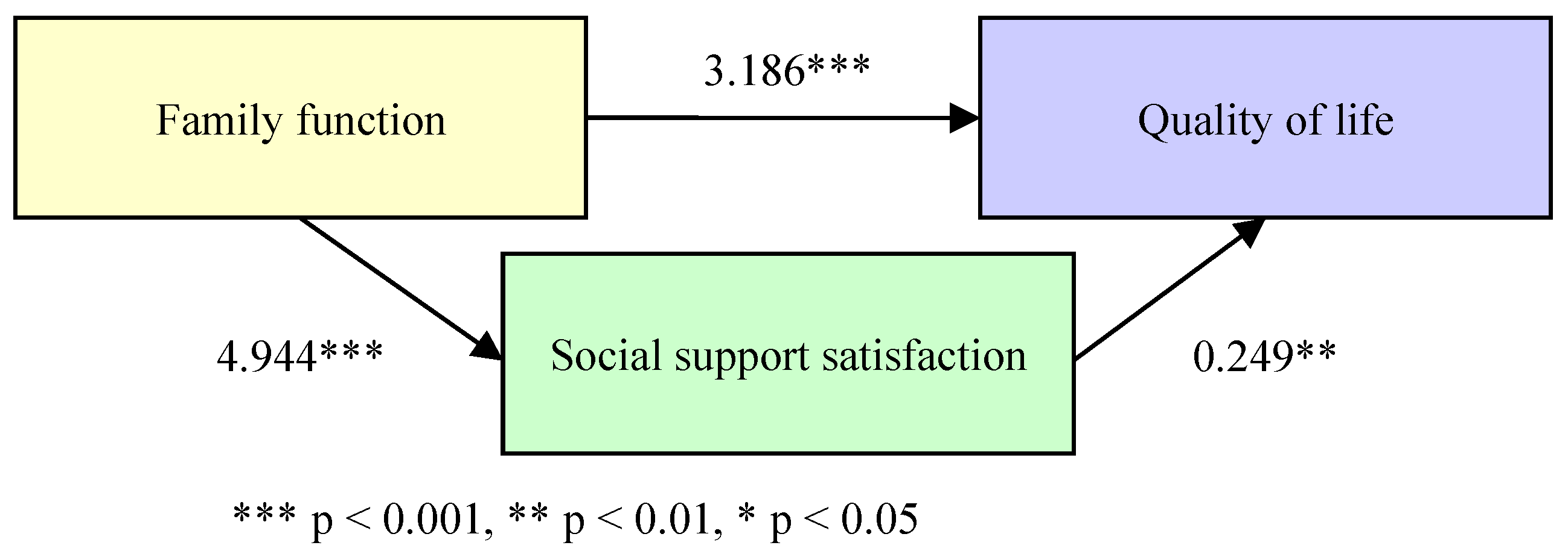
| Variables | β | SE | 95%C.I. | Bootstrap 95%C.I. | ||
| Lower | Upper | Lower | Upper | |||
| Family function→Quality of life | 3.186*** | 0.568 | 2.047 | 4.324 | 2.047 | 4.406 |
| Family function→Social support | 4.944*** | 0.752 | 3.438 | 6.451 | 3.470 | 6.359 |
| Family function→Social support→Quality of life | 0.249** | 0.076 | 0.096 | 0.402 | 0.123 | 0.387 |
| Effect | SE | 95%C.I. | Bootstrap 95%C.I. | |||
| Total effect | 4.418*** | 0.461 | 3.494 | 5.342 | ─ | ─ |
| Direct effect | ||||||
| Family function→Quality of life | 3.186*** | 0.568 | 2.047 | 4.324 | ─ | ─ |
| Indirect effect | ||||||
| Family function→Social support→Quality of life | 1.232*** | 0.332 | ─ | ─ | 0.627 | 1.931 |
| Variables | β | SE | 95%C.I. | Bootstrap 95%C.I. | ||
| Lower | Upper | Lower | Upper | |||
| Family function→Feelings of loneliness | -1.905*** | 0.520 | -2.947 | -0.862 | -2.784 | -0.981 |
| Family function→Social support | 4.944*** | 0.752 | 3.438 | 6.451 | 3.470 | 6.330 |
| Family function→Social support→Feelings of loneliness | -0.183* | 0.070 | -0.323 | -0.043 | -0.302 | -0.071 |
| Effect | SE | 95%C.I. | Bootstrap 95%C.I. | |||
| Total effect | -2.811*** | 0.409 | -3.632 | -1.991 | ─ | ─ |
| Direct effect | ||||||
| Family function→Feelings of loneliness | -1.905*** | 0.520 | -2.947 | -0.862 | ─ | ─ |
| Indirect effect | ||||||
| Family function→Social support→Feelings of loneliness | -0.906** | 0.313 | ─ | ─ | -1.571 | -0.337 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




