Submitted:
03 July 2025
Posted:
04 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Management of the Patients
2.3. Follow-Up
2.4. Study Variables
2.5. Statistical Analysis
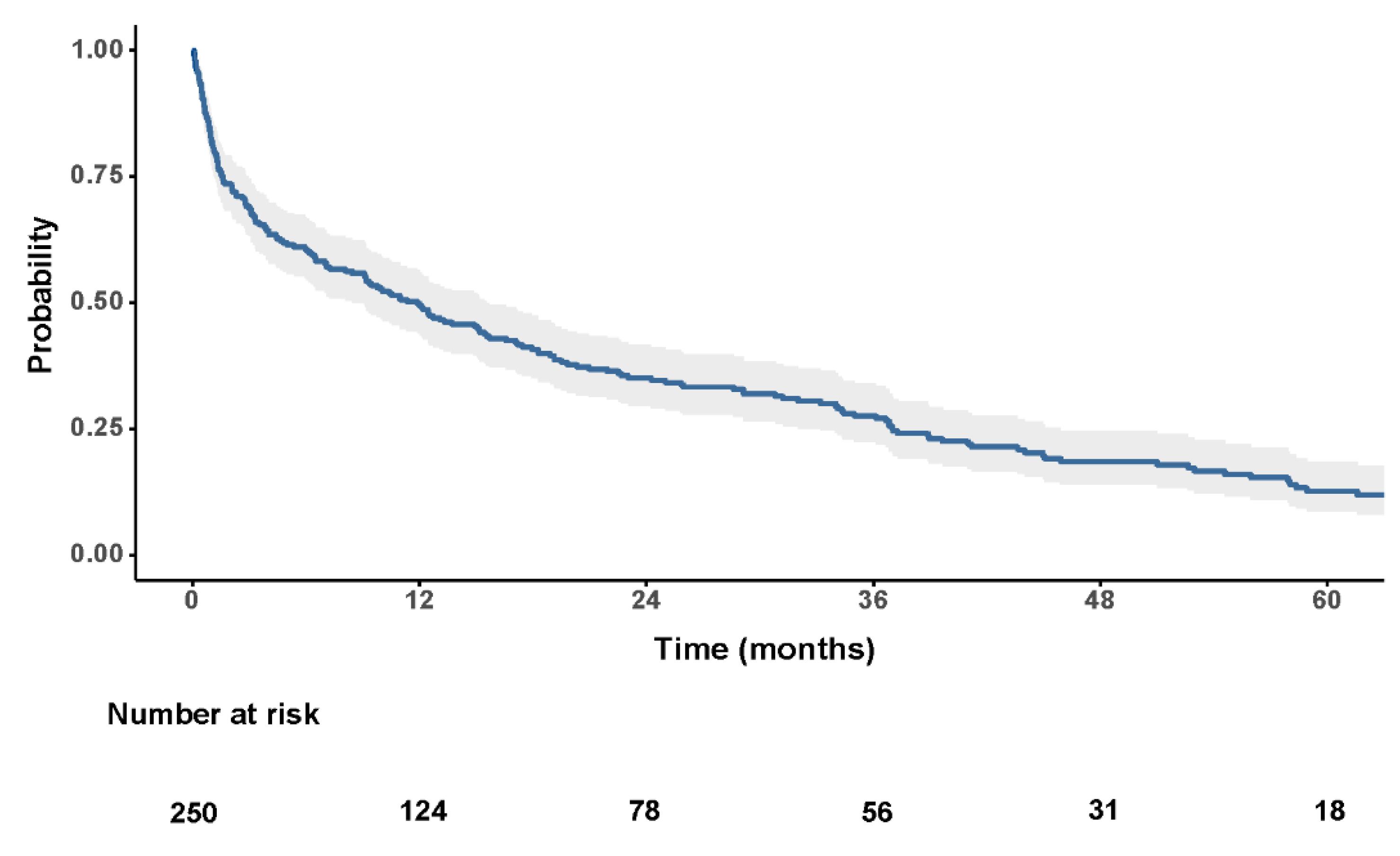
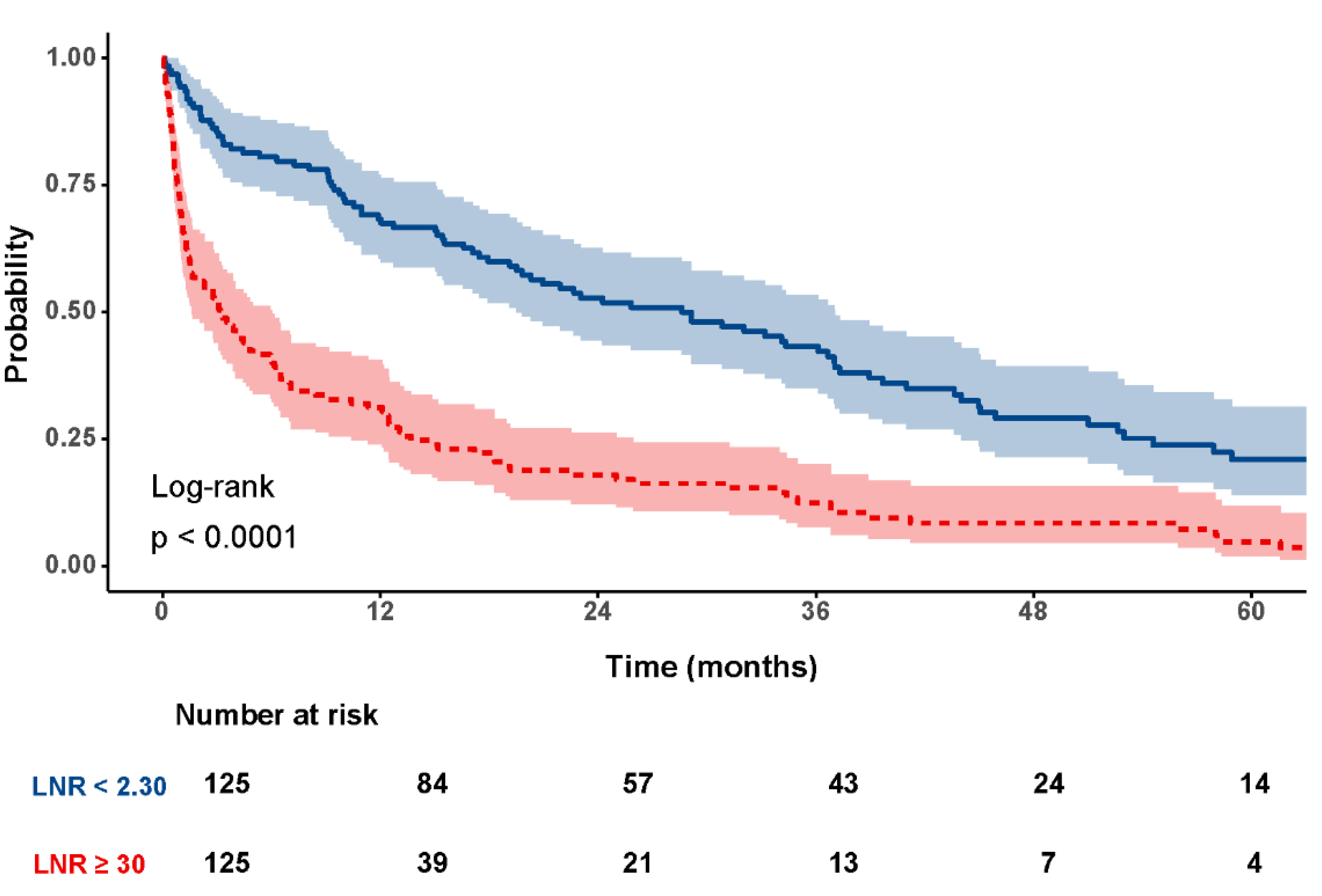
3. Results
3.1. Baseline Characteristics
3.2. Univariate Cox Regression Analysis
3.3. C-Index–Based Evaluation of Prognostic Variables
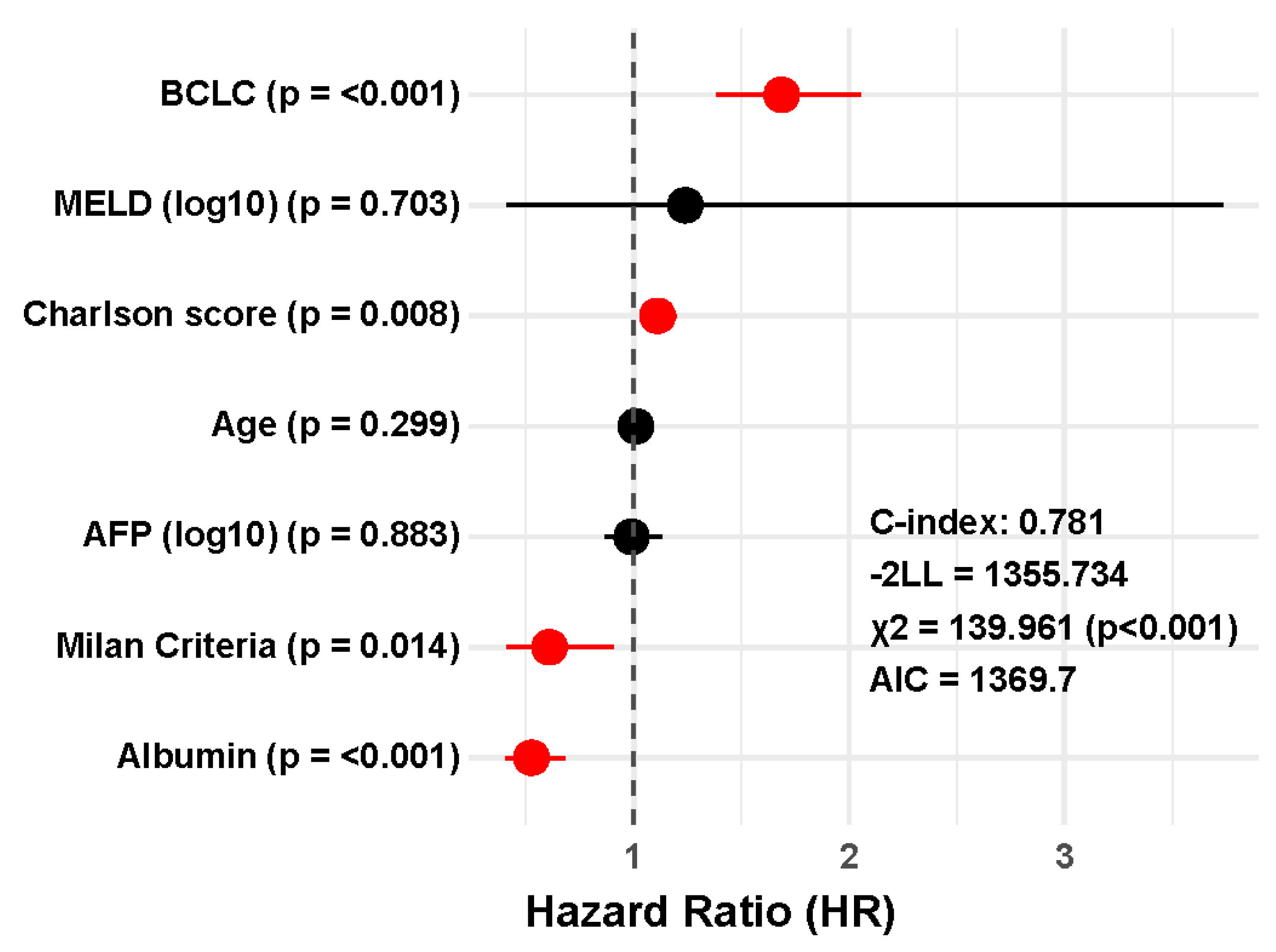
3.4. Multivariate Cox Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HCC | Hepatocellular carcinoma |
| BCLC | Barcelona Clinic Liver Cancer |
| AFP | Alpha-fetoprotein |
| MELD | Model for End-Stage Liver Disease |
| NLR | Neutrophil-to-lymphocyte ratio |
| PLR | Platelet-to-lymphocyte ratio |
| MLR | Monocyte-to-lymphocyte ratio |
| SIRI | Systemic Inflammation Response Index |
| SIII | Systemic Immune-inflammation Index |
| TACE | Transcatheter arterial chemoembolization |
| C-index | Harrell’s concordance index |
| AIC | Akaike Information Criterion |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2024, 74, 229–263. [Google Scholar] [CrossRef]
- de Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G.M. Global Burden of Cancer Attributable to Infections in 2018: A Worldwide Incidence Analysis. Lancet Glob Health 2020, 8, e180–e190. [Google Scholar] [CrossRef]
- Wang, J.; Qiu, K.; Zhou, S.; Gan, Y.; Jiang, K.; Wang, D.; Wang, H. Risk Factors for Hepatocellular Carcinoma: An Umbrella Review of Systematic Review and Meta-Analysis. Ann Med 2025, 57. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.G.; Llovet, J.M.; Yarchoan, M.; Mehta, N.; Heimbach, J.K.; Dawson, L.A.; Jou, J.H.; Kulik, L.M.; Agopian, V.G.; Marrero, J.A.; et al. AASLD Practice Guidance on Prevention, Diagnosis, and Treatment of Hepatocellular Carcinoma. Hepatology 2023, 78, 1922–1965. [Google Scholar] [CrossRef]
- Tan, D.J.H.; Setiawan, V.W.; Ng, C.H.; Lim, W.H.; Muthiah, M.D.; Tan, E.X.; Dan, Y.Y.; Roberts, L.R.; Loomba, R.; Huang, D.Q. Global Burden of Liver Cancer in Males and Females: Changing Etiological Basis and the Growing Contribution of NASH. Hepatology 2023, 77, 1150–1163. [Google Scholar] [CrossRef]
- Siegel, R.L.; Kratzer, T.B.; Giaquinto, A.N.; Sung, H.; Jemal, A. Cancer Statistics, 2025. CA Cancer J Clin 2025, 75. [Google Scholar] [CrossRef] [PubMed]
- Giannini, E.G.; Farinati, F.; Ciccarese, F.; Pecorelli, A.; Rapaccini, G.L.; Di Marco, M.; Benvegnù, L.; Caturelli, E.; Zoli, M.; Borzio, F.; et al. Prognosis of Untreated Hepatocellular Carcinoma. Hepatology 2015, 61, 184–190. [Google Scholar] [CrossRef]
- Nevola, R.; Ruocco, R.; Criscuolo, L.; Villani, A.; Alfano, M.; Beccia, D.; Imbriani, S.; Claar, E.; Cozzolino, D.; Carlo Sasso, F.; et al. Predictors of Early and Late Hepatocellular Carcinoma Recurrence. World J Gastroenterol 2023, 29, 1243–1260. [Google Scholar] [CrossRef] [PubMed]
- Yilma, M.; Houhong Xu, R.; Saxena, V.; Muzzin, M.; Tucker, L.Y.; Lee, J.; Mehta, N.; Mukhtar, N. Survival Outcomes Among Patients With Hepatocellular Carcinoma in a Large Integrated US Health System. JAMA Netw Open 2024, 7, e2435066. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC Strategy for Prognosis Prediction and Treatment Recommendation: The 2022 Update. J Hepatol 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Kim, K.M.; Shim, S.G.; Sinn, D.H.; Song, J.E.; Kim, B.S.; Kim, H.G. Child-Pugh, MELD, MELD-Na, and ALBI Scores: Which Liver Function Models Best Predicts Prognosis for HCC Patient with Ascites? Scand J Gastroenterol 2020, 55, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Ota, M.; Komeda, K.; Iida, H.; Ueno, M.; Kosaka, H.; Nomi, T.; Tanaka, S.; Nakai, T.; Hokutou, D.; Matsumoto, M.; et al. The Prognostic Value of Preoperative Serum Markers and Risk Classification in Patients with Hepatocellular Carcinoma. Ann Surg Oncol 2023, 30, 2807–2815. [Google Scholar] [CrossRef]
- Brown, Z.J.; Tsilimigras, D.I.; Ruff, S.M.; Mohseni, A.; Kamel, I.R.; Cloyd, J.M.; Pawlik, T.M. Management of Hepatocellular Carcinoma: A Review. JAMA Surg 2023, 158, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Jeng, L.-B.; Chan, W.-L.; Teng, C.-F. Prognostic Significance of Serum Albumin Level and Albumin-Based Mono- and Combination Biomarkers in Patients with Hepatocellular Carcinoma. Cancers (Basel) 2023, 15, 1005. [Google Scholar] [CrossRef]
- Lin, S.; Hu, S.; Ran, Y.; Wu, F. Neutrophil-to-Lymphocyte Ratio Predicts Prognosis of Patients with Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Transl Cancer Res 2021, 10, 1667–1678. [Google Scholar] [CrossRef]
- Min, G.T.; Li, Y.M.; Yao, N.; Wang, J.; Wang, H.P.; Chen, W. The Pretreatment Neutrophil-Lymphocyte Ratio May Predict Prognosis of Patients with Liver Cancer: A Systematic Review and Meta-Analysis. Clin Transplant 2018, 32. [Google Scholar] [CrossRef]
- Ma, W.; Zhang, P.; Qi, J.; Gu, L.; Zang, M.; Yao, H.; Shi, X.; Wang, C.; Jiang, Y. Prognostic Value of Platelet to Lymphocyte Ratio in Hepatocellular Carcinoma: A Meta-Analysis. Sci Rep 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Chen, H.; Chen, Z.; Tan, J.; Wu, F.; Li, X. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Patients with Hepatocellular Carcinoma Receiving Curative Therapies: A Systematic Review and Meta-Analysis. BMC Cancer 2025, 25, 571. [Google Scholar] [CrossRef]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular Carcinoma. The Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- Pinto Marques, H.; Gomes da Silva, S.; De Martin, E.; Agopian, V.G.; Martins, P.N. Emerging Biomarkers in HCC Patients: Current Status. Int J Surg 2020, 82, 70–76. [Google Scholar] [CrossRef]
- Balkwill, F.; Mantovani, A. Inflammation and Cancer: Back to Virchow? The Lancet 2001, 357, 539–545. [Google Scholar] [CrossRef]
- Arvanitakis, K.; Mitroulis, I.; Germanidis, G. Tumor-Associated Neutrophils in Hepatocellular Carcinoma Pathogenesis, Prognosis, and Therapy. Cancers (Basel) 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. JNCI: Journal of the National Cancer Institute 2014, 106. [Google Scholar] [CrossRef]
- Li, B.; Zhou, P.; Liu, Y.; Wei, H.; Yang, X.; Chen, T.; Xiao, J. Platelet-to-Lymphocyte Ratio in Advanced Cancer: Review and Meta-Analysis. Clinica Chimica Acta 2018, 483, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Mo, D.C.; Liu, X.; Lv, Y.J.; Qin, Y.Q.; Xie, G.S. Is Monocyte-to-Lymphocyte Ratio the Best Systematic Inflammatory Biomarker for the Prognosis of Gastrointestinal Stromal Tumors? J Surg Oncol 2019, 119, 1024–1025. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-S.; Kim, S.Y.; Moon, A. C-Reactive Protein Signaling Pathways in Tumor Progression. Biomol Ther (Seoul) 2023, 31, 473–483. [Google Scholar] [CrossRef]
- Xu, H.; Ma, Y.; Deng, F.; Ju, W.; Sun, X.; Wang, H. The Prognostic Value of C-Reactive Protein/Albumin Ratio in Human Malignancies: An Updated Meta-Analysis. Onco Targets Ther 2017, Volume 10, 3059–3070. [Google Scholar] [CrossRef]
- Qi, Q.; Zhuang, L.; Shen, Y.; Geng, Y.; Yu, S.; Chen, H.; Liu, L.; Meng, Z.; Wang, P.; Chen, Z. A Novel Systemic Inflammation Response Index (SIRI) for Predicting the Survival of Patients with Pancreatic Cancer after Chemotherapy. Cancer 2016, 122, 2158–2167. [Google Scholar] [CrossRef]
- van ’t Land, F.R.; Aziz, M.H.; Michiels, N.; Mieog, J.S.D.; Bonsing, B.A.; Luelmo, S.A.C.; Homs, M.Y.V.; Groot Koerkamp, B.; Papageorgiou, G.; van Eijck, C.H.J. Increasing Systemic Immune-Inflammation Index During Treatment in Patients With Advanced Pancreatic Cancer Is Associated With Poor Survival: A Retrospective, Multicenter, Cohort Study. Ann Surg 2023, 278, 1018–1023. [Google Scholar] [CrossRef]
- Proctor, M.J.; Morrison, D.S.; Talwar, D.; Balmer, S.M.; Fletcher, C.D.; O’reilly, D.S.J.; Foulis, A.K.; Horgan, P.G.; Mcmillan, D.C. A Comparison of Inflammation-Based Prognostic Scores in Patients with Cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 2011, 47, 2633–2641. [Google Scholar] [CrossRef]
- Hashimoto, K.; Ikeda, Y.; Korenaga, D.; Tanoue, K.; Hamatake, M.; Kawasaki, K.; Yamaoka, T.; Iwatani, Y.; Akazawa, K.; Takenaka, K. The Impact of Preoperative Serum C-reactive Protein on the Prognosis of Patients with Hepatocellular Carcinoma. Cancer 2005, 103, 1856–1864. [Google Scholar] [CrossRef]
- Gomez, D.; Farid, S.; Malik, H.Z.; Young, A.L.; Toogood, G.J.; Lodge, J.P.A.; Prasad, K.R. Preoperative Neutrophil-to-Lymphocyte Ratio as a Prognostic Predictor after Curative Resection for Hepatocellular Carcinoma. World J Surg 2008, 32, 1757–1762. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Wu, F.; Du, L.; Dong, Y.; Lin, S. Significant Association between High Neutrophil-Lymphocyte Ratio and Poor Prognosis in Patients with Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Front Immunol 2023, 14, 1211399. [Google Scholar] [CrossRef]
- Giannone, F.; Slovic, N.; Pessaux, P.; Schuster, C.; Baumert, T.F.; Lupberger, J. Inflammation-Related Prognostic Markers in Resected Hepatocellular Carcinoma. Front Oncol 2023, 13, 1267870. [Google Scholar] [CrossRef]
- Minici, R.; Venturini, M.; Guzzardi, G.; Fontana, F.; Coppola, A.; Piacentino, F.; Torre, F.; Spinetta, M.; Maglio, P.; Guerriero, P.; et al. A Multicenter International Retrospective Investigation Assessing the Prognostic Role of Inflammation-Based Scores (Neutrophil-to-Lymphocyte, Lymphocyte-to-Monocyte, and Platelet-to-Lymphocyte Ratios) in Patients with Intermediate-Stage Hepatocellular Carcinoma (HCC) Undergoing Chemoembolizations of the Liver. Cancers (Basel) 2024, 16, 1618. [Google Scholar] [CrossRef]
- Halazun, K.J.; Hardy, M.A.; Rana, A.A.; Woodland IV, D.C.; Luyten, E.J.; Mahadev, S.; Witkowski, P.; Siegel, A.B.; Brown, R.S.; Emond, J.C. Negative Impact of Neutrophil-Lymphocyte Ratio on Outcome after Liver Transplantation for Hepatocellular Carcinoma. Ann Surg 2009, 250, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J Chronic Dis 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Qi, X.; Guo, X. Child-Pugh Versus MELD Score for the Assessment of Prognosis in Liver Cirrhosis: A Systematic Review and Meta-Analysis of Observational Studies. Medicine 2016, 95. [Google Scholar] [CrossRef]
- van ’t Land, F.R.; Aziz, M.H.; Michiels, N.; Mieog, J.S.D.; Bonsing, B.A.; Luelmo, S.A.C.; Homs, M.Y.V.; Groot Koerkamp, B.; Papageorgiou, G.; van Eijck, C.H.J. Increasing Systemic Immune-Inflammation Index During Treatment in Patients With Advanced Pancreatic Cancer Is Associated With Poor Survival: A Retrospective, Multicenter, Cohort Study. Ann Surg 2023, 278, 1018–1023. [Google Scholar] [CrossRef]
- Mazzaferro, V.; Regalia, E.; Doci, R.; Andreola, S.; Pulvirenti, A.; Bozzetti, F.; Montalto, F.; Ammatuna, M.; Morabito, A.; Gennari, L. Liver Transplantation for the Treatment of Small Hepatocellular Carcinomas in Patients with Cirrhosis. N Engl J Med 1996, 334, 693–700. [Google Scholar] [CrossRef]
- Brentnall, A.R.; Cuzick, J. Use of the Concordance Index for Predictors of Censored Survival Data. Stat Methods Med Res 2018, 27, 2359–2373. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E.; Lee, K.L.; Mark, D.B. Multivariable Prognostic Models: Issues in Developing Models, Evaluating Assumptions and Adequacy, and Measuring and Reducing Errors. Stat Med 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Shen, M.; Hu, P.; Donskov, F.; Wang, G.; Liu, Q.; Du, J. Tumor-Associated Neutrophils as a New Prognostic Factor in Cancer: A Systematic Review and Meta-Analysis. PLoS One 2014, 9, e98259. [Google Scholar] [CrossRef]
- Gregory, A.D.; Houghton, A.M.G. Tumor-Associated Neutrophils: New Targets for Cancer Therapy. Cancer Res 2011, 71, 2411–2416. [Google Scholar] [CrossRef]
- Lu, S.D.; Wang, Y.Y.; Peng, N.F.; Peng, Y.C.; Zhong, J.H.; Qin, H.G.; Xiang, B. De; You, X.M.; Ma, L.; Li, L.Q. Preoperative Ratio of Neutrophils to Lymphocytes Predicts Postresection Survival in Selected Patients with Early or Intermediate Stage Hepatocellular Carcinoma. Medicine (United States) 2016, 95. [Google Scholar] [CrossRef]
- Zheng, J.; Seier, K.; Gonen, M.; Balachandran, V.P.; Kingham, T.P.; D’Angelica, M.I.; Allen, P.J.; Jarnagin, W.R.; DeMatteo, R.P. Utility of Serum Inflammatory Markers for Predicting Microvascular Invasion and Survival for Patients with Hepatocellular Carcinoma. Ann Surg Oncol 2017, 24, 3706–3714. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Bai, N.; Hu, X.; OuYang, X.W.; Yao, L.; Tao, Y.; Wang, Z. Preoperative Inflammatory Markers of NLR and PLR as Indicators of Poor Prognosis in Resectable HCC. PeerJ 2019, 7, e7132. [Google Scholar] [CrossRef] [PubMed]
- Dai, T.; Deng, M.; Ye, L.; Liu, R.; Lin, G.; Chen, X.; Li, H.; Liu, W.; Yang, Y.; Chen, G.; et al. Prognostic Value of Combined Preoperative Gamma-Glutamyl Transpeptidase to Platelet Ratio and Fibrinogen in Patients with HBV-Related Hepatocellular Carcinoma after Hepatectomy. Am J Transl Res 2020, 12, 2984. [Google Scholar]
- Wu, W.; Wang, Q.; Han, D.; Li, J.; Nie, Y.; Guo, D.; Yang, L.; Tao, K.; Zhang, X.; Dou, K. Prognostic Value of Preoperative Inflammatory Markers in Patients with Hepatocellular Carcinoma Who Underwent Curative Resection. Cancer Cell Int 2021, 21, 500. [Google Scholar] [CrossRef]
- Silva, J.P.M.; Coelho, F.F.; Cassenote, A.J.F.; Jeismann, V.B.; Fonseca, G.M.; Kruger, J.A.P.; de Meira Júnior, J.D.; Nahas, S.C.; Herman, P. Preoperative Inflammatory Markers as Prognostic Predictors after Hepatocellular Carcinoma Resection: Data from a Western Referral Center. BMC Surg 2022, 22, 329. [Google Scholar] [CrossRef]
- Zhou, J.; Yang, D. Changes in Inflammatory Markers Predict the Prognosis of Resected Hepatocellular Carcinoma with Child–Pugh A. Current Oncology 2022, 29, 5800–5809. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Li, X.; Geng, M.; Ye, X.; Liu, H.; Liu, Y.; Wan, G.; Wang, X. Pretreatment Neutrophil-Lymphocyte Ratio: An Independent Predictor of Survival in Patients with Hepatocellular Carcinoma. Medicine (United States) 2015, 94, e639. [Google Scholar] [CrossRef]
- Sullivan, K.M.; Groeschl, R.T.; Turaga, K.K.; Tsai, S.; Christians, K.K.; White, S.B.; Rilling, W.S.; Pilgrim, C.H.C.; Gamblin, T.C. Neutrophil-to-lymphocyte Ratio as a Predictor of Outcomes for Patients with Hepatocellular Carcinoma: A Western Perspective. J Surg Oncol 2014, 109, 95–97. [Google Scholar] [CrossRef]
- Li, S.C.; Xu, Z.; Deng, Y.L.; Wang, Y.N.; Jia, Y.M.; Ding, J. Higher Neutrophil-Lymphocyte Ratio Is Associated with Better Prognosis of Hepatocellular Carcinoma. Medicine (United States) 2020, 99, E20919. [Google Scholar] [CrossRef]
- Xiao, W.-K.; Chen, D.; Li, S.-Q.; Fu, S.-J.; Peng, B.-G.; Liang, L.-J. Prognostic Significance of Neutrophil-Lymphocyte Ratio in Hepatocellular Carcinoma: A Meta-Analysis. BMC Cancer 2014, 14, 117. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Li, J.; Deng, H.; Li, H.; Su, C.; Guo, X. Neutrophil-to-Lymphocyte Ratio for the Prognostic Assessment of Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis of Observational Studies. Oncotarget 2016, 7, 45283–45301. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Si, G.; Zhu, F.; Hui, J.; Cai, S.; Huang, C.; Cheng, S.; Fathy, A.H.; Xiang, Y.; Li, J. Prognostic Role of Platelet to Lymphocyte Ratio in Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Oncotarget 2017, 8, 22854–22862. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Cai, J.; Li, H.; Zeng, K.; He, L.; Fu, H.; Zhang, J.; Chen, L.; Yao, J.; Zhang, Y.; et al. Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio as Prognostic Predictors for Hepatocellular Carcinoma Patients with Various Treatments: A Meta-Analysis and Systematic Review. Cell Physiol Biochem 2017, 44, 967–981. [Google Scholar] [CrossRef]
- Hu, D.-H.; Yu, S.-M. Association between Platelet to Lymphocyte Ratio (PLR) and Overall Survival (OS) of Hepatocellular Carcinoma (HCC): A Meta-Analysis. Cell Mol Biol 2017, 63, 30–32. [Google Scholar] [CrossRef]
- Kim, H.; Choi, H.Z.; Choi, J.M.; Kang, B.M.; Lee, J.W.; Hwang, J.W. Sarcopenia with Systemic Inflammation Can Predict Survival in Patients with Hepatocellular Carcinoma Undergoing Curative Resection. J Gastrointest Oncol 2022, 13, 744–753. [Google Scholar] [CrossRef]
- Wang, Q.; Qiao, W.; Liu, B.; Li, J.; Yuan, C.; Long, J.; Hu, C.; Zang, C.; Zheng, J.; Zhang, Y. The Monocyte to Lymphocyte Ratio Not Only at Baseline but Also at Relapse Predicts Poor Outcomes in Patients with Hepatocellular Carcinoma Receiving Locoregional Therapy. BMC Gastroenterol 2022, 22, 98. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.X.; Ruan, D.Y.; Li, Y.; Wu, D.H.; Ma, X.K.; Chen, J.; Chen, Z.H.; Li, X.; Wang, T.T.; Lin, Q.; et al. Lymphocyte-to-Monocyte Ratio Predicts Survival of Patients with Hepatocellular Carcinoma after Curative Resection. World J Gastroenterol 2015, 21, 10898–10906. [Google Scholar] [CrossRef]
- Lin, S.; Lin, Y.; Fang, Y.; Mo, Z.; Hong, X.; Ji, C.; Jian, Z. Clinicopathological and Prognostic Value of Preoperative Lymphocyte to Monocyte Ratio for Hepatocellular Carcinoma Following Curative Resection. Medicine 2021, 100, e24153. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Tang, Z. Prognostic and Clinicopathological Significance of Systemic Inflammation Response Index in Patients with Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Front Immunol 2024, 15. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Huang, Y.; Lin, T. Prognostic Impact of Elevated Pre-Treatment Systemic Immune-Inflammation Index (SII) in Hepatocellular Carcinoma. Medicine 2020, 99, e18571. [Google Scholar] [CrossRef]
- Hu, B.; Yang, X.R.; Xu, Y.; Sun, Y.F.; Sun, C.; Guo, W.; Zhang, X.; Wang, W.M.; Qiu, S.J.; Zhou, J.; et al. Systemic Immune-Inflammation Index Predicts Prognosis of Patients after Curative Resection for Hepatocellular Carcinoma. Clin Cancer Res 2014, 20, 6212–6222. [Google Scholar] [CrossRef]
- Fu, H.; Zheng, J.; Cai, J.; Zeng, K.; Yao, J.; Chen, L.; Li, H.; Zhang, J.; Zhang, Y.; Zhao, H.; et al. Systemic Immune-Inflammation Index (SII) Is Useful to Predict Survival Outcomes in Patients after Liver Transplantation for Hepatocellular Carcinoma within Hangzhou Criteria. Cell Physiol Biochem 2018, 47, 293–301. [Google Scholar] [CrossRef]
- Lin, N.; Li, J.; Ke, Q.; Wang, L.; Cao, Y.; Liu, J. Clinical Significance of C-Reactive Protein to Albumin Ratio in Patients with Hepatocellular Carcinoma: A Meta-Analysis. Dis Markers 2020, 2020. [Google Scholar] [CrossRef]
- Uno, H.; Claggett, B.; Tian, L.; Inoue, E.; Gallo, P.; Miyata, T.; Schrag, D.; Takeuchi, M.; Uyama, Y.; Zhao, L.; et al. Moving Beyond the Hazard Ratio in Quantifying the Between-Group Difference in Survival Analysis. J Clin Oncol 2014, 32, 2380–2385. [Google Scholar] [CrossRef]
- McLernon, D.J.; Giardiello, D.; Van Calster, B.; Wynants, L.; van Geloven, N.; van Smeden, M.; Therneau, T.; Steyerberg, E.W.; McLernon, D.J.; Giardiello, D.; et al. Assessing Performance and Clinical Usefulness in Prediction Models with Survival Outcomes: Practical Guidance for Cox Proportional Hazards Models. Ann Intern Med 2023, 176, 105–114. [Google Scholar] [CrossRef]

| Variable | n (%) | Univariate Analysis (HR – CI 95%) |
p |
|---|---|---|---|
| Age (mean ± SD) | 68 (±10,4) | 1.03 (1.01 – 1.05) | <0.001* |
| Sex: - men - women |
195 (78,0) 55 (22,0) |
0.91 (0.65 – 1.26) | 0.561 |
| Charlson score (median – IQR) | 7 (6,0 – 9,0) | 1.27 (1.20 – 1.34) | <0.001* |
| Diabetes mellitus: - No - Yes |
133 (53.2) 117 (46.8) |
1.16 (0.89 – 1.53) | 0.277 |
| OH Chirrosis: - No - Yes |
170 (68.0) 80 (32.0) |
1.13 (0.85 – 1.52) | 0.397 |
| AFP (Log10) (ng/mL) (median – IQR) | 10.27 (3.15 – 428.46) | 1.33 (1.19 – 1.48) | <0.001* |
| Albumin (g/dL) (median – IQR) | 3,4 (2,8 – 4,0) | 0.46 (0.37 – 0.56) | <0.001* |
| Child classification: A B C |
127(50,8) 75 (30,0) 26 (10,4) |
2.49 (2.01 – 3.08) | <0.001* |
| Milan criteria: - No - Yes |
105 (42,0) 143 (57,2) |
0.36 (0.26 – 0.48) | <0.001* |
| BCLC classification: 0 A B C D |
11 (4,4) 101 (40,4) 49 (19,6) 57 (22,8) 32 (12,8) |
2.10 (1.93 – 2.40) | <0,001* |
| MELD score (median – IQR) | 10,04 (7,90 – 13,63) | 1.07 (1.04 – 1.10) | <0.001* |
| NLR (median – IQR) | 2,34 (1,5 – 3,9) | 1.12 (1.08 – 1.15) | <0.001* |
| PLR (median – IQR) | 94,92 (61,57 – 139,37) | 1.02 (1.01 – 1.03) | <0.001* |
| MLR (median – IQR) | 0.40 (0.28 – 0.59) | 1.21 (1.02 – 1.43) | 0.028* |
| SIRI (median – IQR) | 1.22 (0.74 – 2.49) | 1.07 (1.05 – 1.09) | <0.001* |
| SIII (Log10) (median – IQR) | 318.2 (160.0 – 587.3) | 2.30 (1.64 – 3.22) | <0.001* |
| Prognostic factor | C-index (Standar Error) | CI 95% |
| BCLC | 0.717 (0.017) | 0.684 – 0.750 |
| Albumine | 0.713 (0.020) | 0.674 – 0.752 |
| Charlson score | 0.672 (0.019) | 0.635 – 0.709. |
| NLR | 0.640 (0.016) | 0.609 – 0.671 |
| Milan criteria | 0.639 (0.016) | 0.608 – 0.670 |
| MELD score | 0.626 (0.023) | 0.581 – 0.671 |
| PLR | 0.605 (0.018) | 0.570 – 0.640 |
| SIII | 0.603 (0.018) | 0.568 – 0.638 |
| Age | 0.595 (0.022) | 0.537 – 0.623. |
| SIRI | 0.593 (0.0 18) | 0.558 – 0.628 |
| AFP | 0.592 (0.025) | 0.543 – 0.641 |
| MLR | 0.585 (0.017) | 0.552 – 0.618 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





