Submitted:
01 July 2025
Posted:
03 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
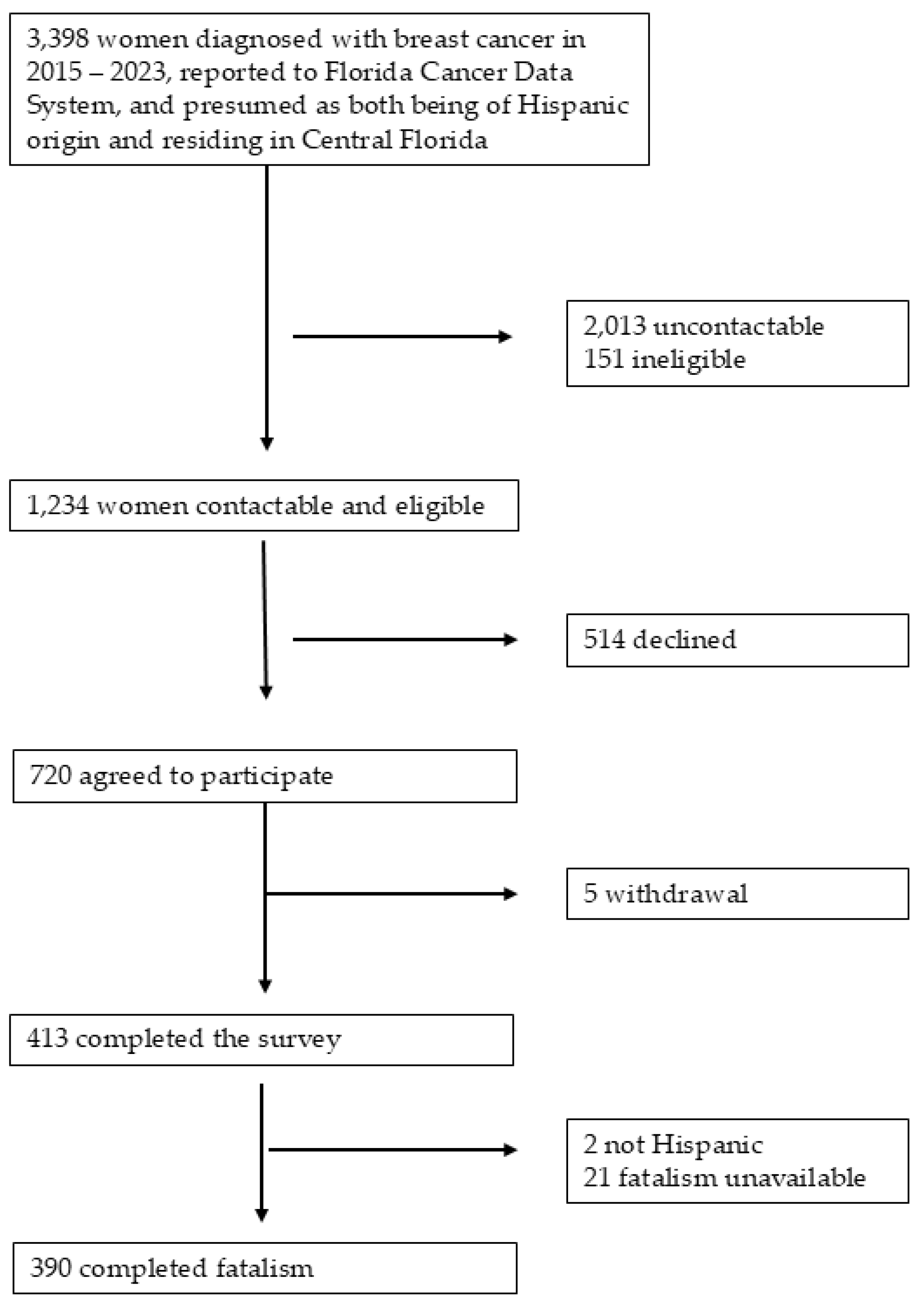
2.1. Study Design and Population
2.2. Measures
2.2.1. Fatalism
2.2.2. Hispanic Origin
2.2.3. Acculturation
2.2.4. Fear of Recurrence
2.2.5. Other Covariates
2.3. Statistical Analysis
3. Results
3.1. Study Participants
3.2. Fatalism Scores by Participant Characteristics
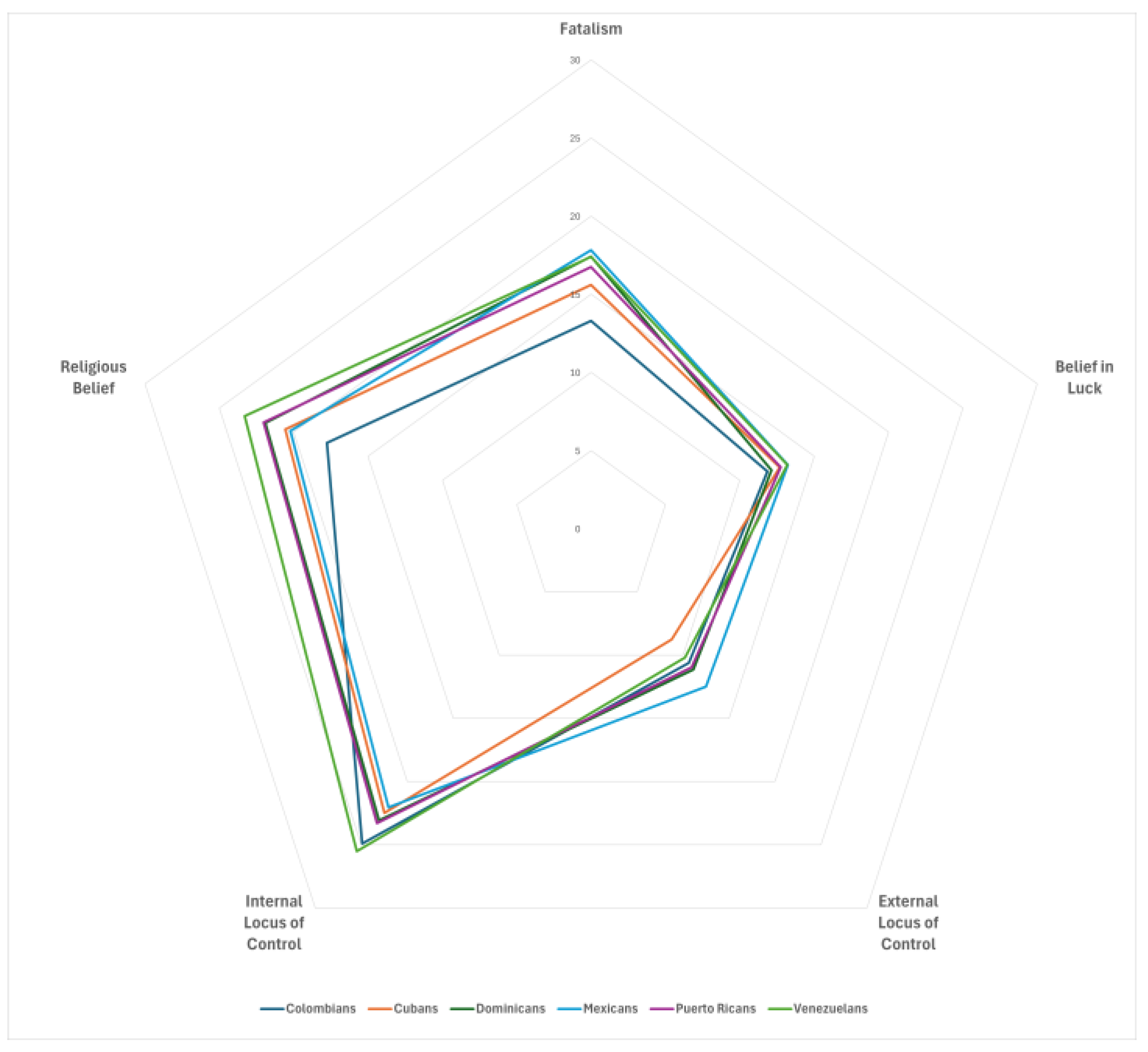
3.3. Characteristics of Fatalism
3.4. Factors Associated with Fatalism
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| QOL | Quality of life |
| US | United States |
| FCDS | Florida Cancer Data System |
| IRB | Institutional Review Board |
| MFM | Multidimensional Fatalism Measure |
| BMI | Body mass index |
| CI | Confidence Interval |
References
- American Cancer Society, Cancer facts & figures for hispanic/latino population 2024-2026. 2024: Atlanta: American Cancer Society, Inc.
- Giaquinto, A.N.; Sung, H.; Newman, L.A.; Freedman, R.A.; Smith, R.A.; Star, J.; Jemal, A.; Siegel, R.L. Breast cancer statistics 2024. CA: A Cancer J. Clin. 2024, 74, 477–495. [CrossRef]
- American Cancer Society, Breast cancer facts & figures 2024-2025. 2024: Atlanta: American Cancer Society.
- Ashing-Giwa, K.T.; Padilla, G.V.; Bohorquez, D.E.; Tejero, J.S.; Garcia, M.; D, P.; Mph Understanding the Breast Cancer Experience of Latina Women. J. Psychosoc. Oncol. 2006, 24, 19–52. [CrossRef]
- Blinder, V.S.; Patil, S.; Thind, A.; Diamant, A.; Hudis, C.A.; Basch, E.; Maly, R.C. Return to work in low-income Latina and non-Latina white breast cancer survivors: A 3-year longitudinal study. Cancer 2011, 118, 1664–1674. [CrossRef]
- Eversley, R.; Estrin, D.; Dibble, S.; Wardlaw, L.; Pedrosa, M.; Favila-Penney, W. Post-Treatment Symptoms Among Ethnic Minority Breast Cancer Survivors. Oncol. Nurs. Forum 2005, 32, 250–256. [CrossRef]
- Almatkyzy, G.; Mojica, C.M.; Stroup, A.M.; Llanos, A.A.; O’malley, D.; Xu, B.; Tsui, J. Predictors of health-related quality of life among Hispanic and non-Hispanic White breast cancer survivors in New Jersey. J. Psychosoc. Oncol. 2020, 39, 595–612. [CrossRef]
- Nápoles-Springer, A.M.; Ortíz, C.; O’brien, H.; Díaz-Méndez, M.; Pérez-Stable, E.J. Use of cancer support groups among Latina breast cancer survivors. J. Cancer Surviv. 2007, 1, 193–204. [CrossRef]
- Yanez, B.; Thompson, E.H.; Stanton, A.L. Quality of life among Latina breast cancer patients: a systematic review of the literature. J. Cancer Surviv. 2011, 5, 191–207. [CrossRef]
- Carver, C.S.; Smith, R.G.; Petronis, V.M.; Antoni, M.H. Quality of life among long-term survivors of breast cancer: different types of antecedents predict different classes of outcomes. Psycho-Oncology 2005, 15, 749–758. [CrossRef]
- Yanez, B.; Stanton, A.L.; Maly, R.C. Breast cancer treatment decision making among Latinas and non-Latina whites: A communication model predicting decisional outcomes and quality of life.. Heal. Psychol. 2012, 31, 552–561. [CrossRef]
- Powe, B.D.R.; Finnie, R.M. Cancer Fatalism. Cancer Nurs. 2003, 26, 454???467–465. [CrossRef]
- Lopez-Class, M.; Perret-Gentil, M.; Kreling, B.; Caicedo, L.; Mandelblatt, J.; Graves, K.D. Quality of Life Among Immigrant Latina Breast Cancer Survivors: Realities of Culture and Enhancing Cancer Care. J. Cancer Educ. 2011, 26, 724–733. [CrossRef]
- Graves, K.D.; Jensen, R.E.; Cañar, J.; Perret-Gentil, M.; Leventhal, K.-G.; Gonzalez, F.; Caicedo, L.; Jandorf, L.; Kelly, S.; Mandelblatt, J. Through the lens of culture: quality of life among Latina breast cancer survivors. Breast Cancer Res. Treat. 2012, 136, 603–613. [CrossRef]
- Fatalism, in Merriam-Webster. 2025: United States.
- Abraído-Lanza, A.F., M.C. Martins, et al., Breast cancer screening among dominican latinas: A closer look at fatalism and other social and cultural factors. Health Education & Behavior, 2015. 42(5): p. 633-641.
- Powe, B.D.; Hamilton, J.; Brooks, P.; PhD, R.B.D.P.; Mph Perceptions of Cancer Fatalism and Cancer Knowledge. J. Psychosoc. Oncol. 2006, 24, 1–13. [CrossRef]
- Remennick, L. The Challenge of Early Breast Cancer Detection among Immigrant and Minority Women in Multicultural Societies. Breast J. 2006, 12, S103–S110. [CrossRef]
- Shahid, F.; Beshai, S.; Del Rosario, N. Fatalism and Depressive Symptoms: Active and Passive Forms of Fatalism Differentially Predict Depression. J. Relig. Heal. 2020, 59, 3211–3226. [CrossRef]
- Vrinten, C.; Wardle, J.; Marlow, L.A. Cancer fear and fatalism among ethnic minority women in the United Kingdom. Br. J. Cancer 2016, 114, 597–604. [CrossRef]
- Bustillo, N.E.; McGinty, H.L.; Dahn, J.R.; Yanez, B.; Antoni, M.H.; Kava, B.R.; Penedo, F.J. Fatalism, medical mistrust, and pretreatment health-related quality of life in ethnically diverse prostate cancer patients. Psycho-Oncology 2015, 26, 323–329. [CrossRef]
- Tsai, W.; Wang, J.H.-Y. Fatalism and Psychological Distress Among Chinese American Breast Cancer Survivors: Mediating Role of Perceived Self-control and Fear of Cancer Recurrence. Int. J. Behav. Med. 2022, 30, 705–713. [CrossRef]
- Baron-Epel, O.; Friedman, N.; Lernau, O. Fatalism and Mammography in a Multicultural Population. Oncol. Nurs. Forum 2009, 36, 353–361. [CrossRef]
- Ghaderi, I.; Kaviani, A.; Fakhrejahani, E.; Mehrdad, N.; Hazar, N.; Karbakhsh, M.
- Gullatte, M.M.; Brawley, O.; Kinney, A.; Powe, B.; Mooney, K. Religiosity, Spirituality, and Cancer Fatalism Beliefs on Delay in Breast Cancer Diagnosis in African American Women. J. Relig. Heal. 2009, 49, 62–72. [CrossRef]
- Florida Department of Health, Procedure guide for studies that utilize patient identifiable data form the florida cancer data system. 2016.
- Esparza, O.A.; Wiebe, J.S.; Quiñones, J. Simultaneous Development of a Multidimensional Fatalism Measure in English and Spanish. Curr. Psychol. 2014, 34, 597–612. [CrossRef]
- Valenti, G.D.; Faraci, P. Instruments measuring fatalism: A systematic review.. Psychol. Assess. 2022, 34, 159–175. [CrossRef]
- Berry, J.W. Acculturation: Living successfully in two cultures. Int. J. Intercult. Relations 2005, 29, 697–712. [CrossRef]
- Wilson, E.J., K.K. Bennett, et al., The interaction between fatalism and religious attendance is negatively associated with mental health-related quality of life in hispanic/latino americans low in acculturation. North American Journal of Psychology, 2020. 22: p. 521.
- U.S. Department of Health and Human Services, Behavioral risk factor surveillance system survey questionnaire. Centers for Disease Control and Prevention (CDC).
- Kandula, N.R.; Diez-Roux, A.V.; Chan, C.; Daviglus, M.L.; Jackson, S.A.; Ni, H.; Schreiner, P.J. Association of Acculturation Levels and Prevalence of Diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2008, 31, 1621–1628. [CrossRef]
- Lerman, C., B.K. Trock B Fau - Rimer, et al., Psychological side effects of breast cancer screening. (0278-6133 (Print)).
- Brettschneider, C.; Leicht, H.; Bickel, H.; Dahlhaus, A.; Fuchs, A.; Gensichen, J.; Maier, W.; Riedel-Heller, S.; Schäfer, I.; Schön, G.; et al. Relative Impact of Multimorbid Chronic Conditions on Health-Related Quality of Life—Results from the MultiCare Cohort Study. PLOS ONE 2013, 8, e66742. [CrossRef]
- Ramirez, A.G.; Suarez, L.; Laufman, L.; Barroso, C.; Chalela, P. Hispanic Women’s Breast and Cervical Cancer Knowledge, Attitudes, and Screening Behaviors. Am. J. Heal. Promot. 2000, 14, 292–300. [CrossRef]
- Díaz, D.; Blanco, A.; Bajo, M.; Stavraki, M. Fatalism and Well-Being Across Hispanic Cultures: The Social Fatalism Scales (SFS). Soc. Indic. Res. 2014, 124, 929–945. [CrossRef]
- Mayo, R.M.; Ureda, J.R.; Parker, V.G.; D, P.; H, D.P. Importance of Fatalism in Understanding Mammography Screening in Rural Elderly Women. J. Women Aging 2001, 13, 57–72. [CrossRef]
- Sukkarieh-Haraty, O.; Egede, L.E.; Kharma, J.A.; Bassil, M. Predictors of Diabetes Fatalism Among Arabs: A Cross-Sectional Study of Lebanese Adults with Type 2 Diabetes. J. Relig. Heal. 2017, 57, 858–868. [CrossRef]
- Cohn, D.V., A. Brown, and M.H. Lopez, Black and hispanic americans see their origins as central to who they are, less so for white adults. 2021, Pew Research Center.
- Otero-Sabogal, R.; Stewart, S.; Sabogal, F.; Brown, B.A.; Pérez-Stable, E.J. Access and Attitudinal Factors Related to Breast and Cervical Cancer Rescreening: Why are Latinas Still Underscreened?. Heal. Educ. Behav. 2003, 30, 337–359. [CrossRef]
- Finkelstein, D.M.; Harding, J.F.; Paulsell, D.; English, B.; Hijjawi, G.R.; Ng’aNdu, J. Economic Well-Being And Health: The Role Of Income Support Programs In Promoting Health And Advancing Health Equity. Heal. Aff. 2022, 41, 1700–1706. [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [CrossRef]
- Harmon, M.P.; Castro, F.G.; Coe, K. Acculturation and Cervical Cancer: Knowledge, Beliefs, and Behaviors of Hispanic Women. Women Heal. 1997, 24, 37–57. [CrossRef]
- Schwartz, S.J.; Unger, J.B.; Zamboanga, B.L.; Szapocznik, J. Rethinking the concept of acculturation: Implications for theory and research. Am. Psychol. 2010, 65, 237–251. [CrossRef]
- Durmaz, H.; Çapik, C. Are Health Fatalism and Styles of Coping with Stress Affected by Poverty? A Field Study. Iran. J. Public Heal. 2023, 52, 575–583. [CrossRef]
| Total | Colombian | Cuban | Dominican | Mexican | Puerto Rican | Venezuelan | Other Hispanic | ||||||||||
| No. of participants | 390 | 100.0 | 34 | 8.7 | 25 | 6.4 | 29 | 7.4 | 22 | 5.6 | 210 | 53.8 | 24 | 6.2 | 46 | 11.8 | |
| Mean (SD) | P-value | ||||||||||||||||
| Age at diagnosis | 55.0 | (11.9) | 56.4 | (9.8) | 57.1 | (12.0) | 55.7 | (13.3) | 50.0 | (12.2) | 55.7 | (11.9) | 53.5 | (12.3) | 52.3 | (11.1) | 0.177 |
| Current age | 59.5 | (11.8) | 60.4 | (9.6) | 61.6 | (12.3) | 60.0 | (13.0) | 55.0 | (11.7) | 60.2 | (11.8) | 57.9 | (12.2) | 57.6 | (11.6) | 0.375 |
| Years since diagnosis | 4.8 | (2.0) | 4.8 | (2.1) | 4.6 | (1.9) | 4.4 | (1.9) | 5.1 | (2.1) | 4.6 | (1.9) | 4.6 | (1.8) | 5.6 | (2.9) | 0.089 |
| Years lived in US | 32.9 | (19.4) | 33.6 | (18.2) | 45.4 | (17.9) | 40.9 | (16.7) | 37.7 | (16.5) | 31.3 | (19.9) | 13.5 | (11.1) | 35.6 | (16.1) | <0.001 |
| Body mass index | 28.7 | (5.7) | 26.7 | (4.8) | 29.3 | (5.6) | 28.1 | (5.4) | 29.5 | (6.5) | 29.2 | (5.9) | 27.8 | (6.2) | 27.9 | (4.4) | 0.194 |
| N, % | P-value | ||||||||||||||||
| Race | 0.029 | ||||||||||||||||
| White | 183 | 46.9 | 15 | 44.1 | 5 | 20.0 | 20 | 69.0 | 12 | 54.5 | 98 | 46.7 | 9 | 37.5 | 24 | 52.2 | |
| Nonwhite | 207 | 53.1 | 19 | 55.9 | 20 | 80.0 | 9 | 31.0 | 10 | 45.5 | 112 | 53.3 | 15 | 62.5 | 22 | 47.8 | |
| Current smoking | 0.729 | ||||||||||||||||
| No | 372 | 95.4 | 32 | 94.1 | 23 | 92.0 | 29 | 100.0 | 22 | 100.0 | 200 | 95.2 | 23 | 95.8 | 43 | 93.5 | |
| Yes | 15 | 3.8 | 2 | 5.9 | 2 | 8.0 | . | . | . | . | 8 | 3.8 | 1 | 4.2 | 2 | 4.3 | |
| Marital status | 0.074 | ||||||||||||||||
| Married | 234 | 60.0 | 20 | 58.8 | 20 | 80.0 | 14 | 48.3 | 15 | 68.2 | 117 | 55.7 | 16 | 66.7 | 32 | 69.6 | |
| Divorced/separated/widowed | 151 | 38.7 | 14 | 41.2 | 4 | 16.0 | 15 | 51.7 | 6 | 27.3 | 90 | 42.9 | 8 | 33.3 | 14 | 30.4 | |
| Household income | 0.090 | ||||||||||||||||
| < $20,000 | 67 | 17.2 | 10 | 29.4 | 3 | 12.0 | 6 | 20.7 | 2 | 9.1 | 37 | 17.6 | 3 | 12.5 | 6 | 13.0 | |
| $20,000 - < $75,000 | 176 | 45.1 | 14 | 41.2 | 5 | 20.0 | 11 | 37.9 | 13 | 59.1 | 100 | 47.6 | 13 | 54.2 | 20 | 43.5 | |
| ≥ $75,000 | 92 | 23.6 | 7 | 20.6 | 11 | 44.0 | 6 | 20.7 | 3 | 13.6 | 48 | 22.9 | 3 | 12.5 | 14 | 30.4 | |
| Prefer not to answer | 55 | 14.1 | 3 | 8.8 | 6 | 24.0 | 6 | 20.7 | 4 | 18.2 | 25 | 11.9 | 5 | 20.8 | 6 | 13.0 | |
| Education level | 0.025 | ||||||||||||||||
| ≤ High school | 122 | 31.3 | 13 | 38.2 | 9 | 36.0 | 11 | 37.9 | 13 | 59.1 | 60 | 28.6 | 4 | 16.7 | 12 | 26.1 | |
| Some college+ | 267 | 68.5 | 21 | 61.8 | 16 | 64.0 | 18 | 62.1 | 8 | 36.4 | 150 | 71.4 | 20 | 83.3 | 34 | 73.9 | |
| Multimorbidity | 0.309 | ||||||||||||||||
| No | 157 | 40.3 | 16 | 47.1 | 10 | 40.0 | 11 | 37.9 | 12 | 54.5 | 75 | 35.7 | 12 | 50.0 | 21 | 45.7 | |
| Yes | 218 | 55.9 | 18 | 52.9 | 14 | 56.0 | 17 | 58.6 | 9 | 40.9 | 129 | 61.4 | 11 | 45.8 | 20 | 43.5 | |
| Language used at home | <0.001 | ||||||||||||||||
| More Spanish | 203 | 52.1 | 22 | 64.7 | 9 | 36.0 | 13 | 44.8 | 10 | 45.5 | 112 | 53.3 | 22 | 91.7 | 15 | 32.6 | |
| Both equally | 86 | 22.1 | 5 | 14.7 | 4 | 16.0 | 7 | 24.1 | 1 | 4.5 | 57 | 27.1 | 1 | 4.2 | 11 | 23.9 | |
| More English | 99 | 25.4 | 7 | 20.6 | 12 | 48.0 | 9 | 31.0 | 10 | 45.5 | 41 | 19.5 | 1 | 4.2 | 19 | 41.3 | |
| Birthplace | 0.167 | ||||||||||||||||
| US | 308 | 79.0 | 31 | 91.2 | 18 | 72.0 | 23 | 79.3 | 18 | 81.8 | 159 | 75.7 | 23 | 95.8 | 36 | 78.3 | |
| Non-US | 81 | 20.8 | 3 | 8.8 | 7 | 28.0 | 6 | 20.7 | 4 | 18.2 | 50 | 23.8 | 1 | 4.2 | 10 | 21.7 | |
| Stage | 0.441 | ||||||||||||||||
| In situ | 65 | 16.7 | 7 | 20.6 | 3 | 12.0 | 7 | 24.1 | 4 | 18.2 | 35 | 16.7 | 1 | 4.2 | 8 | 17.4 | |
| Localized | 158 | 40.5 | 12 | 35.3 | 12 | 48.0 | 11 | 37.9 | 7 | 31.8 | 87 | 41.4 | 17 | 70.8 | 12 | 26.1 | |
| Regional/Distant | 66 | 16.9 | 4 | 11.8 | 4 | 16.0 | 5 | 17.2 | 3 | 13.6 | 41 | 19.5 | 2 | 8.3 | 7 | 15.2 | |
| Surgery | 0.467 | ||||||||||||||||
| No | 15 | 3.8 | 3 | 8.8 | 1 | 4.0 | 1 | 3.4 | . | . | 7 | 3.3 | 1 | 4.2 | 2 | 4.3 | |
| Breast-conserving surgery | 199 | 51.0 | 20 | 58.8 | 18 | 72.0 | 16 | 55.2 | 12 | 54.5 | 102 | 48.6 | 10 | 41.7 | 21 | 45.7 | |
| Mastectomy | 176 | 45.1 | 11 | 32.4 | 6 | 24.0 | 12 | 41.4 | 10 | 45.5 | 101 | 48.1 | 13 | 54.2 | 23 | 50.0 | |
| Radiation therapy | 0.160 | ||||||||||||||||
| No | 209 | 53.6 | 16 | 47.1 | 8 | 32.0 | 15 | 51.7 | 11 | 50.0 | 115 | 54.8 | 13 | 54.2 | 31 | 67.4 | |
| Yes | 170 | 43.6 | 18 | 52.9 | 15 | 60.0 | 14 | 48.3 | 10 | 45.5 | 89 | 42.4 | 11 | 45.8 | 13 | 28.3 | |
| Chemotherapy | 0.008 | ||||||||||||||||
| No | 217 | 55.6 | 21 | 61.8 | 18 | 72.0 | 15 | 51.7 | 9 | 40.9 | 117 | 55.7 | 6 | 25.0 | 31 | 67.4 | |
| Yes | 172 | 44.1 | 12 | 35.3 | 7 | 28.0 | 14 | 48.3 | 13 | 59.1 | 93 | 44.3 | 18 | 75.0 | 15 | 32.6 | |
| ER status | 0.347 | ||||||||||||||||
| Negative | 54 | 13.8 | 5 | 14.7 | 3 | 12.0 | 4 | 13.8 | 6 | 27.3 | 24 | 11.4 | 6 | 25.0 | 6 | 13.0 | |
| Positive | 319 | 81.8 | 27 | 79.4 | 22 | 88.0 | 22 | 75.9 | 15 | 68.2 | 176 | 83.8 | 18 | 75.0 | 39 | 84.8 | |
| Fear of recurrence | 0.470 | ||||||||||||||||
| Low | 132 | 33.8 | 13 | 38.2 | 12 | 48.0 | 8 | 27.6 | 10 | 45.5 | 63 | 30.0 | 10 | 41.7 | 16 | 34.8 | |
| Moderate | 201 | 51.5 | 19 | 55.9 | 11 | 44.0 | 15 | 51.7 | 11 | 50.0 | 109 | 51.9 | 13 | 54.2 | 23 | 50.0 | |
| High | 50 | 12.8 | 2 | 5.9 | 2 | 8.0 | 6 | 20.7 | 1 | 4.5 | 33 | 15.7 | 1 | 4.2 | 5 | 10.9 | |
| Variable | Category | N | Estimated Mean (95% CI) | P-value | |
|---|---|---|---|---|---|
| Total | 16.4 | (15.8–17.0) | |||
| Hispanic origin | Colombian | 34 | 13.3 | (11.2–15.4) | 0.060 |
| Cuban | 25 | 15.6 | (13.1–18.1) | ||
| Dominican | 29 | 17.4 | (15.1–19.7) | ||
| Mexican | 22 | 17.8 | (15.2–20.5) | ||
| Puerto Rican | 210 | 16.7 | (15.9–17.6) | ||
| Venezuelan | 24 | 17.4 | (14.9–132.8) | ||
| Other Hispanic | 46 | 15.8 | (14.1–17.7) | ||
| Current age (years) | 20 - < 40 | 15 | 18.7 | (15.5–21.8) | 0.377 |
| 40 - < 55 | 131 | 16.6 | (15.5–17.7) | ||
| 55 - 70 | 159 | 15.9 | (14.9–16.9) | ||
| ≥ 70 | 85 | 16.7 | (15.3– 18.0) | ||
| Race | White | 207 | 15.9 | (15.1–16.8) | 0.111 |
| Nonwhite | 183 | 17.0 | (16.0–17.9) | ||
| Body mass index (kg/m2) | < 25 | 109 | 16.2 | (15.1–17.4) | 0.709 |
| 25 - < 30 | 141 | 16.3 | (15.2–17.3) | ||
| ≥ 30 | 135 | 16.8 | (15.7–17.9) | ||
| Current smoking | No | 372 | 16.3 | (15.7–17.0) | 0.304 |
| Yes | 15 | 18.1 | (14.8–21.3) | ||
| Marital status | Married | 234 | 16.6 | (15.7–17.4) | 0.770 |
| Unmarried | 151 | 16.4 | (15.3–17.4) | ||
| Household income | < $20,000 | 67 | 18.5 | (17.0–20.0) | 0.004 |
| $20,000 - < $75,000 | 176 | 16.1 | (15.2–17.0) | ||
| ≥ $75,000 | 92 | 15.1 | (13.8–16.3) | ||
| Prefer not to answer | 55 | 17.1 | (15.5–18.8) | ||
| Education level | ≤ High school | 122 | 18.2 | (17.1–19.3) | < 0.001 |
| Some college or more | 267 | 15.6 | (14.8–16.4) | ||
| Language use at home | More Spanish | 203 | 17.1 | (16.2–17.9) | 0.007 |
| Both equally | 86 | 17.0 | (15.6–18.3) | ||
| More English | 99 | 14.7 | (13.5–16.0) | ||
| Birthplace | United States | 81 | 15.8 | (14.4–17.2) | 0.314 |
| Outside United States | 308 | 16.6 | (15.9–17.3) | ||
| Multimorbidity | No | 157 | 16.7 | (15.7–17.7) | 0.513 |
| Yes | 218 | 16.2 | (15.4–17.1) | ||
| Cancer stage | In Situ | 65 | 16.2 | (14.6–17.7) | 0.574 |
| Localized | 158 | 16.1 | (15.1–17.1) | ||
| Regional/Distant | 66 | 17.0 | (15.5–18.6) | ||
| Surgery | No | 15 | 13.8 | (10.6–17.0) | 0.259 |
| Breast-conserving surgery | 199 | 16.6 | (15.7– 17.5) | ||
| Mastectomy | 176 | 16.5 | (15.5–17.4) | ||
| Radiotherapy | No | 209 | 16.4 | (15.6–17.3) | 0.895 |
| Yes | 170 | 16.4 | (15.4–17.3) | ||
| Chemotherapy | No | 217 | 16.3 | (15.4–17.1) | 0.527 |
| Yes | 172 | 16.7 | (15.7–17.6) | ||
| Estrogen receptor | Negative | 54 | 16.3 | (14.6–18.0) | 0.881 |
| Positive | 319 | 16.4 | (15.7–17.1) | ||
| Years since diagnosis (years) | < 2 | 42 | 14.1 | (12.2–16.1) | 0.043 |
| 2 - < 5 | 216 | 16.8 | (16.0–17.7) | ||
| 5 - < 10 | 132 | 16.5 | (15.4–17.6) | ||
| Years lived in US | < 10 | 64 | 16.1 | (14.5–17.6) | 0.718 |
| 10 - < 30 | 119 | 16.8 | (15.6–17.9) | ||
| ≥ 30 | 206 | 16.3 | (15.4–17.2) | ||
| Fear of recurrence | Low | 132 | 15.6 | (14.5–16.7) | 0.039 |
| Moderate | 201 | 16.6 | (15.7–17.4) | ||
| High | 50 | 18.2 | (16.5–20.0) | ||
| Variable | Fatalism | Religious belief | External locus of control | Internal locus of control | Belief in luck |
|---|---|---|---|---|---|
| Mean (SD) | 16.4 (6.3) | 21.3 (7.5) | 10.9 (5.3) | 23.4 (5.0) | 12.6 (4.7) |
| Correlation Matrix: Correlation Coefficient (P-value) | |||||
| Religious belief | 0.394 (P< 0.001) |
||||
| External locus of control | 0.400 (P< 0.001) |
0.125 (P= 0.014) |
|||
| Internal locus of control | 0.150 (P= 0.003) |
-0.003 (P= 0.949) |
-0.045 (P= 0.677) |
||
| Belief in luck | 0.273 (P< 0.001) |
0.156 (P= 0.002) |
0.384 (P< 0.001) |
0.060 (P= 0.234) |
|
| Characteristics | Parameter | β | SE | P-value |
|---|---|---|---|---|
| Intercept | 19.3 | 2.4 | <.0001 | |
| Hispanic Origin (Ref: Puerto Rican) | Colombian | -4.0 | 1.2 | 0.001 |
| Cuban | -0.9 | 1.4 | 0.527 | |
| Dominican | -0.1 | 1.2 | 0.945 | |
| Mexican | 1.3 | 1.5 | 0.395 | |
| Venezuelan | 1.3 | 1.4 | 0.357 | |
| Other Hispanic | -0.7 | 1.1 | 0.522 | |
| Current age (Ref: 20 - < 40) | 40 - < 55 | -2.0 | 1.7 | 0.252 |
| 55 - < 70 | -2.9 | 1.7 | 0.099 | |
| 70 + | -3.3 | 1.8 | 0.075 | |
| Race (ref: white) | Non-white | 0.6 | 0.7 | 0.327 |
| Household income (Ref: < $20,000) | $20,000 - < $75,000 | -2.3 | 0.9 | 0.011 |
| ≥ $75,000 | -2.4 | 1.1 | 0.033 | |
| Prefer not to answer | -1.3 | 1.1 | 0.259 | |
| Education (Ref: ≤ High school) | Some college + | -1.9 | 0.8 | 0.012 |
| Language use at home (Ref: More Spanish) | Both equally | -0.2 | 0.9 | 0.815 |
| More English | -2.0 | 1.0 | 0.042 | |
| Years lived in US (ref: < 10) | 10 - < 30 | 0.9 | 1.0 | 0.390 |
| 30+ | 1.5 | 1.1 | 0.147 | |
| Years since diagnosis (Ref: < 2) | 2 - < 5 | 1.9 | 1.1 | 0.086 |
| ≥ 5 | 1.9 | 1.1 | 0.099 | |
| Fear of recurrence (Ref: Low) | Moderate | 0.8 | 0.7 | 0.276 |
| High | 1.7 | 1.1 | 0.126 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





