Submitted:
25 June 2025
Posted:
26 June 2025
You are already at the latest version
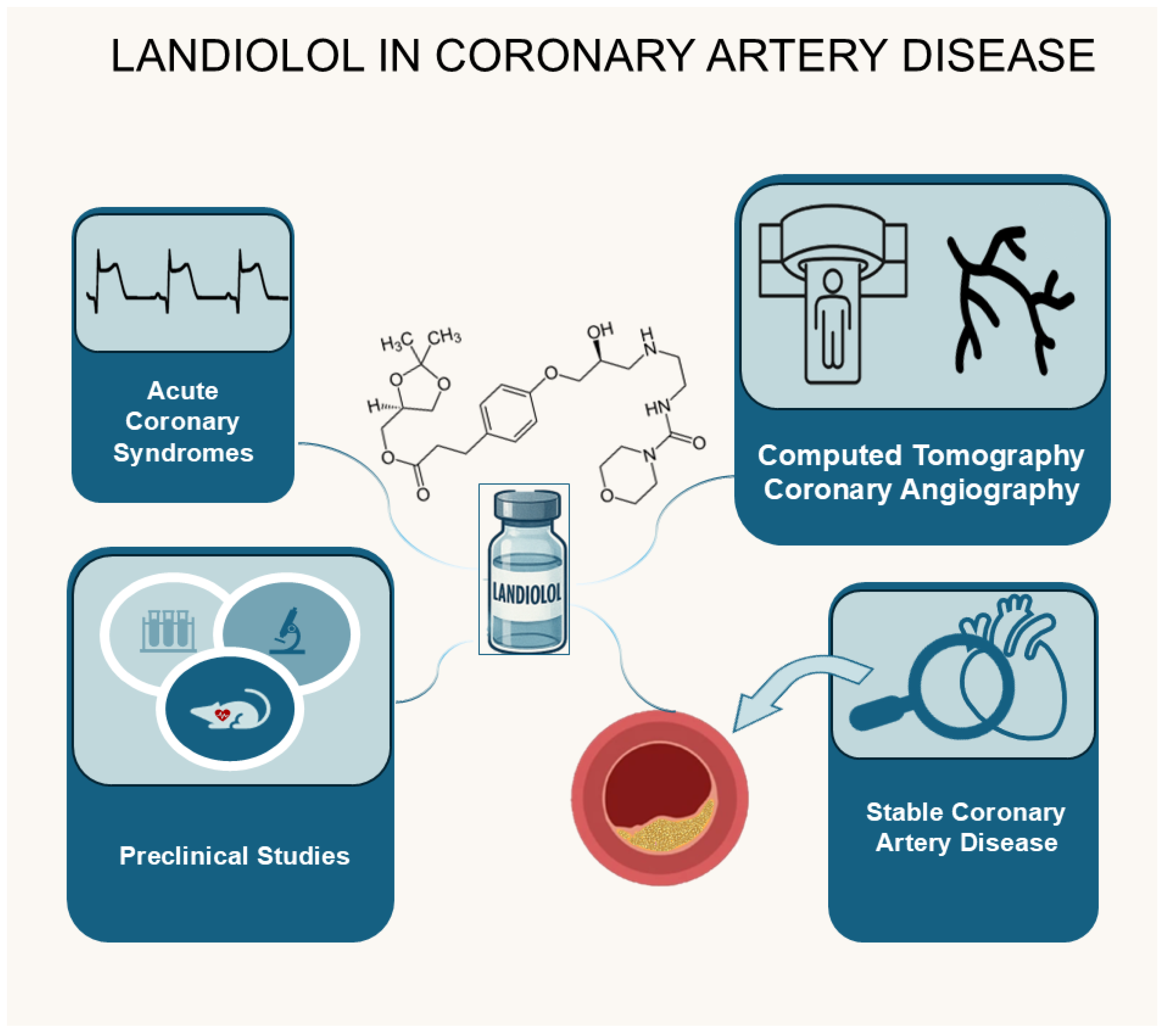
Abstract
Keywords:
Introduction
Landiolol Properties
Landiolol in Acute Coronary Syndromes (ACS)—Clinical Evidence and Study Outcomes
Reduction in Myocardial Salvage Index (MSI)
Reduction in Myocardial Oxygen Demand—Hemodynamic Effects
Percutaneous Coronary Intervention Results
Arrhythmia Management
Safety Outcomes
Long Term Outcomes
Landiolol in Computed Tomography Coronary Angiography (CTCA)
Heart Rate Reduction and Normalization Timeline
Image Quality Analysis
Safety Outcomes
Landiolol in Stable CAD—Clinical Evidence and Study Outcomes
Landiolol in Animal Studies with CAD
Discussion
Disclosure Statement
Author Contributions
Funding
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| CAD | Coronary artery disease |
| BBs | Beta Blockers |
| pPCI | primary Percutaneous Coronary Intervention |
| bpm | beats per minute (bpm |
| CTCA | Computed Tomography Coronary Angiography |
| ACSs | Acute coronary syndromes |
| ESC | European Society of Cardiology |
| STEMI | ST-elevation myocardial infarction |
| NSTEMI | Non ST-elevation myocardial infarction |
| SVTs | Supraventricular tachyarrhythmias |
| AF | Atrial Fibrillation |
| HR | Heart Rate |
| MSI | Reduction in Myocardial Salvage Index |
| CMR | Cardiac Magnetic Resonance |
| RCTs | Randomized Control Trials |
| STR | ST-segment Resolution |
| MBG | Myocardial Brush Grade |
| VF | Ventricular Fibrillation |
| VT | Ventricular Tachycardia |
| NSVT | Non-sustained Ventricular Tachycardia |
| BNP | B-type Natriuretic Peptide |
| LVEF | Left Ventricular Ejection Fraction |
| LVEDV | Left Ventricular End-Diastolic Volume |
| LVEDV | Left Ventricular End-Systolic Volume |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| AVB | Atrioventricular Block |
| CK | Creatine Kinase |
| CK-AUC | CK area under the curve |
| EF | Ejection Fraction |
| LVWSI | Left Ventricular Wall Motion Score Index |
| APN | Adiponectin |
| IRI | Ischemia-Reperfusion Injury |
| IPC | Ischemic Precondition |
| FEV1 | Forced Expiratory Volume in 1 second |
References
- Stark, B.; Johnson, C.; Roth, G.A. GLOBAL PREVALENCE OF CORONARY ARTERY DISEASE: AN UPDATE FROM THE GLOBAL BURDEN OF DISEASE STUDY. Circ. 2024, 83, 2320. [Google Scholar] [CrossRef]
- Park, J.; Han, J.-K.; Kang, J.; Chae, I.-H.; Lee, S.Y.; Choi, Y.J.; Rhew, J.Y.; Rha, S.-W.; Shin, E.-S.; Woo, S.-I.; et al. Optimal Dose and Type of β-blockers in Patients With Acute Coronary Syndrome Undergoing Percutaneous Coronary Intervention. Am. J. Cardiol. 2020, 137, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Ropers, U.; Ropers, D.; Pflederer, T.; Anders, K.; Kuettner, A.; Stilianakis, N.I.; Komatsu, S.; Kalender, W.; Bautz, W.; Daniel, W.G.; et al. Influence of Heart Rate on the Diagnostic Accuracy of Dual-Source Computed Tomography Coronary Angiography. Circ. 2007, 50, 2393–2398. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. ESC 2023 guidelines for the treatment of acute coronary syndromes developed by the task force for the treatment of acute coronary syndromes of the European Society of Cardiology (ESC). 2024, 25, E1–E112. [CrossRef]
- Tsuchiya, H.; Mizogami, M. Characteristic interactivity of landiolol, an ultra-short-acting highly selective β1-blocker, with biomimetic membranes: Comparisons with β1-selective esmolol and non-selective propranolol and alprenolol. Front Pharmacol. 2013;4:150.
- Domanovits, H.; Wolzt, M.; Stix, G. Landiolol: pharmacology and its use for rate control in atrial fibrillation in an emergency setting. Eur. Hear. J. Suppl. 2018, 20, A1–A3. [Google Scholar] [CrossRef]
- Sun, B.; Wang, C.Y.; Chen, R.R. Clinical Efficacy and Safety of Early Intravenous Administration of Beta-Blockers in Patients Suffering from Acute ST-Segment Elevation Myocardial Infarction Without Heart Failure Undergoing Primary Percutaneous Coronary Intervention: A Study-Level Meta-Analysis of Randomized Clinical Trials. Cardiovasc. Drugs Ther. 2023, 38, 833–846. [Google Scholar] [CrossRef]
- Miyamoto, M.; Miyoshi, T.; Osawa, K.; Mori, A.; Oka, T.; Ito, H. Efficacy of early intravenous landiolol, an ultrashort-acting beta-blocker on infarct size and its safety in patients with myocardial infarction undergoing primary PCI: a randomized, controlled study. Eur. Hear. J. 2020, 41. [Google Scholar] [CrossRef]
- Miyamoto, M.; Osawa, K.; Miyoshi, T.; Mori, A.; Yoshikawa, M.; Oka, T.; Ichikawa, K.; Nakamura, K.; Ito, H. Efficacy and Safety of Early Intravenous Landiolol on Myocardial Salvage in Patients with ST-segment Elevation Myocardial Infarction before Primary Percutaneous Coronary Intervention: A Randomized Study. 2021, 75, 289–297. [CrossRef]
- Hoshi, T.; Sato, A.; Nishina, H.; Kakefuda, Y.; Wang, Z.; Noguchi, Y.; Aonuma, K. Acute hemodynamic effects of landiolol, an ultra-short-acting beta-blocker, in patients with acute coronary syndrome: Preliminary study. J. Cardiol. 2012, 60, 252–256. [Google Scholar] [CrossRef]
- Kiyokuni, M.; Konishi, M.; Sakamaki, K.; Kawashima, C.; Narikawa, M.; Doi, H.; Iwata, K.; Tomari, S.; Nakayama, N.; Komura, N.; et al. Beneficial effect of early infusion of landiolol, a very short-acting beta-1 adrenergic receptor blocker, on reperfusion status in acute myocardial infarction. Int. J. Cardiol. 2016, 221, 321–326. [Google Scholar] [CrossRef]
- Hanada, K.; Higuma, T.; Nishizaki, F.; Sukekawa, T.; Yokota, T.; Yamada, M.; Saito, S.; Kushibiki, M.; Oikawa, K.; Abe, N.; et al. Randomized Study on the Efficacy and Safety of Landiolol, an Ultra-Short-Acting.BETA.1-Adrenergic Blocker, in Patients With Acute Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Circ. J. 2012, 76, 439–445. [Google Scholar] [CrossRef]
- Higuchi, H. FEASIBILITY OF CONTINUOUS INTRAVENOUS ADMINISTRATION OF LANDIOLOL FOR ACUTE MYOCARDIAL INFARCTION :FIRST CLINICAL EXPERIENCE AND ITS SAFE DIRECTIONS FOR USE. Circ. 2010, 55, A102.E953. [Google Scholar] [CrossRef]
- Hoedemaker, N.P.; Roolvink, V.; de Winter, R.J.; van Royen, N.; Fuster, V.; García-Ruiz, J.M.; Er, F.; Gassanov, N.; Hanada, K.; Okumura, K.; et al. Early intravenous beta-blockers in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: A patient-pooled meta-analysis of randomized clinical trials. Eur. Hear. Journal. Acute Cardiovasc. Care 2020, 9, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Kiyokuni, M.; Mitsuhashi, T.; Sugano, T.; Endo, T.; Ishigami, T.; Ishikawa, T.; Umemura, S.; Kiyokuni, K. Abstract 10337: Using Landiolol During Primary Percutaneous Coronary Intervention Attenuates Myocardial Reperfusion Injury in Patients With ST-segment Elevation Acute Myocardial Infarction. Circulation 2015, 132. [Google Scholar] [CrossRef]
- Fujita, M.; Yamashita, T.; Nakata, M.; Nishikido, T.; Chinen, T.; Kikuchi, T.; Nakamura, K.; Meguro, K.; Keida, T.; Ohira, H. Low Dose Landiolol During Very Acute Phase of Acute Myocardial Infarction Improves Brain Natriuretic Peptide Level in the Chronic Phase. J. Card. Fail. 2010, 16, S150–S151. [Google Scholar] [CrossRef]
- Fujita, M.; Ohira, H.; Yamashita, T.; Nakata, M.; Nishikido, T.; Chinenn, T.; Kikuchi, T.; Nakamura, K.; Meguro, K.; Keida, T. Chronic Phase Effect of Landiolol about Left Ventricular Volume in Patients with Acute Myocardial Infarction after Primary Percutaneous Coronary Intervention. J. Card. Fail. 2012, 18, S171. [Google Scholar] [CrossRef]
- Maruyama, T.; Takada, M.; Hasuike, T.; Yoshikawa, A.; Namimatsu, E.; Yoshizumi, T. Radiation dose reduction and coronary assessability of prospective electrocardiogram-gated computed tomography coronary angiography: comparison with retrospective electrocardiogram-gated helical scan. J Am Coll Cardiol. 2008;52(18):1450-5.
- So, A.; Hsieh, J.; Narayanan, S.; Thibault, J.-B.; Imai, Y.; Dutta, S.; Leipsic, J.; Min, J.; LaBounty, T.; Lee, T.-Y. Dual-energy CT and its potential use for quantitative myocardial CT perfusion. J. Cardiovasc. Comput. Tomogr. 2012, 6, 308–317. [Google Scholar] [CrossRef]
- Jinzaki, M.; Hirano, M.; Hara, K.; Suzuki, T.; Yamashina, A.; Ikari, Y.; et al. A randomized, double-blind, placebo-controlled, phase II dose-finding study of the short acting β1-blocker, landiolol hydrochloride, in patients with suspected ischemic cardiac disease. The international journal of cardiovascular imaging. 2013;29 Suppl 1(Suppl 1):7-20.
- Hirano, M.; Yamashina, A.; Hara, K.; Ikari, Y.; Jinzaki, M.; Iino, M.; et al. A randomized, double-blind, placebo-controlled, phase III study of the short-acting β1-adrenergic receptor blocker landiolol hydrochloride for coronary computed tomography angiography in Japanese patients with suspected ischemic cardiac disease. Clinical drug investigation. 2014;34(1):53-62.
- Hirano, M.; Hara, K.; Ikari, Y.; Jinzaki, M.; Iino, M.; Hamada, C.; Kuribayashi, S. Dose-Finding Study of Landiolol Hydrochloride: A Short-Acting β1-Blocker for Controlling Heart Rate During Coronary Computed-Tomography Angiography in Japan. Adv. Ther. 2013, 30, 803–818. [Google Scholar] [CrossRef]
- Isobe, S.; Sato, K.; Sugiura, K.; Mimura, T.; Kobayashi, M.; Meno, C.; Kato, M.; Ishii, H.; Murohara, T. Feasibility of Intravenous Administration of Landiolol Hydrochloride for Multislice Computed Tomography Coronary Angiography Initial Experience. Circ. J. 2008, 72, 1814–1820. [Google Scholar] [CrossRef]
- Kido, T.; Mochizuki, T.; Hirano, M.; Yamada, Y.; Tanaka, R.; Kanzaki, S.; Higashi, M.; Jinzaki, M.; Yoshioka, K.; Kuribayashi, S. Radiation-Dose-Lowering Effects of Landiolol Hydrochloride in Coronary Angiography Using Computed Tomography (DELIGHT) – A Prospective Multicenter Study –. Circ. J. 2016, 80, 1225–1231. [Google Scholar] [CrossRef]
- Kokubo, R.; Hirano, M.; Tajima, Y.; Yunaiyama, D.; Saito, K. Effects of β-blocker Administration on Cardiac Function: A Coronary Computed Tomography Angiography Study. Curr. Med Imaging Former. Curr. Med Imaging Rev. 2022, 18, 1517–1525. [Google Scholar] [CrossRef]
- Barwig, M.; Janisch, M.; Gessl, J.; Kübler, W.; König, C.; Schwantzer, G.; Schöllnast, H. Efficacy of bolus injections of landiolol hydrochloride as premedication in coronary artery CT angiography. Insights into Imaging 2025, 16, 1–8. [Google Scholar] [CrossRef]
- Osawa, K.; Miyoshi, T.; Sato, S.; Akagi, N.; Morimitsu, Y.; Nakamura, K.; Kohno, K.; Kusano, K.; Kanazawa, S.; Ito, H. Safety and Efficacy of a Bolus Injection of Landiolol Hydrochloride as a Premedication for Multidetector-Row Computed Tomography Coronary Angiography. Circ. J. 2013, 77, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Yamaji, K.; Saho, T.; Matsuzaki, Z.; Yuda, I.; Soga, Y.; Shirai, S.; Ando, K.; Nobuyoshi, M. A comparison of bolus injection of landiolol versus oral administration of propranolol before cardiac computed tomography. SpringerPlus 2014, 3, 93. [Google Scholar] [CrossRef] [PubMed]
- Koyoshi, R.; Shiga, Y.; Idemoto, Y.; Ueda, Y.; Tashiro, K.; Kuwano, T.; Kitajima, K.; Fujimi, K.; Kawamura, A.; Ogawa, M.; et al. Safety of Landiolol Hydrochloride as a Premedication for Producing an Appropriate Heart Rate for Multidetector-Row Computed Tomography Coronary Angiography. J. Clin. Med. Res. 2018, 10, 22–26. [Google Scholar] [CrossRef]
- Haengnam, P. MYOCARDIAL PROTECTION BY INTRACORONARY ADMINISTRATION OF SHORT-ACTING BETA-BLOCKER, LANDIOLOL, DURING ELECTIVE PERCUTANEOUS CORONARY INTERVENTION. Circ. 2010, 55, A123.E1150–A123.E1150. [Google Scholar] [CrossRef]
- Park, H.; Otani, H.; Noda, T.; Sato, D.; Okazaki, T.; Ueyama, T.; Iwasaka, J.; Yamamoto, Y.; Iwasaka, T. Intracoronary followed by intravenous administration of the short-acting β-blocker landiolol prevents myocardial injury in the face of elective percutaneous coronary intervention. Int. J. Cardiol. 2013, 167, 1547–1551. [Google Scholar] [CrossRef]
- Kiyokuni, M.; Konishi, M.; Saigusa, Y.; Iwata, K.; Nakayama, N.; Komura, N.; Sugano, T.; Ishigami, T.; Ishikawa, T.; Yamanaka, T.; et al. Randomized controlled trial of landiolol, a short-acting beta-1 adrenergic receptor blocker, illustrating changes in high-molecular weight adiponectin levels after elective percutaneous coronary intervention. Hear. Vessel. 2020, 35, 1510–1517. [Google Scholar] [CrossRef]
- Shibata, S.; Okamoto, Y.; Endo, S.; Ono, K. Direct Effects of Esmolol and Landiolol on Cardiac Function, Coronary Vasoactivity, and Ventricular Electrophysiology in Guinea-Pig Hearts. J. Pharmacol. Sci. 2012, 118, 255–265. [Google Scholar] [CrossRef]
- Yu, S.; Katoh, T.; Okada, H.; Makino, H.; Mimuro, S.; Sato, S. Landiolol does not enhance the effect of ischemic preconditioning in isolated rat hearts. J. Anesthesia 2010, 24, 208–214. [Google Scholar] [CrossRef]
- Kimura-Kurosawa, S.; Kanaya, N.; Kamada, N.; Hirata, N.; Nakayama, M.; Namiki, A. Cardioprotective effect and mechanism of action of landiolol on the ischemic reperfused heart. J. Anesthesia 2007, 21, 480–489. [Google Scholar] [CrossRef]
- Park, H.; Otani, H.; Oishi, C.; Fujikawa, M.; Yamashita, K.; Okazaki, T.; Sato, D.; Ueyama, T.; Iwasaka, J.; Yamamoto, Y.; et al. Efficacy of intracoronary administration of a short-acting β-blocker landiolol during reperfusion in pigs. Int. J. Cardiol. 2011, 146, 347–353. [Google Scholar] [CrossRef]
- Mitsis, A.; Myrianthefs, M.; Sokratous, S.; Karmioti, G.; Kyriakou, M.; Drakomathioulakis, M.; Tzikas, S.; Kadoglou, N.P.E.; Karagiannidis, E.; Nasoufidou, A.; et al. Emerging Therapeutic Targets for Acute Coronary Syndromes: Novel Advancements and Future Directions. Biomedicines 2024, 12, 1670. [Google Scholar] [CrossRef] [PubMed]
- Mitsis, A.; Panayiotis, A.; John, L.; Michaela, K.; Stefanos, S.; Georgia, K.; et al. Role of Inflammation Following An Acute Myocardial Infarction: Design of INFINITY. Biomarkers in Medicine. 2023;17(23):971-81.
- Nasoufidou, A.; Papazoglou, A.S.; Stachteas, P.; Karagiannidis, E.; Samaras, A.; Alexiou, S.; Mourtzos, M.-A.; Kassimis, G.; Fragakis, N. Intravenous Landiolol for Rate Control in Supraventricular Tachyarrhythmias in Patients with Left Ventricular Dysfunction: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1683. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Kihara, Y. Lower Radiation Exposure Needs Lower Heart Rate. Circ. J. 2016, 80, 1106–1107. [Google Scholar] [CrossRef] [PubMed]
- Fujito, K.; Takayanagi, R.; Kimura, K.; Yokoyama, H.; Yamada, Y. Evaluation of clinical bradycardiac effect and respiratory adverse effect of β-blocking agents in coronary computed tomography angiography based on theoretical analysis. European Journal of Drug Metabolism and Pharmacokinetics. 2016;41(2):157-67.
- Igarashi, A.; Kaori, F.; Masaharu, H.; Fukuda, T. Cost minimization analysis of beta-blocker at the time of CT imaging for suspected of coronary heart disease in Japan. Journal of Medical Economics. 2014;17(2):142-7.
- Sanad, M.H.; Farag, A.B.; Motaleb, M.A. Radioiodination and biological evaluation of landiolol as a tracer for myocardial perfusion imaging: preclinical evaluation and diagnostic nuclear imaging. Radiochim. Acta 2018, 106, 1001–1008. [Google Scholar] [CrossRef]
| Study ID | Type of study | Population | Total N, Landiolol dosage/comparator | Main outcomes and Adverse Events |
|---|---|---|---|---|
| Miyamoto et al. 2020 [8] |
Multi center RCT |
STEMI |
47 patients randomized to Landiolol (n=23) Controls (n=24) |
|
| Hanada et al. 2012 [12] |
Single center RCT |
STEMI | 96 patients after PCI randomized to Landiolol (n=47) Controls (n=49) |
|
| Fujita et al. 2010 [16] |
Single center RCT |
AMI | 48 patients randomly assigned to Landiolol (n=25) Controls (n=23) |
|
| Fujita et al. 2012 [17] |
Single center RCT |
AMI | 79 patients randomly assigned to Landiolol (n=42) Controls (n=37) |
|
| Higuchi et al. 2010 [13] |
Single center RCT |
Anterior AMI | 26 patients after PCI Landiolol (n=14) Controls (n=12) |
|
| Kiyokuni et al. 2016 [11] |
Single-center Observational |
NSTEMI STEMI |
115 patients Landiolol (n=55) Controls (n= 60) |
|
| Hoshi et al. 2012 [10] |
Single center Observational |
ACS | Landiolol (n=22) |
|
| Sun et al. 2023 [7] |
Meta-analysis 7 RCTs |
STEMI | 3 Landiolol studies vs placebo Hanada et al. 2012 Kiyokuni et al. 2016 Miyamoto et al. 2021 |
|
| Study ID | Type of Study | Study Population (main characteristics) | Total N, Landiolol dosage/comparator | Main outcomes and Adverse Events |
|---|---|---|---|---|
| Jinzaki et al. 2013 [20] | Multi- Center RCT |
Adults with suspected CAD Inclusion: chest pain with positive findings on exercise (ECG) or positive findings on MBF/ cardiac US |
n = 183 patients Permuted-block randomization 3 groups n1 = 58: 0.06mg/kg of landiolol n2 = 61: 0.125mg/kg of landiolol n3 = 64: placebo All patients received 300-600 mg of nitroglycerin first |
(Εfficacy) HR at the time of CTCA: lower mean HR values in the landiolol groups (P = 0.003 and P<0.001, respectively) and lower in the high-dose group (P = 0.002). HR reduction was significantly greater in both landiolol groups (both P<0.001) and in the 0.125mg/kg group the achieved rate was lower (P=0.007). The rapid reduction started immediately, became significant at 15min and stopped being significantly lower than the placebo group after 30min in both landiolol groups. (Safety) BP: No difference after 30min. Adverse events: No difference among groups. CTCA analysis: Per patient and per artery analysis: correct classification proportion significantly higher in 0.125 mg/kg group Per segment analysis: assessable segments and correct classification proportion significantly higher in both landiolol groups |
| Hirano et al. 2014 [21] |
Multi Center RCT |
Patients ≥ 20 years with suspected CAD Inclusion: (1) presented with stable angina (2) HR 70–90 bpm before nitrates |
n = 258 patients Permuted-block randomization Groups n1 = 130: 0.125 mg/k of landiolol n2 = 128: placebo group Bolus injection of study drug. CCTA after 4-7min. |
(Efficacy) HR: significantly lower in the landiolol group (62.6 ± 8.5bpm vs 72.9 ± 12bpm, p<0.0001). HR reduction was significantly higher in the landiolol group (-19.1 ± 8.1 % vs −5.9 ± 9.7 %, p<0.0001). No significant difference was any more found at 30 min after administration. (Safety) BP: mean SBP significantly lower in landiolol group (125.1 ± 20.7mmHg vs 132.7 ± 20.7mmHg, p<0.05), but recovered to the baseline value at 30 min. No serious adverse event or event requiring treatment. CTCA analysis: Image Quality Score: both at optimal and at mid-diastole reconstruction a score of 2 or 3 was significantly higher in the landiolol group per subject, vessels and segment (p<0.0001). |
| Nakamura et al. 2014 [28] |
Single Center RCT |
Patients who underwent CTCA |
N = 354 patients 3 groups n1 = 188 (bolus dose of 0.125 mg/kg) n2 = 213 [bolus dose + 3.75mg) n3 = 277 oral propranolol 1.5 hours before CT |
(Efficacy) HR was significantly lower in the propranolol group (61.6 ± 8.0 bpm) than in the n1 group [64.1 ± 7.4/min, P < 0.001), but there was no significant difference in the image quality (P = 0.91). Average HR tended to be lower in n2 group (67.2 ± 6.9/min) compared with the n1 group [69.0 ± 6.9/min, P = 0.10) and there was a significant difference in image quality between these two groups (P = 0.02). (Safety): A patient developed bradycardia and another hypotension. They were asymptomatic and both recovered after 5min and 10min respectively. |
| Hirano et al 2013 [22] |
Multi Center Observational |
Patients with suspected ischemic cardiac disease | N = 90 patients 3groups of landiolol n1 = 0.125 mg/kg (Group L) n2 = 0.25 mg/kg (Group M) n3 = 0.5 mg/kg (Group H) CCTA 3-7 min after administration |
(Efficacy) HR reduced in all groups in a dose-dependent way (15.55 ± 6.56% in Group L, 16.48 ± 7.80% in Group M, and 21.49 ± 6.13% in Group H (Group L vs Group H, P = 0.0008; Group M vs Group H, P = 0.0109). (Safety) BP decrease was minimal in all groups and returned to baseline levels after administration. CTCA analysis: coronary stenosis was diagnosable in all groups with no significant difference. |
| Isobe et al. 2008 [23] |
Prospective Observational |
Patients with known or suspected CAD undergoing MSCT on admission to hospital | N = 145 patients receiving landiolol continuously injected 15min before starting MSCT CAG and stopped immediately after. Final dose of landiolol hydrochloride was 0.036± 0.005 mg·kg-1·min-1 |
(Efficacy) HR: significantly reduced during injection of landiolol hydrochloride (51.8±3.1beats/min, p< 0.0001), quickly recovered 15 min after cessation of injection (62.8±7.9beats/min), and was maintained until sleep. All patients achieved the target HR ≤55 beats/min at the start of the CT scan. Mean time to reach the target HR was 13.4±3.8 min. HR variability was significantly reduced during CT acquisition compared with before administration of landiolol. (Safety) BP: no significant changes were observed. No adverse effects were reported. (CCTA analysis) Per segment analysis and per-artery analysis were performed |
| Koyoshi et al. 2018 [29] |
Single Center Prospective |
CTA for suspected CAD or at least onecardiac risk factor | N = 176 patients One bolus injection of landiolol (16.1 ± 7.4 mg) 4min before scan. |
(Efficacy) HR before administration, after administration and in the end of scan: 83 ± 10 bpm, 62 ± 7bpm and 69 ± 8 bpm respectively (p<0.001)) HR upon entry to the CT room: 70 - 79 bpm (74 ± 3 bpm) (n = 76): 61 ± 6 bpm during scan 80 - 89 bpm (84 ± 3) (n = 60): 63 ± 7 bpm during scan ≥ 90 bpm (98 ± 6) (n = 40): 65 ± 7 bpm during scan (Safety) SBP/DBP from 136 ± 17/80 ± 12 before scan to 123 ± 18/72 ± 12 mmHg after scan, 8 patients (4.5%) had adverse events, but none was severe or required stopping drug administration. |
| Kido et al. 2016 [24] |
Multi Center Prospective |
CTCA for suspected ischemic heart disease | N = 219 patients | (Efficacy) Mean HR after administration was 59.9±6.4 bpm compared to 69.3±7.3 bpm before, P<0.001. 80% of the patients achieved HR ≤65 bpm. (Safety) HR and BP of all the patients recovered after the scan. No adverse events during the study. (CCTA analysis) The mean radiation dose was 50% derived from the inferred dose before use of landiolol (4.5±3.2 vs. 9.0±3.7 mSv; P<0.001). |
| Kokubo et al. 2022 [25] |
Single Center Retrospective |
CTCA for suspected ischemic heart disease | N = 142/244 patients received landiolol |
(Efficacy) HR decreased significantly (p < 0.001). No significant changes on EF. |
| Barwig et al. 2025 [26] |
Single Center Retrospective |
Patients with HR > 60bpm underwent CTCA | N = 37 patients N1: 23 patients without oral BB premedication N2: 14 with prior BB use Fractional administration 1 – 5 doses (60mg) mean dose (± SD): 0.526 ± 0.3 mg/kg |
(Efficacy) HR ≤ 60 bpm was achieved in 13 patients (35%) and a HR≤ 65 bpm was achieved in 25 patients (68%). Mean ± SD of HR before and during CT: −11 ± 9 bpm in total, −14 ± 10 bpm in group 1 and −6 ± 5 bpm in group 2. Statistically significant in all groups. (Safety) No adverse effects occurred. |
| Osawa et al. 2013 [27] |
Single Center Observational |
Patients who underwent MDCT coronary angiography |
N = 66 patients received landiolol | (Efficacy) HR significantly reduced 5 minutes after injection of landiolol and recovered shortly after. (Safety) SBP did not decrease significantly. Adverse events not observed in patients receiving landiolol. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





