Submitted:
23 June 2025
Posted:
24 June 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
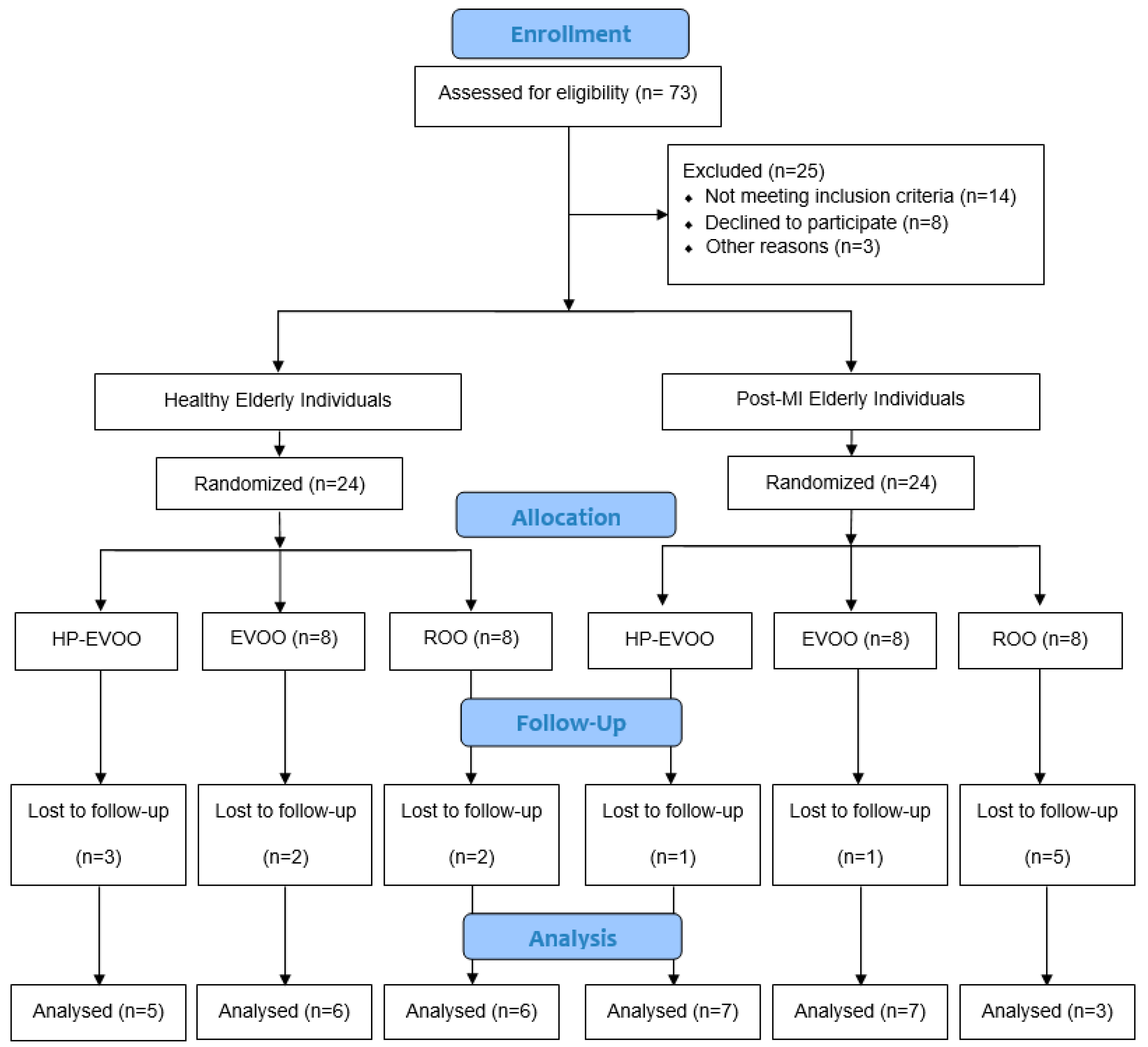
2.1. Study Design and Subjects
2.2. Olive Oils
2.3. Blood Collection
2.4. Biochemical Analyses
2.4.1. Plasma Total (poly)phenols Measurement
2.4.2. Ferric Reducing Antioxidant Power (FRAP)
2.4.3. PON-1 Activity Measurement
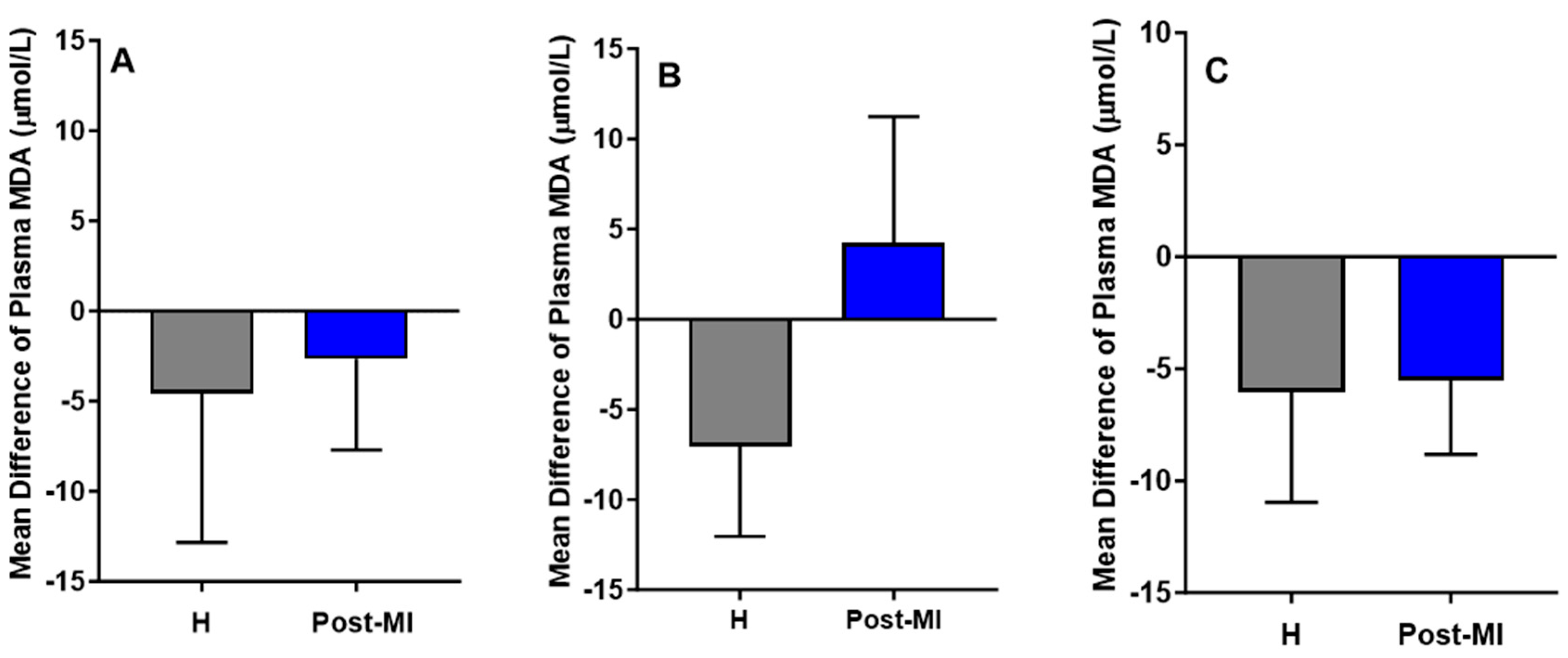
2.4.4. MDA Measurement
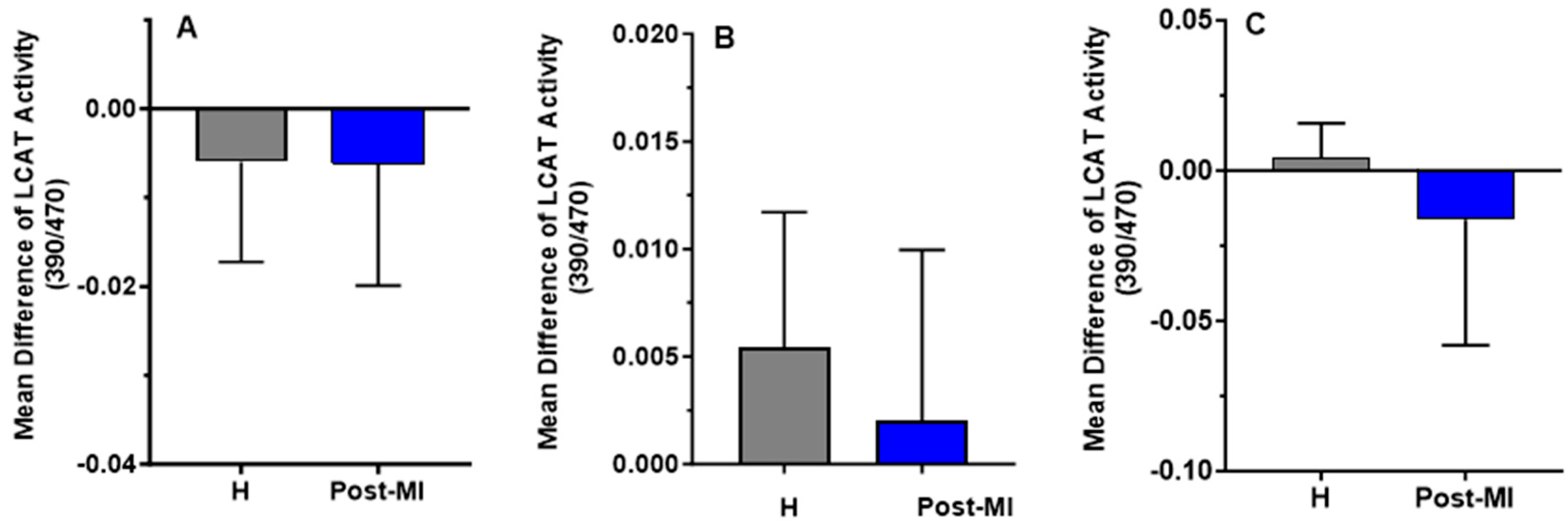
2.4.5. LCAT Activity Measurement
2.5. Statistical Analysis
3. Results
3.1. Participants Characteristics
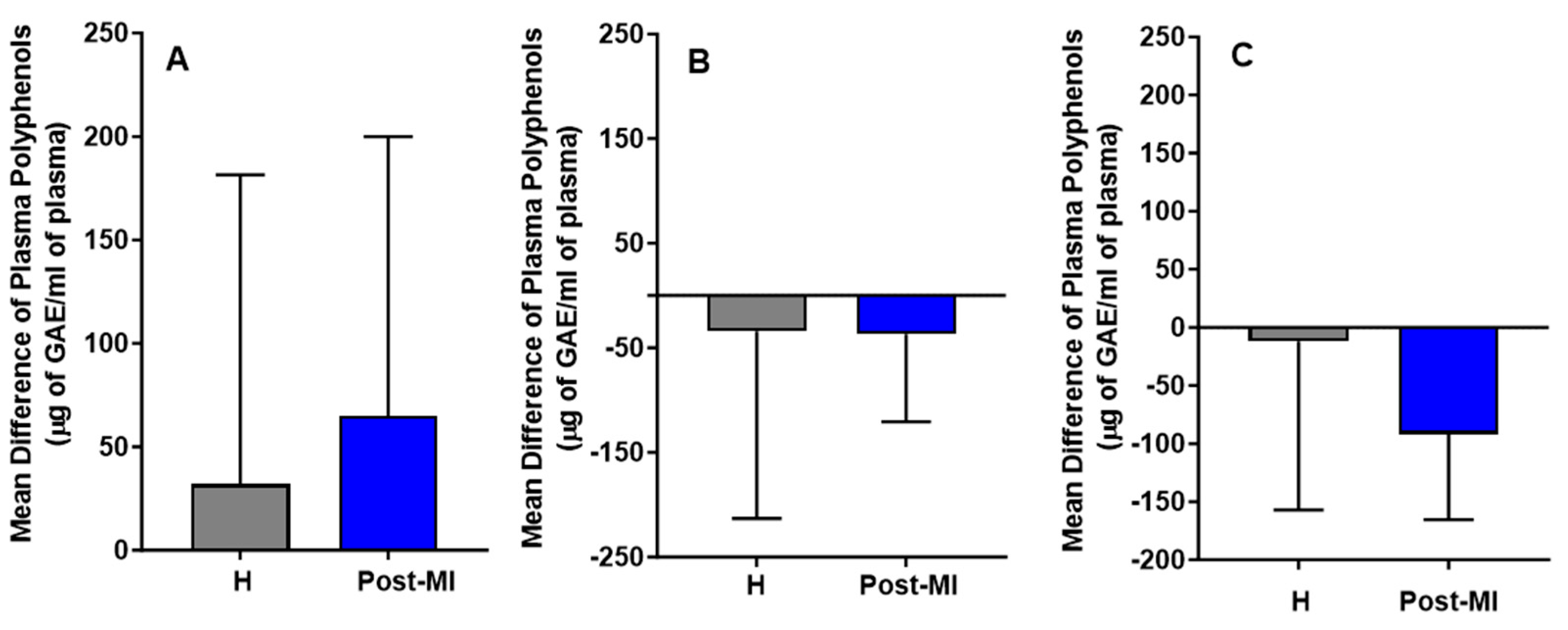
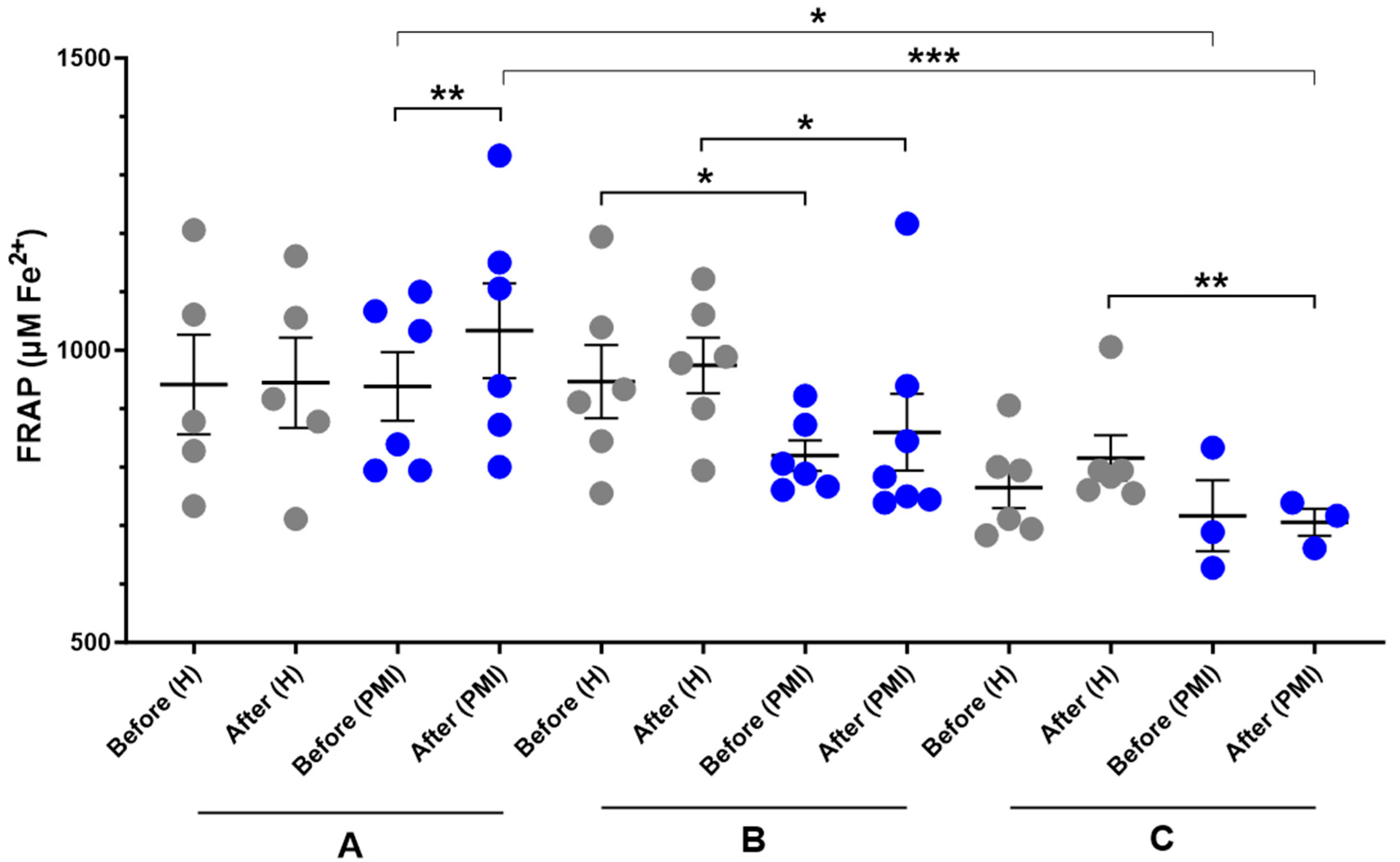
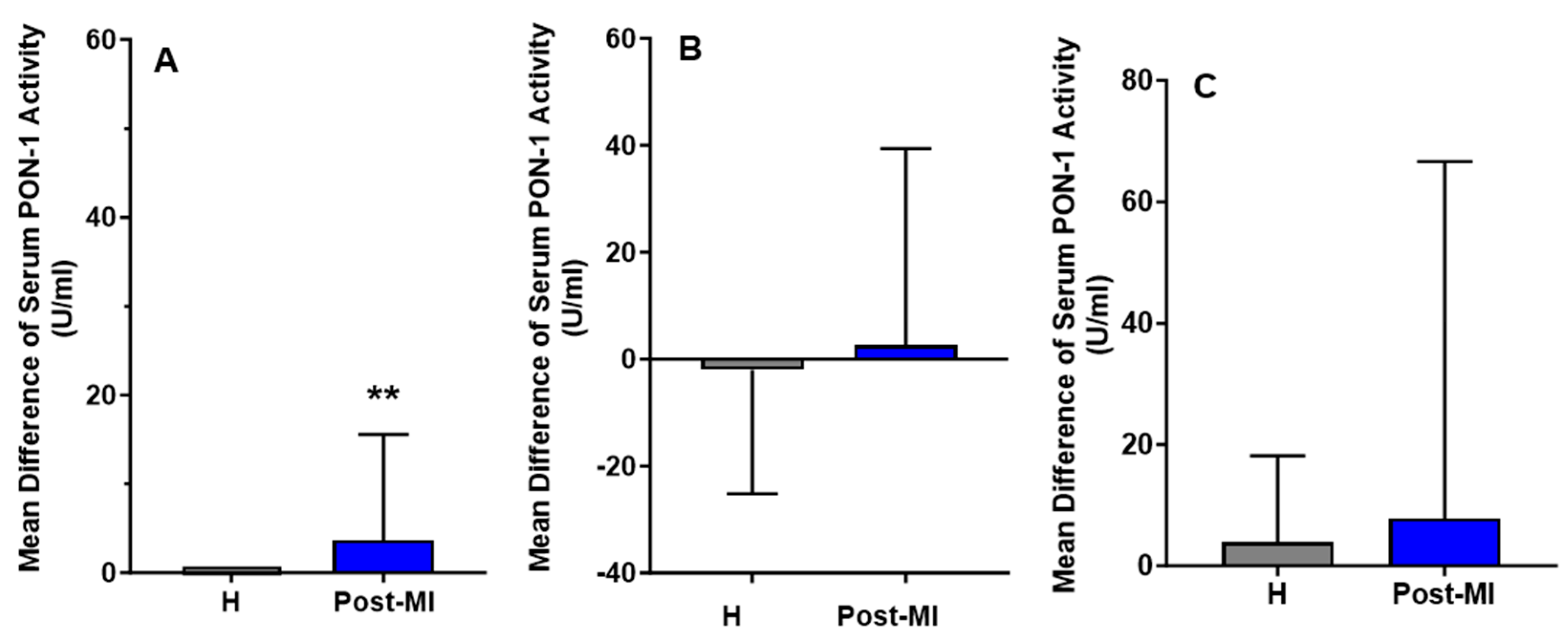
3.2. Biochemical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nedkoff L, Briffa T, Zemedikun D, Herrington S, Wright FL. Global Trends in Atherosclerotic Cardiovascular Disease. Clin Ther. 2023 Nov;45(11):1087–91. [CrossRef]
- Wolf D, Ley K. Immunity and Inflammation in Atherosclerosis. Circ Res. 2019 Jan 18;124(2):315–27.
- Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, et al. Atherosclerosis. Nature Reviews Disease Primers. 2019 Aug 16;5(1):56.
- Kariuki JK, Imes CC, Engberg SJ, Scott PW, Klem ML, Cortes YI. Impact of lifestyle-based interventions on absolute cardiovascular disease risk: a systematic review and meta-analysis. JBI Evid Synth. 2024 Jan 1;22(1):4–65. [CrossRef]
- Zhang W, Zheng Y, Yan F, Dong M, Ren Y. Research progress of quercetin in cardiovascular disease. Front Cardiovasc Med. 2023;10:1203713. [CrossRef]
- Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Cerletti C, et al. Interaction between Mediterranean diet and statins on mortality risk in patients with cardiovascular disease: Findings from the Moli-sani Study. Int J Cardiol. 2019 Feb 1;276:248–54. [CrossRef]
- Guasch-Ferré M, Hu FB, Martínez-González MA, Fitó M, Bulló M, Estruch R, et al. Olive oil intake and risk of cardiovascular disease and mortality in the PREDIMED Study. BMC Med. 2014 May 13;12:78.
- Guo X, Tresserra-Rimbau A, Estruch R, Martínez-González MA, Medina-Remón A, Castañer O, et al. Effects of Polyphenol, Measured by a Biomarker of Total Polyphenols in Urine, on Cardiovascular Risk Factors After a Long-Term Follow-Up in the PREDIMED Study. Oxid Med Cell Longev. 2016;2016:2572606.
- Covas MI, Nyyssönen K, Poulsen HE, Kaikkonen J, Zunft HJF, Kiesewetter H, et al. The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann Intern Med. 2006 Sep 5;145(5):333–41.
- Perrone MA, Gualtieri P, Gratteri S, Ali W, Sergi D, Muscoli S, et al. Effects of postprandial hydroxytyrosol and derivates on oxidation of LDL, cardiometabolic state and gene expression: a nutrigenomic approach for cardiovascular prevention. J Cardiovasc Med (Hagerstown). 2019 Jul;20(7):419–26.
- Boronat A, Mateus J, Soldevila-Domenech N, Guerra M, Rodríguez-Morató J, Varon C, et al. Cardiovascular benefits of tyrosol and its endogenous conversion into hydroxytyrosol in humans. A randomized, controlled trial. Free Radic Biol Med. 2019 Nov 1;143:471–81. [CrossRef]
- EFSA Panel on Dietetic Products N and A (NDA). Scientific opinion on the substantiation of health claims related to polyphenols in olive and protection of LDL particles from oxidative damage (ID 1333, 1638, 1639, 1696, 2865), maintenance of normal blood HDL cholesterol concentrations (ID 1639), maintenance of normal blood pressure (ID 3781),“anti-inflammatory properties”(ID 1882),“contributes to the upper respiratory tract health”(ID 3468),“can help to maintain a normal function of gastrointestinal tract”(3779), and “contributes to body defences against external agents”(ID 3467) pursuant to Article 13 (1) of Regulation (EC) No 1924/2006. EFSA journal. 2011;9(4):2033.
- Mancebo-Campos V, Salvador MD, Fregapane G. EFSA Health Claims-Based Virgin Olive Oil Shelf-Life. Antioxidants (Basel). 2023 Aug 4;12(8). [CrossRef]
- Visioli F, Poli A, Gall C. Antioxidant and other biological activities of phenols from olives and olive oil. Med Res Rev. 2002 Jan;22(1):65–75.
- De la Torre-Carbot K, Jauregui O, Gimeno E, Castellote AI, Lamuela-Raventós RM, López-Sabater MC. Characterization and quantification of phenolic compounds in olive oils by solid-phase extraction, HPLC-DAD, and HPLC-MS/MS. Journal of agricultural and food chemistry. 2005;53(11):4331–40. [CrossRef]
- Fitó M, Cladellas M, De La Torre R, Marti J, Alcántara M, Pujadas-Bastardes M, et al. Antioxidant effect of virgin olive oil in patients with stable coronary heart disease: a randomized, crossover, controlled, clinical trial. Atherosclerosis. 2005;181(1):149–58. [CrossRef]
- Zrelli H, Kusunoki M, Miyazaki H. Role of hydroxytyrosol-dependent regulation of HO-1 expression in promoting wound healing of vascular endothelial cells via Nrf2 de novo synthesis and stabilization. Phytotherapy Research. 2015;29(7):1011–8. [CrossRef]
- Wang W chen, Xia Y min, Yang B, Su X ni, Chen J kuan, Li W, et al. Protective Effects of Tyrosol against LPS-Induced Acute Lung Injury via Inhibiting NF-κB and AP-1 Activation and Activating the HO-1/Nrf2 Pathways. Biological and Pharmaceutical Bulletin. 2017;40(5):583–93.
- Vijakumaran U, Shanmugam J, Heng JW, Azman SS, Yazid MD, Haizum Abdullah NA, et al. Effects of Hydroxytyrosol in Endothelial Functioning: A Comprehensive Review. Molecules. 2023 Feb 16;28(4). [CrossRef]
- Karković Marković A, Torić J, Barbarić M, Jakobušić Brala C. Hydroxytyrosol, Tyrosol and Derivatives and Their Potential Effects on Human Health. Molecules. 2019 May 24;24(10).
- Hohmann CD, Cramer H, Michalsen A, Kessler C, Steckhan N, Choi K, et al. Effects of high phenolic olive oil on cardiovascular risk factors: A systematic review and meta-analysis. Phytomedicine. 2015 Jun 1;22(6):631–40.
- George ES, Marshall S, Mayr HL, Trakman GL, Tatucu-Babet OA, Lassemillante ACM, et al. The effect of high-polyphenol extra virgin olive oil on cardiovascular risk factors: A systematic review and meta-analysis. Critical Reviews in Food Science and Nutrition. 2019 Sep 25;59(17):2772–95. [CrossRef]
- Morvaridzadeh M, Cohen AA, Heshmati J, Alami M, Berrougui H, Zoubdane N, et al. Effect of Extra Virgin Olive Oil on Anthropometric Indices, Inflammatory and Cardiometabolic Markers: a Systematic Review and Meta-Analysis of Randomized Clinical Trials. The Journal of Nutrition. 2024 Jan 1;154(1):95–120. [CrossRef]
- Feingold KR, Grunfeld C. Effect of inflammation on HDL structure and function. Current Opinion in Lipidology [Internet]. 2016;27(5). Available from: https://journals.lww.com/co-lipidology/fulltext/2016/10000/effect_of_inflammation_on_hdl_structure_and.12.aspx.
- Oprescu N, Micheu MM, Scafa-Udriste A, Popa-Fotea NM, Dorobantu M. Inflammatory markers in acute myocardial infarction and the correlation with the severity of coronary heart disease. Ann Med. 2021 Dec;53(1):1041–7. [CrossRef]
- Djekic S, Vekic J, Zeljkovic A, Kotur-Stevuljevic J, Kafedzic S, Zdravkovic M, et al. HDL Subclasses and the Distribution of Paraoxonase-1 Activity in Patients with ST-Segment Elevation Acute Myocardial Infarction. International Journal of Molecular Sciences. 2023;24(11). [CrossRef]
- Annema W, Willemsen HM, de Boer JF, Dikkers A, van der Giet M, Nieuwland W, et al. HDL function is impaired in acute myocardial infarction independent of plasma HDL cholesterol levels. Journal of clinical lipidology. 2016;10(6):1318–28. [CrossRef]
- Li S, Peng Y, Wang X, Qian Y, Xiang P, Wade SW, et al. Cardiovascular events and death after myocardial infarction or ischemic stroke in an older Medicare population. Clin Cardiol. 2019 Mar;42(3):391–9. [CrossRef]
- Farràs M, Fernández-Castillejo S, Rubió L, Arranz S, Catalán Ú, Subirana I, et al. Phenol-enriched olive oils improve HDL antioxidant content in hypercholesterolemic subjects. A randomized, double-blind, cross-over, controlled trial. The Journal of Nutritional Biochemistry. 2018 Jan 1;51:99–104. [CrossRef]
- Serafini M, Maiani G, Ferro-Luzzi A. Alcohol-free red wine enhances plasma antioxidant capacity in humans. J Nutr. 1998 Jun;128(6):1003–7. [CrossRef]
- Seres I, Paragh G, Deschene E, Fulop TJ, Khalil A. Study of factors influencing the decreased HDL associated PON1 activity with aging. Exp Gerontol. 2004 Jan;39(1):59–66. [CrossRef]
- Nezami N, Ghorbanihaghjo A, Rashtchizadeh N, Argani H, Tafrishinejad A, Ghorashi S, et al. Atherogenic changes of low-density lipoprotein susceptibility to oxidation, and antioxidant enzymes in pulmonary tuberculosis. Atherosclerosis. 2011 Jul;217(1):268–73. [CrossRef]
- Yagi, K. Yagi K. A simple fluorometric assay for lipoperoxide in blood plasma. Biochem Med. 1976 Apr;15(2):212–6. [CrossRef]
- Bender C, Strassmann S, Golz C. Oral Bioavailability and Metabolism of Hydroxytyrosol from Food Supplements. Nutrients. 2023 Jan 9;15(2). [CrossRef]
- Pastor A, Rodríguez-Morató J, Olesti E, Pujadas M, Pérez-Mañá C, Khymenets O, et al. Analysis of free hydroxytyrosol in human plasma following the administration of olive oil. Journal of Chromatography A. 2016 Mar 11;1437:183–90. [CrossRef]
- Alemán-Jiménez C, Domínguez-Perles R, Medina S, Prgomet I, López-González I, Simonelli-Muñoz A, et al. Pharmacokinetics and bioavailability of hydroxytyrosol are dependent on the food matrix in humans. Eur J Nutr. 2021 Mar;60(2):905–15. [CrossRef]
- de Bock M, Thorstensen EB, Derraik JGB, Henderson HV, Hofman PL, Cutfield WS. Human absorption and metabolism of oleuropein and hydroxytyrosol ingested as olive (Olea europaea L.) leaf extract. Mol Nutr Food Res. 2013 Nov;57(11):2079–85. [CrossRef]
- Wood E, Hein S, Mesnage R, Fernandes F, Abhayaratne N, Xu Y, et al. Wild blueberry (poly)phenols can improve vascular function and cognitive performance in healthy older individuals: a double-blind randomized controlled trial. Am J Clin Nutr. 2023 Jun;117(6):1306–19. [CrossRef]
- Ruiz-García I, Ortíz-Flores R, Badía R, García-Borrego A, García-Fernández M, Lara E, et al. Rich oleocanthal and oleacein extra virgin olive oil and inflammatory and antioxidant status in people with obesity and prediabetes. The APRIL study: A randomised, controlled crossover study. Clin Nutr. 2023 Aug;42(8):1389–98. [CrossRef]
- Poznyak AV, Nikiforov NG, Markin AM, Kashirskikh DA, Myasoedova VA, Gerasimova EV, et al. Overview of OxLDL and its impact on cardiovascular health: focus on atherosclerosis. Frontiers in Pharmacology. 2021;11:613780. [CrossRef]
- Jiang H, Zhou Y, Nabavi SM, Sahebkar A, Little PJ, Xu S, et al. Mechanisms of oxidized LDL-mediated endothelial dysfunction and its consequences for the development of atherosclerosis. Frontiers in cardiovascular medicine. 2022;9:925923. [CrossRef]
- Tsutsui T, Tsutamoto T, Wada A, Maeda K, Mabuchi N, Hayashi M, et al. Plasma oxidized low-density lipoprotein as a prognostic predictor in patients with chronic congestive heart failure. J Am Coll Cardiol. 2002 Mar 20;39(6):957–62. [CrossRef]
- Lopez-Huertas E, Fonolla J. Hydroxytyrosol supplementation increases vitamin C levels in vivo. A human volunteer trial. Redox Biology. 2017;11:384–9. [CrossRef]
- Jemai H, Fki I, Bouaziz M, Bouallagui Z, El Feki A, Isoda H, et al. Lipid-Lowering and Antioxidant Effects of Hydroxytyrosol and Its Triacetylated Derivative Recovered from Olive Tree Leaves in Cholesterol-Fed Rats. J Agric Food Chem. 2008 Apr 1;56(8):2630–6. [CrossRef]
- Calabriso N, Gnoni A, Stanca E, Cavallo A, Damiano F, Siculella L, et al. Hydroxytyrosol ameliorates endothelial function under inflammatory conditions by preventing mitochondrial dysfunction. Oxidative medicine and cellular longevity. 2018;2018(1):9086947. [CrossRef]
- Fitó M, Cladellas M, de la Torre R, Martí J, Alcántara M, Pujadas-Bastardes M, et al. Antioxidant effect of virgin olive oil in patients with stable coronary heart disease: a randomized, crossover, controlled, clinical trial. Atherosclerosis. 2005 Jul 1;181(1):149–58. [CrossRef]
- Ikonomidis I, Katogiannis K, Chania C, Iakovis N, Tsoumani M, Christodoulou A, et al. Association of hydroxytyrosol enriched olive oil with vascular function in chronic coronary disease. European Journal of Clinical Investigation. 2023 Jul 1;53(7):e13983. [CrossRef]
- Colica C, Di Renzo L, Trombetta D, Smeriglio A, Bernardini S, Cioccoloni G, et al. Antioxidant Effects of a Hydroxytyrosol-Based Pharmaceutical Formulation on Body Composition, Metabolic State, and Gene Expression: A Randomized Double-Blinded, Placebo-Controlled Crossover Trial. Oxid Med Cell Longev. 2017;2017:2473495.
- Vissers M, Zock P, Wiseman S, Meyboom S, Katan M. Effect of phenol-rich extra virgin olive oil on markers of oxidation in healthy volunteers. European Journal of Clinical Nutrition. 2001 May 1;55(5):334–41.
- Quirós-Fernández R, López-Plaza B, Bermejo LM, Palma-Milla S, Gómez-Candela C. Supplementation with Hydroxytyrosol and Punicalagin Improves Early Atherosclerosis Markers Involved in the Asymptomatic Phase of Atherosclerosis in the Adult Population: A Randomized, Placebo-Controlled, Crossover Trial. Nutrients. 2019 Mar 16;11(3). [CrossRef]
- Sirca TB, Mureșan ME, Pallag A, Marian E, Jurca T, Vicaș LG, et al. The Role of Polyphenols in Modulating PON1 Activity Regarding Endothelial Dysfunction and Atherosclerosis. Int J Mol Sci. 2024 Mar 4;25(5). [CrossRef]
- Mahrooz, A. Mahrooz A. Chapter Three - Pleiotropic functions and clinical importance of circulating HDL-PON1 complex. In: Makowski GS, editor. Advances in Clinical Chemistry [Internet]. Elsevier; 2024. p. 132–71. Available from: https://www.sciencedirect.com/science/article/pii/S0065242324000647.
- Kumar M, Ali W, Yadav K, Kaumri S, Mishra S, Nardi P, et al. High-Density Lipoprotein-Associated Paraoxonase-1 (PON-1) and Scavenger Receptor Class B Type 1 (SRB-1) in Coronary Artery Disease: Correlation with Disease Severity. Journal of Clinical Medicine. 2024;13(18). [CrossRef]
- Durrington PN, Bashir B, Soran H. Paraoxonase 1 and atherosclerosis. Frontiers in Cardiovascular Medicine. 2023;10:1065967.
- Manning PJ, Jong SA de, Ryalls AR, Sutherland WHF. Paraoxonase 1 activity in chylomicrons and VLDL: the effect of type 2 diabetes and meals rich in saturated fat and oleic acid. Lipids. 2012;47(3):259–67. [CrossRef]
- Boshtam M, Razavi AE, Pourfarzam M, Ani M, Naderi GA, Basati G, et al. Serum paraoxonase 1 activity is associated with fatty acid composition of high density lipoprotein. Dis Markers. 2013;35(4):273–80. [CrossRef]
- Farràs M, Castañer O, Martín-Peláez S, Hernáez Á, Schröder H, Subirana I, et al. Complementary phenol-enriched olive oil improves HDL characteristics in hypercholesterolemic subjects. A randomized, double-blind, crossover, controlled trial. The VOHF study. Molecular Nutrition & Food Research. 2015 Sep 1;59(9):1758–70.
- Oldoni F, Baldassarre D, Castelnuovo S, Ossoli A, Amato M, van Capelleveen J, et al. Complete and partial lecithin: cholesterol acyltransferase deficiency is differentially associated with atherosclerosis. Circulation. 2018;138(10):1000–7. [CrossRef]
- Kunnen S, Van Eck M. Lecithin: cholesterol acyltransferase: old friend or foe in atherosclerosis? Journal of lipid research. 2012;53(9):1783–99.
- Ossoli A, Pavanello C, Calabresi L. High-Density Lipoprotein, Lecithin: Cholesterol Acyltransferase, and Atherosclerosis. Endocrinol Metab. 2016 Jun 10;31(2):223–9.
- Tanigawa H, Billheimer JT, Tohyama J ichiro, Fuki IV, Ng DS, Rothblat GH, et al. Lecithin: cholesterol acyltransferase expression has minimal effects on macrophage reverse cholesterol transport in vivo. Circulation. 2009 Jul 14;120(2):160–9.
- Calabresi L, Baldassarre D, Simonelli S, Gomaraschi M, Amato M, Castelnuovo S, et al. Plasma lecithin:cholesterol acyltransferase and carotid intima-media thickness in European individuals at high cardiovascular risk. J Lipid Res. 2011 Aug;52(8):1569–74. [CrossRef]
- Stadler JT, Bärnthaler T, Borenich A, Emrich IE, Habisch H, Rani A, et al. Low LCAT activity is linked to acute decompensated heart failure and mortality in patients with CKD. Journal of Lipid Research [Internet]. 2024 Sep 1 [cited 2025 May 26];65(9). [CrossRef]
| HP-EVOO | EVOO | ROO | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy | Post-MI | p-value (Between groups) |
Healthy | Post-MI | p-value (Between groups) |
Healthy | Post-MI | p-value (Between groups) |
||
| Sex | Women | 1 | 1 | 3 | 2 | 4 | 1 | |||
| Men | 4 | 6 | 3 | 5 | 2 | 2 | ||||
| Age | 71 ± 2.34 | 75.71 ± 2.97 | 0.272 | 76.67 ± 1.82 | 71.5 ± 2.19 | 0.124 | 76 ± 2.87 | 73.67 ± 2.33 | 0.618 | |
|
Weight (kg) |
Before | 94 ± 15.70 | 79.79 ± 4.66 | 0.339 | 68.85 ± 7.37 | 73.13 ± 3.15 | 0.584 | 78.78 ± 5.34 | 81.73 ± 14.09 | 0.814 |
| After | 95.62 ± 16.82 | 80.58 ± 4.98 | 0.376 | 69.32 ± 6.90 | 75.96 ± 2.98 | 0.433 | 81.83 ± 4.10 | 82.83 ± 13.06 | 0.714 | |
|
p-value (Within groups) |
0.300 | 0.062 | 0.473 | 0.909 | 0.156 | 0.641 | ||||
|
BMI (kg/m2) |
Before | 31.51 ± 4.85 | 26.58 ± 1.06 | 0.431 | 25.70 ± 2.00 | 27.15 ± 1.08 | 0.521 | 28.47 ± 1.86 | 28.33 ± 2.75 | 0.969 |
| After | 32.05 ± 5.20 | 27.08 ± 1.19 | 0.536 | 25.93 ± 1.88 | 28.09 ± 1.274 | 0.536 | 29.61 ± 1.60 | 28.97 ± 2.48 | 0.828 | |
|
p-value (Within groups) |
0.307 | 0.062 | 0.385 | 0.812 | 0.184 | 0.318 | ||||
|
Systolic BP (mmHg) |
Before | 143.4 ± 6.76 | 147.0 ± 9.27 | 0.778 | 136.4 ± 6.50 | 131.1 ± 2.50 | 0.413 | 146.0 ± 9.55 | 132.0 ± 1.52 | 0.351 |
| After | 144.4 ± 5.51 | 126.0 ± 9.15 | 0.137 | 124.3 ± 11.83 | 137.0 ± 7.50 | 0.412 | 141.8 ± 12.38 | 136.3 ± 12.12 | 0.789 | |
|
p-value (Within groups) |
0.731 | 0.051 | 0.366 | 0.589 | 0.539 | 0.730 | ||||
|
Diastolic BP (mmHg) |
Before | 82.60 ± 1.36 | 76.14 ± 1.80 | 0.024 | 80.20 ± 11.18 | 79.57 ± 2.25 | 0.406 | 81.50 ± 2.66 | 78.33 ± 2.66 | 0.357 |
| After | 84.40 ± 1.36 | 79.50 ± 3.87 | 0.299 | 74.50 ± 3.83 | 81.00 ± 5.814 | 0.684 | 80.33 ± 4.74 | 78.33 ± 6.36 | 0.812 | |
|
p-value (Within groups) |
0.321 | 0.328 | >0.999 | 0.812 | 0.672 | >0.999 | ||||
| CRP (mg/L) | Before | 2.60 ± 1.10 | 2.957 ± 1.31 | 0.621 | 1.95 ± 0.52 | 1.14 ± 0.19 | 0.188 | 1.13 ± 0.24 | 1.63 ± 0.73 | 0.690 |
| After | 2.48 ± 1.65 | 1.817 ± 0.48 | 0.541 | 2.23 ± 0.58 | 1.15 ± 0.22 | 0.162 | 1.20 ± 0.18 | 0.70 ± 0.10 | 0.059 | |
|
p-value (Within groups) |
> 0.999 | >0.999 | 0.377 | 0.500 | 0.562 | 0.500 | ||||
| TC (mmol/L) | Before | 4.89 ± 0.29 | 3.12±0.22 | 0.0007 | 5.07 ± 0.25 | 3.15 ± 0.19 | 0.0003 | 4.71 ± 0.27 | 3.09 ± 0.09 | 0.0054 |
| After | 4.89 ± 0.29 | 3.30±0.27 | 0.003 | 5.375 ± 0.18 | 3.08 ± 0.16 | <0.0001 | 4.81 ± 0.49 | 3.05 ± 0.11 | 0.047 | |
|
p-value (Within groups) |
0.991 | 0.575 | 0.179 | 0.654 | 0.739 | 0.269 | ||||
| TG (mmol/L) | Before | 1.11 ± 0.35 | 1.21 ± 0.26 | >0.999 | 1.38 ± 0.22 | 1.15 ± 0.35 | 0.400 | 0.88 ± 0.13 | 0.87 ± 0.07 | 0.956 |
| After | 0.95 ± 0.17 | 1.62 ± 0.48 | 0.258 | 1.45 ± 0.31 | 0.84 ± 0.061 | 0.063 | 0.98 ± 0.10 | 0.85 ± 0.10 | 0.479 | |
|
p-value (Within groups) |
0.437 | 0.313 | 0.710 | 0.812 | 0.528 | 0.431 | ||||
| HDL-C (mmol/L) | Before | 1.72 ± 0.23 | 1.13 ± 0.11 | 0.031 | 1.59 ± 0.25 | 1.18 ± 0.11 | 0.202 | 1.69 ± 0.15 | 1.28 ± 0.08 | 0.125 |
| After | 1.79 ± 0.24 | 1.13 ± 0.16 | 0.048 | 1.68 ± 0.27 | 1.27 ± 0.09 | 0.167 | 1.69 ± 0.18 | 1.390 ± 0.09 | 0.316 | |
|
p-value (Within groups) |
0.380 | 0.486 | 0.082 | 0.425 | 0.957 | 0.085 | ||||
|
LDL-C (mmol/L) |
Before | 2.66 ± 0.31 | 1.43 ± 0.24 | 0.010 | 2.84 ± 2.84 | 1.44 ± 0.10 | 0.0001 | 2.61 ± 0.21 | 1.41 ± 0.03 | 0.006 |
| After | 2.66 ± 0.26 | 1.42 ± 0.24 | 0.007 | 3.02 ± 0.11 | 1.42 ± 0.10 | <0.0001 | 2.68 ± 0.35 | 1.27 ± 0.07 | 0.030 | |
|
p-value (Within groups) |
0.961 | 0.724 | 0.344 | 0.897 | 0.765 | 0.063 | ||||
|
non-HDL-C (mmol/L) |
Before | 3.07 ± 0.42 | 1.99 ± 0.23 | 0.035 | 3.47 ± 0.23 | 1.92 ± 0.13 | 0.002 | 3.01 ± 0.18 | 1.81 ± 0.01 | 0.002 |
| After | 3.10 ± 0.26 | 2.17 ± 0.18 | 0.016 | 3.68 ± 0.17 | 1.80 ± 0.14 | <0.0001 | 3.12 ± 0.34 | 1.66±0.037 | 0.022 | |
|
p-value (Within groups) |
0.668 | 0.665 | 0.312 | 0.602 | 0.671 | 0.021 | ||||
| Lp (a) (nmol/L) | Before | 32.56 ± 10.69 | 71.55 ± 34.68 | 0.349 | 52.82 ± 45.12 | 72.06 ± 29.37 | 0.190 | 114.1 ± 29.97 | 141.4 ± 51.41 | 0.635 |
| After | 31.56 ± 10.52 | 89.67 ± 40.08 | 0.231 | 60.82 ± 50.50 | 104.1 ± 43.38 | 0.142 | 107.0 ± 24.09 | 81.00 ± 13.23 | 0.497 | |
|
p-value (Within groups) |
0.228 | 0.353 | 0.250 | 0.437 | 0.601 | 0.263 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





