Submitted:
17 June 2025
Posted:
18 June 2025
You are already at the latest version
Abstract

Keywords:
1. Introduction
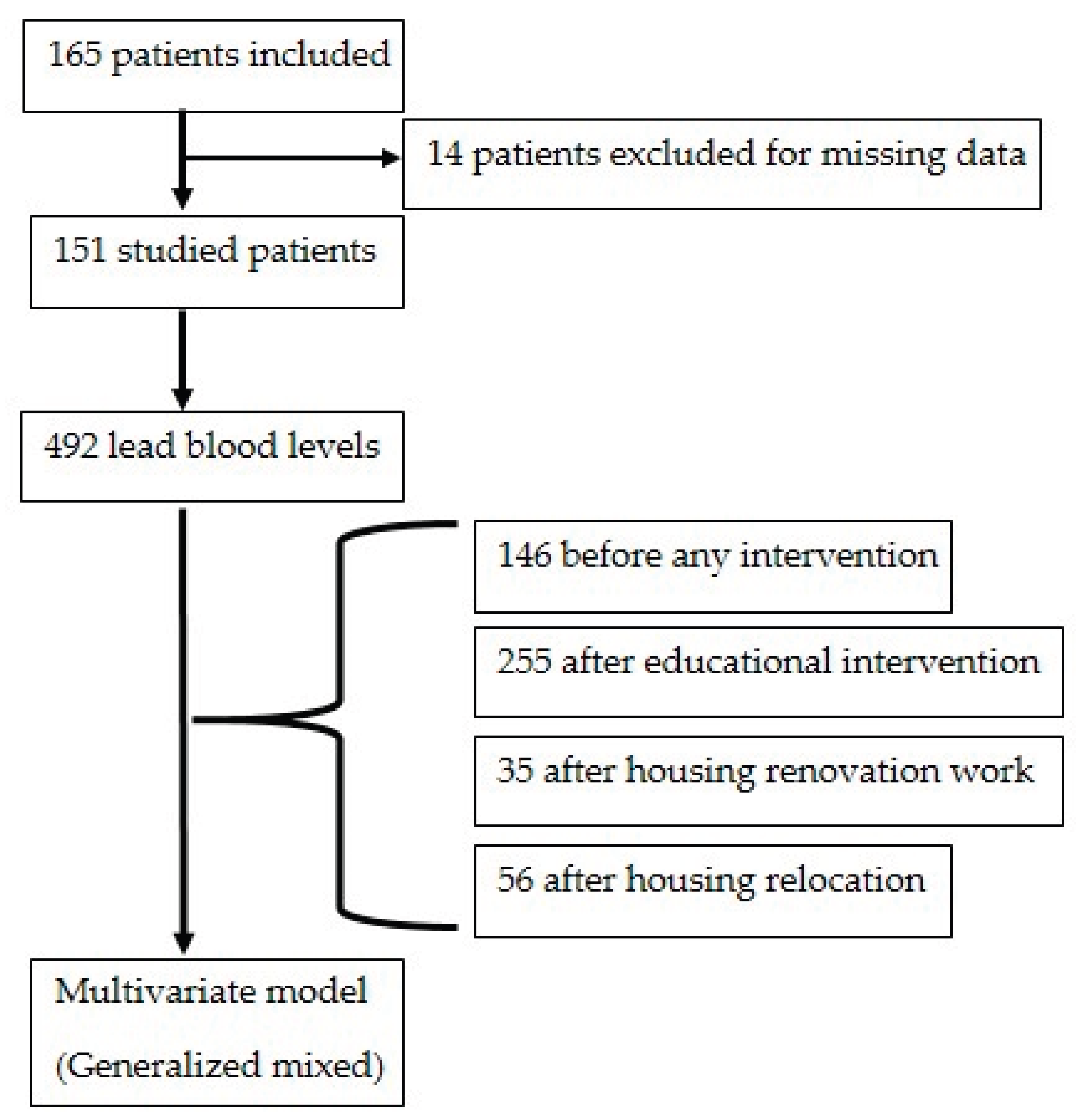
2. Materials and Methods
3. Results
3.1. Initial Situation
3.2. Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HEPA | High-Efficiency Particulate Air |
| RCT | Randomized Control Trial |
References
- Environmental burden of disease associated with inadequate housing: a method guide to the quantification of health effects of selected housing risks in the WHO European Region. Accessed April 19, 2025. https://www.who.int/publications/i/item/9789289057899.
- Saturnisme de l’enfant. Accessed April 17, 2025. https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-de-la-mere-et-de-l-enfant/saturnisme-de-l-enfant.
- Détermination de nouveaux objectifs de gestion des expositions au plomb. Accessed June 11, 2025. https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=444.
- Rollin L, Carré N, Garnier R, Greater Paris lead poisoning monitoring system (système de surveillance du saturnisme en Ile-de-France [SSSILF]). Follow-up of children suffering from lead poisoning or at risk of lead poisoning in Greater Paris, 1992--2002. Rev Epidemiol Sante Publique. 2008;56(6):391-397. [CrossRef]
- Solet JL, Renault P, Denys JC, et al. [Discovery and follow-up of a lead-poisoning outbreak in a shantytown of Le Port, Reunion Island]. Rev Epidemiol Sante Publique. 2013;61(4):329-337. [CrossRef]
- Chapitre IV : Lutte contre la présence de plomb ou d’amiante. (Articles L1334-1 à L1334-17) - Légifrance. Accessed April 17, 2025. https://www.legifrance.gouv.fr/codes/section_lc/LEGITEXT000006072665/LEGISCTA000006171529/#LEGISCTA000050703003.
- HCSP. Mise à jour du guide pratique de dépistage et de prise en charge des expositions au plomb chez l’enfant mineur et la femme enceinte. Haut Conseil de la Santé Publique; 2017. Accessed April 17, 2025. https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=643.
- Amitai Y, Graef JW, Brown MJ, Gerstle RS, Kahn N, Cochrane PE. Hazards of “deleading” homes of children with lead poisoning. Am J Dis Child 1960. 1987;141(7):758-760. [CrossRef]
- Shani Z, Scott RG, Schofield LS, et al. Effect of a home intervention program on pediatric asthma in an environmental justice community. Health Promot Pract. 2015;16(2):291-298. [CrossRef]
- de Blay F, Fourgaut G, Hedelin G, et al. Medical Indoor Environment Counselor (MIEC): role in compliance with advice on mite allergen avoidance and on mite allergen exposure. Allergy. 2003;58(1):27-33. [CrossRef]
- Montaudié-Dumas I, Giovannini-Chami L, Debai C, et al. [Impact on the indoor environment of allergic children of the medical counselor on indoor environment, after two successive visits at 6 months interval]. Arch Pediatr Organe Off Soc Francaise Pediatr. 2013;20(12):1288-1295. [CrossRef]
- Yeoh B, Woolfenden S, Wheeler D, Alperstein G, Lanphear B. Household interventions for prevention of domestic lead exposure in children. Cochrane Database Syst Rev. 2008;(2):CD006047. [CrossRef]
- Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Household interventions for secondary prevention of domestic lead exposure in children. Cochrane Database Syst Rev. 2020;10(10):CD006047. [CrossRef]
- US EPA O. Lead Laws and Regulations. February 12, 2013. Accessed April 19, 2025. https://www.epa.gov/lead/lead-laws-and-regulations.
- Ministère de la santé et des solidarités. L’intoxication par le plomb de l’enfant et la femme enceinte : guide pratique. Published online 2006. https://sante.gouv.fr/IMG/pdf/guide_depistage_saturnisme-3.pdf.
- Décret n°2002-120 du 30 janvier 2002 relatif aux caractéristiques du logement décent pris pour l’application de l’article 187 de la loi n° 2000-1208 du 13 décembre 2000 relative à la solidarité et au renouvellement urbains. - Légifrance. Accessed May 15, 2025. https://www.legifrance.gouv.fr/loda/id/JORFTEXT000000217471/.
- The Challenge of Slums - Global Report on Human Settlements 2003 | UN-Habitat. Accessed June 13, 2025. https://unhabitat.org/the-challenge-of-slums-global-report-on-human-settlements-2003.
- HCSP. Mise à jour du guide pratique de dépistage et de prise en charge des expositions au plomb chez l’enfant mineur et la femme enceinte. Haut Conseil de la Santé Publique; 2017. Accessed May 15, 2025. https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=643.
- Les conseillers (CMEI/CHS). APPA. Accessed May 18, 2025. https://www.appa.asso.fr/habitat-sante/les-conseillers/.
- Jordan CM, Yust BL, Robison LL, Hannan P, Deinard AS. A randomized trial of education to prevent lead burden in children at high risk for lead exposure: efficacy as measured by blood lead monitoring. Environ Health Perspect. 2003;111(16):1947-1951. [CrossRef]
- Shen X ming, Yan C huai, Wu S hu, Shi R. [Parental education to reduce blood lead levels in children with mild and moderate lead poisoning: a randomized controlled study]. Zhonghua Er Ke Za Zhi Chin J Pediatr. 2004;42(12):892-897..
- Alcock G, Das S, Shah More N, et al. Examining inequalities in uptake of maternal health care and choice of provider in underserved urban areas of Mumbai, India: a mixed methods study. BMC Pregnancy Childbirth. 2015;15:231. [CrossRef]
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. [CrossRef]
- Dixon SL, Jacobs DE, Wilson JW, Akoto JY, Nevin R, Scott Clark C. Window replacement and residential lead paint hazard control 12 years later. Environ Res. 2012;113:14-20. [CrossRef]
- Sarigiannis DA, Hansen U. Considering the cumulative risk of mixtures of chemicals - a challenge for policy makers. Environ Health Glob Access Sci Source. 2012;11 Suppl 1(Suppl 1):S18. [CrossRef]
- Braun JM, Hornung R, Chen A, et al. Effect of Residential Lead-Hazard Interventions on Childhood Blood Lead Concentrations and Neurobehavioral Outcomes: A Randomized Clinical Trial. JAMA Pediatr. 2018;172(10):934-942. [CrossRef]
- Campbell C, Tran M, Gracely E, et al. Primary prevention of lead exposure: the Philadelphia lead safe homes study. Public Health Rep Wash DC 1974. 2011;126 Suppl 1(Suppl 1):76-88. [CrossRef]
- Hilts SR, Hertzman C, Marion SA. A controlled trial of the effect of HEPA vacuuming on childhood lead exposure. Can J Public Health Rev Can Sante Publique. 1995;86(5):345-350..
- Rhoads GG, Ettinger AS, Weisel CP, et al. The effect of dust lead control on blood lead in toddlers: a randomized trial. Pediatrics. 1999;103(3):551-555. [CrossRef]
- Krezanoski PJ, Comfort AB, Hamer DH. Effect of incentives on insecticide-treated bed net use in sub-Saharan Africa: a cluster randomized trial in Madagascar. Malar J. 2010;9:186. [CrossRef]
- Lanphear BP, Howard C, Eberly S, et al. Primary prevention of childhood lead exposure: A randomized trial of dust control. Pediatrics. 1999;103(4 Pt 1):772-777. [CrossRef]
- Farrell KP, Brophy MC, Chisolm JJ, Rohde CA, Strauss WJ. Soil lead abatement and children’s blood lead levels in an urban setting. Am J Public Health. 1998;88(12):1837-1839. [CrossRef]
- Miller FG, Brody H. Clinical equipoise and the incoherence of research ethics. J Med Philos. 2007;32(2):151-165. [CrossRef]
- Article L1334-1 - Code de la santé publique - Légifrance. Accessed March 25, 2025. https://www.legifrance.gouv.fr/codes/article_lc/LEGIARTI000031928008.
- Mal-logement en France : la bombe sociale a explosé | Fondation pour le Logement. Accessed May 14, 2025. http://www.fondationpourlelogement.fr/nos-publications/communiques-de-presse/mal-logement-en-france-la-bombe-sociale-explose.
- Section 1 : Conditions d’attribution des logements et plafonds de ressources. (Articles L441 à L441-2-9) - Légifrance. Accessed May 14, 2025. https://www.legifrance.gouv.fr/codes/id/LEGISCTA000006176320/.
- Chapitre V : Autorisation préalable de mise en location (Articles L635-1 à L635-11) - Légifrance. Accessed June 11, 2025. https://www.legifrance.gouv.fr/codes/section_lc/LEGITEXT000006074096/LEGISCTA000028781374/.
- Ajay SV, Kirankumar PS, Sanath K, Prathish KP, Haridas A. An experimental simulation study of conventional waste burning practices in India for the assessment and inventorisation of PCDD/F/dl-PCB emissions. J Environ Manage. 2022;303:114109. [CrossRef]
- Akortia E, Olukunle OI, Daso AP, Okonkwo JO. Soil concentrations of polybrominated diphenyl ethers and trace metals from an electronic waste dump site in the Greater Accra Region, Ghana: Implications for human exposure. Ecotoxicol Environ Saf. 2017;137:247-255. [CrossRef]
- Wang JZ, Mott S, Magwood O, et al. The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: a systematic review. BMC Public Health. 2019;19(1):1528. [CrossRef]
- Boreland F, Lesjak M, Lyle D. Evaluation of home lead remediation in an Australian mining community. Sci Total Environ. 2009;408(2):202-208. [CrossRef]
- Seth R, Girotra TG, Mohammad I, Qaiyum Y, Taneja I, Raman S. Mobile health van as an intervention to provide clinical support and health promotion to street children and marginalised populations in the National Capital Region of Delhi: a mixed-methods evaluation. BMJ Paediatr Open. 2025;9(1):e002988. [CrossRef]
- Stormacq C, Van den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot Int. 2019;34(5):e1-e17. [CrossRef]
- Reviving health mediation during the COVID-19 crisis and beyond: an implementation study in deprived neighbourhoods of Marseille, France - PubMed. Accessed May 9, 2025. https://pubmed.ncbi.nlm.nih.gov/39022414/.
- Laporte R, Babe P, Jouve E, et al. Developing and Validating an Individual-Level Deprivation Index for Children’s Health in France. Int J Environ Res Public Health. 2022;19(24):16949. [CrossRef]
- SPF. Un programme national de médiation en santé auprès et avec les gens du Voyage et les habitants de bidonvilles et squats. Accessed May 15, 2025. https://www.santepubliquefrance.fr/import/un-programme-national-de-mediation-en-sante-aupres-et-avec-les-gens-du-voyage-et-les-habitants-de-bidonvilles-et-squats.
- Hill AB. THE ENVIRONMENT AND DISEASE: ASSOCIATION OR CAUSATION? Proc R Soc Med. 1965;58(5):295-300. [CrossRef]
- Cantor AG, Hendrickson R, Blazina I, Griffin J, Grusing S, McDonagh MS. Screening for Elevated Blood Lead Levels in Childhood and Pregnancy: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2019;321(15):1510-1526. [CrossRef]
- Jacobs DE. Lead screening update from the US Preventive Services Task Force. J Pediatr. 2019;212:243. [CrossRef]
- Schünemann H, Hill S, Guyatt G, Akl EA, Ahmed F. The GRADE approach and Bradford Hill’s criteria for causation. J Epidemiol Community Health. 2011;65(5):392-395. [CrossRef]
- Hall W. Austin Bradford Hill’s “Environment and disease: Association or causation.” Addict Abingdon Engl. 2024;119(2):386-390. [CrossRef]
- Loke YK, Mattishent K. Propensity score methods in real-world epidemiology: A practical guide for first-time users. Diabetes Obes Metab. 2020;22 Suppl 3:13-20. [CrossRef]
- LOI N° 2012-300 Du 5 Mars 2012 Relative Aux Recherches Impliquant La Personne Humaine (1).; 2012.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual authors and contributors and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
| Legal housing | Slum | P | ||
| N (%) | 85 (56.3) | 66 (43.7) | ||
| Boys | 52 (61.2) | 41 (62.1) | 0.13 | |
| Age at diagnosis (years)* | 4.9 (1.7) | 5.9 (2.0) | 0.14 | |
| Sources of lead exposure | ||||
| Decayed paints | 63 (74.1) | 7 (10,6) | <0.0005 | |
| Smoke and dusts (burning, recycling) | 21 (24.7) | 63 (95.5) | <0.0005 | |
| Polluted water (leaded pipes) | 2 (3.0) | 0 (0.0) | 0.51 | |
| Risk co-factors | ||||
| Pica-geophagy behavior | 10 (11.8) | 0 (0,0) | 0.005 | |
| Surrounding cases | 77 (90.6) | 63 (95.5) | 0.35 | |
| Asssociated housing substandard criteria | 44 (51.8) | 57 (86.4) | <0.0005 | |
| Parental at-risk occupation | 15 (17.6) | 54 (81.8) | <0.0005 | |
| Blood lead level at diagnosis (μg/l)* | 110.7 (34.5) | 138.4 (32.2) | 0.01 | |
| * mean (standard deviation) | ||||
| Housing type | Legal | Slum | |||
| Coefficient (Standard error) | p | Coefficient (Standard error) | p | ||
| Intercept | 71.4 (12.9) | < 0.0001 | 105.8 (11.4) | < 0.0001 | |
| Inclusion age < 7 years | 19.2 (12.0) | 0.11 | 47.7 (13.7) | 0.001 | |
| Associated housing substandard criteria |
36.6 (11.3) | < 0.005 | - | ||
| Time (months) | 4.3 (1.54) | < 0.01 | 1.0 (0.94) | 0.29 | |
| Interaction time * intervention, after : | |||||
| Home-based educational intervention | -5.4 (1.52) | < 0.001 | -2.1 (0.82) | 0.01 | |
| Housing remediation | -6.0 (1.57) | < 0.001 | - | ||
| Housing relocation | -5.7 (1.56) | < 0.001 | -4.5 (1.0) | < 0.0001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





