Introduction
Millions of people throughout the world are still coping with the long-term repercussions of SARS-CoV-2 infection more than five years after the start of the COVID-19 pandemic. With thousands of scholarly articles and at least 170 systematic reviews addressing terms like "long COVID," "post-acute sequelae of COVID-19" (PASC), "chronic COVID-19," or "post-COVID-19 condition," there is a substantial amount of research on this topic. Research needs to evaluate all Long COVID alternative therapies to verify their safety navigation as well as their efficacy and suitability within evidence-based healthcare systems. Several patients with variable and complicated Long COVID symptoms adopt complementary treatments which may include herbal medicine and acupuncture alongside mind-body practices. The absence of standardized clinical trials coupled with the lack of proper scientific validation risks patient safety regarding the effectiveness of such treatments. A formal examination process helps determine successful treatments while directing medical protocols and mitigates wrong medical information that patients receive.
The current investigation serves to explore existing research regarding alternative treatments of Long COVID symptoms while emphasizing knowledge gaps and therapeutic insights. Alternative medical practices have received increased interest as supplementary healthcare pathways to standard medical approaches when treating long COVID symptoms. Studies have investigated alternative methods such as herbal medicine and acupuncture along with homeopathy practices along with mindfulness and Ayurveda for treating fatigue along with respiratory symptoms and neurological symptoms that occur because of post-COVID syndrome. Integrative medicine together with functional approaches offer patients holistic care methods which utilize nutrition alongside supplementation and traditional healing practices. However, many healthcare providers are still unclear about how to assess and treat patients with long COVID. With no clear agreement on efficient treatment protocols or standardized care guidelines for individuals afflicted by this crippling condition, the medical community finds it difficult to manage the complex symptoms and long-term effects that follow initial infection. This persistent challenge underscores the complexity of post-COVID-19 conditions [
1,
2]
Health professionals shall evaluate alternative treatment methods for Long COVID since both its prevalence continues to rise and established therapeutic approaches yield limited results. The long-lasting effects of COVID-19 infections that produce ongoing symptoms trigger various patients to seek treatment from complementary and alternative medicine (CAM) practices. The narrative review shows that CAM therapies incorporate acupuncture alongside dietary supplements and neuro-meditation techniques which demonstrate effectiveness against Long COVID fatigue symptoms and cognitive problems and neuropsychiatric disorders.
Multiple studies have provided positive initial findings but an extensive analysis of the subject remains sparse. Most current studies face important limitations because they do not perform robust randomized controlled trials that would validate both effectiveness and safety performance. Systematic evaluation of these treatments becomes essential because it enables healthcare professionals to confirm their effectiveness and security standards. Such evidence-based recommendations will help health professionals alongside enabling patients to make better treatment choices through informed decisions. The increases in alternative therapy demand require extensive research which should fill knowledge gaps to optimize health care delivery for Long COVID patients.
Due to significant variations in sampling frames, inclusion criteria, participant demographics, diagnostic processes, and study design, epidemiological studies on extended COVID are challenging to analyse and synthesize. These studies often produce results that are skewed by certain factors since they mirror the traits of the populations they are intended for. The experience of individuals who were initially more unwell is overrepresented in follow-up research on patients who are discharged from hospitals, for instance, because these studies typically concentrate on those with more severe COVID-19 instances. The experiences of younger or female people may also be overlooked in studies on military veterans covered by insurance plans, which tend to focus on older men.
There is bias in other studies since they rely on surveys of persons who have been participated in online COVID support groups for a long time. In general, these individuals were more aggressive and knowledgeable when seeking help, suggesting that their symptoms were serious enough to necessitate peer support. The results of these surveys might therefore not accurately represent the broader population of long-term COVID-19 patients, especially those with less severe symptoms or those who do not frequent these online discussion boards. Moreover, research using electronic health data, both retrospective and prospective, typically concentrate on individuals who were officially diagnosed with COVID-19 or extended COVID, excluding those who experienced symptoms but were not officially diagnosed.
These studies can provide insight into the severe outcomes of COVID-19 and its long-term effects, but they do not represent the experiences of the great majority of long-term COVID patients who survive but nevertheless have symptoms. Comparably, case series from specialty clinics are often biased toward patients who were sent for specialized care, indicating that their symptoms were severe or complicated enough to call for such care. Those with milder or less well-known symptoms may not seek or need specialist care, therefore this group may not be typical of the broader population.
Another well-known approach is community-based surveys, which mostly depend on peoples answering questionnaires. But because those who have been negatively affected by long-term COVID are more likely to respond to surveys, this method adds bias. People with less severe symptoms or those who have recovered might be less likely to take part, which would cause the results to overrepresent more major cases.
There are additional challenges when researching prolonged COVID in primary care populations that are not chosen. After an initial infection, many people may experience persistent symptoms and never see their primary care physician. They are rarely officially identified or documented as having prolonged COVID, even if they have, which makes monitoring and research more difficult. Additionally, this lack of identification limits the ability to study long-term COVID, especially in regions of the world where the disease is either unidentified or not well understood. Additionally, there is a notable lack of research on extended COVID in low- and middle-income countries, where the healthcare system may not be sufficient for managing or diagnosing the diseases, let alone monitoring its prevalence and effects. Because of this, we still don't fully understand long-term COVID, especially in these countries, and more research is needed to provide us a better global picture of the disease [
1,
3,
4,
5,
6,
7,
8,
9,
10]. Examining the body of research on alternative therapies for Long COVID and assessing the effectiveness and safety of complementary and alternative medicine (CAM) interventions in reducing common symptoms are the objectives of this narrative review.
The practices of Complementary and Alternative Medicine (CAM) encompass different medical approaches beyond traditional healthcare that include herbal medicine alongside acupuncture and yoga and homeopathy. Alternative medicine systems now attract medical interest for their management of Long COVID by utilizing holistic treatment since patients experience less adverse effects than traditional medicine. People use CAM treatment methods because their standard medical care has failed either in helping their condition or doesn't address continuing symptoms affecting fatigue level, memory problems and pain experiences. Scientific research needs to assess both the safety and effectiveness of complementary and alternative medicine (CAM) for Long COVID symptoms since the condition lacks full medical understanding because CAM provides potential symptom management solutions.
Alternative Therapies for Long COVID Treatment
Phytotherapy
The use of alternative therapies, notably phytotherapy, has received increased attention in the treatment of Long COVID, a disorder that affects a large number of people after recovering from COVID 19. It is estimated that 10% to 20% of people who recover from COVID-19 have persistent symptoms, which are now known as Long COVID. These chronic symptoms, which can affect several organ systems, frequently necessitate continuing and successful treatment measures. Given the complexity of the ailment and the difficulties created by the lack of clear therapies, many people are turning to complementary and alternative techniques.
Phytotherapy, or the use of herbal medicines, has emerged as a viable treatment for the various symptoms linked with Long COVID. According to research, herbal therapies have the potential to be used as part of clinical management for people suffering from these long-term symptoms. Certain herbal treatments have been found to be very effective for specific Long COVID symptoms. For example, Uncaria tomentosa is recommended for cough treatment, while Ginkgo biloba may help with cardiovascular difficulties. Mangifera indica Linnaeus has the ability to relieve neuromuscular symptoms, whereas Valeriana officinalis may be effective in treating central nervous system-related problems.
Furthermore, there is a rising movement to incorporate herbal medicine into basic healthcare systems, such as Brazil's Unified Health System (SUS). Standardizing the use of phytotherapy alongside traditional allopathic medications may provide a more comprehensive approach to Long COVID management. By introducing herbal treatments into Primary Health Care settings, healthcare providers may be able to deliver more comprehensive treatment programs that address the vast spectrum of symptoms reported by Long COVID patients, assisting them in their recovery process [
11].
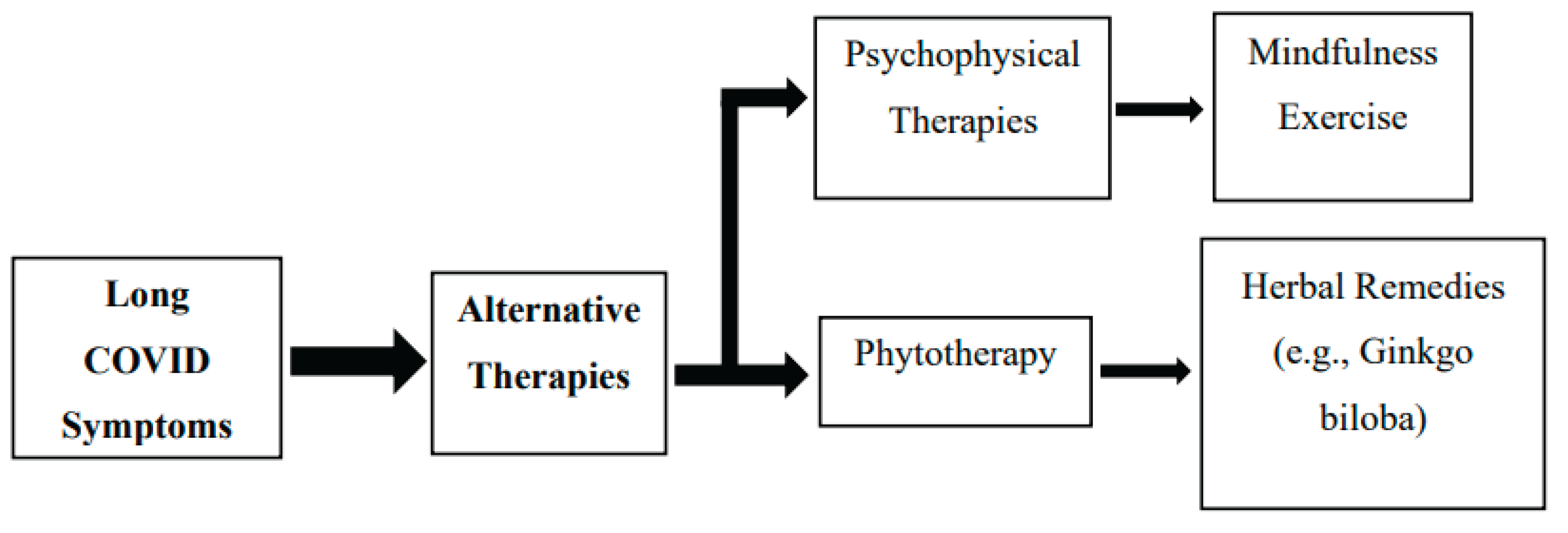
Figure 1.
Overview of Alternative Therapies for Long COVID. The existing literature regarding the use of alternative therapies for Long COVID.
Figure 1.
Overview of Alternative Therapies for Long COVID. The existing literature regarding the use of alternative therapies for Long COVID.
Psychophysical Therapies
Several psychophysical therapies have been recommended as viable treatment options for managing Long COVID symptoms, offering patients a multifaceted approach to improve both physical and mental well-being. These therapies, which integrate physical and psychological components, aim to address the multisystemic nature of Long COVID and have demonstrated potential in alleviating some of its persistent symptoms.
One widely recognized psychophysical intervention is exercise therapy, which has long been acknowledged for its benefits in enhancing overall health. Regular physical activity can improve cardiovascular function, muscle strength, and mood-factors that may contribute to reducing symptoms such as fatigue, muscle weakness, and cognitive dysfunction commonly observed in Long COVID patients. However, exercise must be prescribed with caution, particularly for individuals experiencing post-exertional malaise (PEM), a symptom frequently associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), which often overlaps with Long COVID.
Mindfulness practices, including meditation and breathing techniques, are also gaining recognition for their role in managing the psychological burden of Long COVID. These practices help reduce stress, promote relaxation, and support mental well-being, which is particularly important given the anxiety, depression, and cognitive difficulties experienced by many patients enduring the long-term effects of the illness.
In addition, oxygen therapy has been suggested as a beneficial treatment, especially for individuals suffering from respiratory issues such as shortness of breath. By improving oxygen delivery to tissues, this therapy may facilitate recovery in patients experiencing ongoing pulmonary symptoms and fatigue, thereby enhancing cellular function and overall vitality.
Emerging evidence also points to the role of certain immunomodulatory therapies in restoring immune system balance, which is often disrupted in Long COVID. These treatments aim to reduce chronic inflammation and support immune regulation. Notably, photobiomodulation (PBM), also known as low-level laser therapy (LLLT), has shown promise as a non-invasive method to stimulate healing and reduce inflammation. PBM utilizes specific wavelengths of light to enhance tissue repair, decrease oxidative stress, and modulate inflammatory responses, offering a potentially effective strategy in managing chronic post-viral conditions.
Furthermore, psychophysical therapies may contribute to neuroendocrine regulation, helping to restore balance in hormonal pathways altered by the virus. For instance, oxytocin, a hormone involved in social bonding and stress regulation, has been implicated in the healing process, suggesting that therapies influencing neuroendocrine functions could support recovery from Long COVID.
Overall, psychophysical therapies encompass a range of integrative approaches that may complement conventional treatments for Long COVID, targeting both the physical and psychological dimensions of the disease. While promising, further research is essential to determine their efficacy, safety, and optimal use in clinical practice [
12]. Notably, recent studies have shown that acupoint stimulation therapy may help relieve symptoms such as palpitations, dyspnea, cognitive impairment, anxiety, and depression, highlighting the need to explore and validate such alternative therapies in the context of Long COVID recovery [
13].
Efficacy and Safety of Alternative Therapies (CAM Interventions) for Long COVID
Recent research has highlighted numerous CAM therapies that may help improve common long-term COVID symptoms. Transcutaneous auricular vagus nerve stimulation has shown promise in alleviating mental fatigue and other neuropsychiatric issues. Neuro-meditation focuses on enhancing cognitive function and promoting mental well-being. Dietary supplements have been investigated for their potential benefits in addressing fatigue and cognitive deficits. Olfactory training has proven particularly effective for individuals experiencing olfactory impairment. Aromatherapy is used to enhance overall well-being and reduce anxiety. Inspiratory muscle training is aimed at improving respiratory function, while online breathing programs are designed to foster relaxation and support respiratory wellness.
Methodology
The secondary approaches for the narrative evaluation of alternate treatments for chronic COVID is to gather information from a range of reliable and varied sources. To guarantee a thorough understanding of the literature that is currently accessible, we have gathered information from both peer and non-peer review sources. We have conducted comprehensive searches for peer-reviewed articles, research articles and grey literature on alternative COVID therapy in academic databases and search engines including PubMed, Google Scholar, ResearchGate, and Academia. Accessing recent studies, ongoing inquiries, and professional viewpoints is made easier by these portals. Official government websites and public health portals have been included since they often offer policy documents, guidelines, and information on alternate therapies for post-COVID sickness.
Search Strategy
In order to identify pertinent literature regarding alternative therapies for Long COVID, a thorough search methodology has been implemented. The search was restricted to peer-reviewed publications, research papers, grey literature, and expert opinions that were accessible through reputable academic databases and libraries. Key sources include government websites, public health portals, Academia, ResearchGate, PubMed, and Google Scholar. The search criteria were a combination of keywords, including "Long COVID," "Post-Acute Sequelae of COVID-19," "alternative therapies," "complementary and alternative medicine," "phytotherapy," and "psychophysical therapies."
The inclusion criteria for this narrative review are as follows: the research papers must be published in English and focus on alternative therapies for long-term COVID symptoms. Only systematic evaluations and peer-reviewed publications are included. In addition to CAM interventions such as phytotherapy, the review emphasizes psychophysical therapies, such as mindfulness and exercise. Articles must have been published between 2020, the inception of the COVID-19 pandemic, and 2024 in order to qualify. Additionally, reports from the government and public health that are relevant to alternative therapies are considered for inclusion.
Conversely, the exclusion criteria encompass the following: Articles published prior to the onset of the COVID-19 pandemic (pre-2020), studies that do not directly address Long COVID, articles that exclusively focus on traditional Western medicine without incorporating CAM interventions, and non-peer-reviewed literature (unless sourced from credible government or health portals).
Inclusion Criteria
Studies published in English.
Research papers discussing alternative therapies for Long COVID symptoms.
Peer-reviewed articles and systematic reviews.
Studies focusing on CAM interventions such as phytotherapy and psychophysical therapies (e.g., mindfulness, exercise).
Papers published from the onset of the COVID-19 pandemic onwards (2020-2024).
Government and public health reports relevant to alternative therapies.
Exclusion Criteria
Studies not directly addressing Long COVID.
Papers focusing solely on traditional Western medicine without including CAM interventions.
Articles published before the COVID-19 pandemic (pre-2020).
Non-peer-reviewed literature, unless from reliable governmental or health portals.
Results
Efficacy of CAM Therapies
The comprehensive review comprised 14 RCTs with a total of 1,195 participants that examined the efficacy of CAM therapies for treating Long COVID symptoms. The major findings from this narrative research imply that CAM therapies can be useful in treating a variety of symptoms common to Long COVID patients.
One major area of improvement seen was in neuropsychiatric diseases, where patients displayed improved mood and cognitive performance after receiving CAM therapies. Given the predominance of symptoms such as brain fog, anxiety, and sadness in Long COVID, our findings underscore the possibility of CAM therapies to help patients overcome mental health issues. Another noteworthy result was a decrease in fatigue, which is one of the most debilitating and chronic symptoms of Long COVID. Participants in numerous researches reported significant reductions in fatigue levels, implying that CAM therapies may be a useful tool for boosting energy levels and overall well-being.
Furthermore, several CAM therapies have been proven to improve dyspnea and lung function, particularly in people with mild-to-moderate lung fibrosis, which can develop following a COVID-19 infection. Improvements in respiratory symptoms were observed, which is especially encouraging for people who have experienced chronic shortness of breath or reduced lung capacity following COVID. These findings imply that CAM techniques may offer a complementary alternative for addressing persistent pulmonary problems.
Safety of CAM Therapies
The review indicated that CAM therapies had a generally good safety profile. Most studies found only mild to moderate side effects, indicating that CAM treatments are relatively safe for Long COVID patients. For example, one study found that self-administered vagus nerve stimulation, a technique for stimulating the vagus nerve to reduce inflammation and regulate numerous biological systems, was associated with only slight skin irritations at the application site. Despite these encouraging safety findings, it is crucial to emphasize that several of the included studies had methodological constraints, such as small sample numbers or a lack of rigorous control measures, necessitating cautious interpretation of the results. Furthermore, high-quality research is required to validate the efficacy and safety of CAM therapies in this setting.
Overall, the analysis suggests that CAM therapies may have promise effects for controlling a wide range of Long COVID symptoms, but additional research is needed to conclusively establish their position within treatment regimens. The potential of these interventions, together with their excellent safety profiles, offers hope for incorporating CAM therapies into comprehensive care plans for Long COVID patients [
14,
15].
Discussion
The rising body of literature on alternative therapies for Long COVID emphasizes the growing awareness of phytotherapy and psychophysical interventions as important components in managing this complex disorder. With an estimated 10-20% of COVID-19 survivors suffering persistent symptoms, often known as Long COVID, the hunt for effective treatments has led many people to investigate CAM.
Phytotherapy, in particular, has shown promise as a feasible treatment for a variety of symptoms linked with Long COVID. Herbal supplement treatments, such as Uncaria tomentosa for cough and Ginkgo biloba for cardiovascular disorders, have specific efficacy, whilst Mangifera indica and Valeriana officinalis address neuromuscular and central nervous system symptoms, respectively. This increased interest is also evident in the incorporation of herbal medications into established healthcare systems, such as Brazil's Unified Health System, which may allow for a more holistic therapeutic approach.
In addition to phytotherapy, psychophysical therapies are an important option for controlling Long COVID symptoms. These therapies, which combine physical and psychological components, have the potential to benefit both physical and mental health. Exercise, for example, has been shown to improve cardiovascular function and mood, although individuals experiencing post-exertional malaise should be cautious.
Other promising approaches include oxygen therapy for respiratory issues and photo biomodulation, which uses certain wavelengths of light to promote healing and reduce inflammation. Furthermore, mindfulness and meditation techniques are gaining popularity because to their efficacy in treating anxiety and cognitive deficits, emphasizing the multidimensional character of Long COVID and the necessity for treatments that address its various symptoms.
Emerging data supporting several CAM therapies, such as transcutaneous auricular vagus nerve stimulation and neuro-meditation, highlights their potential benefits in treating neuropsychiatric symptoms, exhaustion, and respiratory difficulties. A comprehensive evaluation of 14 randomized controlled studies found significant improvements in mood, cognitive function, and fatigue levels among patients who used CAM therapies, indicating that they could be a helpful addition to traditional therapy approaches. Notably, the safety profile of these therapies is generally positive, with most studies showing only minor to moderate adverse effects. However, methodological limitations in some studies need care when interpreting results and highlight the need for further thorough research to establish efficacy and safety.
Conclusion
The investigation of alternative therapies, particularly phytotherapy and psychophysical interventions, offers a promising avenue for addressing the intricate and multidimensional symptoms of Long COVID. Given that a substantial number of individuals who are recovering from COVID-19 are still experiencing persistent symptoms, the incorporation of herbal medicines-including Ginkgo biloba and Uncaria tomentosa as herbal supplements-into clinical management could offer targeted alleviation for a variety of signs and symptoms of the condition. In addition, psychophysical therapies, which include mindfulness practices, oxygen therapy, and physical exercise, provide a comprehensive approach to enhancing both mental and physical health.
The potential efficacy of CAM therapies is evident in the growing body of research, which suggests that they can significantly enhance respiratory health and neuropsychiatric conditions, in addition to having a favourable safety profile. Nevertheless, the constraints of current research necessitate additional rigorous research to substantiate these discoveries and establish standardized protocols for the implementation of these therapies in clinical environments. In conclusion, the integration of alternative therapies into comprehensive care programs has the potential to improve the recovery of Long COVID patients by addressing both their physical ailments and psychological challenges.
Funding
The work is supported by Indian Council of Medical Research (ICMR), New Delhi under Task Force Research Scheme (54/4/GER/Indo-Sweden/2022-NCD-II).
Conflict of Interest
None.
References
- Frallonardo L, Segala FV, Chhaganlal KD, Yelshazly M, Novara R, Cotugno S, et al. Incidence and burden of long COVID in Africa: a systematic review and meta-analysis. Sci Rep. 2023 Dec 6;13(1):21482. Available from: https://www.nature.com/articles/s41598-023-48258-3.
- Kostka K, Roel E, Trinh NTH, Mercadé-Besora N, Delmestri A, Mateu L, et al. The burden of post-acute COVID-19 symptoms in a multinational network cohort analysis. Nat Commun. 2023 Nov 17;14(1):7449. Available from: https://www.nature.com/articles/s41467-023-42726-0.
- Ledford, H. How common is long COVID? Why studies give different answers. Nature. 2022 Jun;606(7916):852-853. [CrossRef]
- Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. 2022; 10(9):863-876. [CrossRef]
- Evans RA, Leavy OC, Richardson M, Elneima O, McAuley HJC, Shikotra A, et al. PHOSP-COVID Collaborative Group. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir Med. 2022 Aug;10(8):761-775. [CrossRef]
- Bowe B, Xie Y, Al-Aly Z. Postacute sequelae of COVID-19 at 2 years. Nat Med. 2023 Sep 21;29(9):2347–2357. Available from: https://www.nature.com/articles/s41591-023-02521-2.
- Cohen K, Ren S, Heath K, Dasmariñas MC, Jubilo KG, Guo Y, et al. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2022 Feb 9;e068414. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj-2021-068414.
- Oaklander AL, Mills AJ, Kelley M, Toran LS, Smith B, Dalakas MC, et al. Peripheral Neuropathy Evaluations of Patients with Prolonged Long COVID. Neurol Neuroimmunol Neuroinflammation. 2022 May;9(3). Available from: https://www.neurology.org/doi/10.1212/NXI.0000000000001146.
- Mateu L, Tebe C, Loste C, Santos JR, Lladós G, López C, et al. Determinants of the onset and prognosis of the post-COVID-19 condition: a 2-year prospective observational cohort study. Lancet Reg Health Eur. 2023 Sep 5;33:100724. [CrossRef]
- Whitaker M, Elliott J, Chadeau-Hyam M, Riley S, Darzi A, Cooke G, et al. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun. 2022 Apr 12;13(1):1957. Available from: https://www.nature.com/articles/s41467-022-29521-z.
- Fabre L da S, Dibo V, Cazarim M de S. Evidências sobre fitoterapia para o tratamento da COVID-longa no âmbito da atenção primária à saúde do SUS. Rev Fitos. 2024 Jul 17;18:e1511. Available from: https://revistafitos.far.fiocruz.br/index.php/revista-fitos/article/view/1511.
- Meng QT, Song WQ, Churilov LP, Zhang FM, Wang YF. Psychophysical therapy and underlying neuroendocrine mechanisms for the rehabilitation of long COVID-19. Front Endocrinol (Lausanne). 2023 Sep 29;14:1120475. [CrossRef]
- Feng BW, Rong PJ. Acupoint stimulation for long COVID: A promising intervention: World J Acupunct Moxibustion. 2023 Jul;33(3):191–197. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1003525723000387.
- Yang J, Lim KH, Lim KT, Woods JT, Mohabbat AB, Wahner-Roedler DL, et al. Complementary and alternative medicine for long COVID: a systematic review of randomized controlled trials. Ther Adv Chronic Dis. 2023 Oct 11;14:20406223231204727. [CrossRef]
- Kim TH, Jeon SR, Kang JW, Kwon S. Complementary and Alternative Medicine for Long COVID: Scoping Review and Bibliometric Analysis. Evid Based Complement Alternat Med. 2022 Aug 4;2022:7303393. Available from: https://www.hindawi.com/journals/ecam/2022/7303393/. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).