1. Introduction
Maternal overweight and obesity significantly increase the risk of complications during pregnancy, labor, and the perinatal period for the child. Additionally, excessive weight gain during pregnancy and the retention of weight postpartum can negatively impact future fertility and subsequent pregnancies [
1]. Baseline (preconception) weight and moderate gestational weight gain are crucial factors for the successful progression of pregnancy. Obesity is linked to a markedly increased risk of developing gestational diabetes, pregnancy-induced hypertension, preeclampsia, venous thromboembolism, and caesarean delivery [
2]. For the fetus, maternal obesity is associated with conditions such as fetal macrosomia and a heightened risk of intrauterine death, as well as an increased incidence of obesity and metabolic syndrome in childhood. These adverse effects are believed to stem from obesity’s detrimental impact on placental function, although the underlying mechanisms remain unclear [
3]. Furthermore, maternal obesity has the potential to perpetuate a cycle of obesity and insulin resistance across generations.
The “Western diet” is associated with a heightened risk of gestational diabetes mellitus and hypertensive disorders. The term “Western diet” refers to a modern dietary pattern that is characterised by a low intake of fruit, vegetables, whole grains, and nuts, and a high intake of red (or processed) meat, processed and refined foods, foods with added sugars, and saturated and trans fats [
5].
Aim: The study aimed to analyse the incidence of obesity and its impact on pregnancy outcome in women delivered by caesarean section from 2021 to 2023 at the “Clinic of Obstetrics and Gynaecology” of the University Hospital “St. George”, Plovdiv.
2. Materials and Methods
A retrospective study was conducted over a three-year period (May 2021 - May 2023) at the “Clinic of Obstetrics and Gynaecology” of the University Hospital “St. George” - Plovdiv. A documentary method was employed to gather data from hospital records, specifically the “Pregnancy and Birth History” sheets of women discharged from the clinic following caesarean section (CS) deliveries. Women were selected randomly. The inclusion criteria were as follows: (1) the patient underwent delivery via CS; (2) complete data from the woman’s medical history at admission and relevant anthropometric measurements were available. The key information collected included: age, parity, height and weight, BMI, abdominal circumference, concomitant diseases, presence of arterial hypertension (AH) or gestational diabetes mellitus (GDM), indications for CS, complications of pregnancy and childbirth. The normality of the distribution of variables was tested using the Kolmogorov–Smirnov test. Data comparisons were performed using the Mann–Whitney test. Mean values of numerical variables were compared using the Independent Samples T-Test. Statistically significant differences were accepted when the P-value was lower than 0.05. Statistical analysis was performed using SPSS version 23.0 software (SPSS Inc., Chicago, IL, USA).
3. Results
Based on the established inclusion criteria, 494 cases of women following a caesarean section (CS) were included in the study sample. The average age of the participants was approximately 29.33 years, with the youngest patient being 14 years old and the oldest at 48 years. Among the women, 91.30% (451) were in their 10th lunar month of pregnancy, while 6.28% (31) were in the ninth lunar month, 1.62% in the eighth month, and 0.81% in the seventh month. The key characteristics of the sample are summarised in
Table 1.
Pregnancy occurred against the backdrop of diabetes (either gestational diabetes mellitus or previous diabetes) in 4.25% (n=21) of the women included in the study.
The analysis of pregnancy outcomes revealed that 51.82% of the women received emergency CS, while 48.18% underwent planned procedures. The primary reason for performing a CS was a previous caesarean, accounting for 37.45% of the cases. Other indications for surgical intervention included moderate preeclampsia in 9.31% (46 women), severe preeclampsia in 2.32% (11 women), abruptio placentae in 1.21% (6 women), a large fetus in 6.07% (30 cases), intrauterine growth restriction (IUGR) in 1.82% (9 cases), polyhydramnios in 1.21% (6 women), blood pressure values unresponsive to therapy in 0.81% (4 women), and obesity in one woman (0.20%). GDM was noted as an indication in 2.43% (12 women), and diabetic fetopathy – in 0.4% (2 women).
It is notable that only one woman was classified as having “obesity” among the reasons for surgical intervention. However, the overall data indicates that the total number of patients with varying degrees of obesity (I, II, or III) is 229, yet only one of these patients had obesity cited as a reason for the surgical procedure.
The analyses indicate that the data concerning the women’s age, weight at admission, and systolic and diastolic arterial pressure do not follow a normal distribution, whereas the weights of the newborns are normally distributed.
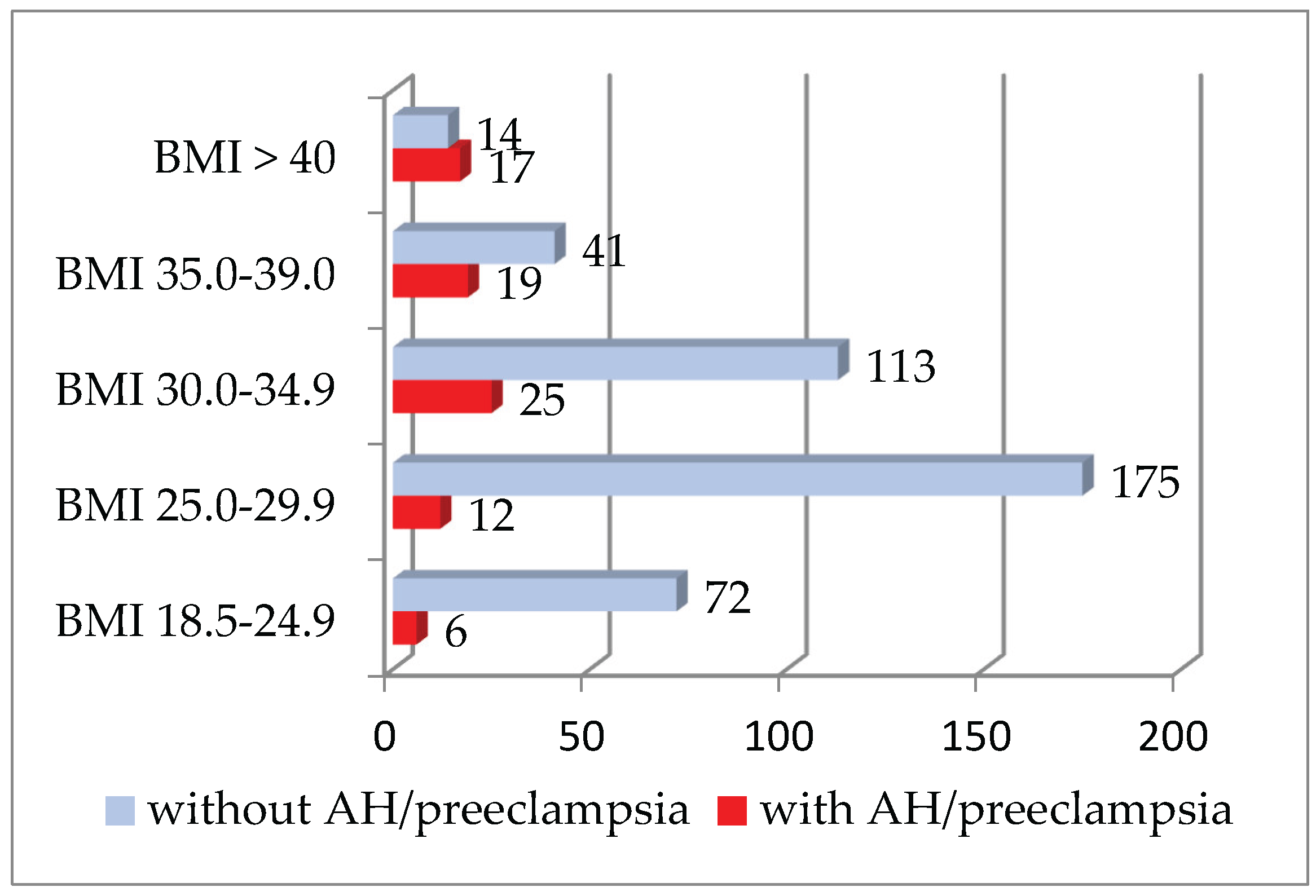
The results indicate that a total of 79 women experienced hypertensive disorders, both pre- and post-pregnancy. Out of these, 64 received treatment, while 15 did not. The conditions identified included preeclampsia (both moderate and severe), pre-existing hypertension (pre-AH), and hypertension with superimposed preeclampsia. Among the patients diagnosed with hypertension, the average weight upon admission was 95.16 ± 21.11 kg, whereas in the uncomplicated group, the mean weight was lower – 78.91 ± 14.71 kg. A statistically significant difference in body weight between the two groups was observed (p<0.001). Additionally, as anticipated, there was a considerable difference in both systolic and diastolic blood pressure measurements between the two groups (p<0.001), although the majority of those affected (64 or 81.01%) were treated, leading to the recorded values being influenced by antihypertensive therapy. This study reveals a distinct trend indicating an increased incidence of hypertension and preeclampsia among obese women. In the cohort with a BMI over 30.0, 26.64% were affected, compared to only 6.79% in the group with a BMI below 30.0.
Figure 1 illustrates the distribution of women affected by hypertensive disorders based on BMI. The number of patients with AH or preeclampsia is shown alongside the unaffected patients. The trend of increasing proportions of hypertension and preeclampsia cases is clear across the three classes of obesity.
Divided into two groups – those with obesity (in all degrees) and those without – we found that the mean systolic pressure values were 122.49±17.705 mmHg and 114.18±13.320 mmHg, respectively. In terms of diastolic pressure, the mean values for both groups of women were 76.73±13.144 mmHg and 70.82±9.543 mmHg, respectively. Statistical analysis reveals a significant difference between the obese and non-obese groups for both measurements (p<0.001).
The mean weight for the newborns in grams is 3091.94±553.066. Among the sample, full-term newborns constitute 87.67% (448), while 63 are classified as premature. The distribution of the children according to degrees of prematurity is detailed in
Table 2.
The comparative analysis of neonatal weights derived from singleton pregnancies among women with and without hypertensive disorders revealed a statistically significant disparity in mean values (p=0.001). The average weight of newborns of women affected by hypertensive disorders was recorded at 2940.66 grams, in contrast to 3172.54 grams for those without such disorders. A notable increase in the risk of preterm delivery was observed among women diagnosed with AH or preeclampsia, with an odds ratio of 3.981 (95% CI 2.078-7.625), indicating an almost fourfold increase in probability. The incidence of premature births among this cohort stands at 23.7%, compared to only 7.2% in the group without hypertensive complications (p<0.001), further highlighting the implications of gestational hypertension on neonatal outcomes.
An examination of maternal age as a contributing factor to the prevalence of AH/ preeclampsia revealed an escalating incidence in mothers over 35 years. The prevalence among women aged 34 years and younger is 14.17%, whereas it escalates to 22.92% in those aged over 35, with these differences established as statistically significant (p=0.037). In refining the analysis, twin pregnancies were excluded to ensure the focus remained on singleton births.
There was a statistically significant difference in the gestational week of delivery between the two groups of women (p=0.001). In women who gave birth with AH/ preeclampsia, the average gestational week at delivery was 36.82±2.246, while for those without hypertensive disorders, it was 38.17±1.584 week. These results align with expectations, considering the complications associated with gestational hypertension and preeclampsia, which often necessitate preterm delivery for the health of the mother and fetus.
When evaluating neonatal weight data, no significant differences were noted within the subset of mothers suffering from diabetes/GDM (p=0.702). It is important to note that our sample comprised only 21 women diagnosed with diabetes. However, a statistically significant disparity was observed in Apgar scores at both the 1-minute and 5-minute marks across both maternal groups – with and without diabetes. The tests revealed p-values p=0.020 (1st minute) and p<0.001 (5th minute).
4. Discussion
The prevalence of overweight and obesity among women of reproductive age has risen significantly over the past three decades, leading to an increasing number of pregnancies complicated by these conditions [
1]. Our study revealed a notable proportion of women with high and very high BMI at the time of admission. Weight gain during pregnancy among different groups of obese women exceeds the recommendations found in existing literature. This excessive weight gain, combined with challenges in achieving postpartum weight loss, can complicate future pregnancies for these women [
1].
Globally, there is a noticeable trend in the rise of hypertensive disorders, affecting approximately 8-10% of all pregnancies [
6]. In our study, the incidence is higher; however, this can be attributed to the specific cohort examined, namely women delivered by CS. Literature indicates that obese and overweight women face a significantly increased risk of operative deliveries, whether elective or emergency, compared to the rest of the pregnant population [
1].
The presence of preeclampsia poses risks to newborns, including prematurity, low birth weight, and fetal distress [
7]. Maternal obesity, particularly high-grade obesity, is strongly correlated with the development of preeclampsia [
8]. Our study observed a clear trend indicating an increase in the number of women experiencing AH/ preeclampsia within the group of obese women.
These findings are consistent with the research conducted by Lewandowska et al. [
9], which suggests that hypertension during pregnancy is linked to newborns with low birth weight and lower gestational age.
In our study, we observed that the average weight gain during pregnancy among obese women is significantly elevated. Maternal obesity, GDM, and high sugar and fat intake can lead to fetal overnutrition, resulting in conditions such as fetal macrosomia or small-for-gestational-age infants [
10].
According to Tabacu et al. [
3], the prevalence of obesity among pregnant women in Europe is approximately 15%, while in the United States, it ranges between 18% and 38%. While these statistics are consistent with our findings, the lack of data from the natural birth cohort means we cannot generalise these rates to our population.
We consider the high share of obese women in our study concerning. Grenier et al. [
11] highlight that there are numerous misconceptions and wrong behavioural patterns among pregnant women, a phenomenon that is certainly applicable in our country. Many believe that pregnancy is a period during which a woman can indulge, “gain as much weight as desired,” “do nothing,” and “eat for two.” There is a misguided belief that any physical activity could adversely affect both the mother and the fetus, and families often encourage such attitudes.
Chang et al. [
12] note that many studies associate advanced maternal age (specifically, women over 35 years) with higher incidences of preeclampsia and other complications. Our findings align with this observation regarding hypertensive complications; however, due to the relatively small sample size of older women in our study, we must interpret the results with caution. A larger cohort study is necessary to draw more definitive conclusions for our population. Similarly, Martin-Alonso et al. [
13] suggest a correlation between high BMI and an increased risk of GDM, but the limited number of cases in our study prevented us from making a meaningful comparison.
5. Conclusions
Pregnancy complications associated with maternal obesity and hypertension impact a significant number of women, and there is a noticeable trend towards increasing rates. Among women who have given birth via caesarean section, a substantial proportion is affected by obesity and overweight. This study indicates a clear trend towards a rise in the frequency of preterm births linked to preeclampsia, as well as an increased incidence of hypertensive disorders in women with elevated BMI. Regrettably, preeclampsia remains a largely under-researched issue. Gaining a deeper understanding of its etiological factors could lead to more effective prevention and management strategies, ultimately resulting in better outcomes for both mothers and their newborns.
Author Contributions
Conceptualization, Z.N., M.V. and M.S.; methodology, E.U. and M.S; software, Z.N. and A.K.-B.; validation, D.T., A.K.-B. and L.G.; formal analysis, M.S. and A.K.-B.; investigation, Z.N. and M.V.; resources, E.U., L.G. and M.S.; data curation, Z.N. and A.K.-B.; writing—original draft preparation, Z.N.; writing—review and editing, D.T., A.K.-B. and L.G.; visualization, Z.N. and M.V.; supervision, E.U. and D.T.; project administration, Z.N., M.V. and M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study complies with the ethical guidelines of the institutions involved. Ethical Committee meeting protocol No 1/05 Feb 2025.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study at their admission to the University Hospital. The informed consent covers scientific and educational activities conducted at the hospital.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from University Hospital “St. George” - Plovdiv and are available from the authors with the permission of University Hospital “St. George” - Plovdiv.
Conflicts of Interest
Authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AH |
Arterial hypertension |
| CS |
Caesarеan section |
| BMI |
Body mass index |
| GDM |
Gestational diabetes mellitus |
| IUGR |
Intrauterine growth restriction |
References
- Langley-Evans, S.C.; Pearce, J.; Ellis, S. Overweight, obesity and excessive weight gain in pregnancy as risk factors for adverse pregnancy outcomes: A narrative review. J Hum Nutr Diet. 2022, 35, 250–264. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, C.; Locati, F.; Parisi, F.; Anelli, G.M.; Ossola, M.W.; Cetin, I. Gestational weight gain as a modifiable risk factor in women with extreme pregestational BMI. Nutrients 2025, 17, 736. [Google Scholar] [CrossRef] [PubMed]
- Tabacu, M.C.; Istrate-Ofiţeru, A.M.; Manolea, M.M.; Dijmărescu, A.L.; Rotaru, L.T.; Boldeanu, M.V.; Şerbănescu, M.S.; Tudor, A.; Novac, M.B. Maternal obesity and placental pathology in correlation with adverse pregnancy outcome. Rom J Morphol Embryol. 2022, 63, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Paredes, C.; Hsu, R.C.; Tong, A.; Johnson, J.R. Obesity and pregnancy. Neoreviews 2021, 22, e78–e87. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Redondo-Flórez, L.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Global impacts of western diet and its effects on metabolism and health: A narrative review. Nutrients 15, 2749. [CrossRef] [PubMed]
- Poniedziałek-Czajkowska, E.; Mierzyński, R.; Leszczyńska-Gorzelak, B. Preeclampsia and obesity - the preventive role of exercise. Int J Environ Res Public Health. 2023, 20, 1267. [Google Scholar] [CrossRef] [PubMed]
- Uzunov, A.V.; Secara, D.C.; Mehedințu, C.; Cîrstoiu, M.M. Preeclampsia and neonatal outcomes in adolescent and adult patients. J Med Life 2022, 15, 1488–1492. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.; Romero, R.; Yeo, L.; Gomez-Lopez, N.; Chaemsaithong, P.; Jaovisidha, A.; Gotsch, F.; Erez, O. The etiology of preeclampsia. Am J Obstet Gynecol. 2022, 226, S844–S866. [Google Scholar] [CrossRef] [PubMed]
- Lewandowska, M.; Więckowska, B.; Sajdak, S.; Lubiński, J. Pre-pregnancy obesity vs. other risk factors in probability models of preeclampsia and gestational hypertension. Nutrients 2020, 12, 2681. [Google Scholar] [CrossRef] [PubMed]
- Marshall, N.E.; Abrams, B.; Barbour, L.A.; Catalano, P.; Christian, P.; Friedman, J.E.; Hay, W.W. Jr.; Hernandez, T.L.; Krebs, N.F.; Oken, E.; Purnell, J.Q.; Roberts, J.M.; Soltani, H.; Wallace, J.; Thornburg, K.L. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol. 2022, 226, 607–632. [Google Scholar] [CrossRef] [PubMed]
- Grenier, L.N.; Atkinson, S.A.; Mottola, M.F.; Wahoush, O.; Thabane, L.; Xie, F.; Vickers-Manzin, J.; Moore, C.; Hutton, E.K.; Murray-Davis, B. Be healthy in pregnancy: Exploring factors that impact pregnant women’s nutrition and exercise behaviours. Matern Child Nutr. 2021, 17, e13068. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.J.; Seow, K.M.; Chen, K.H. Preeclampsia: Recent advances in predicting, preventing, and managing the maternal and fetal life-threatening condition. Int J Environ Res Public Health 2023, 20, 2994. [Google Scholar] [CrossRef] [PubMed]
- Martin-Alonso, R.; Prieto, P.; Fernández-Buhigas, I.; German-Fernandez, C.; Aramburu, C.; Piqueras, V.; Cuenca-Gomez, D.; Ferrer, E.; Rolle, V.; Santacruz, B.; et al. Association between perinatal outcomes and maternal risk factors: A cohort study. Medicina 2024, 60, 1071. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).