1. Introduction
In December 2019, the emergence of pneumonia cases [
1,
2] in the Chinese city of Wuhan led to the discovery of the SARS-CoV-2 virus, responsible for COVID-19, which was declared a global pandemic by the World Health Organization (WHO) on 11 March 2020. Since then, more than 770 million cases and around 7 million official deaths have been recorded [
3,
4], with long-term projections indicating greater impact on mortality too. The disease is mainly transmitted through respiratory droplets and contaminated surfaces, with variable symptoms ranging from severe to no symptoms at all.
Despite the emergence of new viral variants, including Alpha, Delta and Omicron, which have affected the diagnosis, the treatment and vaccine efficacy, as well as preventive interventions such as social distancing, masks and vaccinations [
5,
6] have greatly reduced the epidemiological impact of COVID-19. However, the pandemic has also caused severe economic and social consequences at a global scale, further exacerbated by worldwide inequalit
y and misinformation.
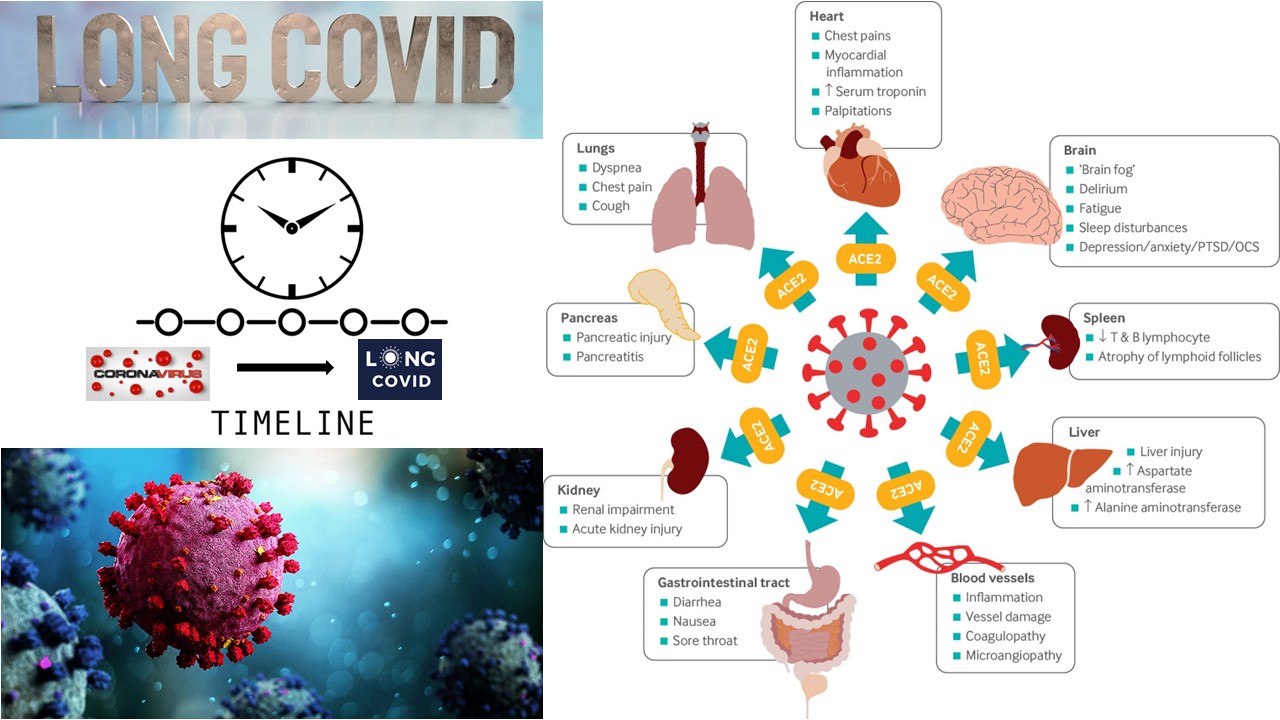
In addition to its acute effects, COVID-19 gave rise to ‘
long COVID’ [
7,
8], a condition characterised by persistent symptoms such as fatigue, cognitive problems and shortness of breath. This syndrome [
9], which can affect various body systems [
10], represents a public health challenge, with no clear assestment of its prevalence. Long
-COVID could represent a further global health crisis, indded additional research into its mechanisms and treatments is needed in order to mitigate its worldwide impact [
11,
12,
13].
Immediately after the beginning of the Covid-19 pandemic, scientific studies appeared in the literature showed the presence of persistent symptoms; as early as March 2021, a review [
14] identifies ‘Long COVID’ as a complex, multifactorial illness that describes the residual effects of the acute COVID-19 infection; while thousands of patients experienced ‘mild’ COVID-19 symptoms not requiring hospital admission, a large proportion were collectively suffering from post-COVID-19 sequelae; most commonly patients present persistent breathlessness, fatigue and cough (other symptoms noted were chest pain, palpitations, neurological symptoms, rashes, gastrointestinal dysfunction and cognitive blunting).
At the same time, in large study [
15], was report that chronic post-COVID “brain fog” has significant association with gender (female), respiratory symptoms at the onset, and the severity of the illness (intensive cure admission).
Another study [
16] based on single-center questionnaire study on 1007 participants recovered for COVID-19, showed that a considerable part of patients had persistent symptoms even 4–5 months later COVID-19 diagnosis, and even for patients with a mild-to-moderate disease suffered from persistent symptoms (respiratory or cardiovascular and neuropsychiatric symptoms); the study concludes that, COVID-19 is different from classical respiratory infections and requires detailed monitoring, even after recovery.
In 2022, one year after the start of vaccination against covid-19, the role of the vaccine in relation to the development of ‘long covid syndrome’ was studied [
17]; in particular most of the results outlines that vaccinated patients show improvement in long COVID symptoms compared to unvaccinated patients and however, the effectiveness of the current evidence is limited, and further research needs to be carried on to identify the impact of vaccination on long COVID symptomatology.
2. Materials and Methods
The study was designed as a non-profit, single-centre observational study with the aim of investigating the long COVID syndrome among health workers (HWs). The adopted approach was descriptive and analytical. It was mainly addressed to aimed at defining and characterising the affected patients, assessing the epidemiological impact of the syndrome, and searching for possible links with (i.e predisposing conditions) between clinics during the acute phase and long-term persistent symptoms.
The monocentric context of the study derives from the recruitment of clinical and non-clinical healthcare workers employed in hospital and outpatient facilities in Basilicata during the period considered (between Jan 2021 to Jan 2023); the use of a sample of workers from the health sector stems from the ease of enrolment as they are subject to health surveillance according to Italian national legislation.
The study population consisted in healthcare workers who contracted COVID-19, which were identified through a regional database. The selection process included a pre-questionnaire addressed to verifiy compliance with predefined basic conditions including diagnosis of SARS-CoV-2 infection by nasopharyngeal swab, availability of information on the period of infection, vaccination cycle against COVID-19, and informed consent on the processing of personal data.
Participants who did not fulfil at least one of the above conditions were excluded from the study. Furthermore, to avoid selection bias, those who had not completed the questionnaire or provided inconsistent or incomplete answers were excluded too.
Data were collected via a structured questionnaire, administered online via the REDCap platform. Invitations to participate were sent, via e-mail, in the period July-September 2024, to about 1,100 healthcare professionals, with a completion period extended until 31 August 2024. To facilitate the questionnaire completion process and increase participation, the participants had the possibility to save their responses and complete the questionnaire in multiple sessions. The questionnaire used derives from a questionnaire used and validated by “Federation of General Practitioners in Italy” and has been modified according to the scientific evidence of long-term symptoms highlighted in the scientific literature.
The questionnaire was divided in three thematic sections in order to collect demographic data (age, gender, weight, height and smoking habits), vaccination history (COVID-19, influenza and pneumococcal) and medical history. Questions were included to record the occurrence of symptoms during the infection and their persistence or possible subsequent appearance, with a focus on respiratory, neurological, cardiological and systemic symptoms. Additional sections were included to assess the impact on quality of life and the presence of pre-existing comorbidities.
The collected data were anonymised in accordance with the Italian Privacy Code (D.lgs. 196/2003) and the European Regulation 2016/679 (GDPR). Processing was performed using the PSPP (GNU PSPP Statistical Analysis Software) by performing descriptive and correlation analysis to identify significant predictors of post-COVID-19 symptoms. Continuous data were classified using specific cut-offs and transformed into qualitative dichotomous variables alloing more precise statistical analysis.
The study was approved by Single Regional Ethics Committee (protocol no. 47866 of 9 September 2020) and conducted according to “Good Clinical Practice guidelines and the principles of the Declaration of Helsinki”. Each participant provided informed consent for the inclusion of their data, ensuring compliance with privacy and data protection regulations.
Data obtained from the questionnaire revealed associations between symptoms experienced and SARS-CoV-2 infection. To investigate this evidence, the Odds Ratio (OR) was calculated.
Variables analyzed and their role as risk or protective factor:
Calculated BMI, subjects with a value greater than 30 (kg/m2) were evaluated;
Gender, associations with Female were considered;
Presence of influenza vaccine;
Full cycle vaccination for Covid-19;
Sars-Cov-2 infection before the first dose of Covid-19 vaccine;
Pandemic waves;
Pharmacological therapy with anti-inflammatories.
Statistical analysis was conducted by calculating the odd ratio (OR) by identifying exposure classes (assuming predisposing risk factors for the development of prolonged symptoms) and assessing the presence of symptoms. Statistical significance was calculated by considering the probability of observing results obtained by chance to be less than 5%).The data processing was authorised by filling in the informed consent administered via the REDCap electronic platform; after acceptance, the system generates a pdf-file of the consent sent by e-mail to the participant. Statistical analysis was conducted using the statistical software PSPP software; the database collected via the REDCap platform was anonymised for the purpose of statistical analysis.
3. Results
3.1. Descriptive Sample Analysis
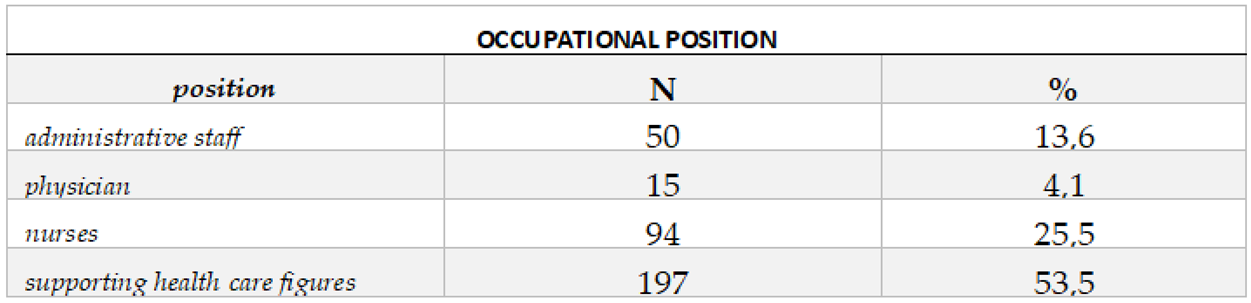
Questionnaires were sent out to approximately 1,100 health workers, obtaining 368 responses, about 33 % of the total. The sample had an average age of 50.38 years, with 59 % of female, 37 % male and 4% did not indicate the gender.
Table 1.
Basic sample description relating to the job and role.
Table 1.
Basic sample description relating to the job and role.
Table 2.
Sample description.
Table 2.
Sample description.
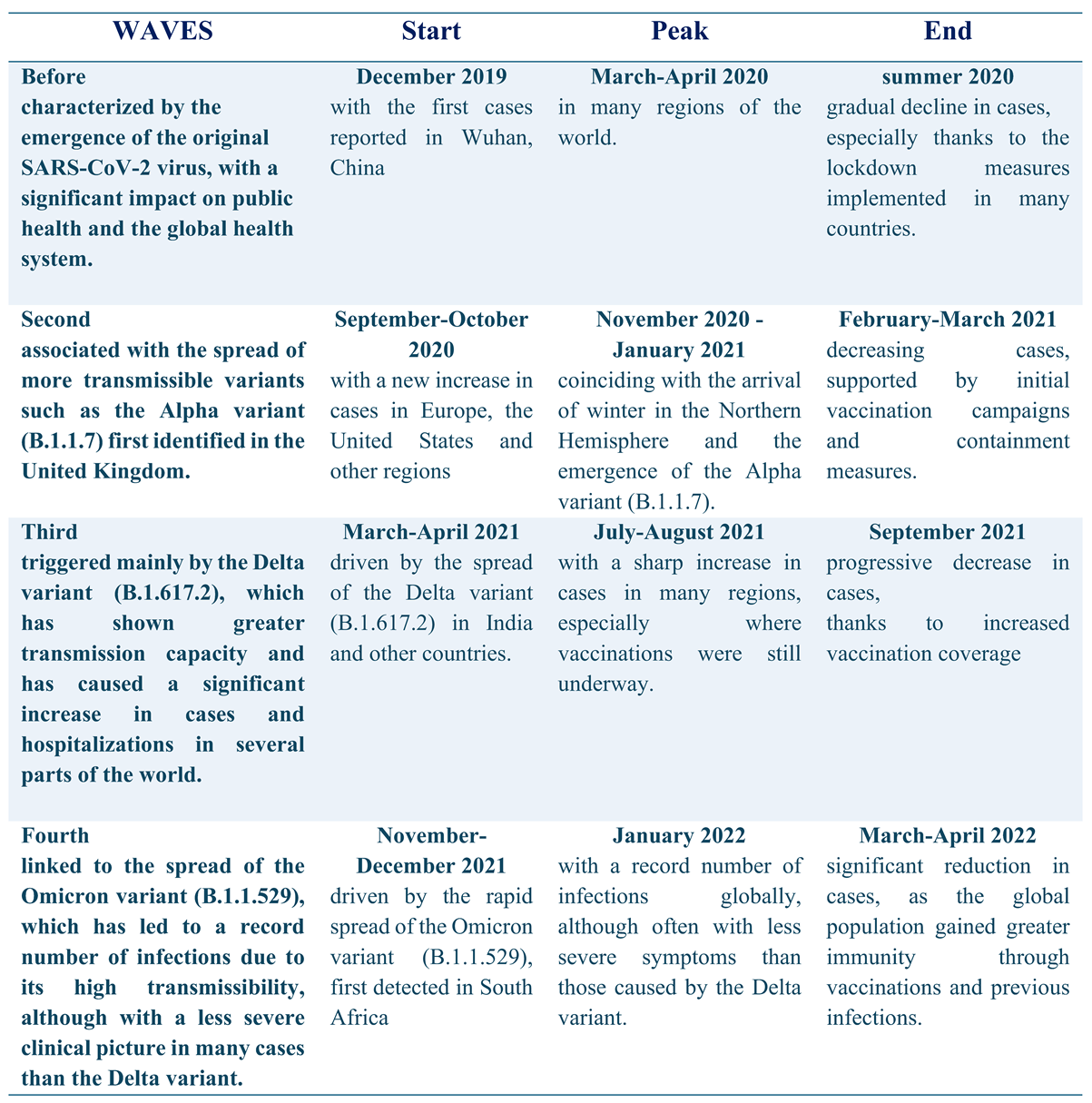
In the sample analysed, 52.7% of participants reported symptoms of fatigue associated with long COVID, a chronic condition whose prevalence varied significantly over time. In the first pandemic wave only 0.7% of the sample reported this symptom, but this percentage rose to 13.3% in the second wave, 14.2% in the third and 29.3% in the fourth wave. Furthermore, in the fourth wave, 38.2% of HWs reported fatigue as a new symptom, highlighting the need to pay particular attention to the long-term effects of the infection; compared to males, the females were associated with a higher risk of persistent fatigue and tachycardia. The second pandemic wave, characterised by the Alpha variant, was associated to an increased risk of neurological symptoms, such as memory problems and slowed thinking.
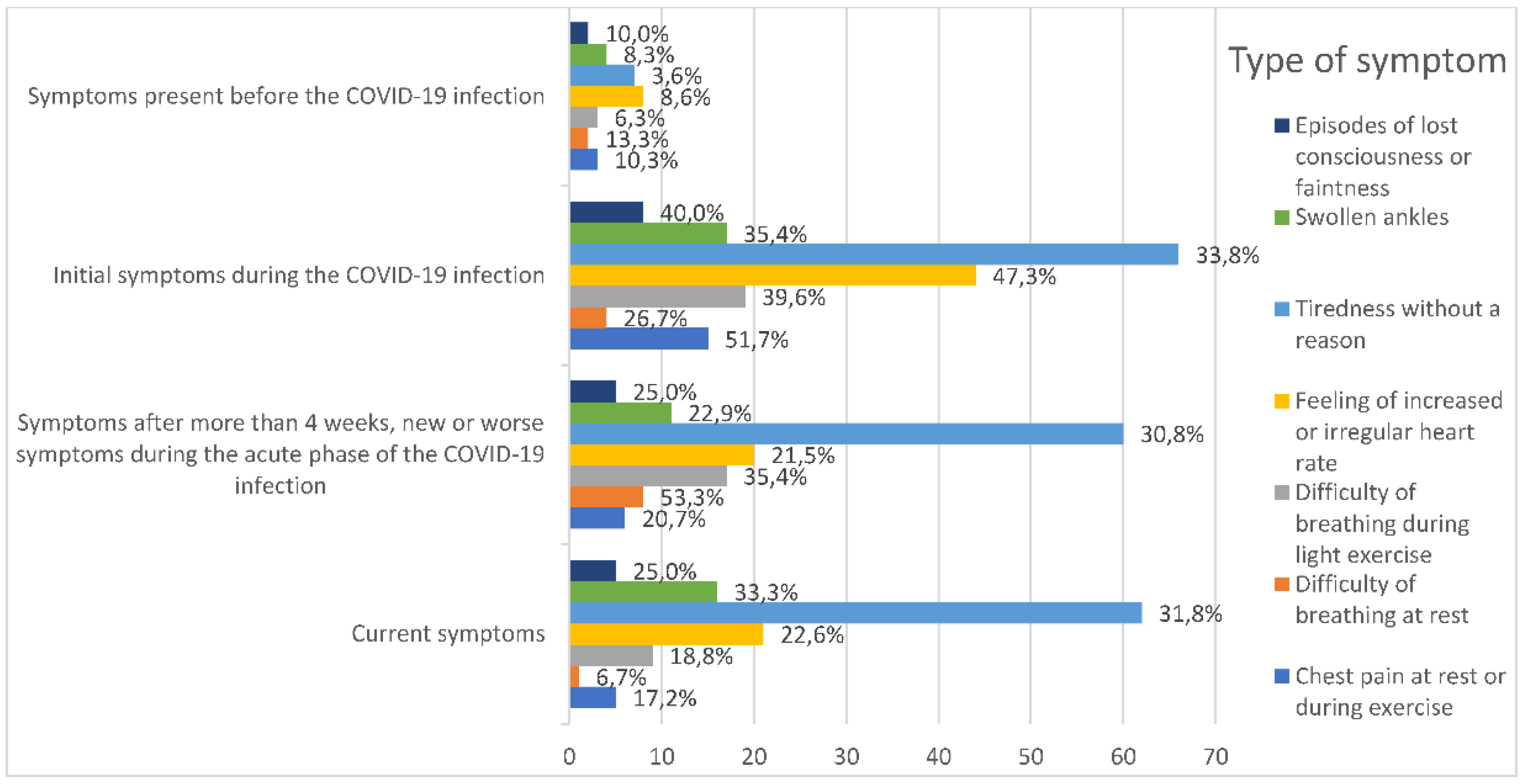
Among the persistent symptoms (
Figure 1), fatigue seemed to be the most common, reported by 22.4% of workers four weeks after infection, and 23.1% of those still continue to experience it today. Other relevant symptoms included tachycardia (7.8%), joint pain (32.9% persistent and 11.6% new) and ankle swelling (6% persistent). Neurological symptoms, such as memory problems, difficulty finding words and slowness in thinking, were reported by 13.1% of workers more than four weeks after infection. In addition, headaches and sleep disorders (9.3%) complete the symptom picture suggesting a complexity of interconnected manifestations.
With regard to demographic and lifestyle characteristics, 14% of the participants with available BMI (body mass index) data had an index of more than (30 kg/m²), indicative of obesity. Regarding smoking habits , 15% of the sample were smokers, 3 % of which consume more than 20 cigarettes per day. This trend further declined with age: in the 25-40 age group, 88% of participants were non-smokers, the percentage dropped to 71% for the group of 41-60, and then raised up to 94% in those over 60 years of age.
An important finding was observed regarding the vaccination coverage: almost 60% of workers received their first dose of anti-COVID-19 vaccine as early as October 2021. However, there was low adherence to the influenza vaccine, with only 35% of the sample vaccinated, and only 19 people reported having received both the flu vaccine and the pneumococcal vaccine.
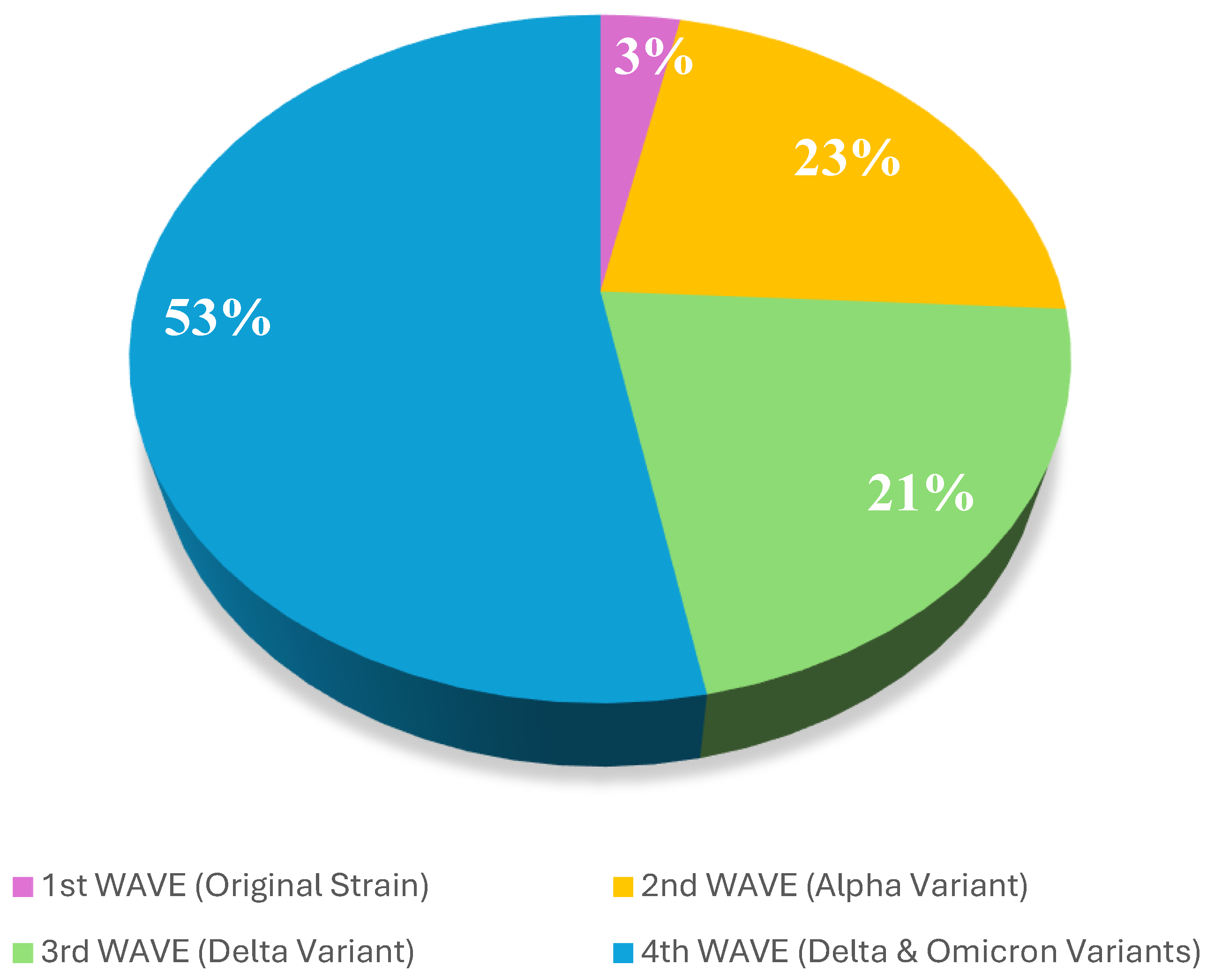
These results highlight that the impact of COVID-19 on healthcare workers has been significant, with persistent manifestations and increasing prevalence of symptoms, especially in more recent waves; analysis of the collected data shows an increasing trend in COVID-19 infections among healthcare workers during the time. Considering that healthcare workers have worked close to the covid-19 patient contact with COVID-19 patients, the growth in infections observed in the various waves becomes particularly significant, as observed in the
Figure 2 witch refers to investigated HWs.
During the first wave (March-September 2020), only 3.3% of healthcare workers contracted the virus, likely due to the containment measures and personal protective equipment adopted in this early phase. However, as the pandemic intensified and cases increased, the second wave (October 2020-July 2021) shoved an increase in infections among healthcare workers, with 23% infected. This reflects the intense exposure to the virus, despite safety measures. The third wave (August 2021-March 2022) reported 20.7% of workers infected, a period in which the high workload and the emergence of more contagious variants increased their exposure. Finally, in the fourth wave (April 2022-December 2023), the peak reaches 53%, probably due to the normalization of daily life and a reduced attention to preventive measures.
Table 3.
Evolution of the Covid-19 along the four waves virus and its appearance (source WHO).
Table 3.
Evolution of the Covid-19 along the four waves virus and its appearance (source WHO).
Finally, none of the participants required invasive or non-invasive oxygen therapy during infection, and the most commonly used drug therapy was anti-inflammatory drugs.
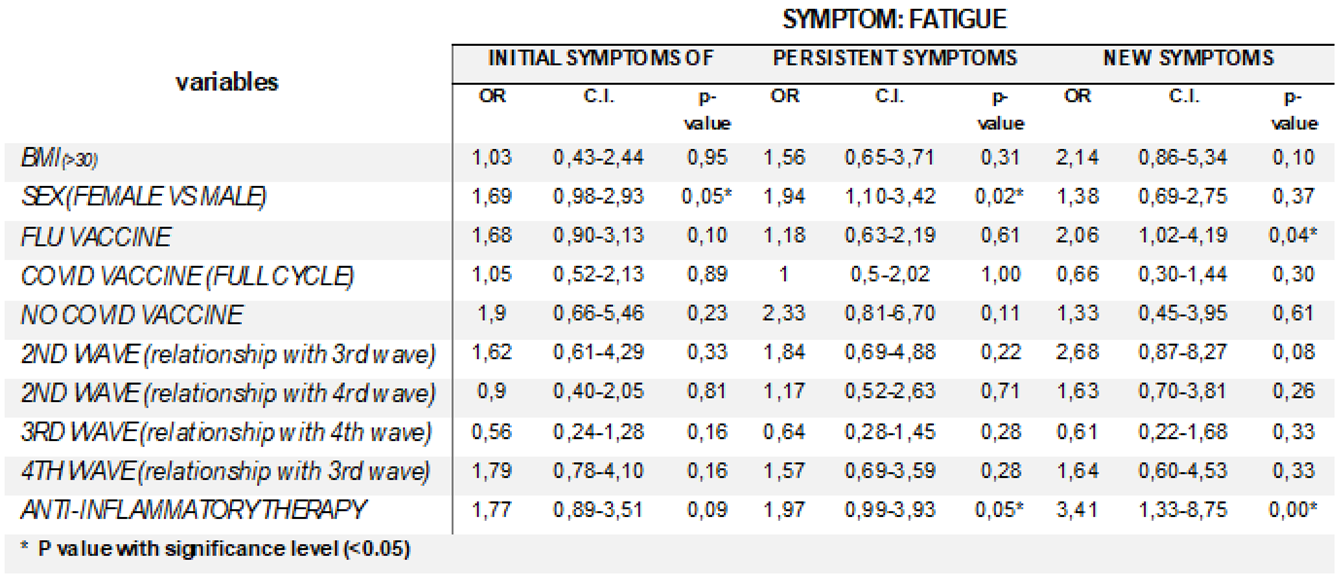
3.2. Data Analisys
With regard to the general part of the symptom history, the symptom of fatigue during the early, persistent stages of the infection and as a newly experienced symptom was assessed. From the analysis of the data collected on fatigue, the female gender emerges as a potential risk factor for this symptom in the different stages of COVID-19 infection (
Table 4).
In general “Persistent symptoms" (OR 1.94, CI 1.10-3.42, p=0.02), suggest that women are significantly more likely to experience persistent fatigue; while for "new fatigue symptoms", there is no significant association between female gender and the occurrence of new fatigue episodes.
3.2.1. Fatigue Symptom
The data on “fatigue” suggest that influenza vaccine might influence the onset of this at various stages of COVID-19 infection; with regard to “new fatigue episodes occurring subsequently” (OR 2.06, CI 1.02-4.19, p=0,04) data outline that influenza vaccinated individuals should have a higher risk of experiencing new post-infection fatigue episodes. OR for the initial symptom of fatigue during infection (1.77, CI 0.89-3.51, p=0,09) show association between use of anti-inflammatory drugs and increased risk of fatigue. “Persistent fatigue during infection” (OR 1.97, CI 0.99-3.93, p=0,05) underlines a more robust association. Finally, data concerning “newly experienced fatigue symptoms” (OR 3.41, CI 1.33-8.75, p<0,001) indicates a strong link between the use of anti-inflammatory drugs and the onset of fatigue.
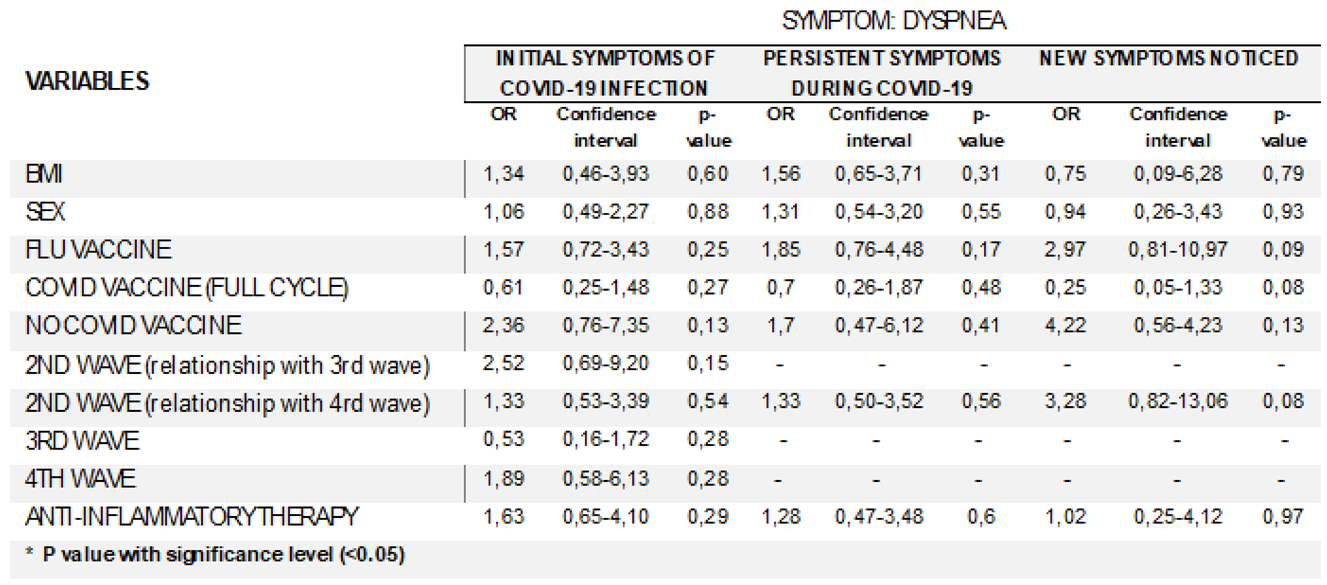
3.2.2. Dyspnoea Symptom
Despite the borderline statistical significance, the data of dyspnea symptom indicate an increasing association between the absence of vaccination and dyspnoea, with OR rising over time (
Table 5). Data suggest that unvaccinated individuals had more than twice the risk of developing dyspnoea compared to vaccinated individuals.
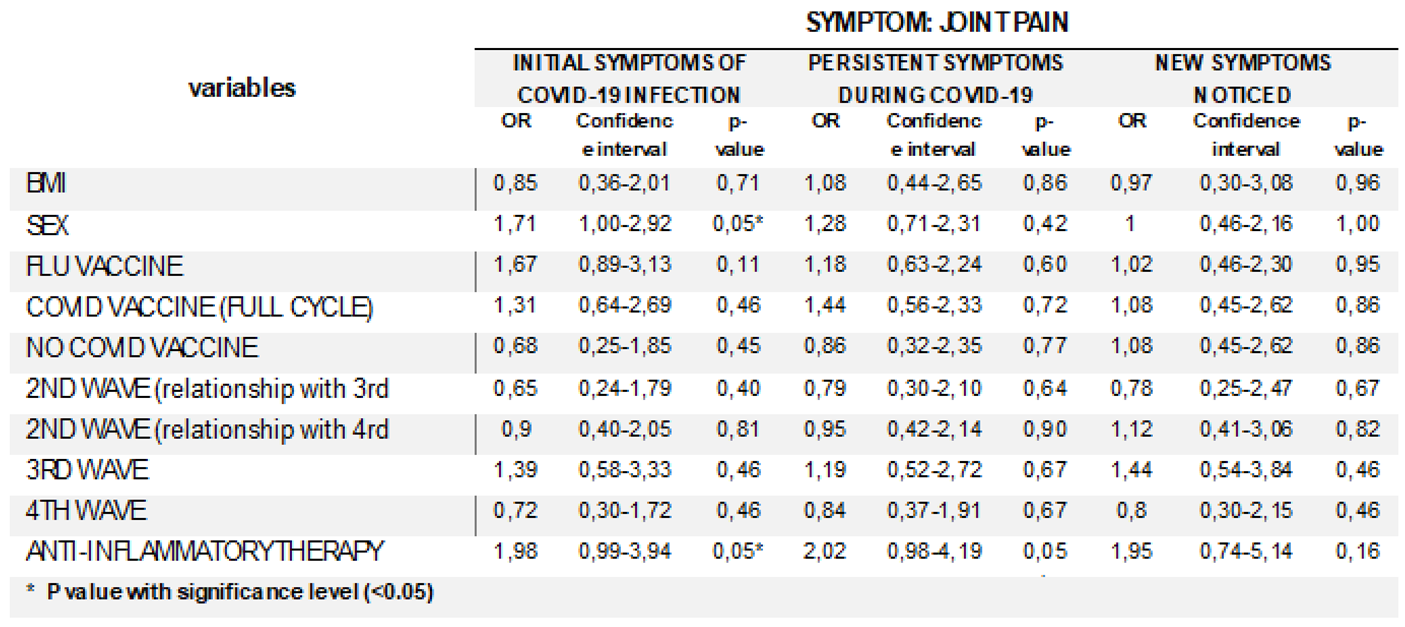
3.2.3. Joint Pain Symptom
The analysis of “joint pain” data shows a possible association between the female gender and the risk of developing joint pain as a post-COVID symptom at various time points, even if this relationship changes over time and exhibits varying levels of statistical significance (
Table 6).
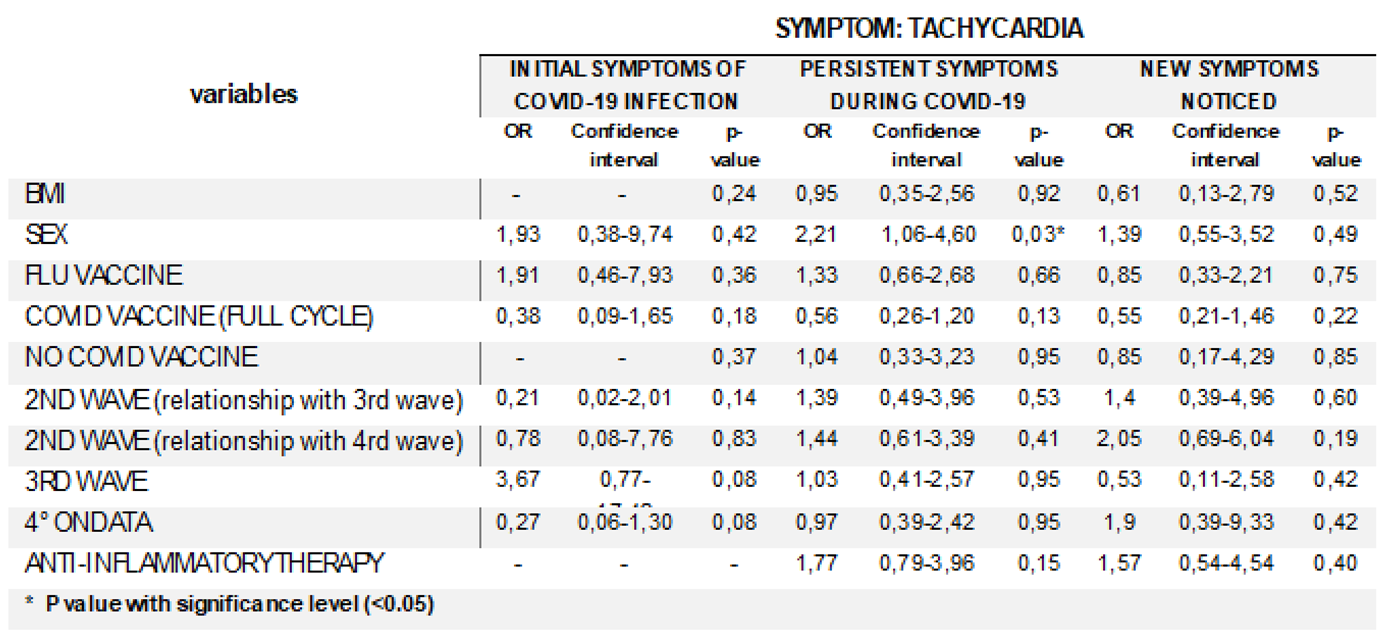
3.2.4. Tachycardia Symptom
The data reported in
Table 7 highlight a possible effect of COVID-19 in temporarily increasing the risk of tachycardia in women, compared to a pre-existing predisposition. Howeverthis influence seems to diminish, over time, bringing the risk back to levels similar to those ex-ante infection.
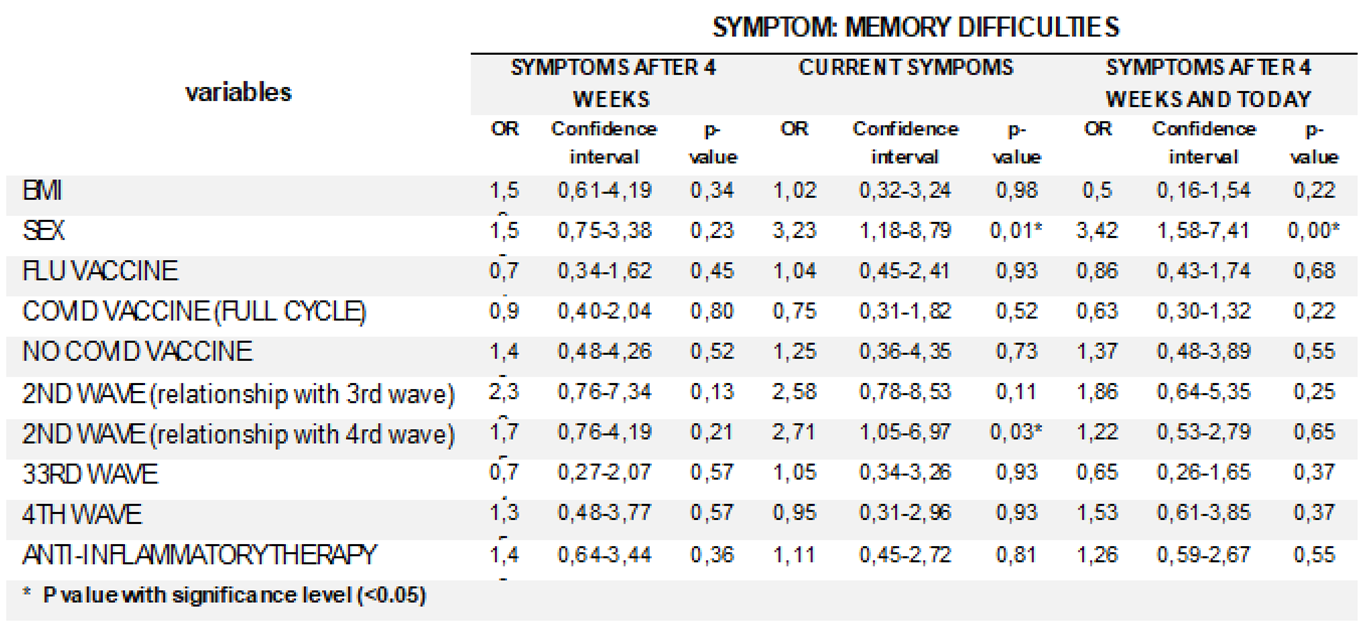
3.2.5. Neurological Symptoms
The analysis reveales a significant increase in risk associated with the female gender, particularly concerning memory problems, difficulty finding words, and slowed thinking. (
Table 8).
Results indicate that women have a significantly increased risk of experiencing persistent cognitive difficulties, suggesting a lasting effect of the infection on neurological function.
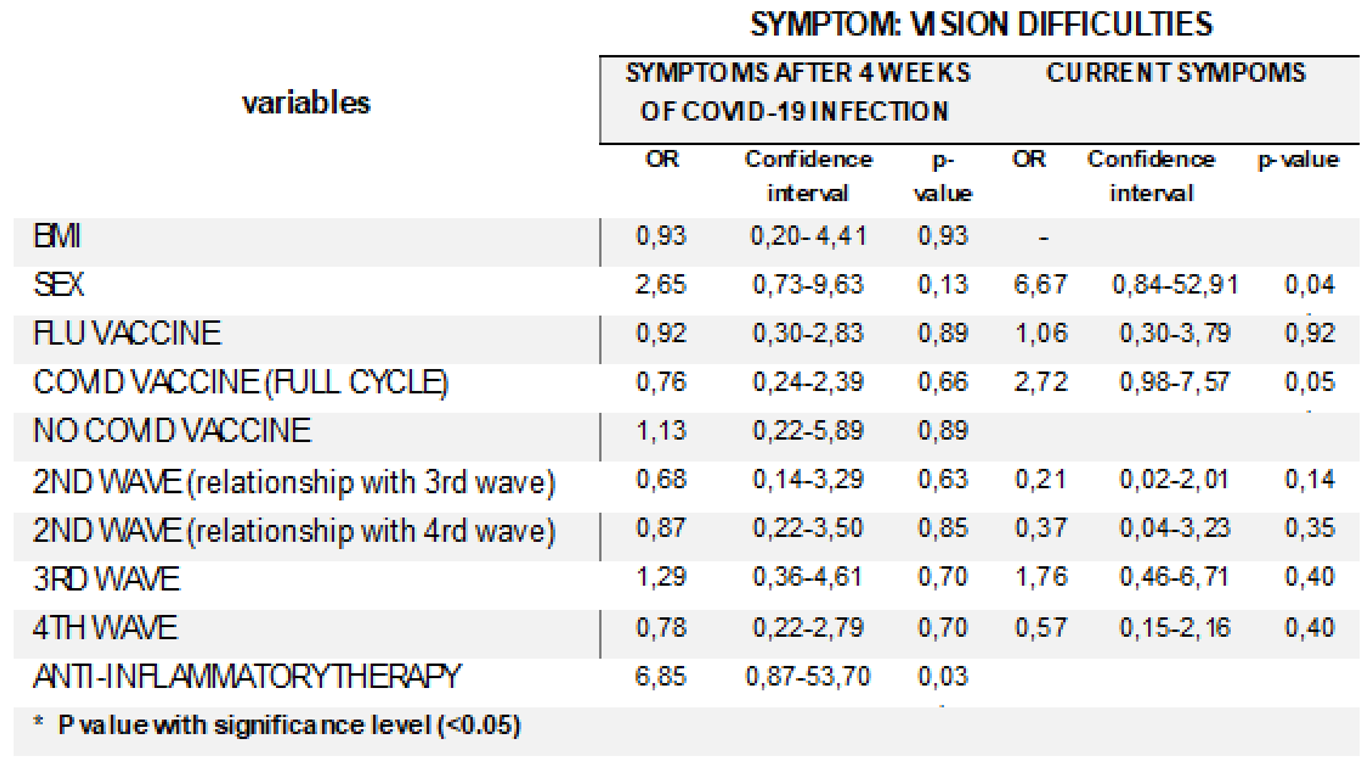
3.2.6. Visual Symptoms
The analysis of visual symptoms, including loss of vision in one or both eyes, double vision, blurred vision, and difficulty focusing, provides important insights into the impact of full vaccination against COVID-19 (
Table 9).
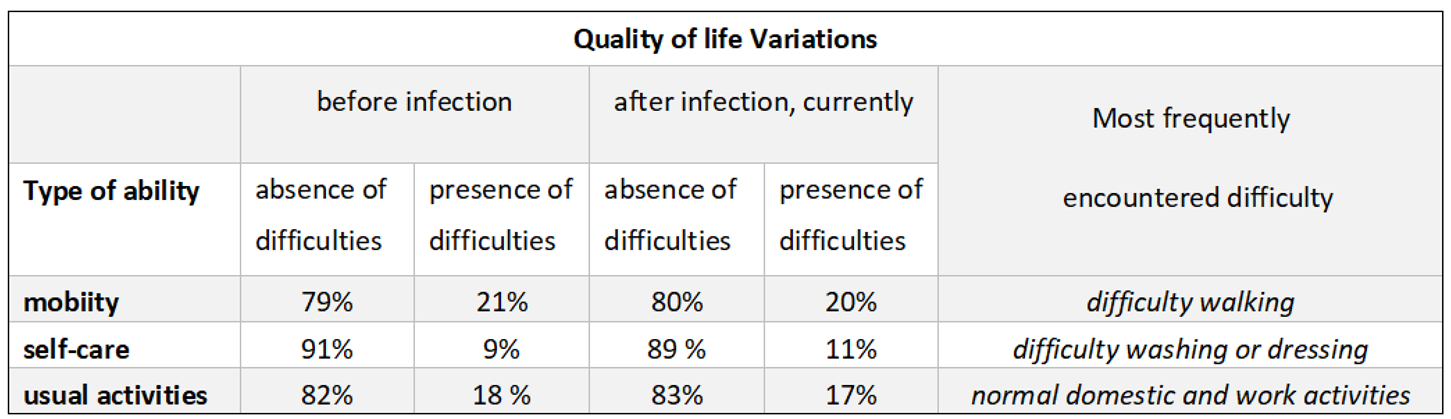
3.2.7. Quality Life
The analysis of the data on quality of life does not show substantial variations with regard to the perception of individual autonomy in the pre- and post-infection period; the sample has not a substantial percentage variations in the number of people who experienced changes in quality of life and personal autonomy.
Table 10.
Quality of life variations.
Table 10.
Quality of life variations.
4. Discussion
Despite the widespread vaccination campaigns and evolving treatment protocols, the persistent symptoms, commonly referred to as ‘long COVID’, remaine a significant concern.
Key factors such as previous influenza vaccination, gender, BMI and time of infection versus vaccination, were explored for their potential associations with these persistent symptoms. In this context, fatigue emerged as one of the most frequently reported debilitating symptoms, affecting both personal well-being and job performance. Analysis utilise data collected through detailed questionnaires, assessing associations between reported symptoms and potential risk factors as arises from statistical approach appropriate for retrospective case-control studies. These findings are particularly important in understanding the role of specific variables, including gender and therapeutic interventions, in modelling the risk profile for long COVID among healthcare workers.
This analysis assesses the correlation between several risk factors and the onset, persistence and recurrence of post-COVID-19 symptoms in previously infected workers, paying particular attention to healthcare workers exposed during the pandemic [
18,
19]. Some risk factors are explored including sex, different pandemic waves (with their respective variants), use of drug therapies with anti-inflammatory drugs, and influenza and anti-COVID-19 vaccinations.
The results of the present study highlight a variety of risk factors including female sex, high body mass index, presence of systemic symptoms with the need for anti-inflammatory therapy, and the presence of persistent and new symptoms occurring in the post-COVID-19 phase. People that received a complete set of the Covid vaccinations [
20] seemes to be associated with a reduction in the probability of developing symptoms linked to "long COVID”. The results clearly indicate the need for further research to better understand the specific dynamics related to long-term COVID susceptibility, considering gender and the role of influenza and anti-COVID-19 vaccination especially. It emerges that the female gender should present risk factor for symptoms such as fatigue, tiredness and tachycardia during and after infection, suggesting a peculiar vulnerability in women that could imply a higher risk of symptom persistence (
Table 4-5-7-8 and 9). Data confirm that the females are significantly associated with the risk of persistent fatigue during infection. In contrast, due to the occurrence of new fatigue episodes in the post-infection phase, the association is not significant. However, the observation of a possible correlation between the influenza vaccine and new post-infection fatigue episodes suggests the need for further investigation to assess susceptibility to new or persistent symptoms in vaccinated subjects. “Persistent fatigue during infection” (OR 1.97, CI 0.99-3.93, p=0,05) underlines a more robust association, suggesting that the use of anti-inflammatory drugs might be related to a significantly increased risk of fatigue during this period. Finally, data concerning “newly experienced fatigue symptoms” indicate a strong link between the use of anti-inflammatory drugs and the onset of fatigue.
Analysis of data on the association between the "symptom dyspnea" (tab.5 ) and covid vaccine (full cycle) shows an increased risk in unvaccinated subjects (OR: 2.36) compared with vaccinated subjects (OR:0.61); analysis of “new symptoms appeared after infection” also shows an increased risk in unvaccinated subjects (OR: 4.22) compared with vaccinated subjects (OR:0.25). In all cases, statistical significance near the threshold suggests studies with increased sample size.
Risk of joint pain (
Table 6) in women appears to be higher in the weeks immediately following infection, suggesting a transient vulnerability in the post-acute period of COVID-19. However, this association tends to diminish in the long term. Again, the use of anti-inflammatory drugs appears to be associated with an increased risk of joint pain, especially in the post-infection period, although significance is limited for new symptoms. Exploration of this association could provide important insights for therapeutic strategies in COVID-19 patients.
Symptoms of fatigue and tachycardia (
Table 4,7) [
21] were associated with the female gender, both during infection and afterwards. This finding, combined with the higher incidence of fatigue in those infected during the second wave (Alpha variant), suggests a different response between the virus variants, with the Alpha variant having a sensitive impact on long-term symptoms. This association is also significant for those who have used anti-inflammatory drugs, particularly for persistent and new symptoms. The importance of long-term patient monitoring appears crucial, especially in women, to manage the potential cardiovascular and systemic consequences of COVID-19.
Neurological symptoms, including memory problems (
Table 8) [
22], word-finding difficulties and slowed thinking, are more frequent in women and patients infected during the second wave. This suggests a greater post-COVID cognitive impact for certain patient groups, outlining the need for careful monitoring and specific interventions to improve cognitive recovery, particularly for women and those infected with the Alpha variant. Data show an association between visual symptoms and the use of anti-inflammatory drugs, suggesting that such therapies may have an impact on these symptoms.
The clinical and public health implications of this study suggest that vaccination should be considered as a preventative measure for the general population, particularly those with risk factors for developing persistent symptoms, such as obesity and chronic lung disease. This would help to prevent increased absenteeism and reduced work performance in all occupational sectors and would generally help to prevent a reduction in quality of life for people at high risk of persistent symptoms. In the future, it will be important to evaluate the proposal of vaccine recalls for employees at risk of long-term illness and to implement proper communication on risk perception and vaccine efficacy.
The most important contribution to the study of predisposing factors for the development of long covid syndrome comes and will come from data acquired in the future, such as those from the study currently in progress [
23]; the current knowledge in literature suggests that the symptoms associated with long covid syndrome and its predisposing factors should be further investigated and studied.
Limitations
The study provides significant associations in the analysis of various risk factors studied; similarly, the role of age at which infection is contracted seems to determine the development of “Long Covid”. Further studies might provide support for the results.
The number of HWs who agreed to participate in the survey is statistically acceptable; in fact a sample of 368 individuals is quite significant , allowing to use classical statistical tools based on the normal distribution.
Author Contributions
Conceptualization, M.N.; Methodology, M.N., M. G.; Software, M.N., M. G.; Validation, M.G, L.M.; Investigation, M.N., L.M.; Data curation, M.N, F.P., A.S. and F.A.; Writing – original draft, M.N. and F.A.; Supervision, M.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study and waiver of the informed consent was approved by the local ethic committee (Single Regional Ethics Committee for Basilicata, Via Potito Petrone 85100 Potenza, Italy, Number of ethic committees statement concerning this study: 46/2023, date of decision: 15/07/2023). The study was conducted according to the principles of the declaration of Helsinki.
Informed Consent Statement
informed consent was requested using the model approved by the local ethics committee
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Johns Hopkins Coronavirus Resource Center [Internet]. [citato 6 ottobre 2024]. COVID-19 Map. Disponibile su: https://coronavirus.jhu.edu/map.html.
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef]
- Emergency use ICD codes for COVID-19 disease outbreak [Internet]. [citato 12 ottobre 2024]. Disponibile su: https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak.
- Peluso, M.J.; Swank, Z.N.; Goldberg, S.A.; Lu, S.; Dalhuisen, T.; Borberg, E.; et al. Plasma-based antigen persistence in the post-acute phase of COVID-19. Lancet Infect Dis. 2024, 24, e345–e347. [Google Scholar] [CrossRef]
- Bonilla, H.; Peluso, M.J.; Rodgers, K.; Aberg, J.A.; Patterson, T.F.; Tamburro, R.; et al. Therapeutic trials for long COVID-19: A call to action from the interventions taskforce of the RECOVER initiative. Front Immunol 2023, 14, 1129459–10.3389. [Google Scholar] [CrossRef] [PubMed]
- Al-Aly, Z.; Topol, E. Solving the puzzle of Long Covid. Science 2024, 383, 830–832. [Google Scholar] [CrossRef] [PubMed]
- Parums, D.V. Editorial: Post-Acute Sequelae of SARS-CoV-2 Infection (PASC). Updated Terminology for the Long-Term Effects of COVID-19. Med Sci Monit. 2023, 29, e941595-1–e941595-2. [Google Scholar] [CrossRef] [PubMed]
- Castanares-Zapatero, D.; Chalon, P.; Kohn, L.; Dauvrin, M.; Detollenaere, J.; Maertens de Noordhout, C.; et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. 2022, 54, 1473–1487. [Google Scholar] [CrossRef] [PubMed]
- Mehandru, S.; Merad, M. Pathological sequelae of long-haul COVID. Nat. Immunol. 2022, 23, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Fineberg, H.V.; Brown, L.; Worku, T.; Goldowitz, I. , curatori. A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences; National Academies Press: Washington, D.C, USA, 2024. [Google Scholar] [CrossRef]
- Bonilla, H.; Peluso, M.J.; Rodgers, K.; Aberg, J.A.; Patterson, T.F.; Tamburro, R.; et al. Therapeutic trials for long COVID-19: A call to action from the interventions taskforce of the RECOVER initiative. Front Immunol 2023, 14, 1129459. [Google Scholar] [CrossRef] [PubMed]
- Alkodaymi, M.S.; Omrani, O.A.; Ashraf, N.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Taribagil, P.; Creer, D.; Tahir, H. ‘Long COVID’ syndrome. BMJ Case Rep 2021, 14, e241485. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Akbari, A.; Emami, A.; et al. Long COVID syndrome-associated brain fog. J Med Virol. Accepted: 18 October 2021. J. Med. Virol. 2022, 94, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Kayaaslan, B.; Eser, F.; Kalem, A.K.; et al. Post-COVID syndrome: A single-center questionnaire study on 1007 participants recovered from COVID-19. J Med Virol. 2021, 93, 6566–6574. [Google Scholar] [CrossRef] [PubMed]
- Mumtaz, A.; Sheikh, A.A.E.; Khan, A.M.; Khalid, S.N.; Khan, J.; Nasrullah, A.; Sagheer, S.; Sheikh, A.B. COVID-19 Vaccine and Long COVID: A Scoping Review. Life 2022, 12, 1066. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; et al. Post-acute COVID-19 syndrome. Nat Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Venter, C.; Laubscher, G.J.; Kotze, M.J.; Oladejo, S.O.; Watson, L.R.; Rajaratnam, K.; Watson, B.W.; Kell, D.B. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc Diabetol. 2022, 21, 148. [Google Scholar] [CrossRef] [PubMed]
- Azzolini, E.; Levi, R.; Sarti, R.; et al. Association Between BNT162b2 Vaccination and Long COVID After Infections Not Requiring Hospitalization in Health Care Workers. JAMA 2022, 328, 676–678. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.S.; Page, A.; Bailey, D.; Langdon, A.; Ong, E.; Seeley, M.-C.; Gallagher, C.; Lau, D.H.; Chieng, J. High Incidence of Autonomic Dysfunction and Postural Orthostatic Tachycardia Syndrome in Patients with Long COVID: Implications for Management and Health Care Planning. Am. J. Med. 2023, 138, 354–361.e1. [Google Scholar] [CrossRef]
- Garmoe, W.; Rao, K.; Gorter, B.; Kantor, R. Neurocognitive Impairment in Post-COVID-19 Condition in Adults: Narrative Review of the Current Literature. Arch Clin Neuropsychol. 2024, 39, 276–289. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.; Davis, A.; Stanley, B.; Julious, S.; et al. Risk Predictors and Symptom Features of Long COVID Within a Broad Primary Care Patient Population Including Both Tested and Untested Patients. Pragmatic and Observational Research 2021, 2021, 93–104. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).