Introduction
Mental health disorders, often referred to as mental health diseases, illnesses, conditions or psychiatric disorders, have become a critical global health concern. According to the Global Health Data Exchange (GHDx), in 2019, approximately 1 in 8 individuals, that is, 970 million people worldwide, were living with a mental health disorder, with anxiety and depression being the most prevalent. The International Classification of Diseases 11th Revision (ICD-11) published by the World Health Organization (WHO), defines mental, behavioural, and neurodevelopmental disorders as “syndromes characterised by clinically significant disturbances in an individual’s cognition, emotional regulation, or behaviour, reflecting dysfunctions in psychological, biological, or developmental processes that underlie mental and behavioural functioning.” These disturbances typically lead to distress or impairment in personal, social, educational, and occupational functioning amongst others. The cause of mental health disorders, as well as those at risk, has been attributed to various factors and is often dependent on the specific mental health disorder in question. However, it can generally be ascribed to a combination of individual, familial, community, and structural factors that can either safeguard or compromise mental health. Traditional methods of diagnosis, prognosis, therapy, and management of these disorders are lacking in accessibility, timeliness, and personalisation, leading to potential misdiagnoses or delays in treatment. These delays can exacerbate symptoms and worsen patient outcomes. In response, artificial intelligence (AI) has emerged as a promising tool to bridge these lapses in recent times however, to what extent? This research aims to methodologically review the current technologies of AI in diagnosing, treating, and managing mental health disorders. It will evaluate the effectiveness of these AI tools, identify existing challenges, and provide recommendations for future research and implementation.
Background
Mental health disorders are often chronic conditions that require long-term monitoring and treatment with most being incurable. These disorders include conditions such as autism spectrum disorder (ASD), schizophrenia, anxiety, depression, bipolar disorder, and post-traumatic stress disorder (PTSD). They contribute significantly to the overall burden of disability, as the forefront source of disability worldwide (GBD 2019 Mental Disorders Collaborators, 2022). Mental health is not only the lack of psychiatric diagnoses, but also the presence of well-being, where individuals can recognize their abilities, cope with normal stresses, work productively, and contribute to their community (WHO, 2004). However, the global burden of mental health disorders continues to increase. According to a 2022 systematic review by WHO, mental health disorders rank among the top ten leading causes of disease burden worldwide. Disability-adjusted life years (DALYs) due to mental health disorders rose from 80.8 million in 1990 to 125.3 million in 2019 (GBD 2019 Mental Disorders Collaborators, 2022). The COVID-19 pandemic further exacerbated the mental health crisis, with significant increases in depression, anxiety, and PTSD reported globally (Xiong et al., 2020). Mental health disorders impose significant personal and societal costs, affecting not just the individuals who suffer from them but also their families, communities, and economies. Globally, mental health conditions cost the economy approximately between $1 trillion and $2.5 trillion annually due to productivity losses and bad health, primarily from common disorders like depression and anxiety with a projected increase to $6 trillion by 2030 (WHO, 2022; The Lancet Global Health, 2020). Both the ICD-11 and Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5-TR) classify mental health disorders into 21 major categories. Some of the primary classifications include Neurodevelopmental Disorders, Schizophrenia and Other Psychotic Disorders, Mood Disorders, Anxiety and Fear-related Disorders, Obsessive-Compulsive and Related Disorders, Disorders Specifically Associated with Stress, Dissociative Disorders, Feeding and Eating Disorders, and Substance Use and Addictive Behaviours. The ubiquity of mental health disorders such as depression, schizophrenia, and bipolar disorder has increased remarkably, posing considerable challenges to healthcare systems globally. Recently, there has been an increase in global efforts to prioritise mental health to lessen the negative impacts of severe forms of mental disorders. Among these efforts is the Comprehensive Mental Health Action Plan initially adopted in 2013, which was extended to 2030 at the 72nd World Health Assembly (Gureje et al. 2015; WHO 2019). As such, the diagnosis, prognosis, treatment, and management of these conditions are of paramount importance. Clinical interviews, psychological testing, medical evaluations, psychotherapy and medication management, continuous monitoring, crisis intervention, rehabilitation, and lifestyle modifications to support long-term well-being are traditional applications for the diagnosis, prognosis, therapy, as well as management of mental health disorders. These traditional approaches often face challenges such as limited access to care, timeliness, high costs, and varying effectiveness based on personalisation.
The integration of Artificial Intelligence (AI) into mental health care has gained significant momentum, heralding a transformative shift in the diagnosis, therapy, and management of various mental health disorders. Consequently, AI technologies, including Machine Learning (ML), Deep Learning (DL), and Natural Language Processing (NLP), are increasingly seen as potential solutions to revolutionise mental health care. These technologies have been used to analyse large datasets, predict treatment outcomes, and provide personalised interventions. AI has become one of the brightest methods for automating cognitive evaluations, a range of tasks and tests for appraising cognitive abilities. Some of these are language, intellect, memory, situations judgement, awareness, and perception (Thakkar et al., 2024). These AI technologies use algorithms that translate information acquired from datasets into meaningful solutions. For instance, such algorithms developed and employed are Neural Networks (NN), Decision Trees (DT), K-nearest neighbours (KNN), Linear Regressions (LR), and Support Vector Machines (SVM) (Nwoye et al., 2020). Most of these algorithms are built using programming software like Python, R-studio, and C++. These AI techniques have taken the role of digital assistants which are crucial in the progress of the health industry to assist health practitioners. Overall, AI offers personalised, scalable, and cost-effective diagnosis, therapy, and management options.
Despite the possibilities of AI in mental health care, its implementation faces obstacles such as data privacy concerns, ethical challenges, and the need for large, diverse datasets to ensure the accuracy and generalizability of AI models. Additionally, with many emerging AI technologies and less progress, the real-world impact of AI on mental health care remains underexplored thus, there is a need for a comprehensive review to understand the role of AI in improving diagnosis, prognosis, treatment outcomes, and patient management across various mental health conditions. By addressing these issues, this study aims to enhance mental health care, ultimately improving patient outcomes and supporting healthcare providers in delivering more effective and personalised care.
Neurodevelopmental disorders, including behavioural and cognitive impairments, arise during the developmental period and involve significant challenges in acquiring and performing intellectual, motor, language, or social functions (WHO, 2022). Among these is ASD, which encompasses a range of conditions characterised by difficulties in social communication and interaction, along with restricted, repetitive behaviours, and inflexible interests or activities. Early intervention, including medications, psychosocial, behavioural, occupational, and speech therapies, can be effective.
Schizophrenia is a severe and debilitating mental illness that affects cognition, thought processes, and behaviour. It is a chronic condition characterised by positive symptoms, such as delusions and hallucinations; negative symptoms, including apathy, lack of motivation, and social withdrawal; and cognitive symptoms, such as disorganised speech, thoughts, psychomotor disturbances, and catatonic behaviour (Möller, 2016). These symptoms can severely disrupt an individual's ability to function in work or school environments (WHO, 2019). While it is a chronic condition, it can be managed effectively with medication, emotional support, psychoeducation, family interventions, and psychosocial rehabilitation (WHO, 2022). Recent advancements in neuroimaging and genetics are aiding in the understanding of schizophrenia’s biological underpinnings, offering hope for more targeted treatments (van Erp et al., 2018).
Depression is the persistent feelings of sadness, irritability, or emptiness, along with a loss of interest or pleasure in activities, lasting most of the day for at least two weeks. It differs from normal mood fluctuations and transient emotional responses to life challenges. Additional symptoms may include poor concentration, excessive guilt, low self-esteem, hopelessness, thoughts of suicide, sleep disturbances, changes in appetite, and fatigue. Individuals with depression are at an increased risk of suicide, yet effective medications and psychological treatments are available.
Anxiety disorders are distinguished by extreme fear, worry, and associated behavioural disturbances, causing serious distress or impairment in daily functioning. Several types of anxiety disorders exist, including generalised anxiety disorder (excessive worry), panic disorder (panic attacks), social anxiety disorder (fear of social situations), and separation anxiety disorder (fear of separation from loved ones). Effective psychological treatments, and in some cases, medication, are available for managing anxiety disorders depending on age and severity (WHO, 2022). Emerging treatments, such as cognitive-behavioural therapy (CBT), have shown efficacy in reducing anxiety symptoms (Hofmann et al., 2012).
Bipolar disorder involves alternating periods of depressive episodes and manic symptoms. During depressive episodes, individuals experience persistent sadness, irritability, or loss of interest in activities, while manic episodes are marked by euphoria, increased activity, rapid speech, inflated self-esteem, decreased need for sleep, distractibility, and impulsive behaviour. Individuals with bipolar disorder are at an increased risk of suicide. Treatment options include psychoeducation, stress management, social functioning enhancement, and medication (WHO, 2022). Advancements in pharmacological treatments, including mood stabilisers and antipsychotics, have been instrumental in managing symptoms and reducing hospitalizations.
Post-traumatic stress disorder (PTSD) often arises after exposure to highly traumatic or life-threatening events like loss of life, resources, social support and social networks, or huge relocation (Cianconi, Betrò, & Janiri, 2020). Symptoms include re-experiencing the trauma through intrusive memories or nightmares, avoidance of reminders of the trauma, and heightened perceptions of threat. These symptoms typically persist for several weeks and significantly impair functioning. Effective psychological treatments for PTSD are available (WHO, 2022).
AI in Diagnosis, Treatment, and Management of Mental Health Disorders
The global burden of mental health disorders highlights the urgent need for effective diagnostic, therapeutic, and management tools. Since traditional mental health care approaches face significant challenges, including limited resources, long wait times, and inconsistent efficacy, AI has emerged as a promising solution providing scalable, personalised, and cost-effective methods with the potential to revolutionise mental health care (Fadele et al., 2024). John McCarthy, a pioneer in AI, described AI as “the process of making machines behave in ways that would be considered intelligent if a human were to do so” (McCarthy, 1959). AI encompasses systems and machines able to do tasks that would normally require human intelligence, like decoding natural language, drawing patterns, learning from experience, and making decisions. These tasks are achieved through algorithms, data processing, and iterative improvement processes (McCarthy, 1959).
The application of AI and ML technologies here enables healthcare professionals to analyse large datasets and identify mental health conditions with a level of precision that is challenging for traditional methods. AI-based tools are particularly valuable in detecting subtle early signs of mental health issues, often before symptoms become severe, allowing for timely intervention and improved patient outcomes (Thakkar et al., 2024).
AI is revolutionizing the diagnosis of mental health disorders by offering more objective, data-driven criteria compared to the subjective approaches of traditional frameworks like DSM-5-TR and ICD-11. By leveraging biomarkers, neuroimaging, and behavioural patterns, AI-based decision support systems (DSS) enhance diagnostic precision (Tutun et al., 2023). For example, AI tools now screen for cognitive impairments and conditions like autism spectrum disorder (ASD) through methods such as eye movement analysis and maternal blood biomarkers (Zheng et al., 2021). Advances in AI-driven neuroimaging analysis also distinguish between disorders like intellectual disability (ID) and developmental delay (DD) using deep neural networks (Thakkar et al., 2024). In schizophrenia, automated speech evaluation and natural language processing (NLP) models detect early psychosis symptoms and predict relapses by analyzing speech patterns and content (Bedi et al., 2015; Corcoran & Cecchi, 2020). For anxiety and depression, digital phenotyping with AI uncovers early signs through behavioural cues from social media and physical activity, providing insights beyond traditional clinical evaluations (Minerva & Giubilini, 2023).
AI-driven tools are revolutionizing mental health treatment by complementing traditional methods with innovative, tech-driven solutions. Mobile applications use AI to send medication reminders, track adherence, monitor mood changes, and provide real-time feedback, ensuring patient engagement and personalised care (Thakkar et al., 2024). These apps also deliver cognitive behavioural therapy (CBT) interventions, enabling individuals to access evidence-based exercises and track progress from home. Virtual therapists and AI chatbots offer immediate psychological support, particularly in underserved regions (Thakkar et al., 2024). Additionally, AI tailors treatment plans by analyzing patient-specific data, such as genetic predispositions and lifestyle factors, predicting the most effective therapies while minimizing trial-and-error in prescribing medications for conditions like depression and bipolar disorder (Tutun et al., 2023). This approach has proven particularly valuable in addressing treatment-resistant depression through optimal combinations of medications and psychotherapeutic strategies (Minerva & Giubilini, 2023).
AI is transforming the management of mental health conditions by enabling continuous monitoring and adaptive care through real-time data analysis. AI tools track symptoms and medication side effects, allowing for timely adjustments to treatment plans (Thakkar et al., 2024). Digital phenotyping via wearables, smartphones, and social media analyzes sleep, activity, and interactions to detect potential crises, alerting healthcare providers and caregivers for preemptive interventions (Minerva & Giubilini, 2023). AI-powered virtual companions, such as therapeutic avatars, as well as conversational agents, such as Schizobot, help patients with schizophrenia manage distressing hallucinations, while robotic companions reduce stress and loneliness in elderly patients (Garety et al., 2021; Pham et al., 2022; Nwoye et al., 2024). Additionally, AI supports caregivers by monitoring changes in mood and behaviour, enhancing patient care and alleviating caregiver burden (Tutun et al., 2023).
AI technologies are revolutionizing mental health care by leveraging advanced algorithms for diagnosis, treatment, and management. Machine learning (ML), including supervised, unsupervised, and reinforcement learning, enables the analysis of patient data to diagnose conditions like schizophrenia, anxiety, and depression, while deep learning (DL) processes neuroimaging data to identify biomarkers (Thakkar et al., 2024; LeCun et al., 2015). Natural language processing (NLP) aids mental health assessment by analyzing speech and text for emotional cues and powering chatbots for therapy (Thakkar et al., 2024; Nag et al., 2023). Reinforcement learning is used in personalised therapy, such as virtual reality exposure for management of anxiety (Graham et al., 2019), while computer vision enhances emotional state assessment and supports children with autism through robotic interventions (Fiske et al., 2019; Pham et al., 2022). Voice computing detects mood disorders via speech analysis, achieving high diagnostic accuracy (Bedi et al., 2015; Taguchi et al., 2018). Wearable devices and physiological signals like heart rate, skin conductance, and sleep patterns provide insights into conditions like anxiety and depression, complemented by VR/AR-based tools and AI wearables like Google Glass for social skill enhancement (Long et al., 2022; Voss et al., 2019). Social media analysis predicts mood fluctuations, while mobile apps democratise mental health care with over 10,000 options available (Cummins et al., 2020; Youper, 2023). Despite challenges in integration and data reliability, AI continues to improve accessibility and personalization in mental health interventions.
AI algorithms are transforming mental health care by enabling early diagnosis, personalised treatment, and continuous management. Artificial Neural Networks (ANNs) like EMPaSchiz have achieved 87% accuracy in diagnosing schizophrenia using functional Magnetic Resonance Imagining (fMRI) data, surpassing traditional methods (Kalmady et al., 2019). Machine learning (ML) and natural language processing (NLP) models have classified PTSD with 82% accuracy and depression with varying accuracy (70–95%) based on datasets and algorithms (Le Glaz et al., 2021). Techniques like support vector machines (SVMs), convolutional neural networks (CNNs), and ensemble models effectively detect cognitive disorders like bipolar disorder and schizophrenia through neuroimaging and physiological markers such as electroencephalogram (EEG) and heart rate variability (HRV) (Cummins et al., 2020; de Bardeci et al., 2021).
AI-driven apps analyze text and social media data for predicting relapses and mood changes (Abdullah et al., 2016), while wearable sensors monitor real-time physiological changes for condition management (Long et al., 2022). Novel approaches like the complex probabilistic hesitant fuzzy N-soft set (CPHFNSS) enhance diagnostic precision by integrating expert input and addressing uncertainty, particularly in resource-constrained settings (Ashraf et al., 2023). As research advances, AI's role in mental health care promises increasingly effective and accessible interventions for diverse populations.
With this, there is clear evidence of rising public interest in AI for mental health, as demonstrated by a 114% increase in related online searches (Banerjee et al., 2024). These AI technologies are now being applied to detect, classify, and monitor mental health conditions with greater accuracy and efficiency than traditional methods. However, despite the rising interest in AI-driven mental health tools, there remain significant gaps and challenges in the field that necessitate further research and comprehensive methodological review of AI technologies in mental health disorders. This study uses a methodological approach that includes evidence-based analysis to review multiple mental health disorders of ASD, schizophrenia, depression, anxiety, bipolar disorder, and PTSD. This research includes a data visualisation and narrative synthesis of the results including the observed challenges and limitations of the AI technologies in the diagnosis, prognosis, treatment, and management of the specified mental health disorders.
Methods
Comprehensive searches were conducted in databases including PubMed and Google Scholar. Keywords and phrases such as "Artificial Intelligence", "AI", "mental health disorders", "mental health", "schizophrenia", "autism", “bipolar disorder”, "anxiety", "depression", "PTSD", "psychosis", and "mental illness", "artificial intelligence in mental health," "machine learning for mental disorders," "AI-based therapy," and "digital mental health" were utilized to capture relevant studies. Boolean operators (AND, OR) were applied to refine search results, and the database search yielded a total of 168 papers. Afterwards, articles were screened to identify and remove duplicate or irrelevant articles. Duplicates were checked by comparing the DOI numbers and article titles; they were also confirmed using Mendeley version 2.124.0. Articles were first selected through title screening and then evaluated based on the inclusion and exclusion criteria. If the abstract did not provide enough information to determine eligibility, a full-text review was performed. The literature selected for the review was based on the predefined inclusion and exclusion criteria, which ensured that only relevant studies were reviewed. Inclusion Criteria specified that only peer-reviewed articles published in English between 2010 and 2024 were selected. Selected articles also had to focus explicitly on AI applications for mental health assessment, diagnosis, therapy, or risk prediction. Exclusion criteria included non-English, non-empirical studies, opinion pieces, and those unrelated to the mental health disorders of choice. The selected studies further underwent quality assurance using the Critical Appraisal Skills Programme (CASP) to ensure they were credible and relevant. After this process, 40 papers were finally selected for inclusion in the review.
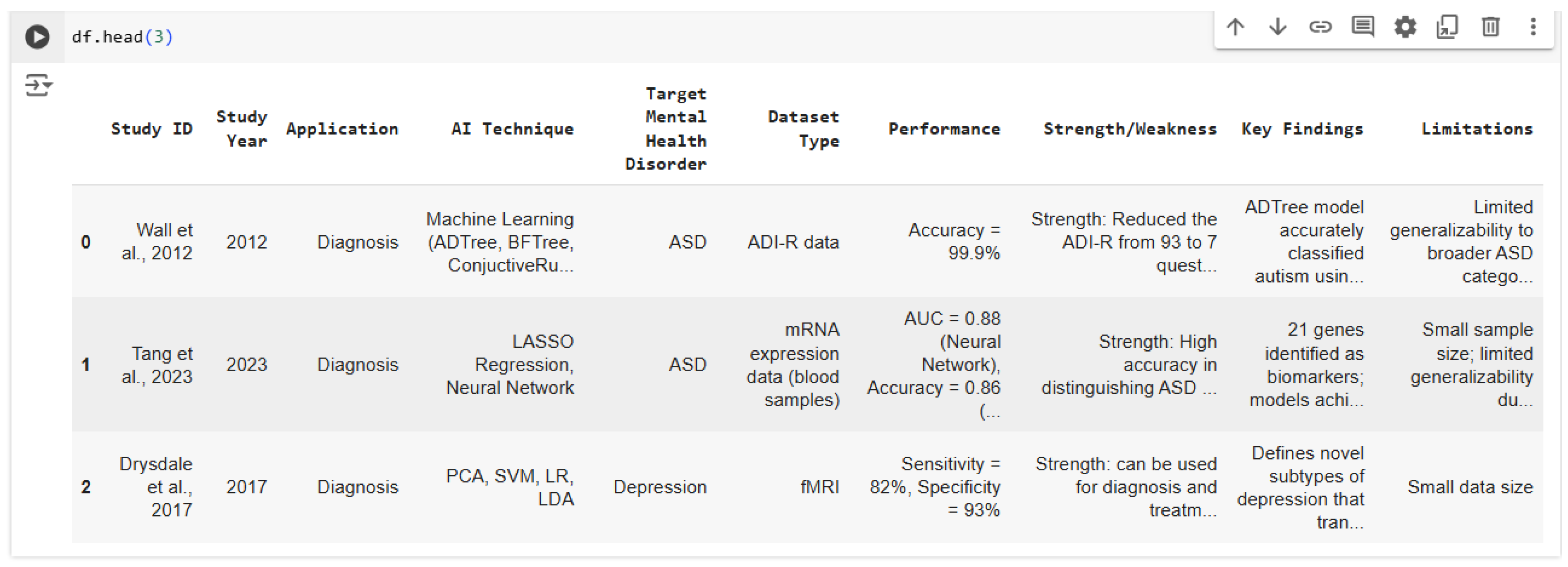
Data points extracted from the selected studies included study ID, study year, application, AI technique, target mental health disorder, dataset type, performance, strength/weakness, key findings, and limitations.
Figure 1.
Image of the first 3 rows of the data extracted.
Figure 1.
Image of the first 3 rows of the data extracted.
The data analysis involved a mixed-methods approach, combining both descriptive statistics and qualitative analysis. Descriptive statistics were used to summarise the study characteristics, AI tools used, and mental health outcomes. Python was utilised to analyse the studies based on the distribution of AI tools/models applied to specific mental disorders and the application areas of AI (diagnosis, treatment, or management). The qualitative analysis involved a thematic synthesis approach to explore the effectiveness of AI interventions for mental health disorders, challenges in implementing AI technologies in clinical settings, as well as recommendations and future research directions for AI in mental health care. The thematic analysis also helped identify common themes, key patterns, and trends across the included studies.
Results
This section discusses the result of a methodological review of AI technologies in the diagnosis, treatment, and management of ASD, schizophrenia, depression, anxiety, bipolar disorder, and PTSD. A variety of AI models, tools, and algorithms have shown promise in improving the diagnosis and management of mental health conditions.
Across studies, Supervised Machine Learning (SML) emerged as the most used AI technique. Common AI algorithms applied to mental health include Naives Bayes, SVM, Long Short-Term Memory (LSTM), Random Forest (RF), CNN, ANN, Logistic Regression (LR), DT, Recurrent Neural Network (RNN), KNN, and Principal component analysis (PCA). These algorithms are used to predict or classify symptoms of mental health conditions by analysing data from a variety of sources, including neuroimaging (Magnetic Resonance Imaging- MRI, fMRI, Electroencephalogram- EEG) and body signals.
For mental health detection, systems often include wearable devices composed of sensors, data acquisition tools, data pre-processing, feature extraction, and machine learning models for mental health condition classification. Filtering algorithms such as wavelet transforms and Kalman filters are frequently employed to remove noise from data, ensuring higher accuracy in detecting mental health issues. Additionally, data evaluation metrics such as root mean square (RMS), mean, root mean square error (RMSE), standard deviation (SD), and interquartile range (IQR) help in feature extraction and model performance evaluation.
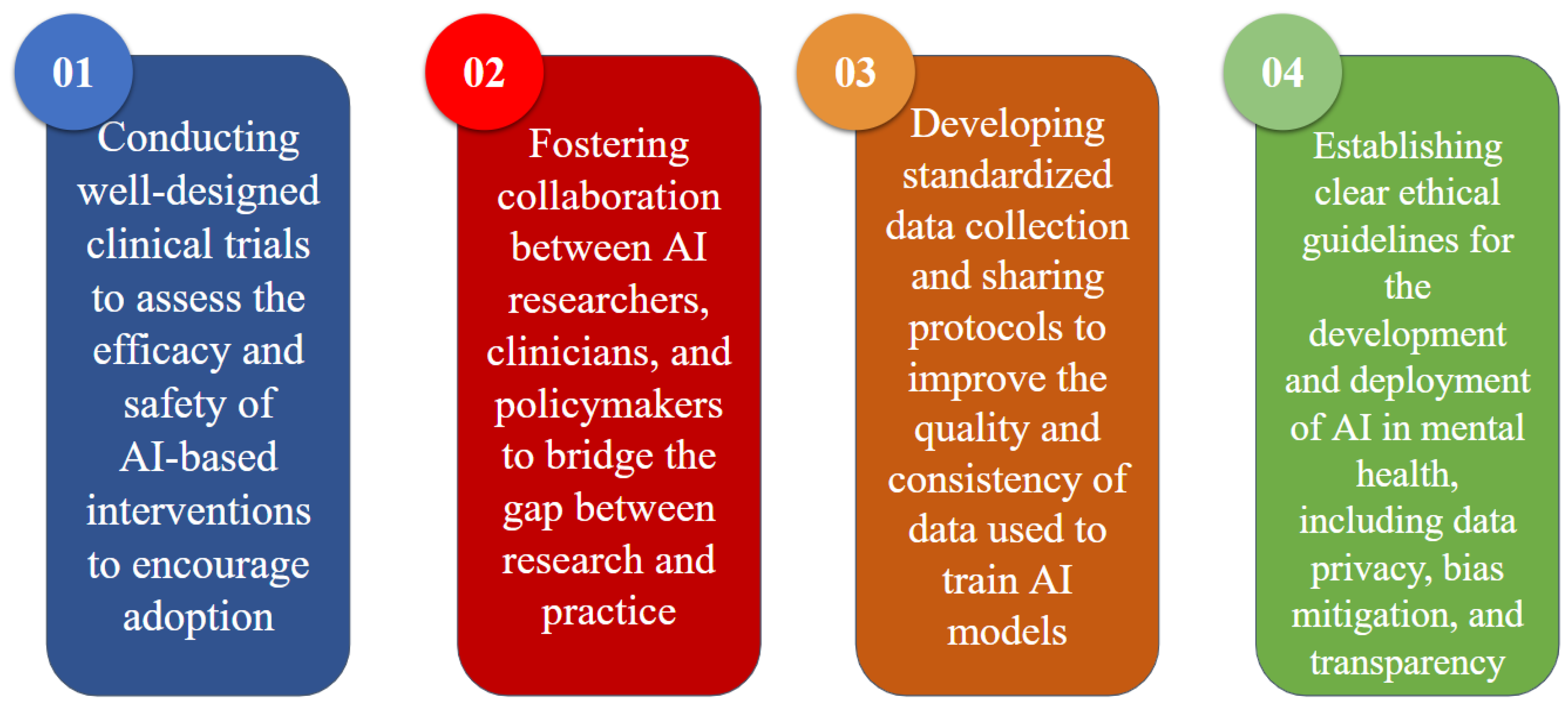
In
Figure 2 below each segment represents a specific AI technique, and the percentages indicate the proportion of studies utilising each method. The presence of multiple models within some studies accounts for the cumulative percentage.
SVM is used in 19.8% of the studies, making it one of the most frequently applied techniques. SVM's popularity can be attributed to its robustness and effectiveness in classification tasks, particularly with smaller datasets and structured data.
CNNs representing 17.3%, are widely applied in studies involving imaging data such as MRI and fMRI scans, where they excel at pattern recognition within complex, high-dimensional data. The frequent use of CNN highlights the importance of visual data in mental health research.
LR and RF account for 9.9% and 8.6% of studies, respectively. Logistic Regression is commonly used due to its simplicity and interpretability, especially in binary classification tasks, while Random Forest is valued for its capability to handle non-linear relationships and reduce overfitting through ensembling.
ANN which constitute 7.4% of the studies, are favoured for their ability to capture complex patterns in both structured and unstructured data. DT used in 11.1% of studies, provide an interpretable model structure, making them suitable for cases where understanding the decision-making process is essential.
Less commonly used techniques include KNN and LSTM networks, each representing 2.5% of the total studies. KNN is typically employed for simpler, lower-dimensional data, while LSTM networks are particularly useful for time-series data, which might explain their limited but specific use cases in mental health studies.
The "Others" category, making up 21% of the studies, encompasses a range of less common techniques such as multilayer perceptron (MLP), Fuzzy Synchronisation Likelihood (FSL), Hierarchical Hidden Markov Models (HMM), Graphical Neural Networks (GNN), Linear Discriminant Analysis (LDA), SustaIn, Kalman filtering, JRip, SimpleCART, ensembling methods, and Naive Bayes. This diversity indicates that researchers are experimenting with a variety of models to address specific challenges in mental health research.
In summary, the chart reveals a preference for SVM, CNN, and other traditional machine learning methods, which are versatile and effective across multiple data types. The "Others" category reflects the ongoing exploration of newer and specialised models, suggesting that AI in mental health is both mature in some areas and evolving in others as researchers continue to experiment with a broader range of techniques.
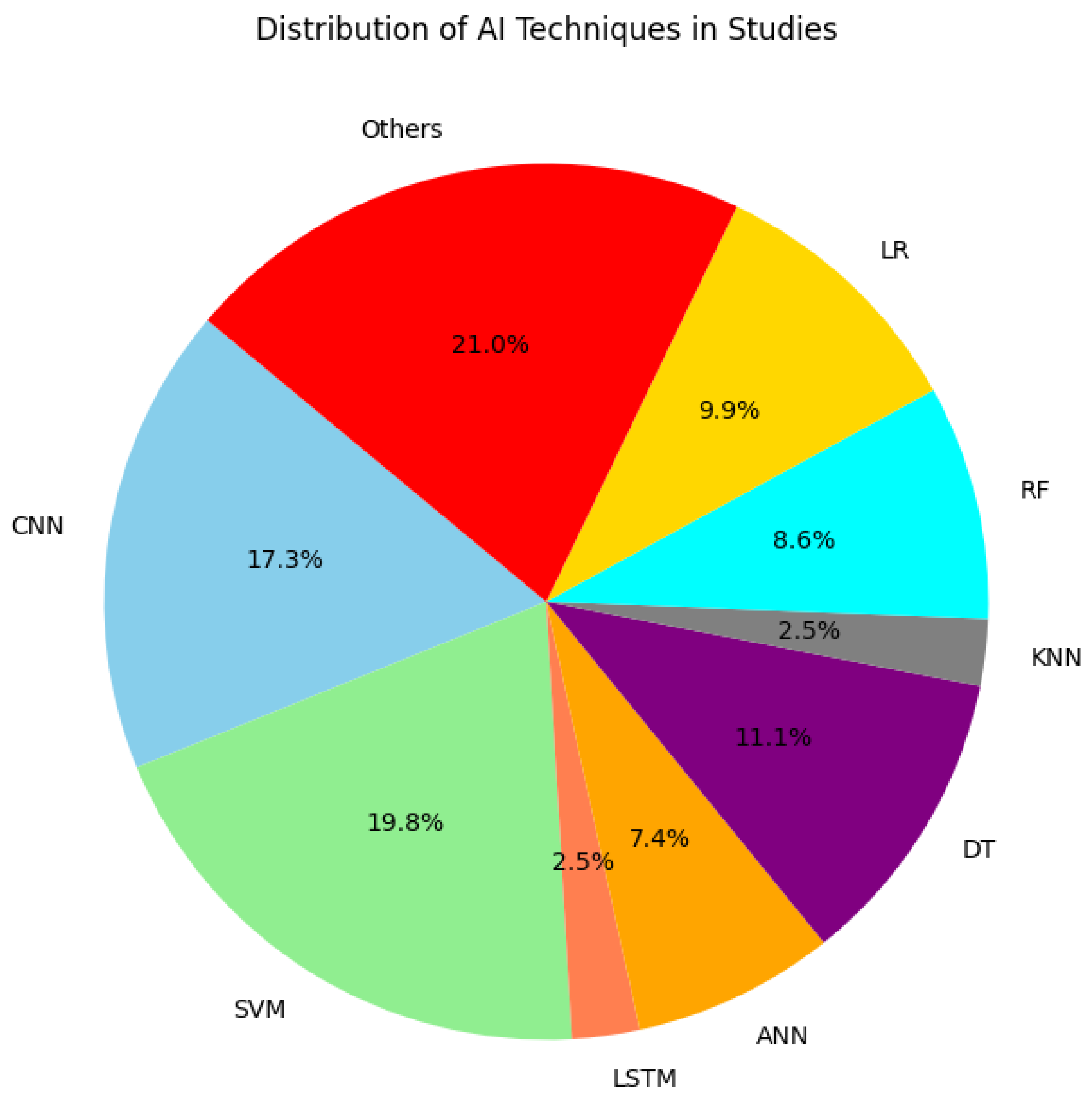
Figure 3 below shows the magnitude of the different application areas of AI in mental health, based on the studies included in this research. More studies focused on the application of AI for Diagnosis, with 25 studies categorised in this area. This suggests that AI's capacity to identify and diagnose mental health disorders has been a significant focus for researchers. This may be because diagnosis is the first step in solution finding. There are also discrepancies in the traditional method of diagnosis hence, necessitating the heavy employment of AI techniques in diagnosing mental health disorders. For instance, schizophrenia has no ascertained markers for identification. Diagnosis requires a physician’s assessment which is time-consuming and can delay advancement in assisting the individual because it is after diagnosis that intervention may occur.
The areas of treatment and prognosis are also explored, but to a lesser extent, with both areas represented in around 3 and 7 studies respectively. This indicates an interest in AI's potential to aid in therapeutic interventions and in predicting the outcomes of mental health conditions over time. The category of management is also represented, with only 6 studies examining how AI can be employed to manage ongoing mental health care, hinting at an emerging field that may require more research attention. Overall, the chart reflects a strong emphasis on diagnostic capabilities, with comparatively less but notable research in AI-driven treatment, prognosis, and management in mental health.
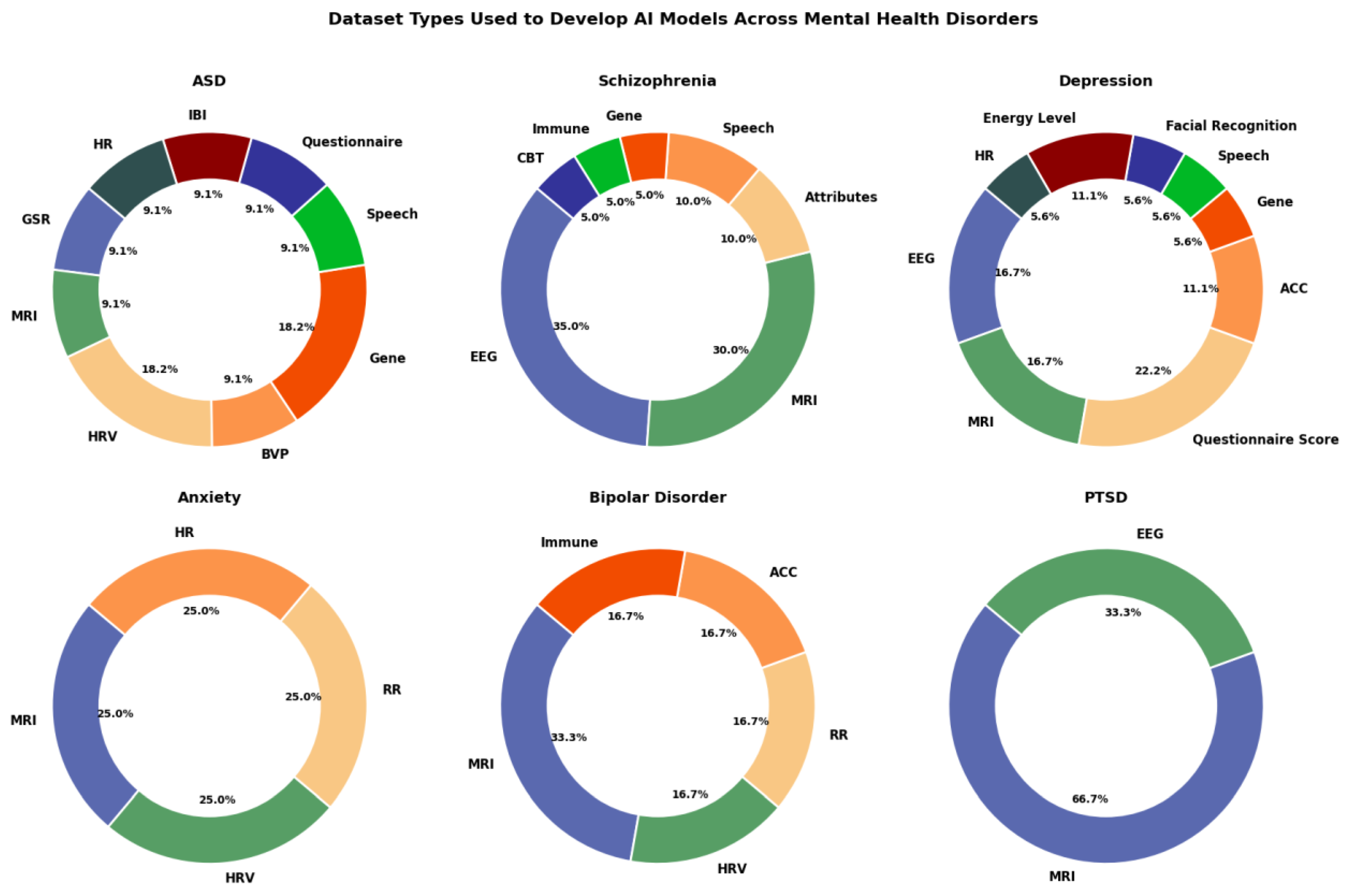
Figure 4 below depicts a series of doughnut charts illustrating the types of datasets used in AI model development across different mental health disorders, with each disorder represented by a separate chart. The charts are segmented by the variety of dataset types, such as EEG, MRI, genetic data, and questionnaire scores, reflecting the focus of AI models within each disorder.
For ASD, the dataset types are quite varied, including Galvanic Skin Response (GSR), MRI, Heart Rate Variability (HRV), Blood Volume Pulse (BVP), Gene data, Speech, Questionnaire, Interbeat-Interval (IBI), and Heart Rate (HR). The largest portions come from Gene data and MRI, each comprising 18.2% of the datasets used, indicating a balanced approach with no single dataset type dominating the research.
Schizophrenia shows a strong preference for EEG and MRI data, which make up 35% and 30% respectively, followed by smaller contributions from Attributes, Speech, Gene, Immune, and CBT data types. The emphasis on EEG and MRI suggests a reliance on brain activity and structural imaging for modelling schizophrenia.
In Depression studies, there is also diversity in data sources, with EEG and MRI accounting for 16.7% each, and Questionnaire scores comprising 22.2%. Other dataset types such as ACC, Gene, Speech, Facial Recognition, Energy Level, and HR are used to a lesser extent. This variety indicates that depression research leverages both biological and self-reported data.
For Anxiety, the data sources are equally distributed among MRI, HRV, Respiratory Rate (RR), and HR, each constituting 25% of the total. This suggests that AI models for anxiety rely on physiological data with no dataset type dominating.
Bipolar Disorder primarily uses MRI data (33.3%), with smaller segments from HRV, RR, ACC, and Immune datasets. The focus on MRI highlights the importance of imaging data, although there is moderate diversity in other data types used.
Lastly, PTSD research is mostly reliant on MRI (66.7%), with EEG data accounting for the remaining 33.3%. This heavy reliance on MRI suggests that PTSD studies predominantly use imaging data to model the disorder, with EEG playing a secondary role.
In summary, the charts show a varied approach to dataset utilisation across mental health disorders, with some conditions like Schizophrenia and Depression using a broader mix of data types. Disorders such as PTSD and Bipolar Disorder lean more heavily on MRI data, while Anxiety research shows a more balanced use of physiological data sources. This visualisation highlights the diversity and specialisation in AI model development based on the unique data needs of each mental health disorder.
This section details the observation from the reviewed studies, on the potential, challenges, and how accurately various AI models can improve the diagnosis, treatment, management, or prognosis of mental health conditions. For instance, AI-based models like ML and Deep Neural Network (DNN) classifiers have been applied to neuroimaging data to predict the onset of mental health disorders such as schizophrenia, depression, and PTSD. Studies focused on ASD generally achieve high accuracy, often between 85% and 95%, especially when using imaging data like MRI and fMRI. CNNs are the most effective in this area because of their strong performance with high-dimensional imaging data. CNNs and DNNs tend to yield the highest accuracy for ASD detection, and in studies where multimodal data (e.g., combining imaging and genetic information) is used, models can reach accuracies above 90%. While model accuracy is high, generalizability remains a concern due to limited dataset diversity. Most high-performing ASD studies rely on data from specific populations, which may limit the model's performance when applied to broader populations.
The accuracy of models for schizophrenia detection and prediction ranges widely but generally falls between 80% and 90%, highly dependent on the dataset type, with EEG and fMRI data showing better results. CNNs, RNN, SVM, and LSTM algorithms perform well in this domain, with CNNs applied to brain imaging data often achieving accuracies of 85% to 90%. LSTMs' capability of analysing time-series data is frequently used with EEG data, yielding moderate to high accuracy. Schizophrenia models, however, often face issues with interpretability, and due to the complex nature of schizophrenia, models may struggle with subtle variations in symptoms across patients, which can affect accuracy.
Studies on depression tend to show moderate accuracy, generally ranging from 70% to 85%, likely due to the reliance on structured or self-reported data, which can be more subjective. Traditional ML models such as LR, DT, and SVMs perform reasonably well, especially when trained on structured data, such as clinical questionnaire responses. CNNs and RNNs are also used with imaging and sequential data, achieving slightly higher accuracy, particularly when fMRI data is utilised. The subjective nature of depression assessments and the lack of objective biomarkers pose difficulties in achieving high accuracy consistently. Similarly, smaller sample sizes in depression studies limit the performance of more complex AI models.
AI models for anxiety disorders commonly achieve accuracies ranging from 70% to 85%. Models analysing self-reported questionnaires or behavioural data tend to have lower accuracy, while those using imaging data (fMRI) achieve slightly higher accuracy. SVMs, DTs, and RF models are frequently used with structured data, such as clinical interviews and self-reported scales, achieving moderate accuracy. CNNs have shown promise in studies that use imaging data, reaching accuracy levels closer to the upper end of the range. Similar to depression, the subjective nature of self-reported data affects accuracy, and the overlapping symptoms between anxiety and other mental health disorders make it harder for models to achieve high accuracy.
Bipolar disorder studies generally report lower accuracies, typically between 65% and 80%, probably because of the episodic character of the disorder and the difficulty in capturing consistent symptoms. Ensemble models and SVMs are commonly used for bipolar disorder studies, with moderate success. When combined with genetic data or imaging data, CNNs and RNNs have shown a potential to improve accuracy, though they are less frequently applied. The cyclical nature of bipolar disorder and its overlap with symptoms of other disorders, like depression, can reduce the accuracy of AI models. Additionally, sample sizes in bipolar studies are often smaller, limiting model training.
PTSD is an area with low study availability in this research. This disorder relies heavily on subjective data thus, has moderate to lower accuracy. PTSD's symptom variability and subjective nature of data impact model performance. However, one notable success is the use of the CNN model in processing fMRI data for predicting PTSD trajectories. The model attained a high accuracy of 88.6% at the first time point. Although a bit lower than some disorders which can be due to limited data size, leading to challenges in model validation. It is further aggravated by the disorder’s diverse symptom presentations and reliance on subjective reports which further reduce model accuracy.
Overall, disorders like ASD and Schizophrenia achieve the highest accuracies, particularly with CNNs and other deep-learning models that work well with imaging data. Depression and Anxiety show moderate accuracy due to their reliance on structured or self-reported data, which is less objective, making traditional ML models like DT and SVM more commonly used. Bipolar Disorder has lower accuracy compared to other disorders, likely due to the episodic nature of the disorder and symptom variability, which complicates model training and prediction, posing unique challenges for AI models. The performance trends indicate that the highest accuracies are achieved in disorders where objective data, such as imaging, is available, like ASD and Schizophrenia, while disorders relying heavily on subjective data, like Depression and Anxiety, tend to have moderate accuracy. However, it may seem that immune-based ML models have proven effective in distinguishing schizophrenia and bipolar disorder from healthy controls, with an area under the curve (AUC) of up to 0.804 in detecting diagnostic patterns through immune markers. These AI interventions improve diagnostic precision and offer non-invasive diagnostic options, such as the use of biomarkers in schizophrenia detection, which reduces the need for more intrusive methods. Furthermore, AI models are shown to augment treatment by predicting treatment outcomes based on genetic and biological data, opening the door for more personalised and targeted therapies. Improving model accuracy across disorders will likely require more diverse datasets, combining multimodal data, and more objective biomarkers where available.
Table 1.
Summary of the analysis of model accuracy by disorders.
Table 1.
Summary of the analysis of model accuracy by disorders.
| Mental Health Disorder |
Model Accuracy Range |
Best-Performing Models |
Limitations |
| Autism Spectrum Disorder (ASD) |
85% - 95%
|
CNN, DNN
|
High accuracy but limited generalizability due to dataset diversity. Studies often rely on specific populations, limiting model performance in broader applications. |
| Schizophrenia |
80% - 90%
|
CNN, SVM, RNN (LSTM)
|
Interpretability issues and complexity due to symptom variations across patients can affect accuracy. |
| Depression |
70% - 85% |
SVM, Logistic Regression (LR), Decision Tree, CNN, RNN |
High variability in accuracy due to subjective assessments and limited objective biomarkers. Small sample sizes limit complex AI model performance. |
| Anxiety Disorders |
70% - 85% |
SVM, Decision Tree, Random Forest, CNN |
Subjectivity in self-reported data affects accuracy, and overlapping symptoms with other disorders make it challenging to achieve high accuracy. |
| Bipolar Disorder |
65% - 80% |
Ensemble Models, SVM, CNN, RNN |
Lower accuracy due to the episodic nature of the disorder and symptom overlap with other conditions, such as depression. Small sample sizes limit model training. |
| Post-Traumatic Stress Disorder (PTSD) |
65% - 80% |
CNN, RNN, Ensemble Models |
Limited studies are available, leading to challenges in model validation. Diverse symptom presentations and reliance on subjective reports reduce model accuracy. |
Diagnostic Applications: Several studies demonstrated the use of AI for diagnosing mental health conditions like depression, anxiety, and schizophrenia. Machine learning algorithms trained on multimodal data, including voice, text, wearable device outputs, and clinical records, achieved high diagnostic accuracy (75-90%). For example:
Natural language processing (NLP) algorithms analyzed linguistic patterns to detect depression with over 85% accuracy.
Speech analysis tools identified markers of anxiety disorders based on prosody and tone changes.
Physiological data, such as heart rate variability captured via wearable devices, supported the detection of post-traumatic stress disorder (PTSD).
These tools offer promise for early and remote diagnosis, addressing limitations in traditional methods such as subjective clinician assessments.
Predictive Models: AI-based predictive models have shown proficiency in forecasting mental health crises. Examples of this include:
Predictive analytics on electronic health records (EHRs) achieve an 85% accuracy rate in identifying suicide risk.
Integration of social media data to detect patterns indicative of mood swings or self-harm ideation.
Predictive tools that combine historical data with current user behaviour, enabling proactive interventions.
These models underscore AI’s role in preemptive care, enhancing clinicians' ability to allocate resources effectively.
Therapeutic Interventions: AI-powered tools for therapy have expanded access to mental health care. Some highlighted interventions include:
Chatbots such as Woebot, Schizobot, and Wysa deliver evidence-based cognitive behavioral therapy (CBT) through user-friendly interfaces.
Virtual reality (VR) environments combined with AI to treat phobias and anxiety by simulating controlled exposure scenarios.
Personalized treatment recommendations based on AI-driven analysis of patient progress and feedback.
Clinical trials have demonstrated these tools’ efficacy, with significant improvements in self-reported mental health metrics observed within weeks of use.
Discussion
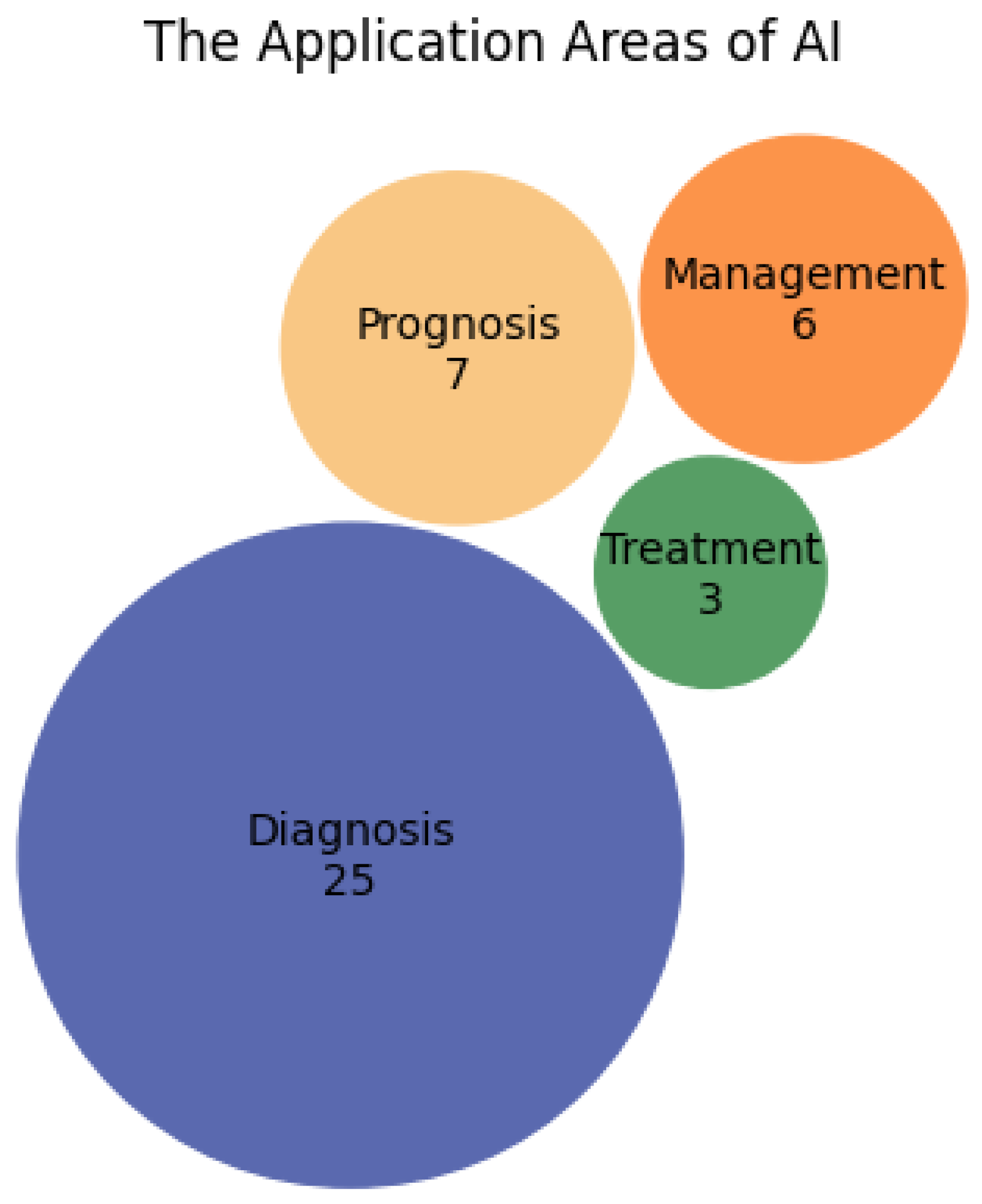
The strengths of AI in mental health lie in its usage in addressing critical gaps in mental health care delivery by enabling scalable, cost-efficient, and personalized interventions. For instance, chatbots address stigma by providing anonymity. Predictive tools facilitate timely interventions, potentially averting crises. Automated systems mitigate stigma and ensure continuity of care, particularly for populations with limited access to mental health professionals. Other identified technologies range from AI-based decision support systems, AI-powered eye movement analysis, autoantibody-based biomarkers, Personal sensing, AI-driven virtual companions and therapeutic avatars, AI-powered alert systems, AI-powered apps such as conversational agents (e.g chatbots), to automated speech analysis. By leveraging big data, AI systems uncover patterns unobservable to human practitioners, advancing precision medicine in mental health. However, despite these advancements, challenges persist. Majorly, data privacy and ethical concerns hinder large-scale adoption, with sensitive mental health information requiring robust protections. Algorithms often lack transparency due to explainability and the black box effect, raising questions about accountability and complicating clinician trust and adoption. Moreover, most AI models are trained on limited datasets, affecting their generalizability across diverse populations. The ethical implications of AI’s decision-making autonomy in critical areas such as suicide prevention also necessitate scrutiny. To overcome these barriers, addressing the identified challenges, and limitations and establishing regulatory frameworks are critical steps in realising the full prospect of AI in this field. Future research should focus on improving dataset diversity, model interpretability, and ethical governance guaranteeing that AI technologies in mental health are both effective and equitable. Future studies should also prioritise the development of explainable AI models that allow clinicians to understand the rationale behind diagnostic predictions. Ensuring that AI tools are interpretable will enhance trust among healthcare providers and patients alike. Furthermore, standardising data sets across neuroimaging and clinical studies is essential to improve the generalizability of AI models. Multicenter collaborations that employ standardised data collection techniques that are then deposited into a general data bank accessible to researchers globally can provide larger, more diverse datasets, improving the robustness and clinical applicability of AI interventions. The integration of multimodal data (e.g., combining genetic, behavioural, and neuroimaging data) is another area where future research can focus. By leveraging multiple data sources, AI models can offer a more holistic approach to achieve mental health diagnosis precision, prognosis, personalised treatment, and management techniques, as seen in studies that utilised a combination of fMRI, EEG, and genetic data for schizophrenia and PTSD prediction. Also, robust policies ensuring data privacy and ethical AI deployment are non-negotiable. Collaborative research involving interdisciplinary teams can enhance model robustness. Additionally, incorporating cultural sensitivity in AI designs can improve applicability in global contexts. Interdisciplinary collaboration between technologists, clinicians, and policymakers is vital to overcoming these challenges and advancing AI’s integration into mental health care.
Figure 5.
Summary of the recommendations.
Figure 5.
Summary of the recommendations.
In conclusion, while this research has its limitations in the number of studies used, it has been able to draw conclusions across board from the studies used, critically examining the reason for the lapses between research and clinical practice. This research has contributed to the advancing body of knowledge by systematically reviewing the current AI technologies, identifying research gaps, and providing recommendations to improve the robustness, reliability, and ethical implementation of AI in mental health care. With the global burden of mental health disorders continuing to rise, AI offers a promising solution to alleviate the pressure on healthcare systems. It is without doubt that AI is reshaping mental health care through innovative diagnostic, predictive, and therapeutic tools. Addressing current limitations in data diversity, transparency, and ethical, technical, and implementation challenges is essential for sustainable integration into mainstream care. Ongoing research and collaboration will be critical to ensuring sustainable and equitable advancements in this field. Future research should focus on developing transparent, adaptable, and user-centric AI models.
References
- Abdullah, S., Matthews, M., Frank, E., Doherty, G., Gay, G., & Choudhury, T. (2016). Automatic detection of social rhythms in bipolar disorder. Journal of the American Medical Informatics Association, 23(5), 538–543. [CrossRef]
- Ashraf, S., Kousar, M., & Chambashi, G. (2023). Identification of mental disorders in South Africa using complex probabilistic hesitant fuzzy N-soft aggregation information. Scientific Reports, 13(1). [CrossRef]
- Banerjee, S.; Dunn, P.; Conard, S.; Ali, A. Mental Health Applications of Generative AI and Large Language Modeling in the United States. Int. J. Environ. Res. Public Health 2024, 21, 910. [CrossRef]
- Bedi, G., Carrillo, F., Cecchi, G. A., Slezak, D. F., Sigman, M., Mota, N. B., & Corcoran, C. M. (2015). Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophrenia, 1(1), 15030. [CrossRef]
- Cianconi, P., Betrò, S., & Janiri, L. (2020). The impact of climate change on mental health: A systematic descriptive review. Frontiers in Psychiatry. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7068211/.
- Corcoran, C. M., & Cecchi, G. A. (2020). Using language processing and speech analysis for the identification of psychosis and other disorders. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 5(8), 770–779. [CrossRef]
- Cummins, N., Matcham, F., Klapper, J., & Schuller, B. (2020). Artificial intelligence to aid the detection of mood disorders. In D. Barh (Ed.), Artificial Intelligence in Precision Health (pp. 231–255). Academic Press.
- de Bardeci M, Ip CT, Olbrich S. (2021). Deep learning applied to electroencephalogram data in mental disorders: A systematic review. Biol Psychol. May;162:108117. Epub 2021 May 13. [CrossRef] [PubMed]
- Fadele, K. P., Igwe, S. C., Toluwalogo, N.-O., Udokang, E. I., Ogaya, J. B., & Lucero-Prisno, D. E. (2024). Mental health challenges in Nigeria: Bridging the gap between demand and resources. Cambridge Prisms: Global Mental Health, 11. [CrossRef]
- Fiske, A., Henningsen, P., & Buyx, A. (2019). Your robot therapist will see you now: Ethical implications of embodied artificial intelligence in psychiatry, psychology, and psychotherapy. Journal of Medical Internet Research, 21(5), e13216. [CrossRef]
- Garety, P., et al. (2021). Optimizing AVATAR Therapy for people who hear distressing voices: Study protocol for the AVATAR2 multi-centre randomized controlled trial. Trials, 22(1), 366–6. [CrossRef]
- GBD 2019 Mental Disorders Collaborators. (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet Psychiatry, 9(2), 137–150. [CrossRef]
- Graham, S., Depp, C., Lee, E. E., Nebeker, C., Tu, X., & Kim, H. C. (2019). Artificial intelligence for mental health and mental illnesses: An overview. Current Psychiatry Reports, 21(1), 1–18. [CrossRef]
- Gureje, O., Chisholm, D., Kola, L., Lasebikan, V., & Saxena, S. (2015). Cost-effectiveness of an essential mental health intervention package in Nigeria. World Psychiatry, 14(1), 1–8.
- Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. [CrossRef]
- Kalmady, S. V., Venkatasubramanian, G., Gangadhar, B. N., Ganesan, V., & Srinivasan, N. (2019). EMPaSchiz—Ensemble algorithm with multiple parcellations for schizophrenia prediction using resting state fMRI. NeuroImage: Clinical, 22, 101761. [CrossRef]
- LeCun, Y., Bengio, Y., & Hinton, G. (2015). Deep learning. Nature, 521(7553), 436–444. 521, 7553, 436–444. [CrossRef]
- Le Glaz A, Haralambous Y, Kim-Dufor DH, Lenca P, Billot R, Ryan TC, Marsh J, DeVylder J, Walter M, Berrouiguet S, Lemey C. Machine Learning and Natural Language Processing in Mental Health: Systematic Review. J Med Internet Res. 2021 May 4;23(5):e15708. [CrossRef] [PubMed] [PubMed Central]
- Long, J., Lei, Y., Peng, L., Xu, P., & Mao, P. (2022). Machine learning algorithms for mental health detection: A review. Journal of Medical Systems, 46(6), 1–13. [CrossRef]
- McCarthy, J. 1959. "Programs with Common Sense" at the Wayback Machine (archived October 4, 2013). In Proceedings of the Teddington Conference on the Mechanisation of Thought Processes, 756–91. London: Her Majesty's Stationery Office. From https://web.archive.org/web/20130512112201/http://www-formal.stanford.edu/jmc/mcc59.html. (Last accessed 28/10/2024).
- Minerva, F., & Giubilini, A. (2023). Is AI the future of mental healthcare? Topoi, 1-9. [CrossRef]
- Möller, H. J. (2016). The relevance of negative symptoms in schizophrenia and how to treat them with psychopharmaceuticals? Psychiatria Danubina, 28(4), 435–440.
- Nag, A., et al. (2023). AI-driven chatbots for mental health: A review. Journal of Internet Medical Research, 25, e32029. [CrossRef]
- Nwoye, E., Muslehat, A.A., Umeh, C., Okodeh, S.O., & Woo, W.L. (2024). SchizoBot: Delivering Cognitive Behavioural Therapy for Augmented Management of Schizophrenia. Digital Technologies Research and Applications. [CrossRef]
- Nwoye, E., Woo, W. L., Fidelis, O., Umeh, C., & Gao, B. (2020). Improved Schizophrenia Diagnosis. Int J Auto AI Mach Learn, 1(1), 17–41.
- Pham, T., et al. (2022). AI-driven robot companions for psychiatric outcomes. Journal of Mental Health and Well-being, 14(3), 112–128.
- Taguchi, T., Tachikawa, H., & Nemoto, K. (2018). Major depressive disorder discrimination using vocal acoustic features. Journal of Affective Disorders, 225, 214–220. [CrossRef]
- van Erp, T. G., Hibar, D. P., Rasmussen, J. M., Glahn, D. C., Pearlson, G. D., Andreassen, O. A., & Thompson, P. M. (2018). Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Molecular Psychiatry, 21(4), 547-553. [CrossRef]
- World Health Organization. (2004). Promoting mental health: Concepts, emerging evidence, practice summary report. World Health Organization.
- World Health Organization. (2019). Mental disorders. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
- World Health Organization. (2022). Mental health interventions and strategies. World Health Organization.
- Thakkar, A., Gupta, A., & De Sousa, A. (2024). Artificial intelligence in positive mental health: A narrative review. Frontiers in Digital Health, 6, 1280235. [CrossRef]
- The Lancet Global Health. (2020). Mental health matters. The Lancet Global Health, 8(11), e1352. [CrossRef]
- Tutun, S., Johnson, M. E., Ahmed, A., Albizri, A., Irgil, S., & Yesilkaya, I. (2023). An AI-based decision support system for predicting mental health disorders. Information Systems Frontiers, 25, 1261-1276. [CrossRef]
- Voss, C., Schwartz, J., Daniels, J., Kline, A., Haber, N., Washington, P., Tariq, Q., Robinson, T. N., Desai, M., Phillips, J. M., Feinstein, C., Winograd, T., & Wall, D. P. (2019). Effect of wearable digital intervention for improving socialization in children with autism spectrum disorder: A randomized clinical trial. JAMA Pediatrics, 173(5), 446–454. [CrossRef]
- Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. [CrossRef]
- Youper. (2023). Acceptability and effectiveness of artificial intelligence therapy for anxiety and depression: Longitudinal observational study. Retrieved from https://youper.com.
- Zheng, Z., Zheng, P., & Zou, X. (2021). Peripheral blood S100B levels in autism spectrum disorder: A systematic review and meta-analysis. Journal of Autism and Developmental Disorders, 51(8), 2569–2577. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).