Submitted:
22 May 2025
Posted:
25 May 2025
You are already at the latest version
Abstract
Keywords:
Introduction
- the distance between the probe and target nerve;
- the cryoprobe diameter;
- the size of the resulting ice ball;
- the temperature of the immediately surrounding tissue (such as blood, which acts as a heat sink);
- the rate and duration of cold application. The latter two factors are highly dependent upon the gas flow rate and the number of ‘freeze cycles’ applied, usually with 2–3 min of freezing followed by 0.5–2 min of thawing.[9]
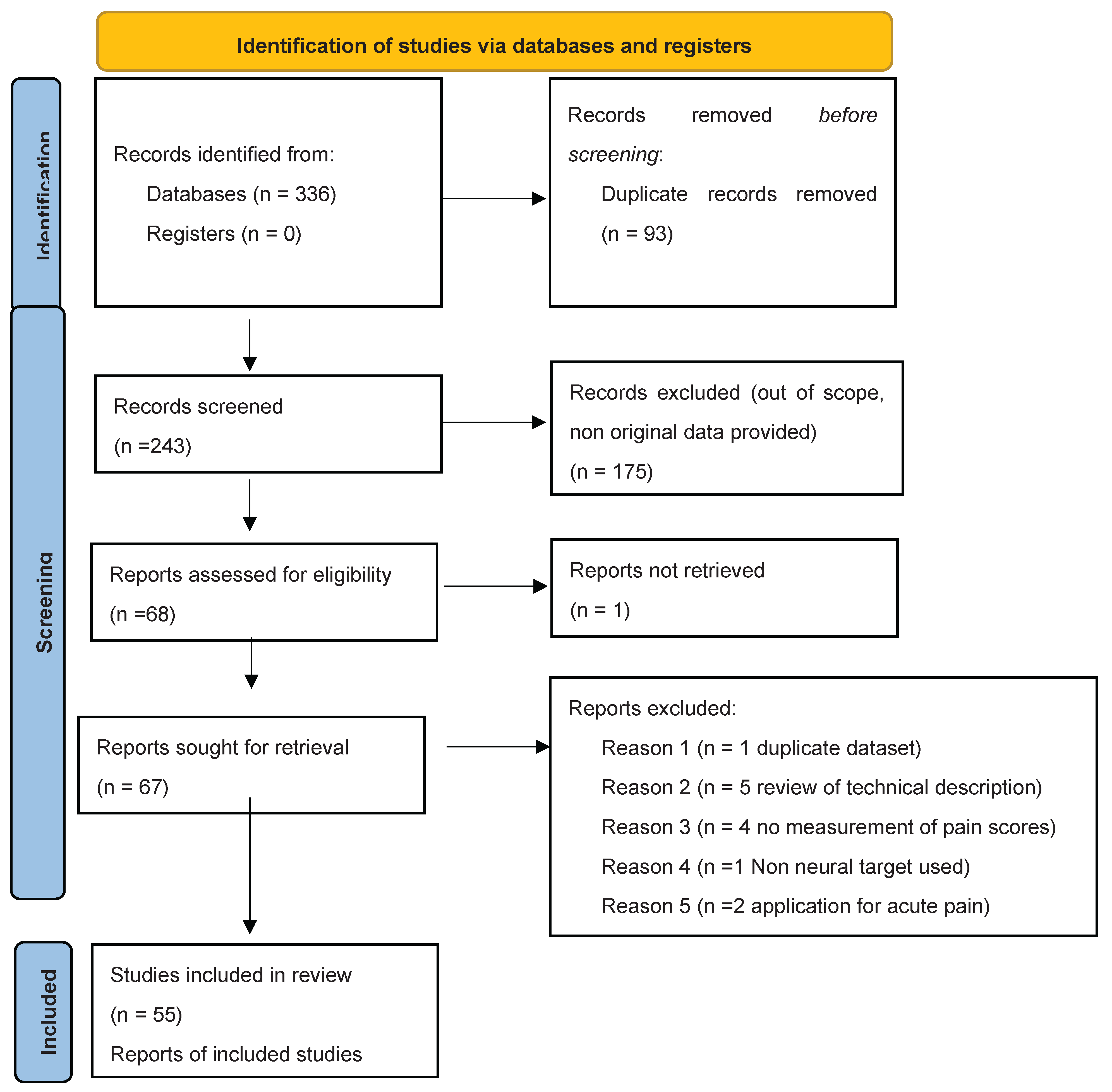
Materials and Methods
Results
Discussion
Conclusion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Werner MU, Kongsgaard UE. I. Defining persistent post-surgical pain: is an update required? Br J Anaesth. 2014;113(1):1-4. [CrossRef]
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. [CrossRef]
- Baker PN, Van Der Meulen JH, Lewsey J, Gregg PJ. The role of pain and function in determining patient satisfaction after total knee replacement: DATA FROM THE NATIONAL JOINT REGISTRY FOR ENGLAND AND WALES. J Bone Joint Surg Br. 2007;89-B(7):893-900. [CrossRef]
- Wylde V, Beswick A, Bruce J, Blom A, Howells N, Gooberman-Hill R. Chronic pain after total knee arthroplasty. EFORT Open Rev. 2018;3(8):461-470. [CrossRef]
- Panagopoulos A, Tsiplakos P, Katsanos K, Antzoulas P, Lakoumentas J. Cooled radiofrequency ablation versus cryoneurolysis of the genicular nerves for the symptomatic pain management in knee osteoarthritis: a study protocol of a prospective, randomized, single-blinded clinical trial. J Orthop Surg. 2023;18(1):295. [CrossRef]
- Slavin BR, Markowitz MI, Klifto KM, Prologo FJ, Taghioff SM, Dellon AL. Cryoanalgesia: Review with Respect to Peripheral Nerve. J Reconstr Microsurg. 2024;40(04):302-310. [CrossRef]
- Wong J, Bremer N, Weyker PD, Webb CAJ. Ultrasound-Guided Genicular Nerve Thermal Radiofrequency Ablation for Chronic Knee Pain. Case Rep Anesthesiol. 2016;2016:1-3. [CrossRef]
- Ilfeld BM, Finneran JJ. Cryoneurolysis and Percutaneous Peripheral Nerve Stimulation to Treat Acute Pain: A Narrative Review. Anesthesiology. 2020;133(5):1127-1149. [CrossRef]
- Ilfeld BM, Gabriel RA, Trescot AM. Ultrasound-guided percutaneous cryoneurolysis for treatment of acute pain: could cryoanalgesia replace continuous peripheral nerve blocks? Br J Anaesth. 2017;119(4):709-712. [CrossRef]
- Radnovich R, Scott D, Patel AT, et al. Cryoneurolysis to treat the pain and symptoms of knee osteoarthritis: a multicenter, randomized, double-blind, sham-controlled trial. Osteoarthritis Cartilage. 2017;25(8):1247-1256. [CrossRef]
- Truong K, Meier K, Ahrens LC, et al. Cryoneurolysis versus radiofrequency ablation outcome on pain experience in chronic low back pain (COPE): a single-blinded randomised controlled trial. RMD Open. 2024;10(2):e004196. [CrossRef]
- Ilfeld BM, Smith CR, Turan A, et al. Ultrasound-guided Percutaneous Cryoneurolysis to Treat Chronic Postamputation Phantom Limb Pain: A Multicenter Randomized Controlled Trial. Anesthesiology. 2023;138(1):82-97. [CrossRef]
- Kvarstein G, Högström H, Allen SM, Rosland JH. Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study. Scand J Pain. 2019;20(1):39-50. [CrossRef]
- Grigsby E, Radnovich R, Nalamachu S. Efficacy and Safety of Cryoneurolysis for Treatment of Chronic Head Pain Secondary to Occipital Neuralgia: A Pilot Study. Local Reg Anesth. 2021;Volume 14:125-132. [CrossRef]
- Perry TA, Segal NA. An open-label, single-arm trial of cryoneurolysis for improvements in pain, activities of daily living and quality of life in patients with symptomatic ankle osteoarthritis. Osteoarthr Cartil Open. 2022;4(3):100272. [CrossRef]
- Yoon JHE, Grechushkin V, Chaudhry A, Bhattacharji P, Durkin B, Moore W. Cryoneurolysis in Patients with Refractory Chronic Peripheral Neuropathic Pain. J Vasc Interv Radiol. 2016;27(2):239-243. [CrossRef]
- Zhan C, Yoon J, Baghai Kermani A, Gupta A, Moore W. Abstract No. 587 Safety and efficacy of computed tomography–guided percutaneous cryoneurolysis for chronic intercostal pain syndrome. J Vasc Interv Radiol. 2020;31(3):S256. [CrossRef]
- Das G, Das S, Sahoo R, Shreyas S, Kanthi B, Sharma VS. Efficacy of cryoneurolysis versus intra-articular steroid in sacroiliac joint pain: A retrospective, case-control study. Indian J Anaesth. 2023;67(11):1004-1008. [CrossRef]
- Sidebottom AJ, Carey EC, Madahar AK. Cryoanalgesia in the management of intractable pain in the temporomandibular joint: a five-year retrospective review. Br J Oral Maxillofac Surg. 2011;49(8):653-656. [CrossRef]
- Prologo JD, Gilliland CA, Miller M, et al. Percutaneous Image-Guided Cryoablation for the Treatment of Phantom Limb Pain in Amputees: A Pilot Study. J Vasc Interv Radiol. 2017;28(1):24-34.e4. [CrossRef]
- Department of Radiology, University of Missouri Columbia, One Hospital Drive, Columbia, United States, University of Missouri Columbia School of Medicine, One Hospital Drive, Columbia, United States, Yasin J, et al. CT-guided cryoablation for post-thoracotomy pain syndrome: a retrospective analysis. Diagn Interv Radiol. 2020;26(1):53-57. [CrossRef]
- Moore W, Kolnick D, Tan J, Yu HS. CT Guided Percutaneous Cryoneurolysis for Post Thoracotomy Pain Syndrome. Acad Radiol. 2010;17(5):603-606. [CrossRef]
- Wolter T, Deininger M, Hubbe U, Mohadjer M, Knoeller S. Cryoneurolysis for zygapophyseal joint pain: a retrospective analysis of 117 interventions. Acta Neurochir (Wien). 2011;153(5):1011-1019. [CrossRef]
- Kim CH, Hu W, Gao J, Dragan K, Whealton T, Julian C. Cryoablation for the treatment of occipital neuralgia. Pain Physician. 2015;18(3):E363-368.
- Nemecek Z, Sturm C, Rauen AC, Reisig F, Streitberger K, Harnik MA. Ultrasound-Controlled Cryoneurolysis for Peripheral Mononeuropathies: A Retrospective Cohort Study. Pain Manag. 2023;13(6):363-372. [CrossRef]
- Parekattil S, Gudeloglu A, Ergun O, Galante A, Etafy M, Mendelson R. MP31-10 A COST EFFECTIVE OFFICE BASED TECHNIQUE FOR ULTRASOUND GUIDED PERI-SPERMATIC CORD CRYOABLATION FOR CHRONIC SCROTAL CONTENT PAIN. J Urol. 2021;206(Supplement 3). [CrossRef]
- Tinnirello A. Genicular nerves ablation for chronic knee pain: A single-center retrospective evaluation comparing four ablation modalities. Pain Pract. 2020;20(S1):7-95. [CrossRef]
- Nezami N, Behi A, Manyapu S, et al. Percutaneous CT-Guided Cryoneurolysis of the Intercostobrachial Nerve for Management of Postmastectomy Pain Syndrome. J Vasc Interv Radiol. 2023;34(5):807-813. [CrossRef]
- McLean BC, Nguyen CD, Newman DP. Cryoablation of the Infrapatellar Branch of the Saphenous Nerve Identified by Non-Invasive Peripheral Nerve Stimulator for the Treatment of Non-Surgical Anterior Knee Pain: A Case Series and Review of the Literature. Cureus. Published online June 21, 2020. [CrossRef]
- Calixte N, Kartal IG, Tojuola B, et al. Salvage Ultrasound-guided Targeted Cryoablation of The Perispermatic Cord For Persistent Chronic Scrotal Content Pain After Microsurgical Denervation Of The Spermatic Cord. Urology. 2019;130:181-185. [CrossRef]
- Bellini M, Barbieri M. Percutaneous cryoanalgesia in pain management: a case-series. Anestezjol Intensywna Ter. 2015;47(2):131-133. [CrossRef]
- Prologo J, Mittal A, Knight J, Hsu D, Dolan R, Com D. Percutaneous CT-guided cryoablation for the management of pudendal neuralgia: Long-Term outcomes. J Vasc Interv Radiol. 2018;29(4):S241-2.
- Bianco GL, D’angelo FP, Dos Santos GF, et al. Genicular Nerve Ultrasound-Guided Cryoanalgesia for the Treatment of Chronic Knee Joint Pain: An Observational Retrospective Study. Pain Ther. Published online March 27, 2025. [CrossRef]
- Filipovski I, Gabriel RA, Kestenholz R. Ultrasound-Guided Cryoneurolysis for the Treatment of Painful Diabetic Neuropathy of the Foot: A Case Series. Cureus. Published online March 16, 2024. [CrossRef]
- Stogicza AR, Peng P. Cryoanalgesia for shoulder pain: a motor-sparing approach to rotator cuff disease. Reg Anesth Pain Med. 2022;47(9):576-580. [CrossRef]
- Dalili D, Ahlawat S, Rashidi A, Belzberg AJ, Fritz J. Cryoanalgesia of the anterior femoral cutaneous nerve (AFCN) for the treatment of neuropathy-mediated anterior thigh pain: anatomy and technical description. Skeletal Radiol. 2021;50(6):1227-1236. [CrossRef]
- Moesker AA, Karl HW, Trescot AM. Treatment of Phantom Limb Pain by Cryoneurolysis of the Amputated Nerve. Pain Pract. 2014;14(1):52-56. [CrossRef]
- Sahoo RK, Das G, Pathak L, Dutta D, Roy C, Bhatia A. Cryoneurolysis of Innervation to Sacroiliac Joints: Technical Description and Initial Results—A Case Series. AA Pract. 2021;15(4):e01427. [CrossRef]
- Mendes-Andrade I, Pagan-Rosado R, Ferreira-Silva N, Hurdle MF. A novel approach to refractory coccydynia: ultrasound- fluoroscopy-guided cryoablation of sacrococcygeal nerve. Pain Manag. 2024;14(10-11):541-547. [CrossRef]
- Shaffer JP, Williams VB, Shin SS. Cryoneurolysis for Digital Neuralgia in Professional Baseball Players: A Case Series. Orthop J Sports Med. 2022;10(5):23259671221096095. [CrossRef]
- Gabriel RA, Kestenholz R, Filipovski I. Repeated Ultrasound-Guided Percutaneous Intercostal Cryoneurolysis for the Management of Chronic Postmastectomy Pain Syndrome: A Case Report. AA Pract. 2024;18(3):e01764. [CrossRef]
- Cachemaille M, Geering S, Broome M. Cryoneurolysis of alveolar nerves for chronic dental pain: A new technique and a case series. Pain Pract. 2023;23(7):851-854. [CrossRef]
- Kočan L, Rapčan R, Sudzina R, et al. Radiofrequency denervation and cryoablation of the lumbar zygapophysial joints in the treatment of positive lumbar facet joint syndrome – a report of three cases. Radiol Case Rep. 2022;17(12):4515-4520. [CrossRef]
- Connelly NR, Malik A, Madabushi L, Gibson C. Use of ultrasound-guided cryotherapy for the management of chronic pain states. J Clin Anesth. 2013;25(8):634-636. [CrossRef]
- Matelich B, Berg A, Habeck J, Hutchins J. B32 Ultrasound-guided cryoneurolysis of the supra scapular nerve for chronic shoulder pain: a case series. In: Ultrasound Guided RA (UGRA). BMJ Publishing Group Ltd; 2022:A99.1-A99. [CrossRef]
- Fox S. Pudendal nerve cryoablation for chronic pelvic pain. Dis Colon Rectum. 2019;62(6):e39-e401. [CrossRef]
- Sarridou D, Papadopoulou D, Paraskevopoulos T, Stavropoulou E. Successful treatment of complex regional pain syndrome type 1 of upper limb with cryoneurolysis of the stellate ganglion: A rare case report. Pain Pract. 2022;22(2):285-287. [CrossRef]
- Ramsook R, Spinner D. (468) Cryoablation of a hip disarticulation residual limb neuroma allowing for ambulation and pain relief: a case report. J Pain. 2016;17(4):S91. [CrossRef]
- Joshi DH, Thawait GK, Del Grande F, Fritz J. MRI-guided cryoablation of the posterior femoral cutaneous nerve for the treatment of neuropathy-mediated sitting pain. Skeletal Radiol. 2017;46(7):983-987. [CrossRef]
- Kalava A, Pham K, Okon S. Cryoneurolysis of the Subcostal Nerve: A Technical Description and Case Report. Cureus. Published online April 3, 2024. [CrossRef]
- Sen S, De Haan JB, Mehrafza M, Hernandez N. Ultrasound-Guided Percutaneous Intercostal Cryoneurolysis for Acute-on-Chronic Pain in CLOVES Syndrome. Cureus. Published online January 22, 2023. [CrossRef]
- Jung EY, Lee SS. Treatment of chronic mini-thoracotomy wound pain and lung herniation with intercostal cryoablation and surgical mesh repair: a case report. J Cardiothorac Surg. 2024;19(1):348. [CrossRef]
- MacRae F, Speirs A, Bursuc A, Hashemi M, Winston P. A Case Report of Cryoneurolysis for Dorsal Foot Pain and Toe Clawing in a Patient With Multiple Sclerosis. Arch Rehabil Res Clin Transl. 2023;5(3):100286. [CrossRef]
- Perese J, Oswald J, Gabriel RA. Ultrasound-Guided Percutaneous Cryoneurolysis for Post-Thoracotomy Pain Syndrome: A Case Report. Cureus. Published online December 23, 2022. [CrossRef]
- Koethe Y, Mannes AJ, Wood BJ. Image-guided Nerve Cryoablation for Post-thoracotomy Pain Syndrome. Cardiovasc Intervent Radiol. 2014;37(3):843-846. [CrossRef]
- Rhame EE, DeBonet AF, Simopoulos TT. Ultrasonographic Guidance and Characterization of Cryoanalgesic Lesions in Treating a Case of Refractory Sural Neuroma. Case Rep Anesthesiol. 2011;2011:1-4. [CrossRef]
- MacRae F, Boissonnault E, Hashemi M, Winston P. Bilateral Suprascapular Nerve Cryoneurolysis for Pain Associated With Glenohumeral Osteoarthritis: A Case Report. Arch Rehabil Res Clin Transl. 2023;5(1):100256. [CrossRef]
- Weber G, Saad K, Awad M, Wong TH. Case Report Of Cryoneurolysis For The Treatment Of Refractory Intercostobrachial Neuralgia With Postherpetic Neuralgia. Local Reg Anesth. 2019;Volume 12:103-107. [CrossRef]
- Yarmohammadi H, Nakamoto D, Azar N, Hayek S, Haaga J. Percutaneous computed tomography guided cryoablation of the celiac plexus as an alternative treatment for intractable pain caused by pancreatic cancer. J Cancer Res Ther. 2011;7(4):481. [CrossRef]
- Rupp A, Panchang P, Smith M. A case report of cryoablation for chronic shoulder pain due to osteoarthritis. Interv Pain Med. 2022;1(4):100146. [CrossRef]
- Kalava A, Kassie R, Borick E. Cryoneurolysis of Intercostal Nerves for Postherpetic Neuralgia: A Case Report. Cureus. Published online September 30, 2024. [CrossRef]
- Hampton H, Kalava A. Ischiorectal Approach to Cryoablation of the Pudendal Nerve Using a Handheld Device: A Report of Two Cases. Cureus. Published online August 30, 2023. [CrossRef]
- Fiala M, Azariah A, Woo J, Aal AKA, Levey A. Treating phantom limb pain: cryoablation of the posterior tibial nerve. Radiol Case Rep. 2022;17(9):3168-3171. [CrossRef]
- Gabriel RA, Finneran JJ, Trescot AM, Ilfeld BM. Ultrasound-Guided Percutaneous Cryoneurolysis for Postoperative Analgesia After Limb Amputation: A Case Series. AA Pract. 2019;12(7):231-234. [CrossRef]
- Davis T, Loudermilk E, DePalma M, et al. Twelve-month analgesia and rescue, by cooled radiofrequency ablation treatment of osteoarthritic knee pain: results from a prospective, multicenter, randomized, cross-over trial. Reg Anesth Pain Med. 2019;44(4):499-506. [CrossRef]
- Santi C, Haag T, Cooke C, Schatman M, Tinnirello A. Two-Centre Retrospective Analysis on Selective Sensory Denervation of Shoulder Joint by Means of Cooled Radiofrequency in Chronic Shoulder Pain. J Pain Res. 2024;Volume 17:3139-3150. [CrossRef]
- Klessinger S, Casser HR, Gillner S, et al. Radiofrequency Denervation of the Spine and the Sacroiliac Joint: A Systematic Review based on the Grades of Recommendations, Assesment, Development, and Evaluation Approach Resulting in a German National Guideline. Glob Spine J. 2024;14(7):2124-2154. [CrossRef]
- Cahani D, Chacko J, Hahn B. Myonecrosis: A Rare Complication of Cryoneurolysis. J Emerg Med. 2019;57(3):e73-e76. [CrossRef]
- Fleischmann E, Lenhardt R, Kurz A, et al. Nitrous oxide and risk of surgical wound infection: a randomised trial. The Lancet. 2005;366(9491):1101-1107. [CrossRef]

| Author, Year | Design | Patients | Targets | Guidance | Follow Up | Outcomes | Notes |
| Radnovich, 2017[10] |
RCT vs Sham | 180 | Saphenous Nerve | Landmark |
120 days | 87.5% responders at 120 days (VAS reduction > 50%) | 61.2% responders in the sham group at 120 days No adverse events |
| Truong, 2024[11] | RCT vs Sham and RF | 120 | Lumbar medial branch | Fluoroscopic | 6 months | No improvement compared to RF or Placebo | |
| Ilfeld, 2023[12] | RCT vs Sham |
144 | Sciatic (post amputation pain) | US | 4 months | No improvement compared to Placebo | |
| Kvarstein, 2019[13] | RCT Vs Steroid Injection | 52 | Occipital Nerve | US | 18 weeks | Pain relief > 50% in 35 % of patients (no difference) | |
| Grigsby, 2021[14] | OP | 26 | Occipital Nerve | Blind | 56 days | NRS reduction > 2 points in 35% of patients | |
| Perry, 2022[15] | OP | 40 | Sural, Saphenous, Superficial and/or Deep fibular nerves | US | 6 months | Mean NRS reduction 2.8 (< than 50% from baseline) | 22 patients completed follow up |
| Yoon,2016[16] |
OP | 22 | Peripheral neuropathy (mixed 3 plantar neuromas, 3 ileoinguinal, 4 posterior tibial, 7 saphenous, 1 gluteal, 1 sural, 1 genicular, 2 digital nerves) | US |
12 months | 3.2 mean VAS reduction at 12 months. Mean pain relief >50% at 3 months |
|
| Zhan, 2020[17] | OP | 18 | Intercostal | CT | 12 months | 2.3 and 1.3 mean VAS reduction at 6 and 9 months respectively | No significant reduction at 12 months |
| Das, 2023[18] | OR | 83 | Sacroiliac Joint | US | 6 Months | 69% patients with pain reief > 50% after 6 months | |
| Sidebottom, 2011[19] |
OR | 17 | TMJ (auricular nerve and TMJ capsule) | Surgical |
NS | Mean duration of pain relief 7 months, 3/17 patients were pain free at 12 months | 2 temporary numbness |
| Prologo,2017[20] | OR | 21 | Phantom Limb Neuroma | US | 194 ±99 Days | Mean NRS reduction 4.2 | |
| Yasin, 2019[21] | OR | 13 | Intercostal Nerves | CT |
Various, 2-18 months | 61.5% of patients with pain relief > 50% | 1 pneumothorax and 3 pseudohernia |
| Moore, 2010[22] | OR | 18 | Intercostal Nerves | CT | Variable (mean 51 days) | Mean Pain Relief <50% |
|
| Wolter, 2011[23] | OR | 91 | Lumbar Medial Branch | CT | 3 Months | Mean NRS decrease 3.50 points | |
| Kim, 2015[24] | OR | 38 | Occipital Nerve | Landmark | 6 Months | Mean NRS Improvement 3.8 | 2 post op neuritis and 1 haematoma |
| Nemecek, 2023 [25] | OR | 24 | Various (intercostal, saphenous, Peroneal, | US | 6 Months | Pain reduction > 30% in 2/24 Patients | |
| Parekattil, 2021[26] | OR | 35 | Genitofemoral, ilioinguinal and inferior hypogastric nerve |
Blind (surgical) | 1 month | Pain reduction > 50% in 68% of patients | |
| Tinnirello, 2020 [27] | OR | 10 | Genicular Nerves | US | 6 months | Pain relief >50% in 50% of patients at 6 months | |
| Nezami, 2022[28] | OR | 14 | Intercostobrachial nerve | CT | 6 months | Mean NRS decrease 2.9 | |
| McLean,2020[29] | OR | 23 | Saphenous nerve, Infrapatellar branch | Blind | Variable | Pain relief > 50% in all patients | Follow up at 6 months for 4 patients, NS for others. |
| Calixte, 2019[30] | OR | 279 | Genitofemoral, ilioinguinal and inferior hypogastric nerve |
Blind (Surgical) | 5 Years | Pain relief > 50% in 64% of patients | |
| Bellini, 2015[31] | OR | 18 | Facet, Knee, Sacroiliac Joint | 4 months | Mean NRS decrease 4/10 | ||
| Prologo, 2018[32] | OR | 14 | Pudendal Nerve | CT | 18 months | Responder rate 63% | Responder definition not stated |
| Lo Bianco, 2025 [33] | OR | 90 | Genicular nerves | US | 9 Months | Mean NRS 5±1 from 7±2 at Baseline | Pain relief > 50% in 56% of Patients at 3 months (NS at 9 Months) |
| Filipovski, 2024[34] | CS | 3 | Superficial peroneal nerve | US | 5 Years | 2 Patients pain free after 5 years, 1 without results | |
| Stogizka, 2024[35] | CS | 4 | Suprascapular, Axillary, Lateropectoral Nerves | US | 6 Months | 3 Patients with pain relief > 60% | |
| Dalili, 2021[36] |
CS | 3 | Anterior femoral cutaneous nerve | MRI |
12 months | 50% VAS reduction at 12 months in all patients | No adverse events |
| Moesker, 2014[37] |
CS | 5 | Phantom limb | US |
5-30 months | 60% of patients with > 50% pain relief | No adverse events |
| Sahoo, 2021[38] | CS | 5 | Lateral Branches of Sacral Dorsal Nerve Roots | US and Fluoro | 6 months | 100% of patients with > 50% pain relief | |
| Mendes-Andrade, 2024 [39] | CS | 2 | Sacrococcygeal Nerve | Fluoro | >50% pain relief in 100% of patients | ||
| Shaffer, 2022[40] | CS | 3 | Digital Nerves | US | 1 year | Pain Relief 100% | |
| Gabriel, 2024[41] | CR | 1 | Intercostal Nerves | US | |||
| Cachemaille, 2023[42] | CS | 4 | Alveolar Nerves | Blind | 3 months | Pain relief > 50% in 2 patients | |
| Kocân, 2022[43] | CS | 2 | Lumbar medial branches | Fluoroscopic | 6 months | Pain relief 50% at 3 months (<50% at 6 months, better result with RF) | 1 patient treated with RF, 2 with cryo |
| Connelly, 2013[44] | CS | 3 | Intercostal Nerves | US | Variable | Pain relief >50% in 2 patients for 9 months, in 1 patients for 3 months | |
| Matelich, 2022[45] | CS | 3 | Suprascapular Nerve | US | 3-6 months | Duration of pain relief 3-6 months | Pain scores not recorded |
| Fox, 2019[46] | CS | 3 | Pudendal Nerve | CT | NS | 2 Patients with > 50% pain relief | |
| Sarridou, 2022[47] | CR | 1 | Stellate Ganglion | US | 6 Months | Pain relief > 50% for 6 months | |
| Ramsook, 2016[48] | CR | 1 | Hip stump neuroma | US | NS | Pain relief | |
| Joshi, 2017[49] | CR | 1 | Posterior femoral cutaneous nerve | MRI | 5 months | Pain relief 100% at 6 months | |
| Kalava, 2024[50] | CR | 1 | Intercostal Nerves | CT | 3 months | 100% pain relief | |
| Sen, 2023[51] | CR | 1 | Intercostal Nerves | US | 5 days | Pain relief 100% | |
| Jung, 2024[52] | CR | 1 | Intercostal Nerves | Surgical | 8 weeks | Pain relief > 50% | |
| MacRae, 2023[53] | CR | 1 | Superficial Fibular Nerve | US | 5 months | Pain relief (no NRS reported) | |
| Perese, 2022[54] | CR | 1 | Intercostal Nerve | US | 2 months | Pain relief > 50% | |
| Koethe, 2014[55] | CR | 1 | Intercostal Nerves | CT | 8 weeks | Paine relief > 50% | |
| Rhame,2011 [56] |
CR | 1 | Sural Nerve | NS | 3 months | “Excellent pain relief” | |
| MacRae, 2023[57] | CR | 1 | Suprascapular Nerve | US | 7 Months | NRS < 2 | |
| Weber, 2019[58] | CR | 1 | Intercostobrachial Nerve | Blind | 1 Month | Pain relief >50% | |
| Yarmohammadi, 2011[59] | CR | 1 | Celiac Plexus | CT | 6 Months | Pain Relief 70% | |
| Rupp, 2022[60] | CR | 1 | Suprascapular Nerve | US | 3 months | Pain Relief > 50% | |
| Kalavla, 2024[61] | CR | 1 | Intercostal Nerves | US | 2 months | Pain relief > 50% | |
| Hampton, 2023[62] | CR | 2 | Pudendal Nerve | Blind | NS | Pain Relief for 3-4 Months | NRS not measured |
| Fiala, 2022[63] | CR | 1 | Phantom Limb Stump | US | NS | Pain relief < 6 weeks | |
| Gabriel, 2024[41] | CR | 1 | Intercostal Nerves | US | 6 Months | Pain relief >50% |
| Author, Year | Patients | Targets | Guidance | Positive outcome at 6 months |
| Truong, 2024[11] | 120 | Lumbar medial branch | Fluoroscopic | NO |
| Perry, 2022[15] | 40 | sural, saphenous, superficial and/or deep fibular nerves | US | NO |
| Yoon, 2016[16] |
22 | Peripheral neuropathy (mixed 3 plantar neuromas, 3 ileoinguinal, 4 posterior tibial, 7 saphenous, 1 gluteal, 1 sural, 1 genicular, 2 digital nerves) | US |
NO |
| Das, 2023[18] | 83 | Sacroiliac Joint | US | YES |
| Tinnirello, 2020 [27] | 10 | Genicular Nerves | US | YES |
| McLean, 2020[29] | 23 | Saphenous nerve, Infrapatellar branch | Blind | YES |
| Calixte, 2019[30] | 279 | Genitofemoral, ilioinguinal and inferior hypogastric |
Surgical | YES |
| Stogizka, 2024[35] | 4 | Suprascapular,Axillary, Lateropectoral | US | YES |
| Dalili, 2021 [36] |
3 | Anterior femoral cutaneous nerve | MRI |
YES |
| Moesker, 2014[37] |
5 | Phantom limb | US |
YES |
| Sahoo, 2021[38] | 5 | Lateral Branches of Sacral Dorsal Nerve Roots | US and Fluoroscopic | YES |
| Shaffer, 2022[40] | 3 | Digital Nerves | US | YES |
| Kocân, 2022[43] | 2 | Lumbar medial branches | Fluoroscopic | NO |
| Connelly, 2013[44] | 3 | Intercostal | US | YES |
| Sarridou, 2022[47] | 1 | Stellate Ganglion | US | YES |
| Yarmohammadi, 2011[59] | 1 | Celiac Plexus | CT | YES |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





