Submitted:
01 May 2025
Posted:
07 May 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Study Sample and Research Design
Ethics
Covariates
Assessment of Depression
Problem Definition
Machine Learning Workflow
Statistical Analysis
Results
Epidemiological Profile and Depression Prevalence among Subjects
Feature Selection
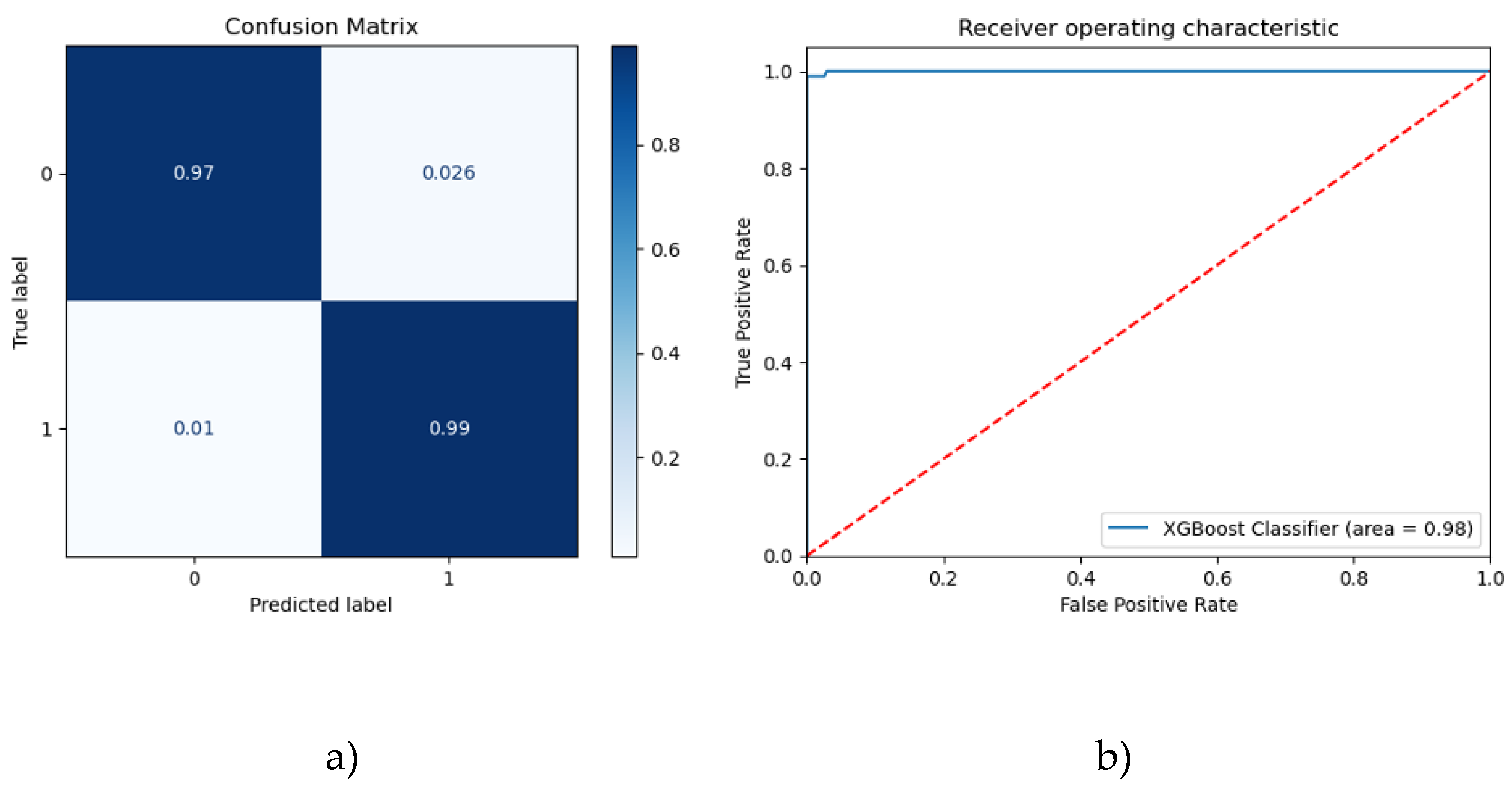
Testing Performance
Explainability
Discussion
Limitations
Future Directions
Conclusions
Author Contributions
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chand, S.P. ; Arif. H. Depression. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Sousa, R.D.; Henriques, A.R.; De Almeida, J.C.; Canhão, H.; Rodrigues, A.M. Unraveling Depressive symptomatology and risk factors in a changing world. Int. J. Environ. Res. Public Health 2023, 20, 6575. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.D.; Loncar, D. Projections of Global Mortality and Burden of Disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.D.; Huang, X.; Fox, K.R.; Franklin, J.C. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br. J. Psychiatry 2018, 212, 279–286. [Google Scholar] [CrossRef]
- Sobieraj, M.; Williams, J.; Marley, J.; Ryan, P. The impact of depression on the physical health of family members. Br. J. Gen. Pract. 1998, 48, 1653–1655. [Google Scholar]
- Nabeshima, T.; Kim, H. Involvement of Genetic and Environmental Factors in the Onset of Depression. Exp. Neurobiol. 2013, 22, 235–243. [Google Scholar] [CrossRef]
- Choi, R.Y.; Coyner, A.S.; Kalpathy-Cramer, J.; Chiang, M.F.; Campbell, J.P. Introduction to Machine Learning, Neural Networks, and Deep Learning. Transl. Vis. Sci. Technol. 2020, 9, 14. [Google Scholar]
- Schlick, T.; Wie, G-W. Machine learning tools advance biophysics. Biophys. J. 2024, 123, E1–E3. [Google Scholar] [CrossRef]
- Bi, Q.; Goodman, K.E.; Kaminsky, J.; Lessler, J. What is machine learning? A primer for the epidemiologist." Am. J. Epidemiol. 2019, 188, 2222–2239. [Google Scholar] [CrossRef]
- Swanson, K.; Wu, E. ; Zhang, A,; Alizadeh, A. A.; Zou, J. From patterns to patients: Advances in clinical machine learning for cancer diagnosis, prognosis, and treatment.” Cell 2023, 186, 1772–1791. [Google Scholar] [CrossRef]
- Ata, N.; Zahoor, I.; Hoda, N.; Adnan, S.M.; Vijayakumar, S.; Louis, F.; Poisson, L.; Rattan, R.; Kumar, N.; Cerghet, M.; Giri, S. Artificial neural network-based prediction of multiple sclerosis using blood-based metabolomics data. Mult. Scler. Relat. Disord. 2024, 92, 105942. [Google Scholar] [CrossRef]
- Egert, M.; Steward, J.E.; Sundaram, C.P. Machine Learning and Artificial Intelligence in Surgical Fields. Indian J. Surg. Oncol. 2020, 11, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Goyal, L.; Mallick, D.C.; Surani, S.R.; Kaushik, N.; Chandramohan, D.; Simhadri, P.K. Artificial Intelligence in Nephrology: Clinical Applications and Challenges. Kidney Medicine 2024, 7, 100927. [Google Scholar] [CrossRef]
- Chafai, N.; Bonizzi, L.; Botti, S.; Badaoui, B. Emerging applications of machine learning in genomic medicine and healthcare. Crit. Rev. Clin. Lab. Sci. 2024, 61, 140–163. [Google Scholar] [CrossRef]
- Calderone, A.; Latella, D.; Bonanno, M.; Quartarone, A.; Mojdehdehbaher, S.; Celesti, A.; Calabrò, R.S. Towards Transforming Neurorehabilitation: The Impact of Artificial intelligence on diagnosis and treatment of Neurological Disorders. Biomedicines 2024, 12, 2415. [Google Scholar] [CrossRef]
- Macpherson, T.; Churchland, A.; Sejnowski, T.; DiCarlo, J.; Kamitani, Y.; Takahashi, H.; Hikida, T. Natural and Artificial Intelligence: A brief introduction to the interplay between AI and neuroscience research. Neural Networks, 2021, 144, 603–613. [Google Scholar] [CrossRef]
- Lee, E.E.; Torous, J.; De Choudhury, M.; Depp, C.A.; Graham, S.A.; Kim, H.; Paulus, M.P.; Krystal, J.H.; Jeste, D.V. Artificial intelligence for Mental health care: clinical applications, barriers, facilitators, and artificial wisdom. Biol. Psychiatry: Cogn. Neurosci. Neuroimaging 2021, 6, 856–864. [Google Scholar] [CrossRef]
- Wickelgren, I. Why do so many mental illnesses overlap? Scientific American. Available online: https://www.scientificamerican.com/article/why-do-so-many-mental-illnesses-overlap/ (accessed on 23 April 2025 Year).
- Levkovich, I. Is artificial intelligence the next Co-Pilot for primary care in diagnosing and recommending treatments for depression? Med. Sci., 2025, 13, 8. [Google Scholar] [CrossRef]
- Mansoor, M.A.; Ansari, K.H. Early Detection of Mental Health Crises through Artifical-Intelligence-Powered Social Media Analysis: A Prospective Observational Study. J. Pers. Med. 2024, 14, 958. [Google Scholar] [CrossRef]
- Park, Y.; Park, S.; Lee, M. Effectiveness of artificial intelligence in detecting and managing depressive disorders: Systematic review. J. Affect. Disord. 2024, 361, 445–456. [Google Scholar] [CrossRef]
- Liu, X.; Jiang, K. Why is Diagnosing MDD Challenging? Shanghai Arch Psychiatry 2016, 28, 343–345. [Google Scholar] [CrossRef]
- Cuijpers, P.; Beekman, A.T.; Reynolds 3rd, C.F. Preventing depression: a global priority. JAMA 2012, 307, 1033–1034. [Google Scholar] [CrossRef] [PubMed]
- López Steinmetz, L.C.; Sison, M.; Zhumagambetov, R.; Godoy, J.C.; Haufe, S. Machine learning models predict the emergence of depression in Argentinean college students during periods of COVID-19 quarantine. Front. Psychiatry 2024, 15, 1376784. [Google Scholar] [CrossRef] [PubMed]
- Zafar, F.; Fakhare Alam, L.; Vivas, R.R.; Wang, J.; Whei, S.J.; Mehmood, S.; Sadeghzadegan, A.; Lakkimsetti, M.; Nazir, Z. The Role of Artificial Intelligence in Identifying Depression and Anxiety: A Comprehensive Literature Review. ” Cureus 2024, 16, e56472. [Google Scholar] [CrossRef] [PubMed]
- Serdari, A.; Manolis, A.; Tsiptsios, D.; Vorvolakos, T.; Terzoudi, A.; Nena, E.; Tsamakis, K.; Steiropoulos, P.; Tripsianis, G. Insight into the relationship between sleep characteristics and anxiety: a cross-sectional study in indigenous and minority populations in northeastern Greece. Psychiatry Res. 2020, 292, 113361. [Google Scholar] [CrossRef]
- Paparrigopoulos, T.; Tzavara, C.; Theleritis, C. Insomnia and its correlates in a representative sample of the Greek population. BMC Public Health 2010, 10, 531. [Google Scholar] [CrossRef]
- Touloumi, G.; Karakatsani, A.; Karakosta, A.; et al. National Survey of Morbidity and Risk Factors (EMENO): protocol for a Health Examination Survey representative of the Adult Greek Population. JMIR Res Protoc. 2019, 8, e10997. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Arvaniti, F.; Stefanadis, C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev. Med. 2006, 44, 335–340. [Google Scholar] [CrossRef]
- World Health Organization, (2000). The world heart: health systems: improving performance.
- Samakouri, M.; Bouhos, G.; Kadoglou, M.; Giantzelidou, A.; Tsolaki, K.; Livaditis, M. Standardization of the Greek version of Zung's Self-rating Anxiety Scale (SAS). Psychiatriki 2012, 23, 212–220. [Google Scholar]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch Gen Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Jemos, J. Beck Depression Inventory; validation in a Greek sample. Athens University Medical School, 1984.
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Tsara, V.E.; Serasli, E.V.; Amfilochiou, A.N. , Constantinidis, Th.; Christaki, P. Greek version of the Epworth Sleepiness Scale. Sleep Breath 2004, 8, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Kotronoulas, G.C.; Papadopoulou, C.N.; Papapetrou, A.N. , Patiraki E. Psychometric evaluation and feasibility of the Greek Pittsburgh sleep quality index (GR-PSQI) in patients with cancer receiving chemotherapy. Support Care Cancer 2011, 19, 1831–1840. [Google Scholar] [CrossRef] [PubMed]
- Lasa, L.; Ayuso-Mateos, J.L.; Vázquez-Barquero, J.L.; Díez-Manrique, F.J.; Dowrick, C.F. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J. Affect. Disord. 2000, 57, 261–265. [Google Scholar] [CrossRef]
- Trevisan, V.; Using SHAP values to explain how your machine learning model works. Medium. Available online: https://towardsdatascience.com/using-shap-values-to-explain-how-your-machine-learning-model-works-732b3f40e137 (accessed on 23 April 2025 Year).
- Kokaliari, E. Quality of life, anxiety, depression, and stress among adults in Greece following the global financial crisis. Int. Soc. Work 2016, 61, 410–424. [Google Scholar] [CrossRef]
- Papadopoulos, F.C.; Petridou, E.; Argyropoulou, S.; Kontaxakis, V.; Dessypris, N.; Anastasiou, A.; Katsiardani, K.P.; Trichopoulos, D.; Lyketsos, C. Prevalence and correlates of depression in late life: a population-based study from a rural Greek town. Int. J. Geriatr. Psychiatry 2005, 20, 350–357. [Google Scholar] [CrossRef]
- Edelstein, B.A.; Drozdick, L.W.; Ciliberti, C.M. Assessment of Depression and Bereavement in Older Adults. In Handbook of Assessment in Clinical Gerontology, 2nd ed.; Lichtenberg, P.A., Eds. 2003; pp. 3–43. www.sciencedirect.com/science/article/abs/pii/ B9780123749611100016.
- Bailey, R.K.; Mokonogho, J.; Kumar, A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr. Dis. Treat. 2019, 15, 603–609. [Google Scholar] [CrossRef]
- Brance, K.; Chatzimpyros, V.; Bentall, R.P. Increased social identification is linked with lower depressive and anxiety symptoms among ethnic minorities and migrants: A systematic review and meta-analysis. Clin. Psychol. Rev. 2023, 99, 102216. [Google Scholar] [CrossRef]
- Li, C.; Ning, G.; Wang, L.; Chen, F. More income, less depression? Revisiting the nonlinear and heterogeneous relationship between income and mental health. Front. Psychol. 2022, 13, 1016286. [Google Scholar] [CrossRef]
- Parra-Mujica, F.; Johnson, E.; Reed, H.; Cookson, R.; Johnson, M. Understanding the relationship between income and mental health among 16- to 24-year-olds: Analysis of 10 waves (2009-2020) of Understanding Society to enable modelling of income interventions. PloS one 2023, 18, e0279845. [Google Scholar] [CrossRef]
- Stylianidis, S.; Souliotis, K. The impact of the long-lasting socioeconomic crisis in Greece. ” BJPsych Int. 2019, 16, 16–18. [Google Scholar] [CrossRef]
- Bjelland, I.; Krokstad, S.; Mykletun, A.; Dahl, A.A.; Tell, G.S.; Tambs, K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc. Sci. Med. 2008, 66, 1334–1345. [Google Scholar] [CrossRef] [PubMed]
- Biswas, M.M. , Das, K.C., Sheikh, I. Psychological implications of unemployment among higher educated migrant youth in Kolkata City, India. Sci. Rep. 2024, 14, 10171. [Google Scholar] [CrossRef] [PubMed]
- Wittchen, H.U.; Kessler, R.C.; Pfister, H.; Höfler, M.; Lieb, R. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatr. Scand. 2000, 102, 14–23. [Google Scholar] [CrossRef]
- Tiller, J.W.G. Depression and anxiety. Med. J. Aust. 2013, 199, S28–S31. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Horn, P.J.; Wuyek, L.A. Anxiety disorders as a risk factor for subsequent depression. Int. J. Psychiatry Clin. Pract. 2010, 14, 244–247. [Google Scholar] [CrossRef]
- Jacobson, N.C.; Newman, M.G. Avoidance mediates the relationship between anxiety and depression over a decade later. J. Anxiety Disord. 2014, 28, 437–445. [Google Scholar] [CrossRef]
- McTeague, L.M.; Rosenberg, B.M.; Lopez, J.W.; Carreon, D.M.; Huemer, J.; Jiang, Y.; Chick, C.F.; Eickhoff, S.B.; Etkin, A. Identification of Common Neural Circuit Disruptions in Emotional Processing Across Psychiatric Disorders. Am. J. Psychiatry 2020, 177, 411–421. [Google Scholar] [CrossRef]
- Fava, M.; Alpert, J.E.; Carmin, C.N.; Wisniewski, S.R.; Trivedi, M.H.; Biggs, M.M.; Shores-Wilson, K.; Morgan, D.; Schwartz, T.; Balasubramani, G.K.; Rush, A.J. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychol Med. 2004, 34, 1299–1308. [Google Scholar] [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Bartels, M.; Cacioppo, J.T.; van Beijsterveldt, T.C.; Boomsma, D.I. Exploring the association between well-being and psychopathology in adolescents. Behav. Genet. 2013, 43, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Gardner, C.O. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am. J. Psychiatry 2014, 171, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Kuria, M.W.; Ndetei, D.M.; Obot, I.S.; Khasakhala, L.I.; Bagaka, B.M.; Mbugua, M.N.; Kamau, J. The Association between Alcohol Dependence and Depression before and after Treatment for Alcohol Dependence. ISRN psychiatry 2012, 2012, 482802. [Google Scholar] [CrossRef] [PubMed]
- Baum-Baicker, C. The Psychological Benefits of Moderate Alcohol Consumption: A Review of the Literature. Drug Alcohol. Depend. 1985, 15, 305–322. [Google Scholar] [CrossRef]
- Kraus, C.; Kautzky, A.; Watzal, V.; Gramser, A.; Kadriu, B.; Deng, Z.; Bartova, L.; Zarate, C.A.; Lanzenberger, R.; Souery, D.; Montgomery, S.; Mendlewicz, J.; Zohar, J.; Fanelli, G.; Serretti, A.; Kasper, S. Body mass index and clinical outcomes in individuals with major depressive disorder: Findings from the GSRD European Multicenter Database. J. Affect. Disord. 2023, 335, 349–357. [Google Scholar] [CrossRef]
- Badillo, N.; Khatib, M.; Kahar, P.; Khanna, D. Correlation Between Body Mass Index and Depression/Depression-Like Symptoms Among Different Genders and Races. Cureus 2022, 14, e21841. [Google Scholar] [CrossRef]
- Cui, H.; Xiong, Y.; Wang, C.; Ye, J.; Zhao, W. The relationship between BMI and depression: a cross-sectional study. Front. Psychiatry 2024, 15, 1410782. [Google Scholar] [CrossRef]
- Vorvolakos, T.; Leontidou, E.; Tsiptsios, D.; Mueller, C.; Serdari, A.; Terzoudi, A.; Nena, E.; Tsamakis, K.; Constantinidis, T.C.; Tripsianis, G. The Association between Sleep Pathology and Depression: A Cross-Sectional Study among Adults in Greece. Psychiatry Res. 2020, 294, 113502. [Google Scholar] [CrossRef]
- Gehrman, P.; Seelig, A.D.; Jacobson, I.G.; Boyko, E.J.; Hooper, T.I.; Gackstetter, G.D.; Ulmer, C.S.; Smith, T.C.; Millennium Cohort Study Team. Predeployment Sleep Duration and Insomnia Symptoms as Risk Factors for New-Onset Mental Health Disorders Following Military Deployment. Sleep 2013, 36, 1009–1018. [Google Scholar] [CrossRef]
- Zhai, L.; Zhang, L.; Zhang, D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depression and Anxiety 2015, 32, 664–670. [Google Scholar] [CrossRef]
- Narita, Z.; Hidese, S.; Kanehara, R.; et al. Association of Sugary Drinks, Carbonated Beverages, Vegetable and Fruit Juices, Sweetened and Black Coffee, and Green Tea with Subsequent Depression: A Five-Year Cohort Study. ” Clin. Nutr. 2024, 43, 1395–1404. [Google Scholar] [CrossRef] [PubMed]
- Lotfaliany, M.; Bowe, S.J.; Kowal, P.; Orellana, L.; Berk, M.; Mohebbi, M. Depression and Chronic Diseases: Co-Occurrence and Communality of Risk Factors. J. Affect. Disord. 2018, 241, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Herrera, P.A.; Campos-Romero, S.; Szabo, W.; Martínez, P.; Guajardo, V.; Rojas, G. Understanding the Relationship between Depression and Chronic Diseases Such as Diabetes and Hypertension: A Grounded Theory Study. Int. J. Environ. Res. Public Health 2021, 18, 12130. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Henríquez, P.; Bes-Rastrollo, M.; Doreste, J. Mediterranean diet and depression. Public Health Nutr. 2006, 9, 1104–1109. [Google Scholar] [CrossRef]
- Mamalaki, E.; Ntanasi, E.; Hatzimanolis, A.; Basta, M.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study. Nutrients, 2023, 15, 359. [Google Scholar] [CrossRef]
- Yin, W.; Löf, M.; Chen, R.; Hultman, C.M.; Fang, F.; Sandin, S. Mediterranean Diet and Depression: A Population-Based Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 153. [Google Scholar] [CrossRef]
- Radkhah, N.; Rasouli, A.; Majnouni, A.; Eskandari, E.; Parastouei, K. The effect of Mediterranean diet instructions on depression, anxiety, stress, and anthropometric indices: A randomized, double-blind, controlled clinical trial. Prev. Med. Rep. 2023, 36, 102469. [Google Scholar] [CrossRef]
- Pérès, K.; Ouvrard, C.; Koleck, M.; Rascle, N.; Dartigues, J.F.; Bergua, V.; Amieva, H. Living in rural area: A protective factor for a negative experience of the lockdown and the COVID-19 crisis in the oldest old population? Int. J. Geriatr. Psychiatry 2021, 36, 1950–1958. [Google Scholar] [CrossRef]
- Nam, S.M.; Peterson, T.A.; Seo, K.Y.; Han, H.W.; Kang, J.I. Discovery of Depression-Associated Factors from a Nationwide Population-Based Survey: Epidemiological Study Using Machine Learning and Network Analysis. J. Med. Internet Res. 2021, 23, e27344. [Google Scholar] [CrossRef]
- Naveen, K.S.; Goel, A.; Dwivedi, S.; Hassan, M. Adding life to years: Role of gender and social and family engagement in geriatric depression in rural areas of Northern India. J. Family Med. Prim. Care 2020, 9, 721. [Google Scholar] [CrossRef]
- Sharma, A.; Verbeke, W.J.M.I. Improving Diagnosis of Depression with XGBOOST Machine Learning Model and a Large Biomarkers Dutch Dataset (n = 11,081). Front. Big Data 2020, 3, 15. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; van Loo, H.; Wardenaar, K.J.; Bossarte, R.M.; Brenner, L.A.; Cai, T.; Ebert, D.D.; Hwang, I.; Li, J.; de Jonge, P.; Nierenberg, A.A.; Petukhova, M.V.; Rosellini, A.J.; Sampson, N.A.; Schoevers, R.A.; Wilcox, M.A.; Zaslavsky, A. M. Testing a machine-learning algorithm to predict the persistence and severity of major depressive disorder from baseline self-reports. Mol. psychiatry 2016, 21, 1366–1371. [Google Scholar] [CrossRef] [PubMed]
- Nahm, F.S. Receiver operating characteristic curve: overview and practical use for clinicians. Korean J. Anesthesiol. 2022, 75, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Richter, T.; Fishbain, B.; Richter-Levin, G.; Okon-Singer, H. Machine Learning-Based Behavioral Diagnostic Tools for Depression: Advances, Challenges, and Future Directions. J. Pers. Med. 2021, 11, 957. [Google Scholar] [CrossRef]
- Qasrawi, R.; Vicuna Polo, S.P.; Abu Al-Halawa, D.; Hallaq, S.; Abdeen, Z. Assessment and Prediction of Depression and Anxiety Risk Factors in Schoolchildren: Machine Learning Techniques Performance Analysis. JMIR Form Res. 2022, 6, e32736. [Google Scholar] [CrossRef]

| Depression | ||||
|---|---|---|---|---|
| Number (%) | Frequency | Proportion (%) | p value | |
| Gender | 0.145 | |||
| Males | 570 (46.5) | 152 | 26.7 | |
| Females | 657 (53.5) | 200 | 30.4 | |
| Age (years) | <0.001 | |||
| ≤40 | 341 (27.8) | 42 | 12.3 | |
| 41 – 60 | 571 (46.5) | 164 | 28.7 | |
| >60 | 315 (25.7) | 146 | 46.3 | |
| Marital status | <0.001 | |||
| Married | 825 (67.2) | 257 | 31.2 | |
| Single | 252 (20.5) | 41 | 16.3 | |
| Divorced | 102 (8.3) | 42 | 41.2 | |
| Widowed | 48 (3.9) | 12 | 25.0 | |
| Cultural status | <0.001 | |||
| Greek Christians | 807 (65.7) | 194 | 24.0 | |
| Greek Muslims | 358 (29.2) | 132 | 36.9 | |
| Expatriated Greeks | 62 (5.1) | 26 | 41.9 | |
| Place of residence | <0.001 | |||
| Urban | 524 (42.7) | 88 | 16.8 | |
| Rural | 703 (57.3) | 264 | 37.6 | |
| Education level | <0.001 | |||
| Low | 406 (33.1) | 211 | 52.0 | |
| Medium | 431 (35.1) | 98 | 22.7 | |
| High | 390 (31.8) | 43 | 11.0 | |
| Presence of child <6 years | 0.029 | |||
| No | 1128 (91.9) | 333 | 29.5 | |
| Yes | 99 (8.1) | 19 | 19.2 | |
| Unemployment | <0.001 | |||
| No | 1121 (91.4) | 303 | 27.0 | |
| Yes | 106 (8.6) | 49 | 46.2 | |
| Financial status | <0.001 | |||
| Low | 614 (50.0) | 213 | 34.7 | |
| Medium | 258 (21.0) | 33 | 12.8 | |
| High | 180 (14.7) | 29 | 16.1 | |
| Depression | ||||
|---|---|---|---|---|
| Number (%) | Frequency | Proportion (%) | p value | |
| Smoking status | 0.242 | |||
| Never/ex-smoker | 808 (65.9) | 223 | 27.6 | |
| Current smoker | 419 (34.1) | 129 | 30.8 | |
| Alcohol consumption | <0.001 | |||
| None | 621 (50.6) | 212 | 34.1 | |
| 1 – 3 glasses/week | 316 (25.8) | 69 | 21.8 | |
| 4 – 6 glasses/week | 215 (17.5) | 42 | 19.5 | |
| >6 glasses/week | 75 (6.1) | 29 | 38.7 | |
| Coffee consumption | <0.001 | |||
| None | 113 (9.2) | 33 | 29.2 | |
| 1 – 2 cups/day | 723 (58.9) | 179 | 24.8 | |
| 3 – 4 cups/day | 322 (26.2) | 99 | 30.7 | |
| > 4 cups/day | 69 (5.6) | 41 | 59.4 | |
| Adherence to MED diet | 0.080 | |||
| Low | 968 (78.9) | 289 | 29.9 | |
| High | 259 (21.1) | 63 | 24.3 | |
| Physical activity | <0.001 | |||
| Low | 1031 (84.0) | 321 | 31.1 | |
| High | 196 (16.0) | 31 | 15.8 | |
| Midday sleep | 0.101 | |||
| No | 520 (42.4) | 162 | 31.2 | |
| Yes | 707 (57.6) | 190 | 26.9 | |
| Sleep duration | <0.001 | |||
| Short | 273 (22.2) | 130 | 47.6 | |
| Normal | 780 (63.6) | 176 | 22.6 | |
| Long | 174 (14.2) | 46 | 26.4 | |
| Depression | ||||
|---|---|---|---|---|
| Number (%) | Frequency | Proportion (%) | p value | |
| BMI status | 0.103 | |||
| Normal | 415 (33.8) | 113 | 27.2 | |
| Overweight | 352 (28.7) | 91 | 25.9 | |
| Obese | 460 (37.5) | 148 | 32.2 | |
| Subjective health status | <0.001 | |||
| Good | 941 (76.7) | 168 | 17.9 | |
| Bad | 286 (23.3) | 184 | 64.3 | |
| Morbidity of chronic illness | <0.001 | |||
| No | 534 (43.5) | 94 | 17.6 | |
| Yes | 693 (56.5) | 258 | 37.2 | |
| Number of chronic diseases | <0.001 | |||
| None | 534 (43.5) | 94 | 17.6 | |
| One | 360 (29.3) | 97 | 26.9 | |
| Two | 208 (17.0) | 87 | 41.8 | |
| More than two | 125 (10.2) | 74 | 59.2 | |
| Family history of depression | <0.001 | |||
| No | 812 (66.2) | 199 | 24.5 | |
| Yes | 415 (33.8) | 153 | 36.9 | |
| Traumatic events in life | <0.001 | |||
| No | 716 (58.4) | 155 | 21.6 | |
| Yes | 511 (41.6) | 197 | 38.6 | |
| Anxiety symptoms | <0.001 | |||
| No | 813 (66.3) | 119 | 14.6 | |
| Yes | 414 (33.7) | 233 | 56.3 | |
| Excessive daytime sleepiness | 0.704 | |||
| No | 1120 (91.3) | 323 | 28.8 | |
| Yes | 107 (8.7) | 29 | 27.1 | |
| Presence of insomnia | 0.042 | |||
| No | 1015 (82.7) | 279 | 27.5 | |
| Yes | 212 (17.3) | 73 | 34.4 | |
| Sleep quality | 0.008 | |||
| Good | 765 (62.3) | 199 | 26.0 | |
| Bad | 462 (37.7) | 153 | 33.1 | |
| Risk Factor | Description | Type of variable |
|---|---|---|
| Gender | Gender (male/female) | Categorical |
| Marital status | Marital status (single/married/divorced/widowed) | Categorical |
| Residence | Area of residence (urban/rural) | Categorical |
| Education | Education level (low/medium/high) | Categorical |
| Unemployment | Unemployment (no/yes) | Categorical |
| Income | Income (low/medium/high) | Categorical |
| Chronic diseases | Chronic diseases (no/yes) | Categorical |
| BMI | Body mass index (normal/overweight/obese) | Categorical |
| Alcohol | Alcohol consumption/week (none/1-3 glasses/4-6 glasses/>6 glasses) | Categorical |
| Coffee | Coffee consumption/day (none/1-2 glasses/3-4 glasses/>4 glasses) | Categorical |
| Med diet | Adherence to Mediterranean diet (no/yes) | Categorical |
| Child <6 years | Presence of a child younger than 6 years of age (no/yes) | Categorical |
| Sleep duration | Sleep duration (short/normal/long) | Categorical |
| Sleepiness | Excessive daytime sleepiness (no/yes) | Categorical |
| Anxiety | Anxiety (no/yes) | Categorical |
| Classifier | Accuracy (%) | f1-score (%) |
Precision (%) |
Sensitivity (Recall) (%) |
Specificity (%) |
Hyperparameters |
|---|---|---|---|---|---|---|
| LR | 79.95 | 79.04 | 78.82 | 79.95 | 90.48 | C: 1, penalty: l2 |
| SVM | 95.66 | 95.64 | 95.63 | 95.66 | 97.80 | C: 10, kernel: rbf |
| XGBoost | 97.83 | 97.85 | 97.94 | 97.83 | 97.44 | gamma: 0, max_depth: 7, min_child_weight: 1 |
| NN | 97.02 | 97.03 | 97.06 | 97.02 | 97.44 | activation: tanh, alpha: 0.0001, hidden_layer_sizes: (10, 20, 50), learning_rate: constant, solver: adam |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





