Submitted:
01 May 2025
Posted:
07 May 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Background of the Study
1.2. Aim of the Study
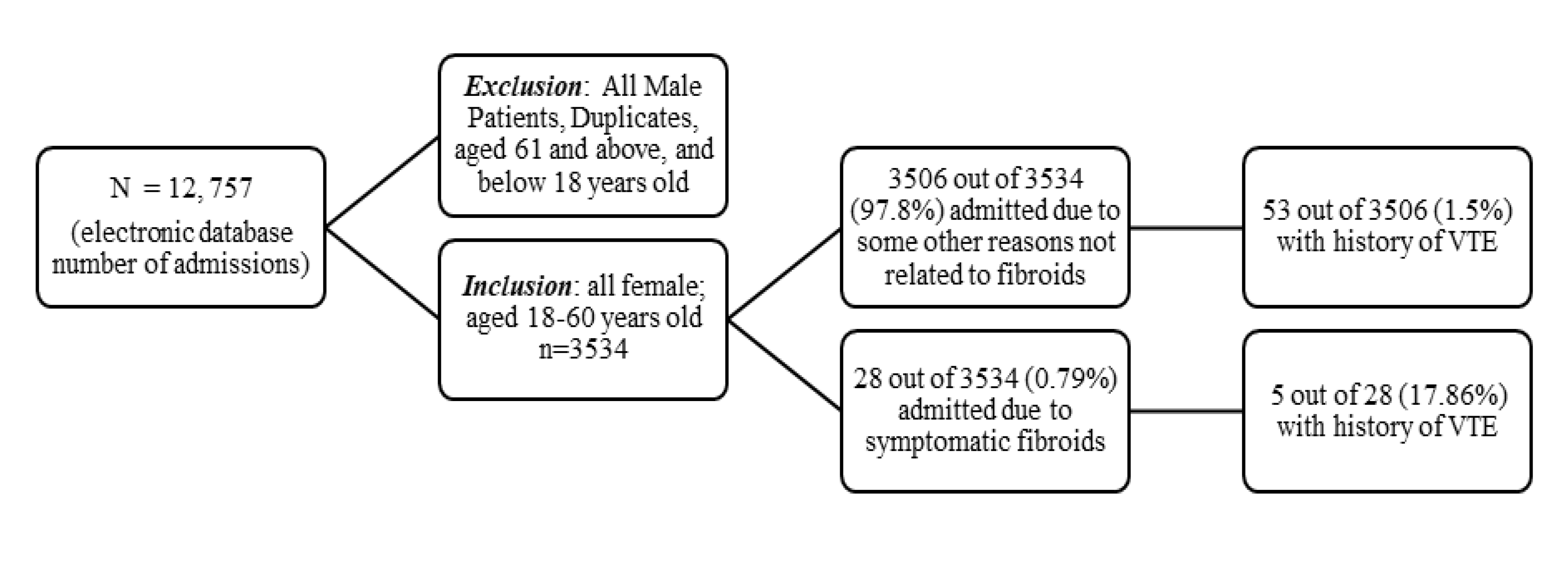
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Study Participants
2.4. Statistical Analysis
3. Results
4. Discussion
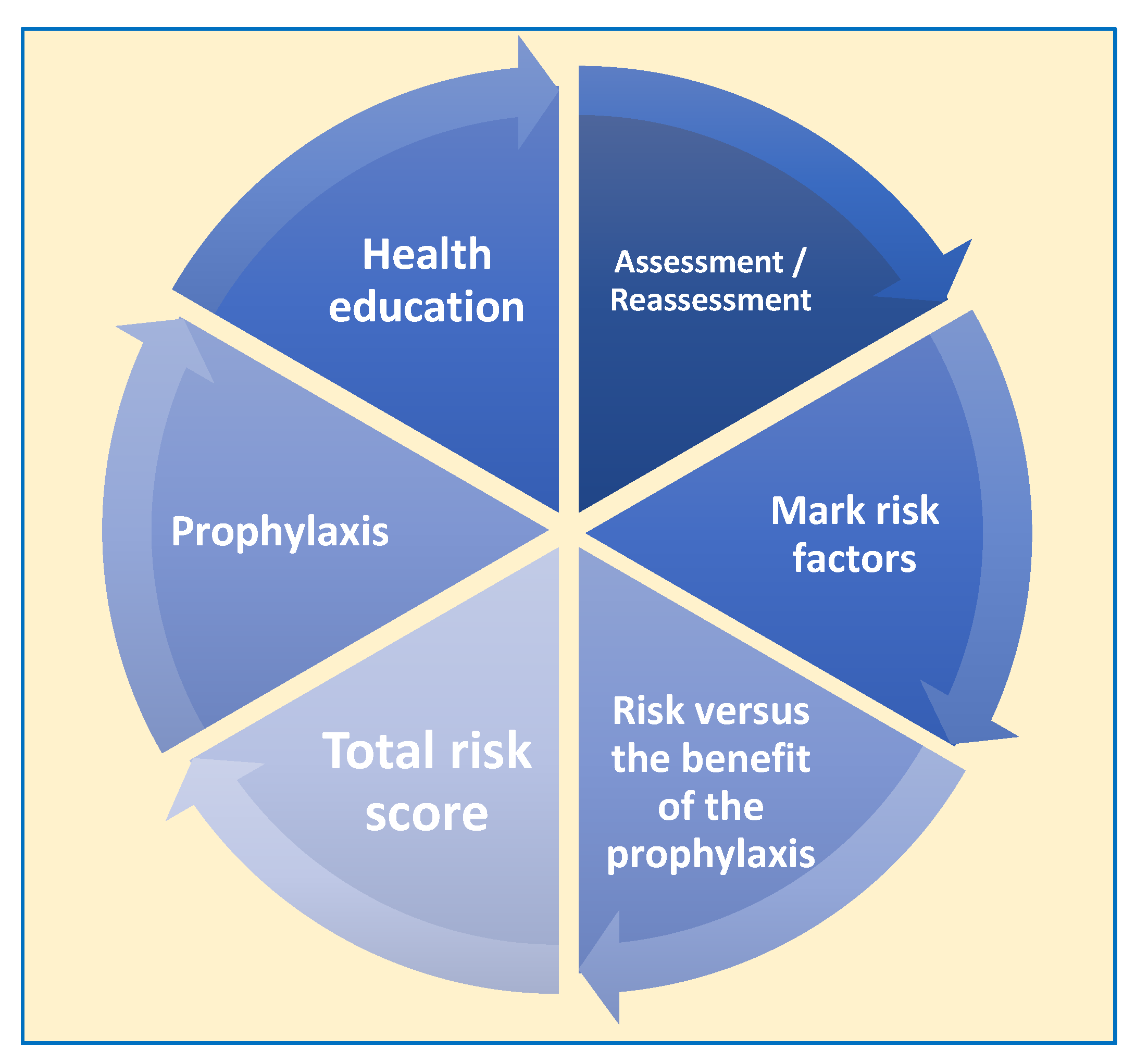
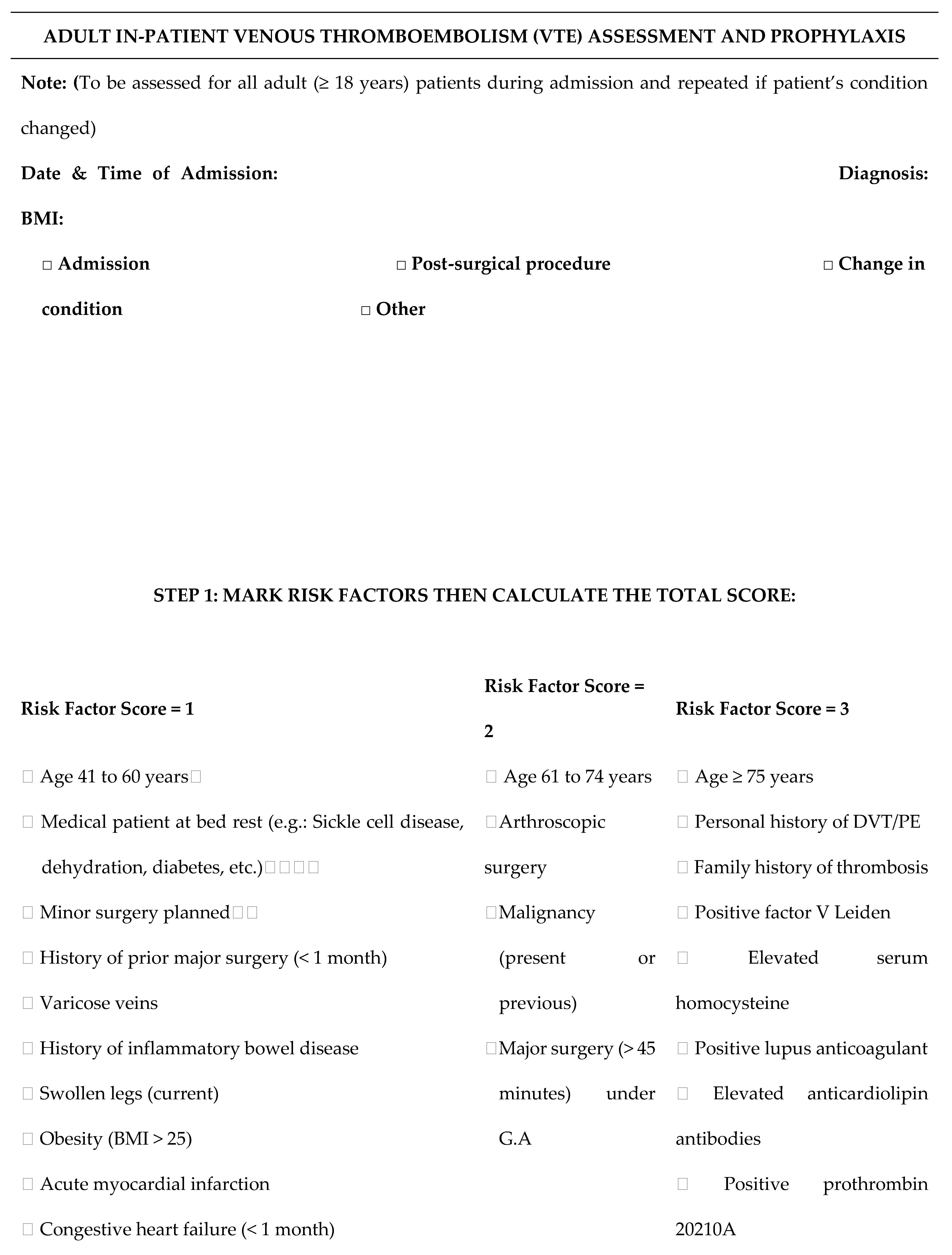
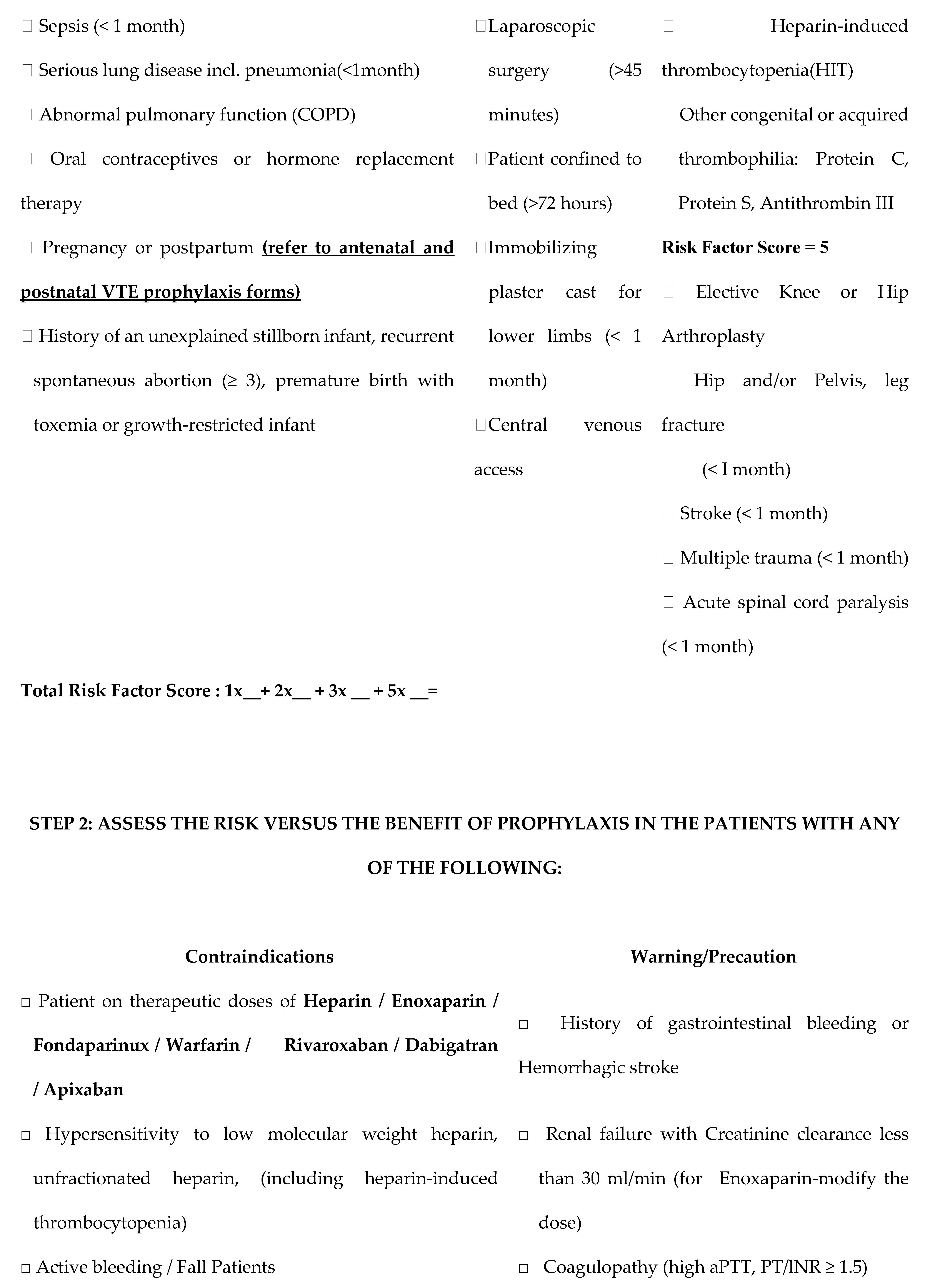
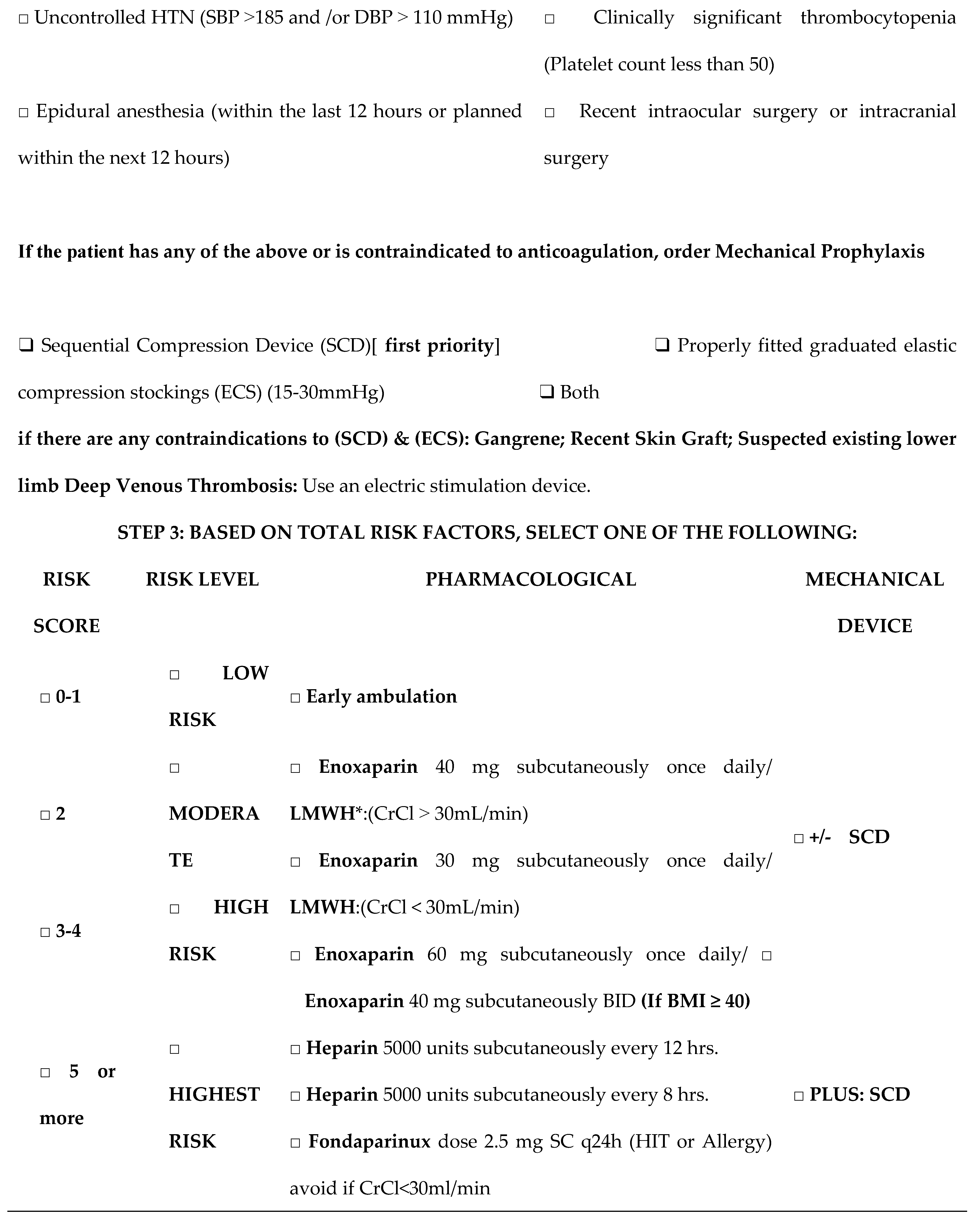
4.1. The Adult In-Patient Venous Thromboembolism (VTE) Assessment and Prophylaxis
4.2. The Significance of Identifying the Potential Risk Factors for VTE
5. Conclusions
Acknowledgments
References
- Agnelli, G., Anderson, F., Arcelus, J., Bergqvist, D., Brecht, J., Greer, I., Heit, J., Hutchinson, J., Kakkar, A., Mottier, D., Oger, E., Samama, M., Spannagl, M., & Cohen, A. (2007). Venous thromboembolism (VTE) in Europe. Thrombosis and Haemostasis, 98(10), 756–764. [CrossRef]
- Brewer, M. B. , Woo, K., & Weaver, F. A. (2015). Venous thromboembolism secondary to uterine fibroids: A case of Phlegmasia cerulea dolens and review of the literature. Annals of Vascular Surgery, 29(2), 364.e5-364.e9. [CrossRef]
- Cai, E., Shao, Y., Suarthana, E., Bergeron, A., Mansour, F. W., & Krishnamurthy, S. (2020). A Case Series of Patients with Large Uterine Fibroids and Venous Thromboembolisms. Journal of Obstetrics and Gynaecology Canada, 43(3), 352–360. [CrossRef]
- Caprini, J. A. (2010). Risk assessment as a guide for the prevention of the many faces of venous thromboembolism. The American Journal of Surgery, 199(1), S3–S10. [CrossRef]
- Clarkesmith, D. E. , Pattison, H. M., Lip, G. Y. H., & Lane, D. A. (2013). Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS ONE, 8(9), e74037. [CrossRef]
- Champagne, B., & Laryea, J. (2013). Venous thromboembolism prophylaxis. Clinics in Colon and Rectal Surgery, 26(03), 153–159. [CrossRef]
- Chaudhary, R. , Damluji, A., Batukbhai, B., Sanchez, M., Feng, E., Serharan, M. C., & Moscucci, M. (2017). Venous thromboembolism prophylaxis: inadequate and overprophylaxis when comparing perceived versus calculated risk. Mayo Clinic Proceedings Innovations Quality & Outcomes, 1(3), 242–247. [CrossRef]
- Davies, M.J., Gray, L.J., & Ahrabian, D. (2017). Chapter 3 Developing the risk score. National Institute for Health Research. https://www.ncbi.nlm.nih.gov/books/NBK409312/.
- Flanagan, L. , Bassa, B. A., Moriarty, J. M., Lyons, F., Sands, F., Comer, C., Solomon, L., & Aínle, F. N. (2024). Hospital PERT: Bridging VTE care across all disciplines. Thrombosis Update, 16, 100181. [CrossRef]
- Giuliani, E., As-Sanie, S., & Marsh, E. E. (2020). Epidemiology and management of uterine fibroids. International Journal of Gynaecology and Obstetrics, 149(1), 3–9. [CrossRef]
- Haut, E. R. , Aboagye, J. K., Shaffer, D. L., Wang, J., Hobson, D. B., Yenokyan, G., Sugar, E. A., Kraus, P. S., Farrow, N. E., Canner, J. K., Owodunni, O. P., Florecki, K. L., Webster, K. L. W., Holzmueller, C. G., Pronovost, P. J., Streiff, M. B., & Lau, B. D. (2018). Effect of Real-time Patient-Centered Education Bundle on Administration of Venous Thromboembolism Prevention in Hospitalized Patients. JAMA Network Open, 1(7), e184741. [CrossRef]
- Heit, J. A. (2015). Epidemiology of venous thromboembolism. Nature Reviews. Cardiology, 12(8), 464–474. [CrossRef]
- Henke, P. K. , Kahn, S. R., Pannucci, C. J., Secemksy, E. A., Evans, N. S., Khorana, A. A., Creager, M. A., & Pradhan, A. D. (2020). Call to action to prevent venous thromboembolism in hospitalized patients: A policy statement from the American Heart Association. Circulation, 141(24). [CrossRef]
- Huang, H. , Kor, C., Chen, C., Chen, H., Yang, P., Tsai, C., & Huang, C. (2018). Increased Risk of Venous Thromboembolism in Women with Uterine Leiomyoma: A Nationwide, Population-Based Case-Control Study. PubMed, 34(1), 66–76. [CrossRef]
- Huang, W. , Anderson, F. A., Spencer, F. A., Gallus, A., & Goldberg, R. J. (2012). Risk-assessment models for predicting venous thromboembolism among hospitalized non-surgical patients: a systematic review. Journal of Thrombosis and Thrombolysis, 35(1), 67–80. [CrossRef]
- Hunt, B. J. (2019b). Preventing hospital-associated venous thromboembolism. BMJ, l4239. [CrossRef]
- Imtiaz, H. , Nguyen, T., Thai, T. T. V., Kouklidis, G., Horgan, M., & Vijayaraghavan, R. (2024). Evaluating the compliance to 24-Hour venous thromboembolism risk re-assessment following orthopaedic surgery at a tertiary center: a Closed-Loop Clinical Audit. Cureus. [CrossRef]
- Kennedy, S. (2023, September 8). Explaining the basics of patient risk scores in healthcare. Healthtech Analytics. https://www.techtarget.com/healthtechanalytics/feature/Explaining-the-Basics-of-Patient-Risk-Scores-in-Healthcare.
- Khan, A. , Shehmar, M., & Gupta, J. (2014). Uterine fibroids: current perspectives. International Journal of Women’s Health, 95. [CrossRef]
- Lacharite-Roberge, A., Raza, F., Bashir, R., Dass, C. A., Moser, G. W., Auger, W. R., Toyoda, Y., Forfia, P. R., & Vaidya, A. (2018). Case series of seven women with uterine fibroids associated with venous thromboembolism and chronic thromboembolic disease. Pulmonary Circulation, 9(1), 1–7. [CrossRef]
- Latif, H., Sosa, V. B., Farid, S., Fernandez, S., Hazen, N., Morozov, V., & Fitzpatrick, K. W. (2020). Venous Thromboembolism in Women with Uterine Fibroids. Blood, 136(Supplement 1), 28–29. [CrossRef]
- Moulder, J. K. , Siedhoff, M. T., Till, S. R., & Moll, S. (2016). Management considerations for patients with uterine fibroids and concurrent venous thromboembolism. Current Opinion in Obstetrics & Gynecology, 28(4), 329–335. [CrossRef]
- Onwuzo, C. , Olukorode, J., Sange, W., Tanna, S. J., Osaghae, O. W., Hassan, A., Kristilere, H., Orimoloye, D. A., Omokore, O., Ganiyu, B., Fayemi, T., & Addeh, E. (2023). A Review of the Preventive Strategies for Venous Thromboembolism in Hospitalized Patients. Cureus. [CrossRef]
- Painter, R. (2022). Patient reassessment is a key physician and nursing responsibility | Painter Law Firm Medical Malpractice Attorneys. https://painterfirm.com/medmal/patient-reassessment-is-a-key-physician-andnursing-responsibility/.
- Pandor, A. , Tonkins, M., Goodacre, S., Sworn, K., Clowes, M., Griffin, X. L., Holland, M., Hunt, B. J., De Wit, K., & Horner, D. (2021). Risk assessment models for venous thromboembolism in hospitalised adult patients: a systematic review. BMJ Open, 11(7), e045672. [CrossRef]
- Popoola, V. O. , Lau, B. D., Shihab, H. M., Farrow, N. E., Shaffer, D. L., Hobson, D. B., Kulik, S. V., Zaruba, P. D., Shermock, K. M., Kraus, P. S., Pronovost, P. J., Streiff, M. B., & Haut, E. R. (2016). Patient Preferences for Receiving Education on Venous thromboembolism Prevention – A survey of Stakeholder Organizations. PLoS ONE, 11(3), e0152084. [CrossRef]
- Shiota, M. , Kotani, Y., Umemoto, M., Tobiume, T., Tsuritani, M., Shimaoka, M., & Hoshiai, H. (2011). Deep-Vein Thrombosis Is Associated with Large Uterine Fibroids. The Tohoku Journal of Experimental Medicine, 224(2), 87–89. [CrossRef]
- Stewart, E. A. (2015). Uterine fibroids. New England Journal of Medicine/˜the œNew England Journal of Medicine, 372(17), 1646–1655. [CrossRef]
- Stewart, E. A. , Laughlin-Tommaso, S. K., Catherino, W. H., Lalitkumar, S., Gupta, D., & Vollenhoven, B. (2016). Uterine fibroids. Nature Reviews. Disease Primers, 2(1). [CrossRef]
- Solari, F. Solari, F., Varacallo, M.A. (2025). Low-Molecular-Weight Heparin (LMWH). National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK525957/.
- U.S. Centers for Disease Control and Prevention. (2024, May 15). About venous thromboembolism (Blood clots). Venous Thromboembolism (Blood Clots). https://www.cdc.gov/blood-clots/about/index.html#:~:text=VTE%20includes%20deep%20vein%20thrombosis,which%20can%20be%20life%2Dthreatening.
| N | Minimum | Maximum | Mean | Std. Deviation | |
| AGE | 3534 | 18 | 60 | 36.27 | 10.442 |
| VTE History | 3534 | 1 | 2 | 1.98 | .126 |
| Symptomatic Fibroid | 3534 | 1 | 2 | 1.99 | .089 |
| Risk Factor Score | 3534 | 1 | 8 | 4.21 | 2.432 |
| Valid N (listwise) | 3534 |
| Risk Category | N | VTE history | HA- VTE |
| Medical and surgical cases | |||
| < 1 (Low risk) | 770 | 0 | 0 |
| 2 (Moderate risk) | 576 | 0 | 0 |
| 3-4 (High risk) | 519 | 7 | 1 |
| ≥5 (Highest risk) | 247 | 38 | 0 |
| Obstetric cases | |||
| Low risk | 214 | 0 | 0 |
| Intermediate risk | 1178 | 7 | 0 |
| High risk | 3 | 0 | 0 |
| Total | 3506 | 52 | 1 |
| Symptomatic fibroid cases | 28 | 4 | 1 |
| Grand Total | 3534 | 58 | |
| Symptomatic Fibroid | VTE History | ||
| Symptomatic Fibroid | Pearson Correlation | Yes | .115** |
| Sig. (2-tailed) | <.001 | ||
| N | 3534 | 3534 | |
| VTE History | Pearson Correlation | .115** | 1 |
| Sig. (2-tailed) | <.001 | ||
| N | 3534 | 3534 | |
| Participant | n = 28 |
| Age (Median, years) | 43 [18-60] |
| With the history of VTE | |
|
4 (14.29 %) |
|
23 (82.14 %) |
|
1 (3.57%) |
| Number of fibroids | |
|
20 (71.43 %) |
|
5 (17.86 %) |
|
3 (10.71 %) |
| Size (Median, in cm) | 7.5 cm |
| Risk Factor Score | |
|
5 (17.86 %) |
|
6 (21.43 %) |
|
14 (50 %) |
|
3 (10.71 %) |
| Prophylaxis | |
|
6 (21.43 %) |
|
10 (35.71 %) |
|
7 (25 %) |
|
5 (17.86%) |
| Surgical procedure | |
|
24 (85.71 %) |
|
2 (7.14 %) |
|
1 (3.57 %) |
|
1 (3.57 %) |
| LOS (median, days) | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





