Introduction
Globally, The growing increase in the prevalence of chronic diseases like diabetes and hypertension is mainly contributed to poor lifestyle behavior and diet [
1]. One of the major keys for improvement and prevention of these chronic diseases with lower adverse effect and cost in comparisons to pharmacological therapy is healthy diet and nutrition [
2].
Doctors whether joiners or resident or general practitioners and even professionals are one of the valid and reliable sources of information on healthy food and nutrition. Most of patients with chronic diseases and their families expected to receive information or advice from their doctors. Accordingly, its important for all medical doctors to have good nutrition and practice to translate it in effective way for prevention and management of these diseases [
3,
4,
5].
Most of the studies that evaluated nutritional care knowledge, practice and experience whether conducted on medical students during their early educational years in medical schools or among medical doctors reported inadequate knowledge and practices this were partly due to that most of medical schools curriculums were emphasizing on disease management rather than prevention, in addition to limited time for continuing nutrition education. This highlight the need for improving nutrition education of medical schools in order to deliver better nutrition care for population [
6,
7,
8].
With the increase of the prevalence of non communicable diseases in Iraq that accompanied by changes in diet habits and lifestyle [
9]. It would be important to incorporate an educational interventions to improve nutrition educational practices during medical schools or continuing medical education on nutrition to achieve better health promotion of the population. Accordingly, the present study aimed to assess nutrition related knowledge, attitude and perceived self-efficacy in nutrition care of newly graduated doctors.
Material and Methods
The present study was approved by scientific committee of family and community medicine department of college of medicine, university of Mosul. A cross sectional study design were carried out from December 2023 till January 2025, in which all newly graduated medical doctors, from both colleges of medicine that present in the city, during the years 2022, 2023, and 2024 were eligible to participate. A total of 385 doctors needed to be collected depending on the following equation [
10]
where n= sample size,
Z= confidence level (95%)
P= population proportion (50%)
e= margin of error (0.05)
To collect the needed sample, a simple random technique were carried out in which every 5th name in the list containing the names of all doctors graduated in these years that obtained for Iraqi Medical association in Ninevah, registration department were included. All doctors sampled were invited to participate to this study and told that their responses would be anonymous, and those who accept to participated, an informed written consent were obtained from them.
Data collected using a special questionnaire form that was adopted from previous validated studies [
11,
12,
13,
14,
15] and were reviewed by experts in nutrition and health education and found to be content valid. In addition, the questionnaire were pre-tested on a sample of 20 newly graduated medical doctors, in order to detect the clarity, and distressfulness of the questionnaire. The time needed to complete the form were between 20 – 25 minutes.
The final questionnaire form measured the following variables:
Demographic characteristics, which were age, sex and name of medical college graduated from.
Knowledge assessment (17 questions), each responses were assigned as a score of 1 for every correct answer, summed and computed out of 100%.
Attitude assessment (6 questions) were assessed based on 3 point Likert scale of 1-3 (1= disagree; 2= neutral; 3= disagree).
Confident level in providing nutritional care (7 questions), were assessed based on 3 point Likert scale of 1-3 ( 1= un confident, 2= neither confident nor un confident, 3= confident)
Satisfaction with nutrition education and training received during medical college education years were assessed by 2 answers either dissatisfied or satisfied.
Data were analyzed statistically Statistical Package for Social Science (SPSS) 19.0. Descriptive statistics (mean, standard deviation and frequency) were calculated. In addition chi square test was used to determine possible relation among variables. A p value less than 0.05 were regarded significant in this analysis.
Result
Only 392 of a total of 420 randomly chosen newly graduated medical doctors, accepted to participated in this study and completed the questionnaire form (response rate = 93%). The mean age was 24.9 ± 0.04 years, 52.3% (n= 193) were females and 47.7% (n= 176) were males.
Table (1 ) shows that the average score of knowledge was 62.3%, with higher scores reported for knowledge related for important nutrients that is preventive for some diseases (70.3%) while lower scores seen for dietary recommendations for cardiovascular diseases (49.4%).
Table 1.
Medical doctors mean scores predicted by nutrition knowledge assessment topics.
Table 1.
Medical doctors mean scores predicted by nutrition knowledge assessment topics.
| No. |
Nutrition topic |
Mean± SD
(n=393) |
| 1 |
Dietary recommendations for cardiovascular diseases(5 items) |
49.4±1.17 |
| 2 |
Nutrients recommended for prevention of diseases (7 items) |
70.3±1.07 |
| 3 |
Diabetes and obesity(2 items) |
64.3± 1.58 |
| |
All topics |
62.3±0.91 |
Table (2) display the study population attitudes towards incorporating nutrition care into daily clinical practice and patient follow up. More than half (52.7% ) of participants showed positive attitudes towards importance of nutrition care as part of daily clinical practice(2.38±0.03). Most of the participants 98% agreed that nutrition assessment must be part of standard care given to patients.
Table 2.
Attitude assessment towards nutritional care of the participants.
Table 2.
Attitude assessment towards nutritional care of the participants.
| No. |
Items |
Disagree |
Neither agree nor disagree |
agree |
| No. |
% |
No. |
% |
No. |
% |
| 1 |
Nutrition assessment must be part of standard patient care |
6 |
1.5 |
2 |
0.5 |
384 |
98 |
| 2 |
Discussing nutrition information is a duty of all medical care providers |
106 |
27 |
110 |
28 |
176 |
44.9 |
| 3 |
Nutritional counselling must be part of routine care to all patients |
85 |
21.7 |
51 |
13 |
256 |
63.3 |
| 4 |
Acute severe malnutrition regarded as a medical emergency |
36 |
9.2 |
66 |
16.8 |
221 |
56.4 |
| 5 |
If nutritional counselling given to patients, they will adopt healthier diet choices |
90 |
23 |
68 |
17.3 |
234 |
59.7 |
| 6 |
Doctors advices can change patient lifestyle (nutrition and physical activity) |
173 |
44.1 |
29 |
7.4 |
190 |
48.5 |
| |
Total |
53 |
13.5 |
132 |
33.7 |
207 |
52.8 |
Majority of the study population reported that they were either un confident (35.5%) or neither confident nor unconfident (52.5%) in providing nutrition care and dietary advices to patients as shown in Table (3). In addition, more than two third of newly graduated medical doctors reported that they were un confident in recommending diet based on serving size (77.8%) or Calculating total calories needed (77%) from food groups for patients.
Table 3.
Newly graduated self confidence in providing nutritional care.
Table 3.
Newly graduated self confidence in providing nutritional care.
| |
Items |
unconfident |
Neither confident nor unconfident |
confident |
| No. |
% |
No. |
% |
No. |
% |
| 1 |
Calculating BMI and WHR based on gender |
39 |
9.9 |
74 |
18.9 |
279 |
71.2 |
| 2 |
Recommending diet for patients with diabetes mellitus |
234 |
59.7 |
80 |
20.4 |
78 |
19.9 |
| 3 |
Discussing role of dietary fats especially saturated fats for elevating blood cholesterol |
62 |
15.8 |
172 |
43.9 |
158 |
40.3 |
| 4 |
Advising diet based on food pyramid serving size |
305 |
77.8 |
53 |
13.5 |
34 |
8.7 |
| 5 |
Role of omega3 fatty acids in heart diseases |
161 |
41.1 |
73 |
18.6 |
158 |
40.3 |
| 6 |
Providing nutrition education on calories obtained form food groups that needed by patients |
302 |
77.1 |
53 |
13.5 |
37 |
9.4 |
| 7 |
Starting nutritional therapy for severely malnourished patient |
179 |
45.7 |
110 |
28 |
103 |
26.3 |
| |
All items |
139 |
35.5 |
206 |
52.5 |
47 |
12 |
Table (4) Doctors with good knowledge have reported a positive attitude for corporation nutrition care into routine patients care more confidence to provide nutritional plan for patients compared with those found to have poor knowledge, a difference of highly statistical value (p = 0.000)
Table 4.
Relation between knowledge, attitude and self-efficacy towards providing nutritional care.
Table 4.
Relation between knowledge, attitude and self-efficacy towards providing nutritional care.
| Items |
Knowledge |
|
| Poor < 50% |
Good ≥ 50% |
P value* |
| Attitude |
|
| Disagree |
29 |
27 |
0.000 |
| Neither agree nor disagree |
79 |
51 |
| Agree |
12 |
194 |
| Self – efficacy |
|
| Un confident |
96 |
70 |
0.000 |
| Neither confident nor un confident |
14 |
138 |
| Confident |
10 |
64 |
| Total |
120 |
272 |
|
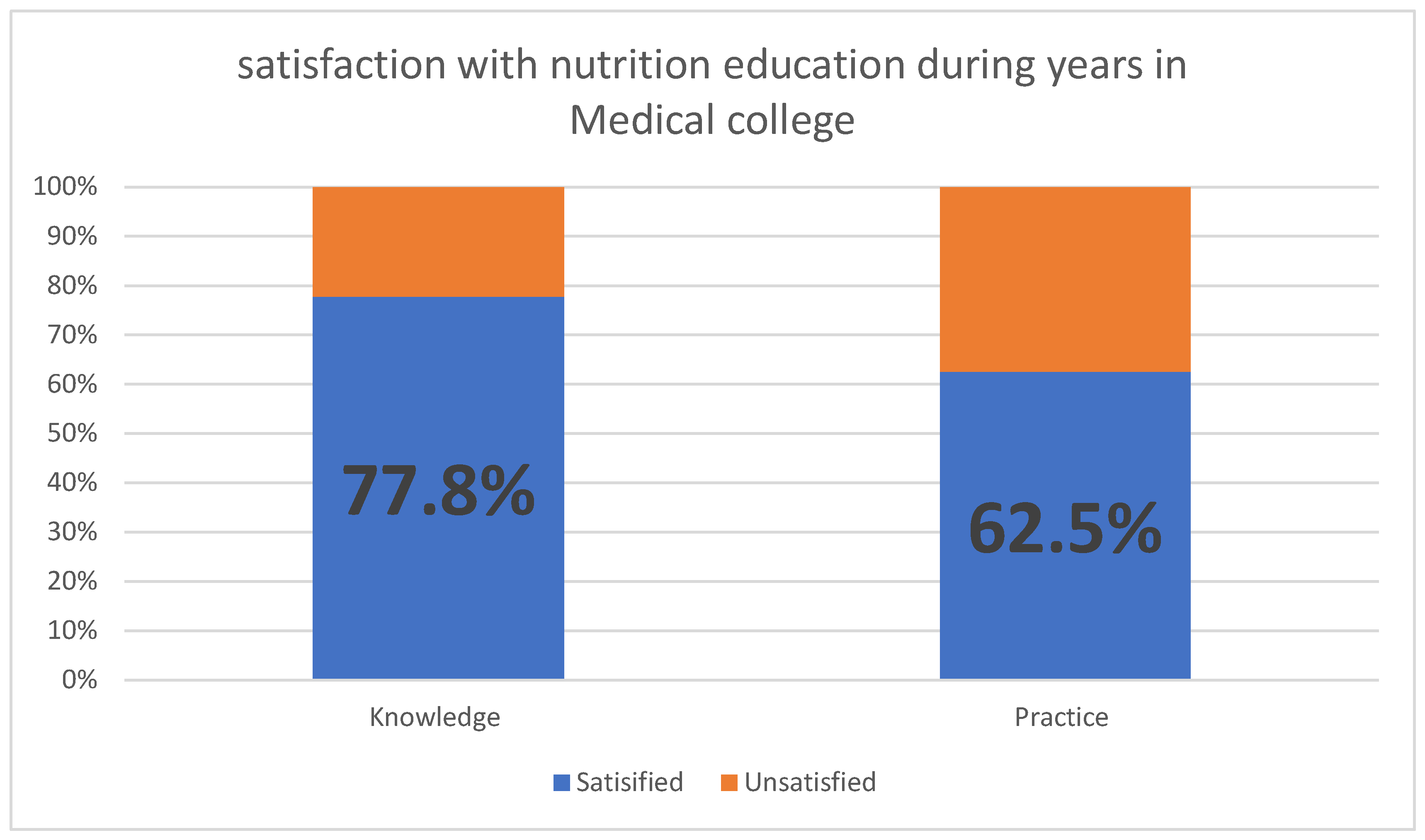
Regarding satisfaction with nutrition knowledge and practice gained during college years of education, Majority were satisfied with knowledge gained by lectures (77.8%) but less satisfied with practice gained (62.5%), as shown in Figure (1).
Figure 1.
Satisfaction with nutrition education during years in Medical college.
Figure 1.
Satisfaction with nutrition education during years in Medical college.
Discussion
The aim of the current study was to assess knowledge, attitude and perceived confidence in providing nutritional care among newly graduated medical doctors from medical Colleges in Mosul City. The present study revealed that the average nutritional knowledge score were 62.3%. This were in accordance to that reported by study conducted among physicians in 4 Gulf countries (Bahrain, Saudia Arbia, United Arab Emirate and Kuwait) in which average nutrition related knowledge score was 62% [
16] and another study done in Ghana showed average score of general practitioners were 64% [
13] but higher than that reported in Jeddah as the average knowledge score of 52% [
17]. This average level of nutrition was good level as stated by a systematic narrative review carried out by Zeldman and Andrade, in which that average of nutrition knowledge scores among physician and nurses were commonly ranged between poor (33%) to very good (72%) [
18].
Despite this good knowledge but a gap were found in assessing knowledge of each topic, the lowest mean score were for nutrition and cardiovascular diseases (49.4%) topic compared to those score for other topics. This findings were in accordance to that displayed by previous studies in Saudi Arabia [
19] and United State [
12]. This is probably due to after graduation medical doctors may fail to remember and integrate basics of nutrition with clinical practice as its taught during pre-clinical years. In addition Flynn M. etal study stated that most of physician had inadequate understanding on carbohydrate, fat, triglycerides and high density lipoprotein metabolism [
20].
All participants in this study exhibited positive attitude (52.8% agree )towards incorporating nutrition care and counselling in daily clinical practice, which is similar to that reported by in Saudi Arabia (51%) [
19]. This results were higher than demonstrated in Croatia (36%) [
21] but lower than displayed in Switzerland (70%) [
22]. However, it was stated that positive attitude of 50% and more are sufficient to ensure acceptable nutritional care [
22]. In addition, perception of importance of nutritional care declined after graduation as shown by Vetter et al. study and many doctors and educators regarded positive perception of nutritional care as an important part of clinical care enhanced better health for patients [
12,
23].
Unfortunately, more than half (52.5%) of the newly graduated doctors displayed that they were neither confident nor unconfident in providing nutrition care for patient with only 12% of them were confident and had good self efficacy to provide nutritional care for patients. This also reported by other studies done in different localities [
15,
24,
25]. This urge the need to incorporated the nutrition care training in clinical years in medical schools teaching in addition to implement training courses after graduation, as suggested by Vetter et al. study in which resident physicians knowledge and counselling skills enhanced by post graduation training [
12].
Those who have good knowledge were significantly (p=0.000) have more positive attitude and more confident than those with poor knowledge. This in agreement with that displayed by Wynn etal study in Canada that carried out among primary care doctors [
26] and Mogree et al. review, as stated improving doctors efficacy in providing care need empowering their empathy and attitude not only increasing knowledge [
27].
Most of the participants were satisfied with nutrition education that received during their teaching years in medical college but thought that clinical training is somewhat need to be continued through training courses included hands on practice sessions on real patients. This were also reported by other studies [
28,
29,
30] in which most of participant were satisfied with nutritional education in their medical schools but need future training courses.
Its worth noting that this study is a cross sectional study makes it difficult to assess cause and effect. In addition collection of data depends on a self- rating of efficacy in providing care which may be affected by social differences and ideas. Although its widely agreed that using self- reported measurement of nutrition efficacy could be used as indirect measure of real competencies [
31].But the present study provides baseline information that could help in improving medical doctors competences and in evaluating healthy nutrition as an critical part in the prevention and even management of chronic non communicable diseases. The use of validated questionnaire in which content validity were examined by professions’ in this filed, random selection of the sample and high response rate (93%) would increases confidence in our results.
Conclusion
Newly graduated medical doctors had good knowledge and positive attitudes regarding nutrition care but had low levels of perceived efficacy in proving nutrition care, this suggest the need for implementing strategies that help to enhance medical doctors confidence level in providing nutrition care during their daily practices.
Source(s) of Support: The author did not receive any type of support to complete the paper.
Conflicts of Interest
The author has no conflicts of interest to declare.
References
- Hacker, K. The Burden of Chronic Disease. Mayo Clin Proc Innov Qual Outcomes 2024, 8, 112–119, Erratum in: Mayo Clin Proc Innov Qual Outcomes 2024, 9, 100588. https://doi.org/10.1016/j.mayocpiqo.2024.11.005. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jepson, R.G.; Harris, F.M.; Platt, S.; et al. The effectiveness of interventions to change six health behaviours: A review of reviews. BMC Public Health 2010, 10, 538. [Google Scholar] [CrossRef]
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition care by primary-care physicians: Advancing our understanding using the COM-B framework. Public Health Nutr. 2020, 23, 41–52. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ball, L.; Leveritt, M.; Cass, S.; Chaboyer, W. Effect of nutrition care provided by primary health professionals on adults’ dietary behaviours: A systematic review. Fam Pract. 2015, 32, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Kraef, C.; Wood, B.; von Philipsborn, P.; Singh, S.; Peterson, S.S.; Kallestrup, P. Primary health care and nutrition. Bull World Health Organ. 2020, 98, 886–893. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nielsen, L.P.; Thomsen, K.H.; Alleslev, C.; Mikkelsen, S.; Holst, M. Implementation of nutritional care in hospitals: A qualitative study of barriers and facilitators using implementation theory. Scand J Caring Sci. 2024, 38, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Kesapragada, S.; Teli, A.; Mullur, L. Assessment of Knowledge and Attitude of Medical Students Towards Nutrition and Health: A Cross-Sectional Study. Cureus 2024, 16, e68329. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dolatkhah, N.; Aghamohammadi, D.; Farshbaf-Khalili, A.; et al. Nutrition knowledge and attitude in medical students of Tabriz University of Medical Sciences in 2017–2018. BMC Res Notes 2019, 12, 757. [Google Scholar] [CrossRef]
- Merzah, M. Trends in incidence, prevalence, and mortality of non-communicable diseases in Iraq (2003-2021). BMC Public Health 2025, 25, 374, Erratum in: BMC Public Health 2025, 25, 530. https://doi.org/10.1186/s12889-025-21743-2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench 2013, 6, 14–17. [Google Scholar] [PubMed] [PubMed Central]
- Makowske, M.; Feinman, R.D. Nutrition education: A questionnaire for assessment and teaching. Nutr J 2005, 4, 2. [Google Scholar] [CrossRef]
- Vetter, M.L.; Herring, S.J.; Sood, M.; Shah, N.R.; Kalet, A.L. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr. 2008, 27, 287–298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mogre, V.; Stevens, F.C.J.; Aryee, P.A.; et al. Nutrition Care Practices, Barriers, Competencies and Education in Nutrition: A Survey Among Ghanaian Medical Doctors. Med.Sci.Educ. 2018, 28, 815–824. [Google Scholar] [CrossRef]
- Hyska, J.; Mersini, E. Assessment of knowledge, attitudes and practices about public health nutrition among students of the University of Medicine in Tirana, Albania. South Eastern European Journal of Public Health 2023. [Google Scholar] [CrossRef]
- Ray, S.; Rajput-Ray, M.; Ball, L.; Crowley, J.; Laur, C.; Roy, S.; et al. Confidence and attitudes of doctors and dietitians towards nutrition care and nutrition advocacy for hospital patients in Kolkata, India. Journal of Biomedical Education 2015, 416021. [Google Scholar] [CrossRef]
- Alzaben, A.S.; Aljahdali, A.A.; Alasousi, L.F.; Alzaben, G.; Kennedy, L.; Alhashem, A. Nutritional Knowledge, Attitudes, and Practices among Family Physician Practitioners in Gulf Countries (Bahrain, Kuwait, Saudi Arabia, and UAE). Healthcare (Basel) 2023, 11, 2633. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Zahrani, A.M.; Al-Raddadi, R.M. Nutritional knowledge of primary health care physicians in Jeddah, Saudi Arabia. Saudi Med J. 2009, 30, 284–287. [Google Scholar] [PubMed]
- Zeldman, J.; Andrade, J.M. Identifying Physicians’ and Nurses’ Nutrition Knowledge Using Validated Instruments: A Systematic Narrative Review. Int J Nutr Food Sci. 2020, 9, 43–53. [Google Scholar] [CrossRef]
- Bawazir, Z.; Alrasheedi, A.; Aljehany, B. Nutritional Knowledge and Attitudes among Physician Interns Graduated from King Abdul-Aziz University, Jeddah, Saudi Arabia. Healthcare (Basel) 2022, 10, 1788, Erratum in: Healthcare (Basel) 2023, 11, 155. https://doi.org/10.3390/healthcare11020155. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Flynn, M.; Sciamanna, C.; Vigilante, K. Inadequate physician knowledge of the effects of diet on blood lipids and lipoproteins. Nutr J. 2003, 2, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dumic, A.; Miskulin, I.; Pavlovic, N.; Cacic Kenjeric, D.; Orkic, Z.; Miskulin, M. Attitudes toward Nutrition Care among General Practitioners in Croatia. J Clin Med. 2018, 7, 60. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Han, S.L.; Auer, R.; Cornuz, J.; Marques-Vidal, P. Clinical nutrition in primary care: An evaluation of resident physicians’ attitudes and self-perceived proficiency. Clin Nutr ESPEN. 2016, 15, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Vrkatić, A.; Grujičić, M.; Jovičić-Bata, J.; Novaković, B. Nutritional Knowledge, Confidence, Attitudes towards Nutritional Care and Nutrition Counselling Practice among General Practitioners. Healthcare 2022, 10, 2222. [Google Scholar] [CrossRef] [PubMed]
- Al-gassimi, O.; Shah, H.B.U.; Sendi, R.; et al. Nutrition competence of primary care physicians in Saudi Arabia: A cross-sectional study. BMJ Open 2020, 10, e033443. [Google Scholar] [CrossRef] [PubMed]
- Crowley, J.; Ball, L.; Han, D.Y.; McGill, A.T.; Arroll, B.; Leveritt, M.; Wall, C. Doctors’ attitudes and confidence towards providing nutrition care in practice: Comparison of New Zealand medical students, general practice registrars and general practitioners. J Prim Health Care. 2015, 7, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Wynn, K.; Trudeau, J.D.; Taunton, K.; Gowans, M.; Scott, I. Nutrition in primary care: Current practices, attitudes, and barriers. Can Fam Physician. 2010, 56, e109-16. [Google Scholar] [PubMed] [PubMed Central]
- Mogre, V.; Aryee, P.A.; Stevens, F.C.J.; et al. Future Doctors’ Nutrition-Related Knowledge, Attitudes and Self-Efficacy Regarding Nutrition Care in the General Practice Setting: A Cross-Sectional Survey. Med.Sci.Educ. 2017, 27, 481–488. [Google Scholar] [CrossRef]
- Mogre, V.; Stevens, F.; Aryee, P.A.; Scherpbier, A.J. Nutrition in Medicine: Medical Students’ Satisfaction, Perceived Relevance and Preparedness for Practice. Health Professions Education 2018, 4, 6. Available online: https://hpe.researchcommons.org/journal/vol4/iss1/6. [CrossRef]
- Sierpina, V.S.; Welch, K.; Devries, S.; Eisenberg, D.; Levine, L.; McKee, J.; Dalal, M.; Mendoza, P.; Gutierrez, J.; Robertson, S.; Rosales, D. What Competencies Should Medical Students Attain in Nutritional Medicine? Explore (NY) 2016, 12, 146–147. [Google Scholar] [CrossRef] [PubMed]
- Gramlich, L.M.; Olstad, D.L.; Nasser, R.; Goonewardene, L.; Raman, M.; Innis, S.; Wicklum, S.; Duerksen, D.; Rashid, M.; Heyland, D.; Armstrong, D.; Roy, C. Medical students’ perceptions of nutrition education in Canadian universities. Appl Physiol Nutr Metab. 2010, 35, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Mihalynuk, T.V.; Scott, C.S.; Coombs, J.B. Self-reported nutrition proficiency is positively correlated with the perceived quality of nutrition training of family physicians in Washington State. Am J Clin Nutr. 2003, 77, 1330–1336. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).