1. Introduction
The clavicle is among the more unique human bones. It serves as a strut for the upper extremity and is the only bony connection between it and the axial skeleton. Loads on the upper extremity are transmitted to the thorax through the clavicle. Combined with its superficial location, these factors make the clavicle the most fractured human bone.[
1,
2]
Middle one-third clavicle fractures account for approximately 80% of clavicle fractures and have traditionally been treated non-operatively based on Neer’s work.[
3] However, Hill, et al studied non-operatively treated, displaced mid-shaft clavicle fracture outcomes, and found patients often fared poorly.[
4] They recommended operative fixation for displaced mid-shaft clavicle fractures. In a randomized clinical trial, the Canadian Orthopaedic Trauma Society found operative fixation of displaced adult mid-shaft clavicle fractures resulted in improved functional outcomes and lower rates of nonunion as well as malunion when compared with non-operative treatment.[
5]
Unfortunately, the orthopedic and vascular literature contains reports of both early and late limb-threatening complications associated with plate-screw constructs for mid-shaft clavicle fractures.[
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16] Unicortical screw fixation may reduce vascular injury risk to subclavian vessels near mid-shaft fractures as the inferior clavicular cortex is not violated with instrumentation utilizing this technique. A hybrid approach utilizing central unicortical locked screws was proposed and whose biomechanical utility was shown.[
17] However, it is unclear if unicortical screws alone (and associated plate fixation) is biomechanically adequate for mid-shaft clavicle fractures. We hypothesized 3.5 mm pelvic reconstruction plates with only unicortical screw fixation would provide comparable stability to more traditional bicortical compression screw constructs with the same plate type.
2. Materials and Methods
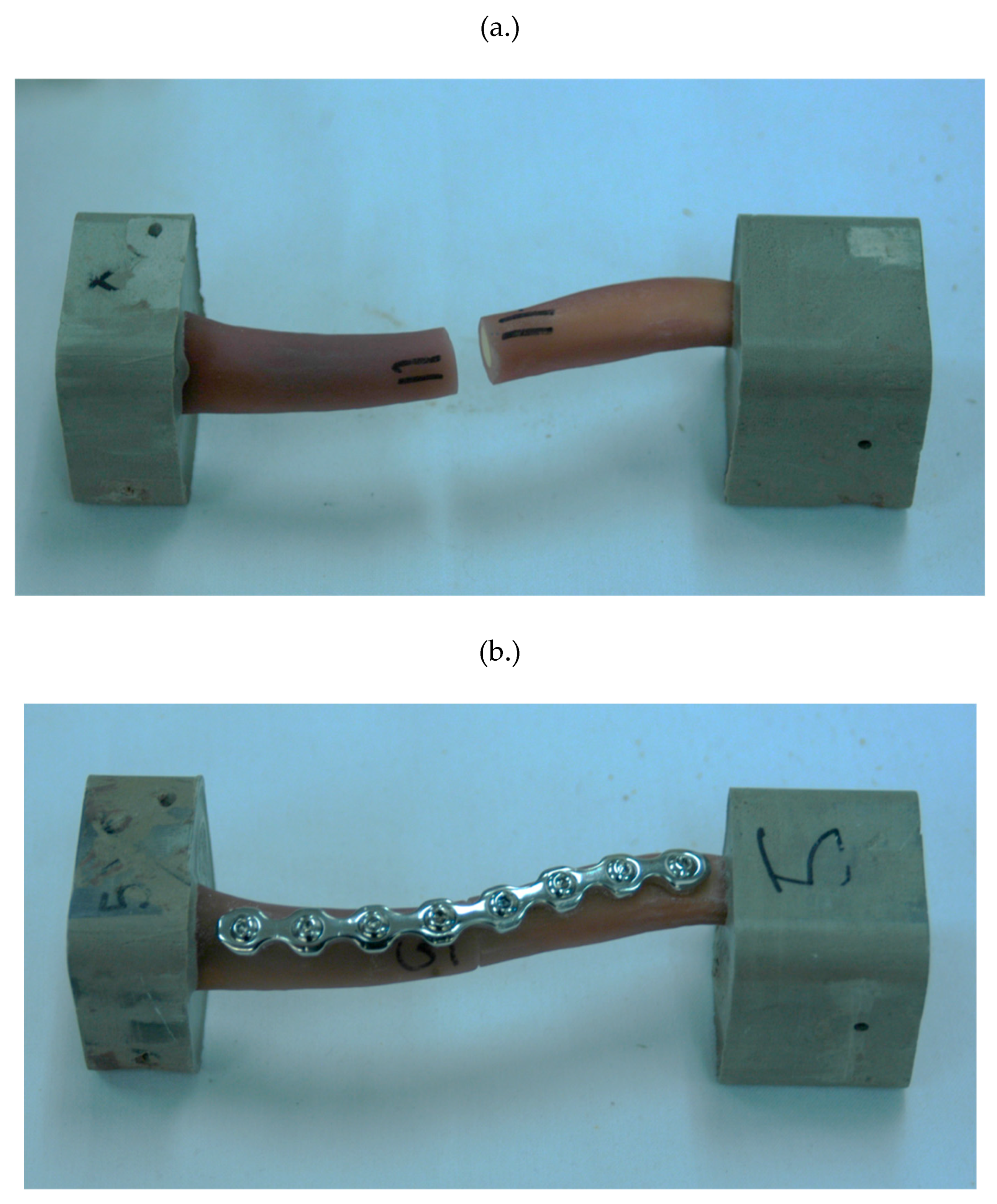
Ten fourth-generation composite clavicle models (Sawbones, Pacific Research Laboratories, Vashon, WA) were used in this study. Each of these synthetic clavicles was designed to replicate the properties of real human bone and had a manufactured mid-shaft osteotomy, meaning an artificial fracture was introduced at the middle section of the bone. These clavicle specimens were randomly assigned to one of two experimental groups for further study.
To ensure consistency in the surgical technique, each clavicle was carefully realigned (reduced) and surgically repaired using standard orthopedic trauma procedures. A single author (CWH) performed all repairs under the close supervision of two experienced attending orthopedic surgeons (EVF and MAM). For each specimen, a contoured, eight-hole, second-generation 3.5 mm locking pelvic reconstruction plate (Synthes, Paoli, PA) was placed on the superior surface of the clavicle to provide structural support and stabilization (
Figure 1).
The study divided the specimens into two groups based on the type of screws used for fixation. In the first group, standard bi-cortical compression screws were used to secure the plate. These screws were tightened to a precise torque using a 1.5 Newton-meter (Nm) torque-limiting driver to ensure uniform tension and secure fixation. In the second group, uni-cortical locking screws were used instead, also tightened with the same 1.5 Nm torque-limiting driver. To maintain consistency, all plates were shaped in the same way using standard handheld plate benders before being affixed to the bone models. In both groups, four screws were placed on each side of the osteotomy to ensure a balanced and stable repair.
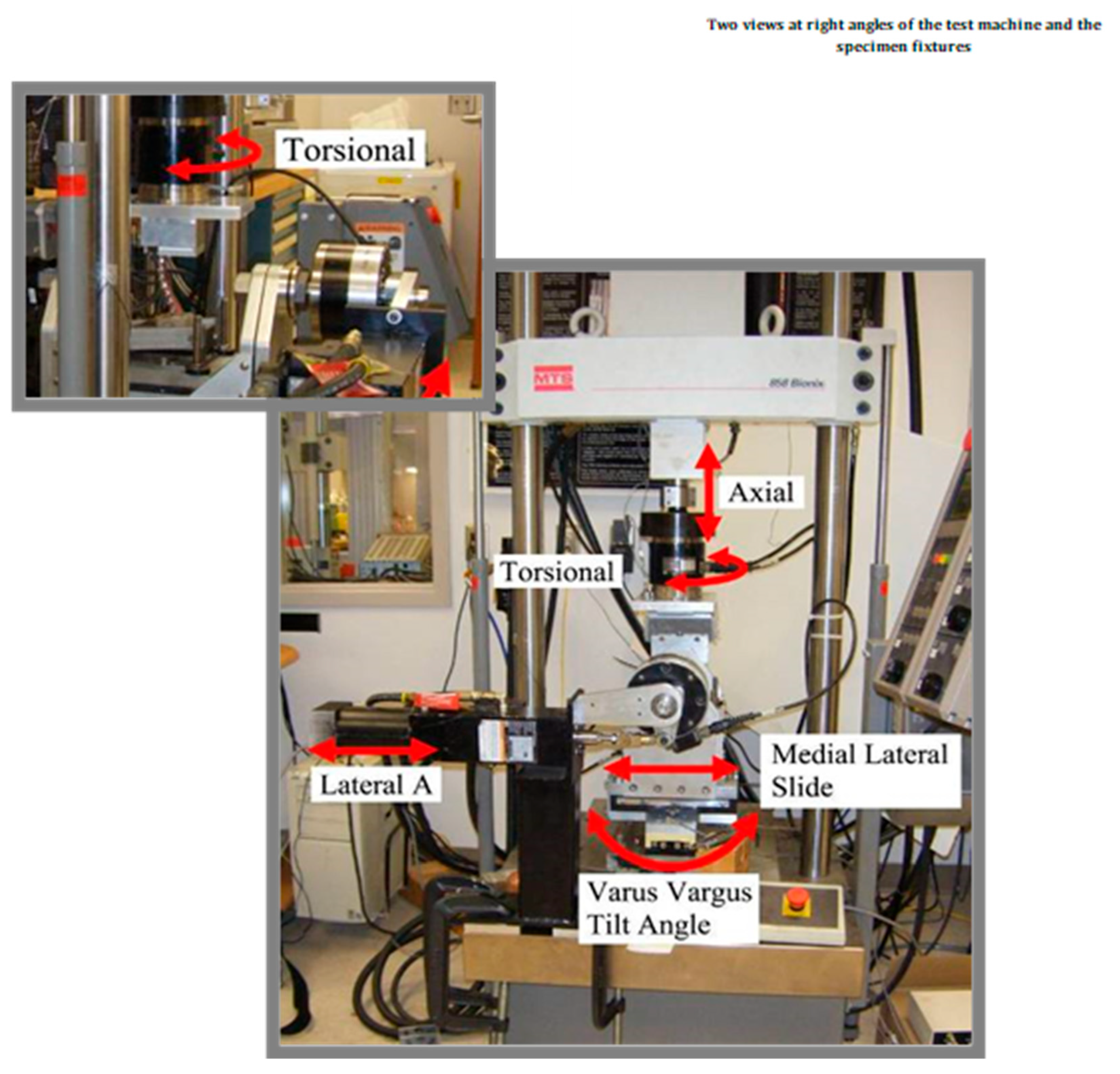
Once the repairs were complete, all specimens were securely embedded (potted) in liquid molding plastic to hold them in place for mechanical testing. The repaired clavicles were then subjected to stiffness testing using a four-axis MTS servohydraulic testing machine. This machine operated under displacement control and tested the specimens under three different loading conditions: axial rotation, anterior/posterior bending, and cephalad/caudad bending (
Figure 2). These loading modes simulated different types of mechanical stress that clavicles may experience in real-life situations, such as twisting, forward-and-backward bending, and upward-and-downward bending.
The mechanical testing procedure included an initial warm-up loop to condition the specimens before data collection. After this, three continuous cycles of mechanical loading were performed, with data recorded at a rate of 100Hz. The range of displacement for each test was determined by conducting a preliminary scouting trial. The final testing parameters were set as follows: axial rotation was tested with a range of ±8.0 degrees, anterior/posterior bending with a range of ±7.2 degrees, and cephalad/caudad bending with a range of +7.2 degrees to -3.6 degrees.
The first loading test conducted was anterior/posterior (AP) bending. In this test, the proximal (closer to the center of the body) end of the clavicle specimen was firmly fixed to the testing machine, while the distal (farther from the center of the body) end was placed in a custom-built movable fixture. This fixture allowed the specimen to bend naturally at the osteotomy site while minimizing unwanted shear forces. Next, the specimens were rotated 180 degrees to undergo cephalad/caudad bending testing, using the same fixture setup. Finally, the axial rotation test was performed by applying torque to the specimen through a piston actuator, simulating a twisting force on the clavicle.
To analyze the results, the collected data were grouped based on the type of screws used for fixation. Descriptive statistical analysis was performed to compare the stiffness of the two groups. A two-sample t-test was used to determine whether there were significant differences between the groups. The significance threshold was set at a p-value of ≤ 0.05, meaning that differences with a p-value at or below this level were considered statistically significant.
3. Results
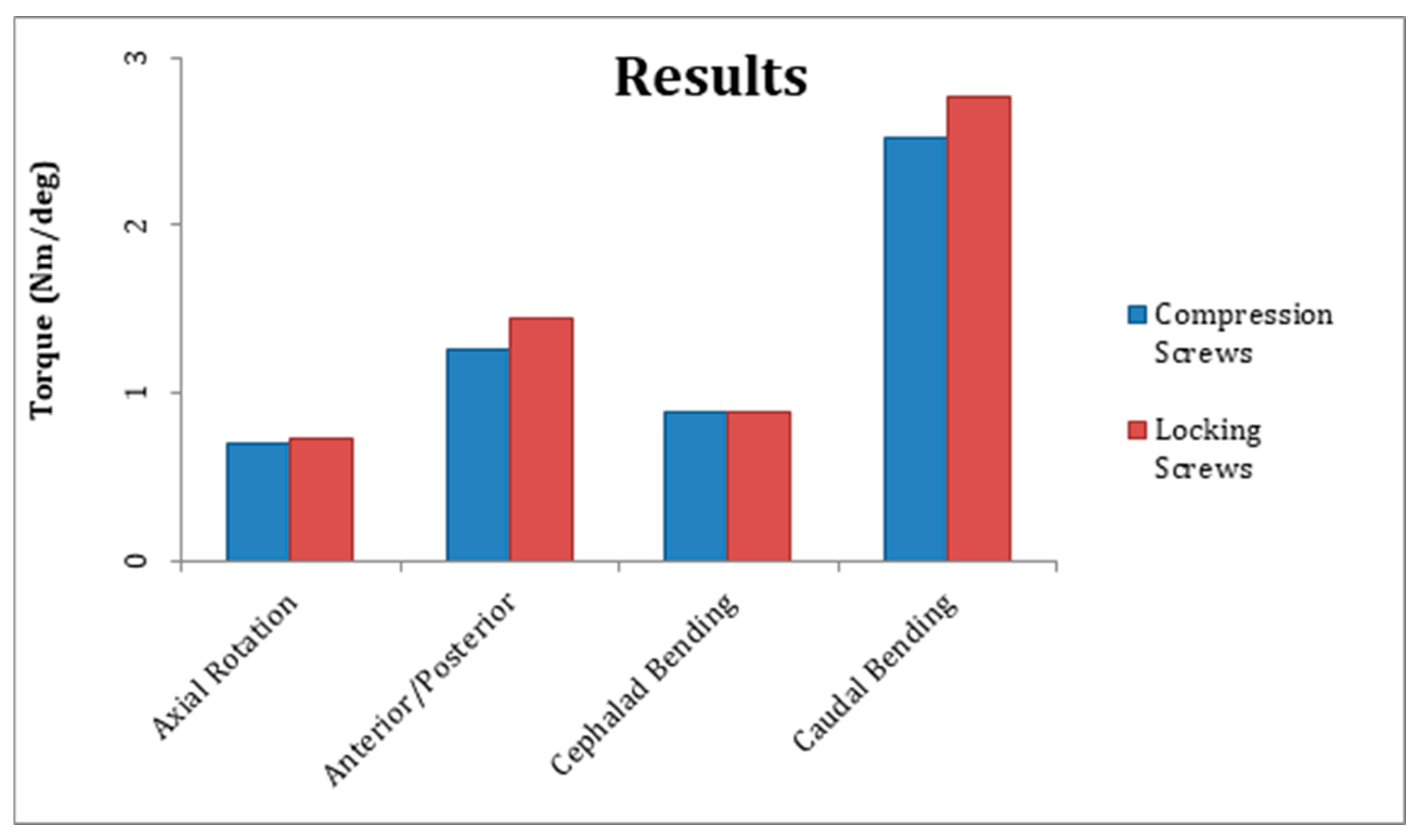
The mean steady-state construct stiffness for axial rotation, cephalad bending, and caudal bending was similar between groups one and two but differed significantly in AP bending (
Table 1,
Figure 3). The mean steady-state construct stiffness for AP bending was 1.255±0.058 Nm/deg for group one and 1.442±0.065 Nm/deg for group two; the difference was significant (p=0.0013). The mean steady-state construct stiffness for axial rotation was 0.701±0.08 Nm/deg for group one and 0.726±0.03 Nm/deg for group two; the difference was not significant (p=0.581). The mean steady-state construct stiffness for cephalad bending was 0.889±0.064 Nm/deg for group one and 0.880±0.044 Nm/deg for group two; the difference was not significant (p=0.807). The mean steady-state construct stiffness for caudal bending was 2.523±0.29 Nm/deg for group one and 2.774±0.25 Nm/deg for group two; the difference was not significant (p=0.182).
4. Discussion
Following the Canadian Orthopaedic Society’s findings that operative fixation of displaced adult mid-shaft fractures resulted in improved functional outcomes with reduced nonunion and malunion (when compared with non-operative treatment), one assumes clavicle fixation rates would increase.[
5] Yet, clavicle fracture fixation is not without risk. Intra-operative or even post-operative vascular injury can be limb threatening.[
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16] Plates and screws are familiar to orthopedic surgeons and provide excellent clavicular shaft rotational control, and constructs that do not violate the inferior clavicular cortex may allow surgical treatment while reducing vascular injury risk. Therefore, the purpose of this study was to perform a biomechanical comparison of mid-shaft clavicle fracture fixation constructs with only unicortical locked screws and those with standard bicortical compression screws.
Previously, Collinge, et. al. described anterior clavicular plate fixation to improve rigidity and decrease vascular injury risk.[
18] But, this technique requires some deltoid detachment laterally and may not allow vascular protection in all. Moreover, Robertson, et. al. suggested anterior-inferior reconstruction plates might be subjected to loads that could cause early mechanical failure.[
19] In fact, Iannotti, et. al. found superior plating of mid-shaft clavicle osteotomies was biomechanically advantageous to anterior plating.[
20] They also found 3.5 mm LCDC plates were better than 2.7 mm DC plates or 3.5 mm reconstruction plates. But it is unclear if improved stability afforded by LCDC plates is clinically important. Also of note, The Canadian group found hardware removal incidence declined with contoured plates.[
5] Finally, in a radiological study, Sinha, et al. defined safe zones for drilling when fixing clavicle fractures, but Hussey, et al. showed no difference in neurovascular injury risk between superior and anterior plate placement.[
21,
22]
Our study is not without limitations. We did not create a gap at the fracture site to simulate comminution. Yet, the dynamic healing process changes the overall local environment in vivo such that the loss of stability (due to comminution) changes continually with healing. Second, we only tested a transverse fracture model. However, oblique fracture lines frequently allow the utilization of an interfragmentary screw that can dramatically stabilize constructs. We felt the utilization of a transverse fracture line would more closely approximate an in vivo environment. Third, we utilized 4th generation composite fracture models. It is possible that cadaver specimens may have changed our results. However, we wished to eliminate bone density variability as one variable that could significantly alter results, so we used consistent specimens. Fourth, we utilized 2nd generation pelvic reconstruction plates that may not be used by some surgeons. However, these plates also allow excellent contouring to bony surfaces. We recognize that these limitations may not allow our results to be generalizable to all clavicle fractures nor the plating systems used to address them. Yet, these limitations do not affect our ability to adequately evaluate the biomechanical differences between unicortical locked screw fixation constructs versus standard bicortical screw fixation constructs in a transverse osteotomy mid-shaft clavicle fracture model in 4th generation composite specimens.
5. Clinical Relevance
Several studies have revealed good outcomes following plate/screw fixation of displaced mid-shaft clavicle fractures.[
4,
5,
18] Catastrophic vascular injury risk mitigation with familiar fixation that does not violate inferior clavicular cortices may influence mid-shaft clavicle fracture treatment algorithms.
6. Conclusion
In a transverse mid-shaft clavicle osteotomy model, superiorly placed bicortical fixation with 3.5 mm pelvic reconstruction plates did not provide greater rigidity than similarly placed unicortical locking 3.5 mm pelvic reconstruction plate/screw fixation constructs. Unicortical locking fixation provided greater rigidity in AP bending.
Author Contributions
Conceptualization of this project was the work of Drs. Fehringer, Mormino, Hartman, Branting, and Haider. Methodology was conceived of by Drs. Haider and Hartman. Appropriate software, validation, and jig configuration was the work of Dr. Haider. Formal analysis was performed by Drs. Haider and Hartman. Drs Mormino, Hartman, and Branting performed the investigation and solicitated resources from Synthes. Data curation was performed by Drs. Branting and Hartman. Original draft preparation was performed by Drs. Hartman and Fehringer. Review and editing was performed by Drs. Zitsch, Lackner, and Fehringer. Visualization and instrumentation was performed by Drs. Mormino, Branting, and Hartman. Drs. Fehringer and Haider supervised, and project administrator was Dr. Hartman. Funding acquisition was through Dr. Hartman. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a Depuy-Synthes grant as well as their donation of all hardware and instrumentation.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest as it relates to this study. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Post M: Current Concepts in the Treatment of Fractures of the Clavicle. Clinical Orthopaedics and Related Research 1989; 245: 89-101.
- Harrington MA, Keller TS, Seiler J, et al. (1993) Geometric properties and the predicted mechanical behavior of adult human clavicles. J Biomech 26, 417–426.
- Neer CS II. Nonunion of the clavicle. JAMA. 1960; 172:1006-1011.
- Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997 Jul;79(4):537-9. [CrossRef] [PubMed]
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007 Jan;89(1):1-10. [CrossRef] [PubMed]
- Johnson B, Thursby P. Subclavian artery injury caused by a screw in a clavicular compression plate. Cardiovasc Surg 1996; 4: 414–5.
- Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997; 43:778–783. [CrossRef]
- Shackford SR. Taming of the screw: a case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma 2003; 55: 840–3.
- Kitsis CK, Marino AJ, Krikler SJ, Birch R. Late complications following clavicular fractures and their operative management. Injury. 2003 Jan;34(1):69-74. [CrossRef] [PubMed]
- Ding M, Hu J, Ni J, Lv H, Song D, Shu. Iatrogenic subclavian arteriovenous fistula: rare complication of plate osteosynthesis of a clavicle fracture. C. Orthopedics. 2012 Feb 17;35(2): e287-9. [CrossRef] [PubMed]
- Clitherow HD, Bain GI. Association between screw prominence and vascular complications after clavicle fixation. Int J Shoulder Surg. 2014 Oct;8(4):122-6. [CrossRef] [PubMed]
- Perera KG, Clifford C, Maddock LJ. Subclavian artery injury secondary to clavicular plate fixation: a novel operative approach. Surg Case Rep. 2015 Apr 15;2015(4): rjv044. [CrossRef] [PubMed]
- Stillwell A, Ioannou C, Daniele L, Tan SL. Osteosynthesis for clavicle fractures: How close are we to penetration of neurovascular structures. Injury. 2017 Feb;48(2):460-463. [CrossRef]
- Pallett SJC, Singh I, Rady N, Goshai H. Delayed Subclavian Artery Aneurysm Following Fixation of a Clavicular Fracture. Vasc Endovascular Surg. 2018 Aug;52(6):459-462. [CrossRef]
- Lewis SD, Chew FS. Clavicle fixation screw impingement causing subclavian artery pseudoaneurysm. Radiol Case Rep. 2019 Jul 29;14(9):1148-1150. [CrossRef]
- Chuaychoosakoon C, Suwanno P, Boonriong T, Suwannaphisit S, Klabklay P, Parinyakhup W, Maliwankul K, Duangnumsawang Y, Tangtrakulwanich. Patient Position is Related to the Risk of Neurovascular Injury in Clavicular Plating: A Cadaveric Study. B. Clin Orthop Relat Res. 2019 Dec;477(12):2761-2768.
- Rawlings M, Knox D, Patel M, Ackland D. A hybrid approach to mid-shaft clavicle fixation. Injury. 2016 Apr; 47(4): 893-8. [CrossRef] [PubMed]
- Collinge C, Devinney S, Herscovici D, DiPasquale T, Sanders R. Anterior-inferior plate fixation of middle-third fractures and non-unions of the clavicle. J Orthop Trauma. 2006 Nov-Dec;20(10):680-6. [CrossRef] [PubMed]
- Robertson, Claire, et al. “Reconstruction Plates for Stabilization of Mid-Shaft Clavicle Fractures: Differences between Nonlocked and Locked Plates in Two Different Positions.” Journal of Shoulder and Elbow Surgery, vol. 18, no. 2, 2009, pp. 204–09. [CrossRef]
- Iannotti MR, Crosby LA, Stafford P, Grayson G, Goulet R. Effects of plate location and selection on the stability of midshaft clavicle osteotomies: a biomechanical study. J Shoulder Elbow Surg. 2002 Sep-Oct;11(5):457-62. [CrossRef] [PubMed]
- Sinha A, Edwin J, Sreeharsha B, Bhalaik V, Brownson P. A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Joint Surg Br. 2011 Sep;93(9):1247-52. [CrossRef] [PubMed]
- Hussey MM, Chen Y, Fajardo RA, Dutta AK. Analysis of neurovascular safety between superior and anterior plating techniques of clavicle fractures. J Orthop Trauma. 2013 Nov;27(11):627-32. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).