Submitted:
25 April 2025
Posted:
28 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
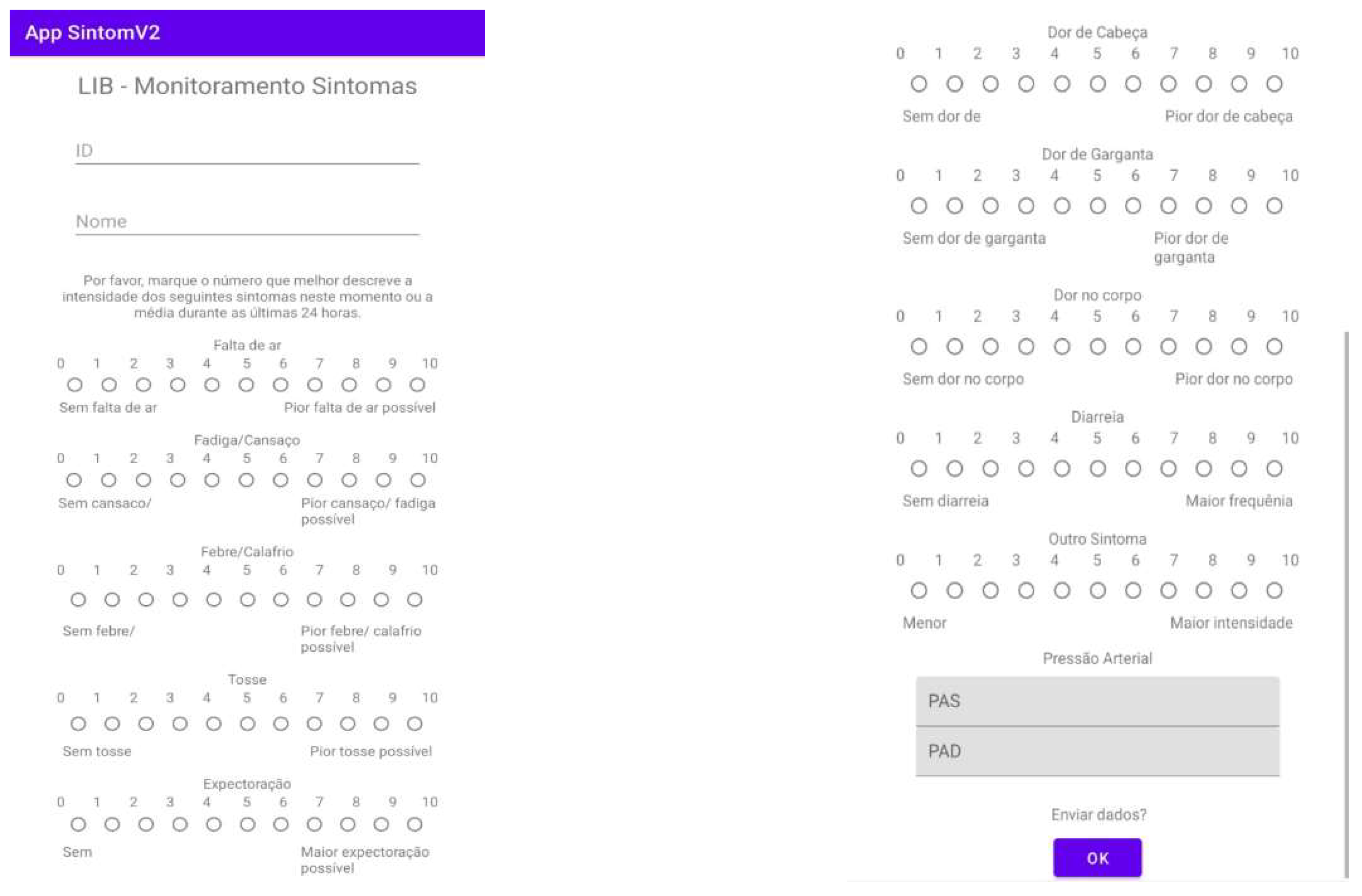
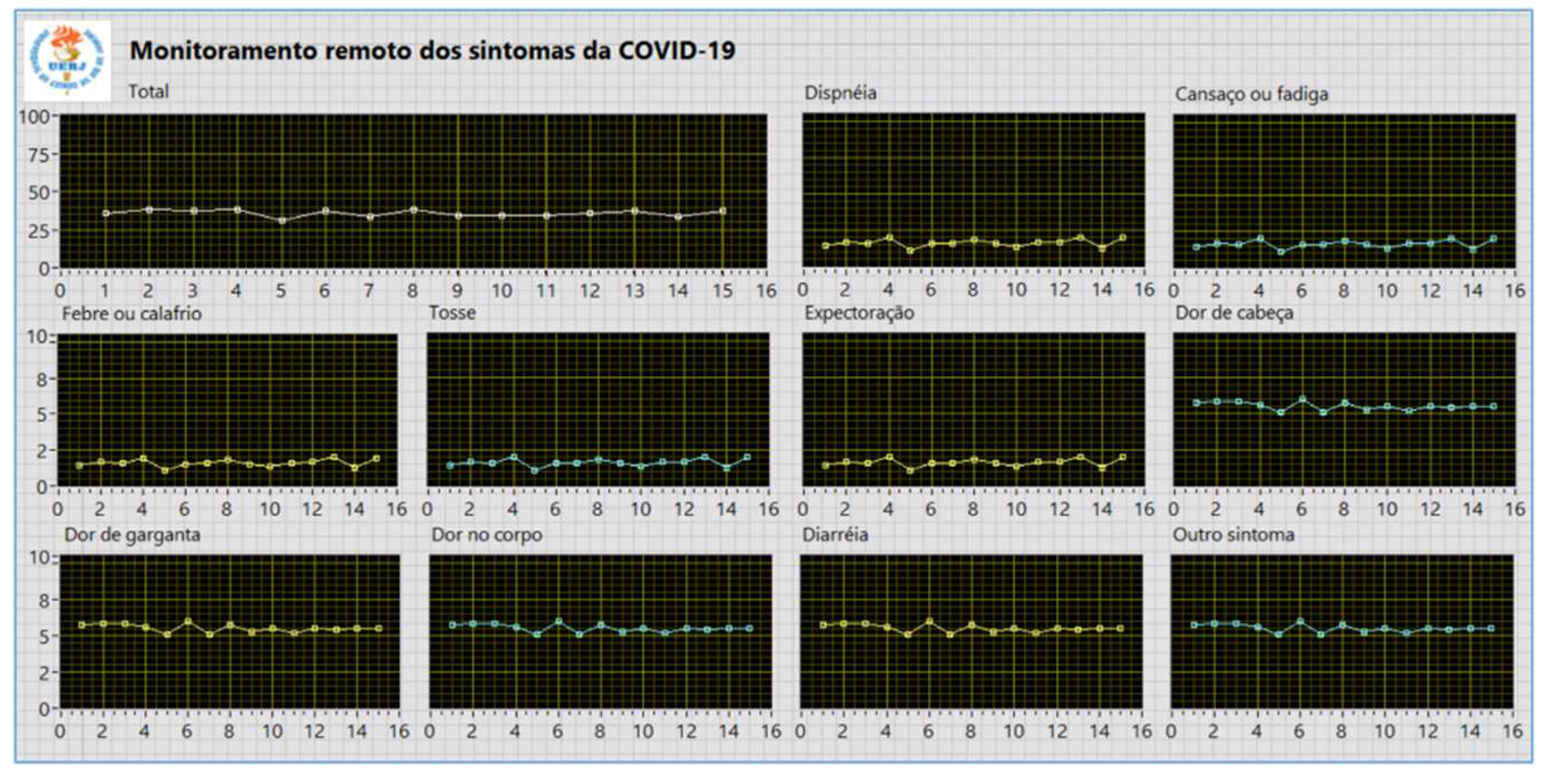
2. Materials and Methods
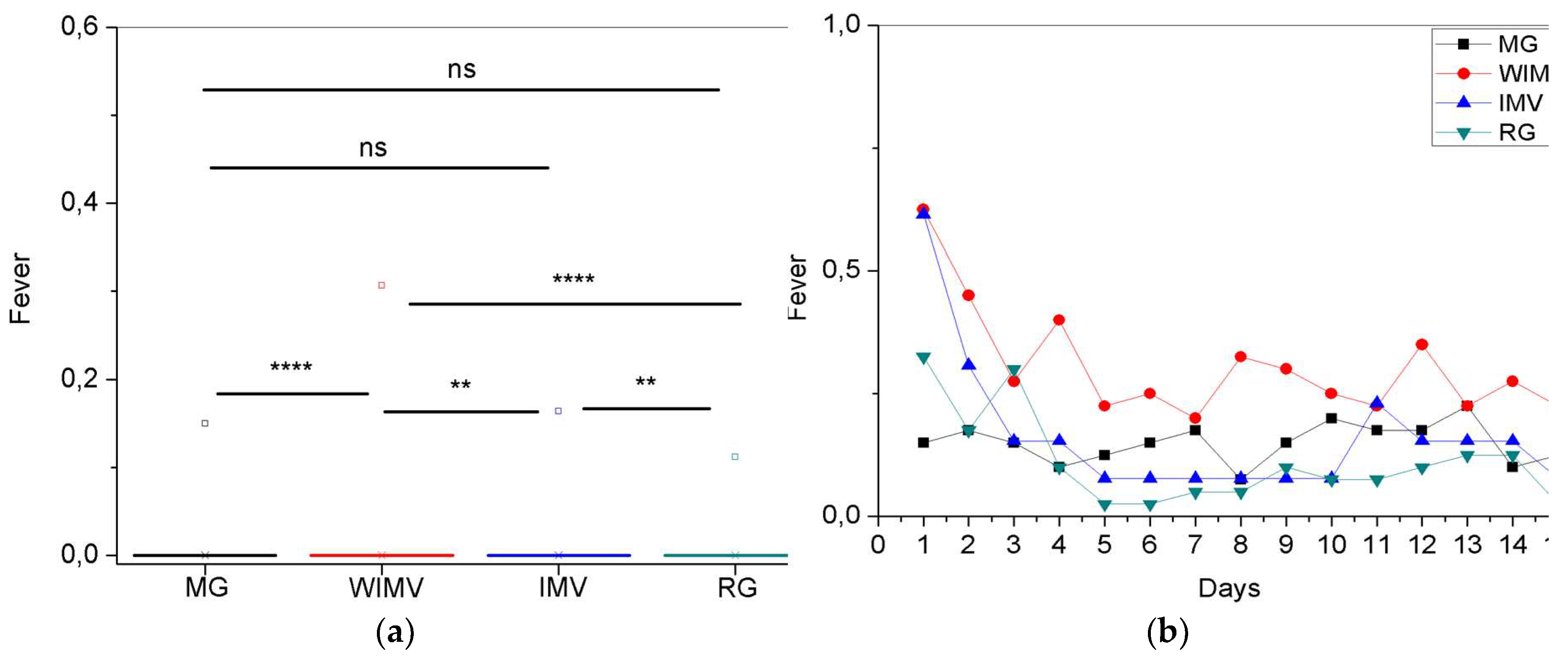
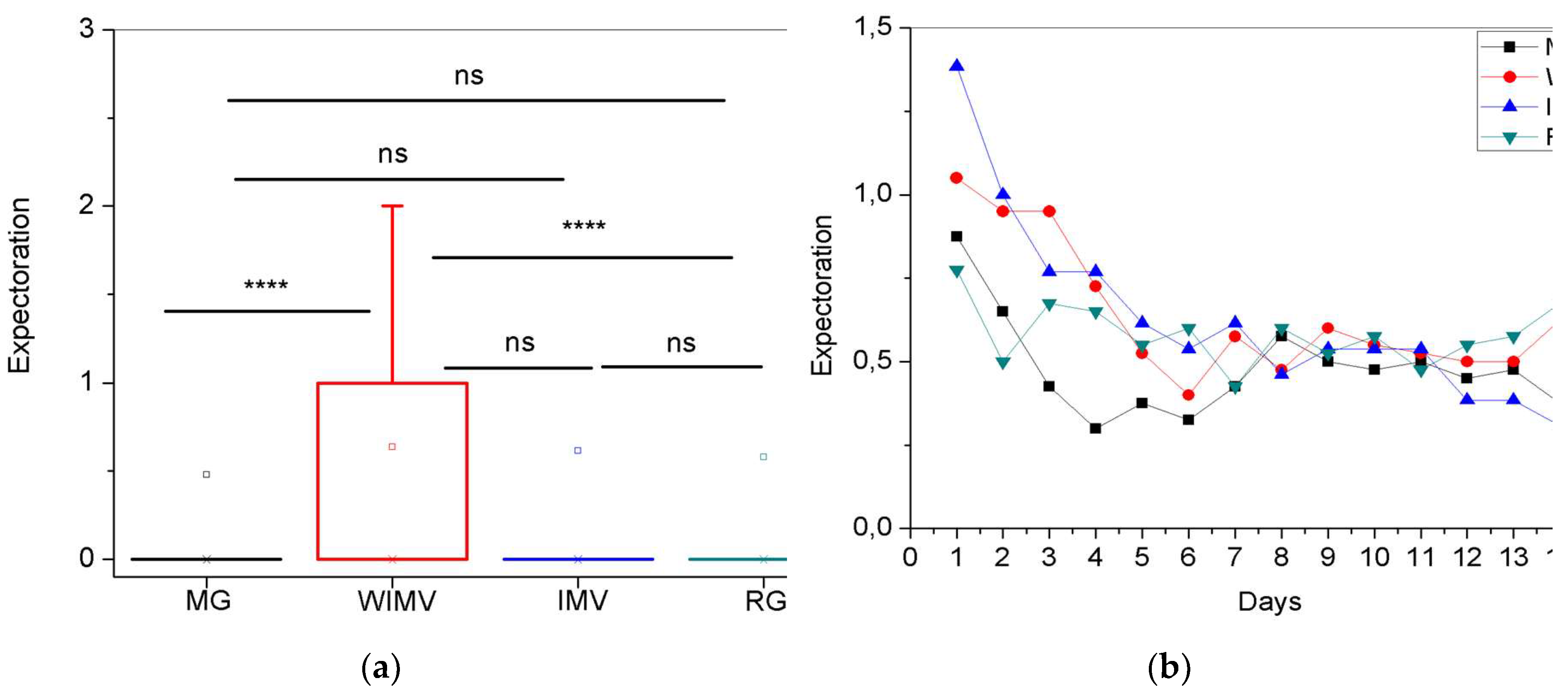
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| BP | Blood pressure |
| CEP/HUPE | Research Ethics Committee of Pedro Ernesto University Hospital |
| COVID-19 | Coronavirus Disease 2019 |
| DBP | Diastolic Blood Pressure |
| ICU | Intensive Care Unit |
| IMV | With invasive mechanical ventilation group |
| MG | Mild group |
| n | number of patients |
| NIV | Non-invasive ventilation |
| ns | not significant |
| RG | Reinfection group |
| RPM | Remote patient monitoring |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SBP | Systolic Blood Pressure |
| SD | Standard deviation |
| WIMV | Without invasive mechanical ventilation group |
Appendix A
Appendix A.1
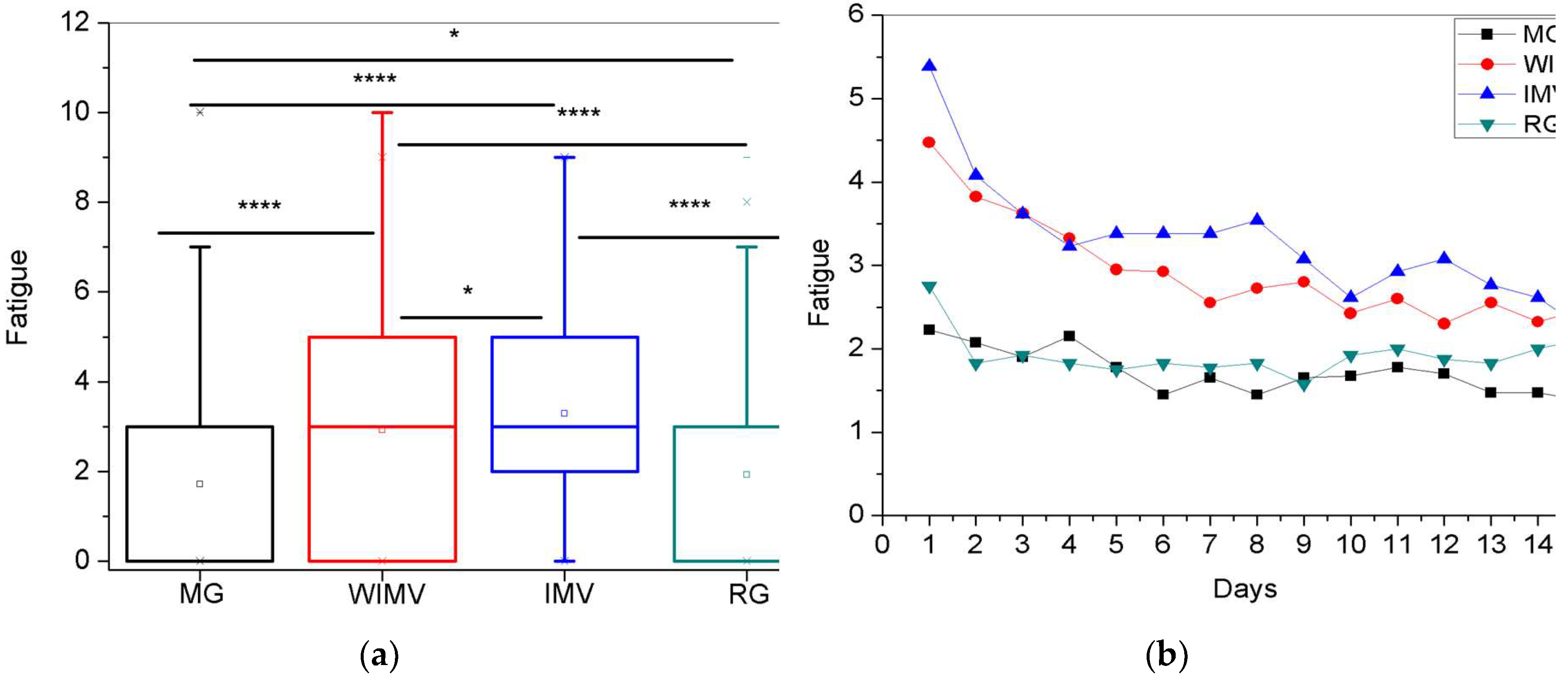
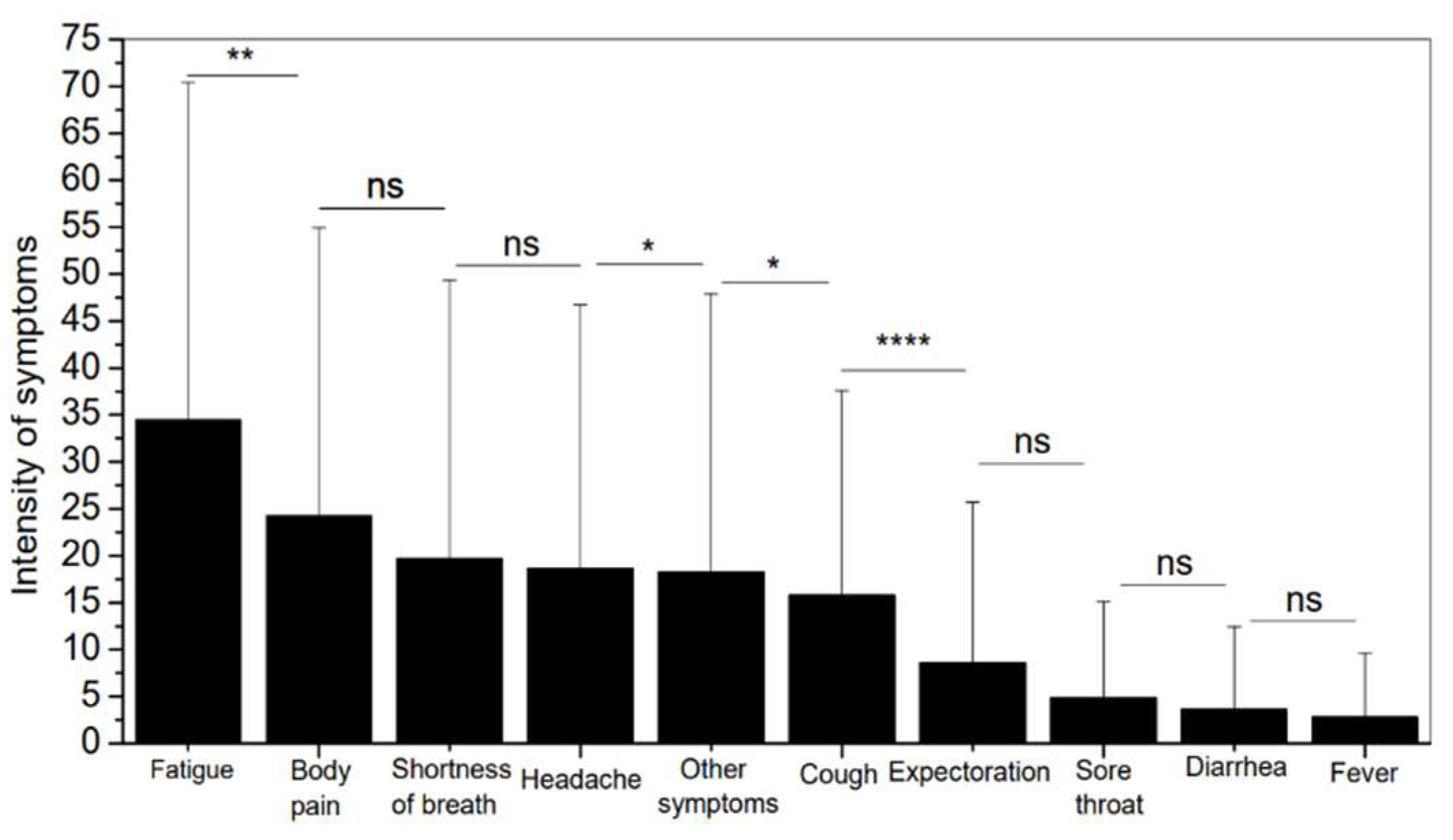
| Fatigue | 34.44 ± 35.99 |
| Body pain | 24.24 ± 30.67 |
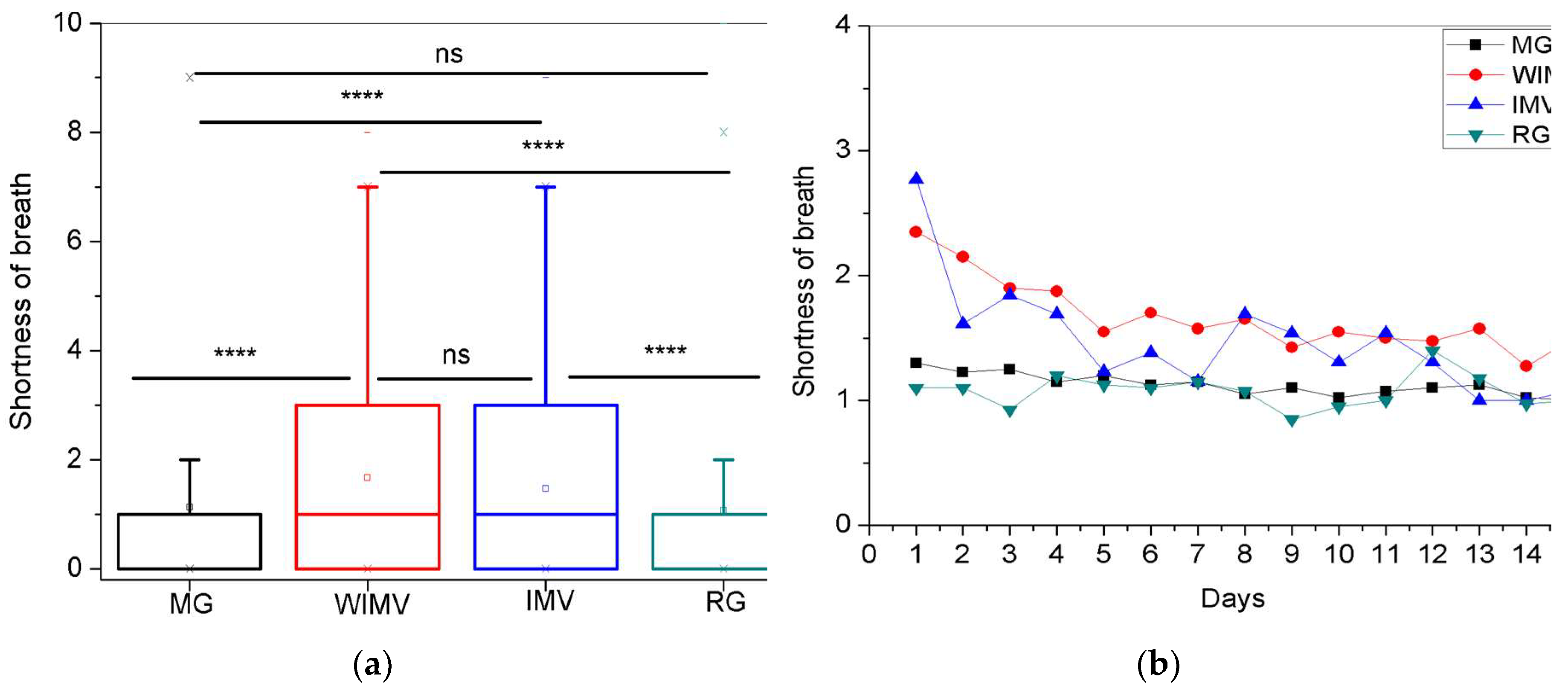
| Shortness of breath | 19.63 ± 29.73 |
| Headache | 18.66 ± 28.07 |
| Other symptoms | 18.28 ± 29.62 |
| Cough | 15.77 ± 21.85 |
| Expectoration | 8.56 ± 17.11 |
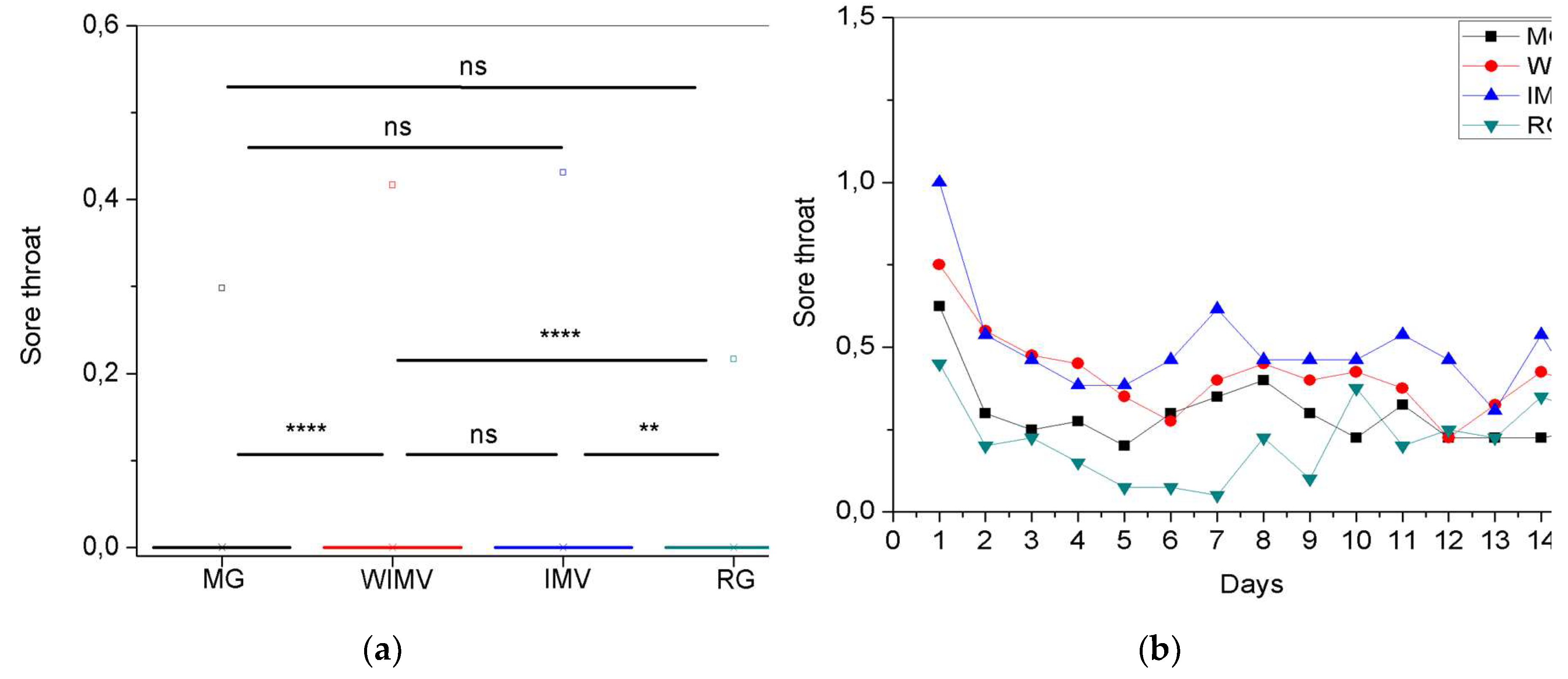
| Sore throat | 4.83 ± 10.28 |
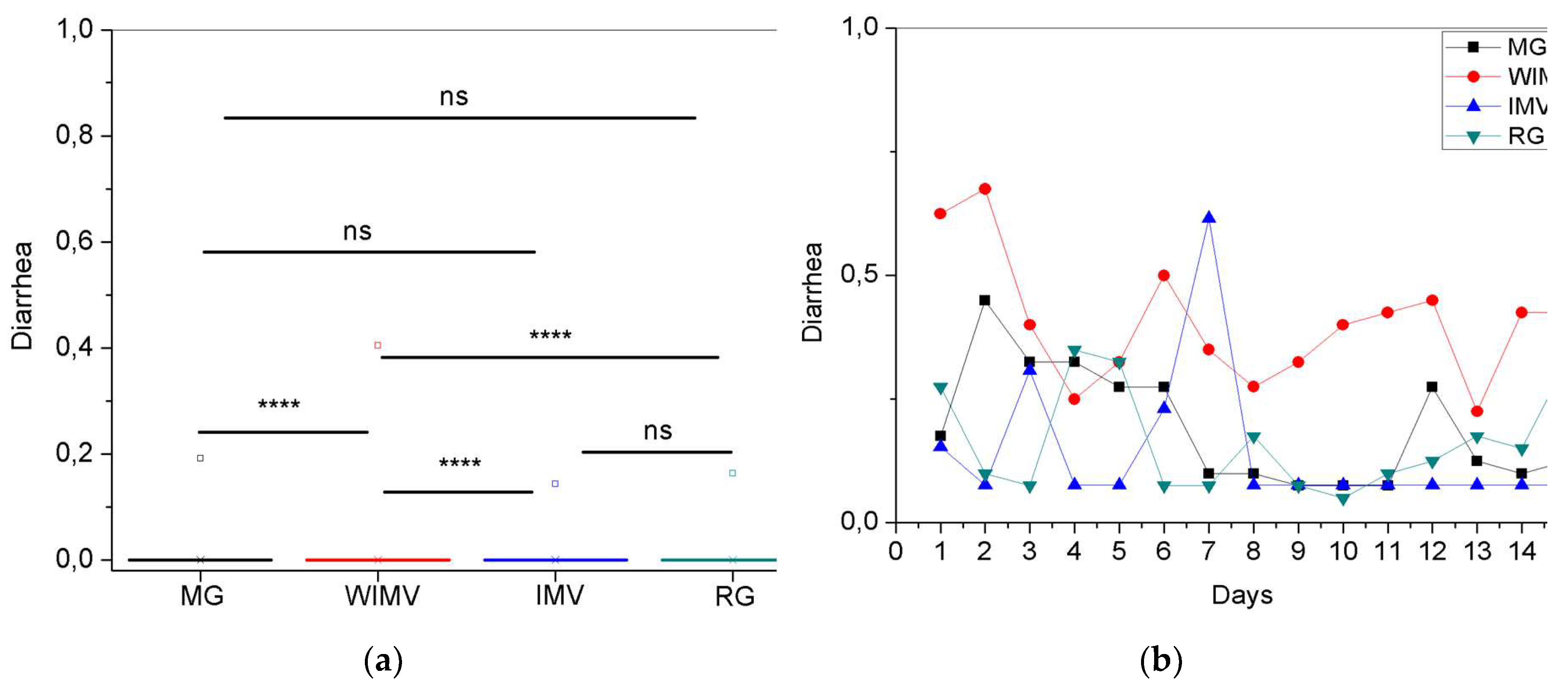
| Diarrhea | 3.63 ± 8.79 |
| Fever | 2.80 ± 6.82 |
Appendix A.2
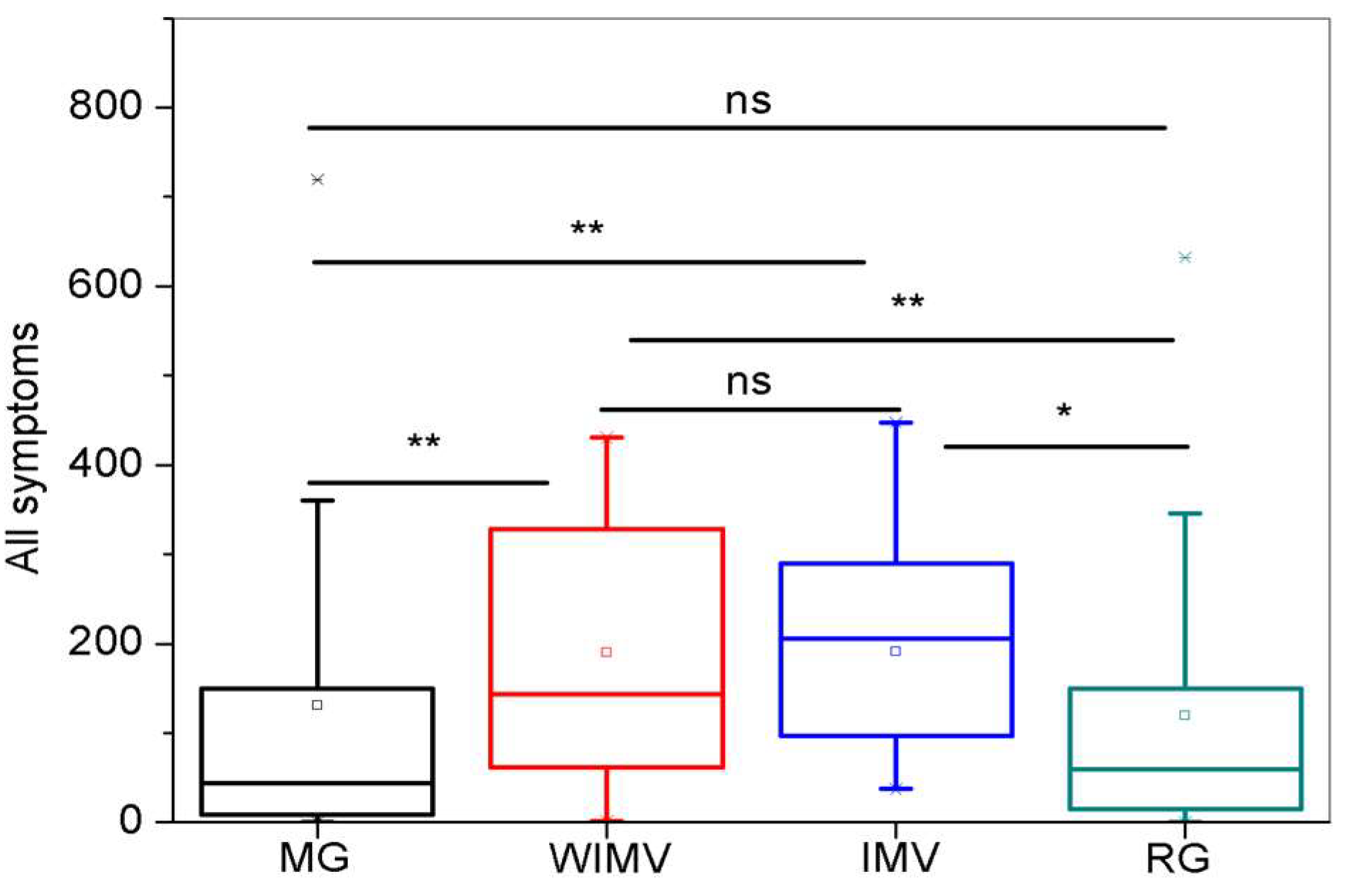
| IMV | 190.61 ± 129.34 |
| WIMV | 190.10 ± 134.48 |
| MG | 130.42 ± 189.37 |
| RG | 119.17 ± 146.91 |
References
- Landete, P.; Quezada Loaiza, C.A.; Aldave-Orzaiz, B.; Muñiz, S.H.; Maldonado, A.; Zamora, E.; Sam Cerna, A.C.; Del Cerro, E.; Alonso, R.C.; Couñago, F. Clinical features and radiological manifestations of COVID-19 disease. World journal of radiology 2020, 12, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Symptoms of COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Acessado em 25/06/2024 (accessed on 25/06/2024).
- Raveendran, A.; Jayadevan, R.; Sashidharan, S. Long COVID: an overview. Diabetes & Metabolic Syndrome: Clinical Research and Reviews 2021, 15, 869–875. [Google Scholar]
- Gordon, W.J.; Henderson, D.; DeSharone, A.; Fisher, H.N.; Judge, J.; Levine, D.M.; MacLean, L.; Sousa, D.; Su, M.Y.; Boxer, R. Remote patient monitoring program for hospital discharged COVID-19 patients. Applied clinical informatics 2020, 11, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Bruera, E.; Kuehn, N.; Miller, M.J.; Selmser, P.; Macmillan, K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. Journal of palliative care 1991, 7, 6–9. [Google Scholar] [CrossRef]
- Wan, S.; Xiang, Y.; Fang, W.; Zheng, Y.; Li, B.; Hu, Y.; Lang, C.; Huang, D.; Sun, Q.; Xiong, Y. Clinical features and treatment of COVID-19 patients in northeast Chongqing. Journal of medical virology 2020, 92, 797–806. [Google Scholar] [CrossRef]
- Abate, S.M.; Checkol, Y.; Mantedafro, B.; Basu, B.; Ethiopia, D. Prevalence and risk factors of mortality among hospitalized patients with COVID-19: a systematic review and meta-analysis. Bull World Health Organ 2020, 10, 6–31. [Google Scholar]
- Soeroto, A.Y.; Soetedjo, N.N.; Purwiga, A.; Santoso, P.; Kulsum, I.D.; Suryadinata, H.; Ferdian, F. Effect of increased BMI and obesity on the outcome of COVID-19 adult patients: A systematic review and meta-analysis. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020, 14, 1897–1904. [Google Scholar]
- Qadar, S.M.Z.; Naz, H.; Shamim, S.; Hashim, F.; Ahmed, S.; Kumar Mehraj, S. Prevalence of Obesity and its Effects in Patients With COVID-19: A Systematic Review and Meta-analysis. Hospital Pharmacy 2024, 59, 341–348. [Google Scholar] [CrossRef]
- Reddy, R.K.; Charles, W.N.; Sklavounos, A.; Dutt, A.; Seed, P.T.; Khajuria, A. The effect of smoking on COVID-19 severity: A systematic review and meta-analysis. Journal of medical virology 2021, 93, 1045–1056. [Google Scholar] [CrossRef]
- Umnuaypornlert, A.; Kanchanasurakit, S.; Lucero-Prisno, D.E.I.; Saokaew, S. Smoking and risk of negative outcomes among COVID-19 patients: A systematic review and meta-analysis. Tobacco induced diseases 2021, 19, 1–13. [Google Scholar] [CrossRef]
- Barthélémy, H.; Mougenot, E.; Duracinsky, M.; Salmon-Ceron, D.; Bonini, J.; Péretz, F.; Chassany, O.; Carrieri, P. Smoking increases the risk of post-acute COVID-19 syndrome: Results from a French community-based survey. Tobacco Induced Diseases 2022, 20, 1–10. [Google Scholar] [CrossRef]
- Hossain, M.A.; Hossain, K.A.; Saunders, K.; Uddin, Z.; Walton, L.M.; Raigangar, V.; Sakel, M.; Shafin, R.; Hossain, M.S.; Kabir, M.F. Prevalence of long COVID symptoms in Bangladesh: a prospective inception cohort study of COVID-19 survivors. BMJ global health 2021, 6, e006838–e006852. [Google Scholar] [CrossRef]
- Daanen, H.; Bose-O’Reilly, S.; Brearley, M.; Flouris, D.A.; Gerrett, N.M.; Huynen, M.; Jones, H.M.; Lee, J.K.W.; Morris, N.; Norton, I. COVID-19 and thermoregulation-related problems: practical recommendations. Temperature 2021, 8, 1–11. [Google Scholar] [CrossRef]
- Ahmad, S.; Rehman, T. Thermoregulation and fever: A brief review. International Journal of Homoeopathic Sciences 2018, 2, 35–37. [Google Scholar] [CrossRef]
- Conti, B.; Tabarean, I.; Andrei, C.; Bartfai, T. Cytokines and fever. Frontiers in Bioscience 2004, 9, 1433–1449. [Google Scholar] [CrossRef]
- Mohandas, S.; Jagannathan, P.; Henrich, T.J.; Sherif, Z.A.; Bime, C.; Quinlan, E.; Portman, M.A.; Gennaro, M.; Rehman, J. Immune mechanisms underlying COVID-19 pathology and post-acute sequelae of SARS-CoV-2 infection (PASC). eLife 2023, 12, 1–19. [Google Scholar] [CrossRef]
- Altmann, D.M.; Boyton, R.J. SARS-CoV-2 T cell immunity: Specificity, function, durability, and role in protection. Science immunology 2020, 5, 1–5. [Google Scholar] [CrossRef]
- Badinlou, F.; Abzhandadze, T.; Rahimian, F.; Jansson-Fröjmark, M.; Hedman-Lagerlöf, M.; Lundgren, T. Investigating the trajectory of post-COVID impairments: a longitudinal study in Sweden. Frontiers in Psychology 2024, 15, 1–12. [Google Scholar] [CrossRef]
- Watase, M.; Miyata, J.; Terai, H.; Sunata, K.; Matsuyama, E.; Asakura, T.; Namkoong, H.; Masaki, K.; Yagi, K.; Ohgino, K. Cough and sputum in long COVID are associated with severe acute COVID-19: a Japanese cohort study. Respiratory Research 2023, 24, 283–292. [Google Scholar] [CrossRef]
- Nadel, J. New approaches to regulation of fluid secretion in airways. Chest 1981, 80, 849–851. [Google Scholar] [CrossRef]
- Tsang, K.W.; Zheng, L.; Ho, J.C.; Lam, W.-k.; Chan, K.-n.; Ho, P.-l.; Ooi, G.C. Sputum elastase in steady-state bronchiectasis. Chest 2000, 117, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Krüger, K.; Töpfner, N.; Berner, R.; Windfuhr, J.; Oltrogge, J.H. Sore Throat. Deutsches Ärzteblatt International 2021, 118, 188–194. [Google Scholar] [CrossRef]
- Renner, B.; Mueller, C.A.; Shephard, A. Environmental and non-infectious factors in the aetiology of pharyngitis (sore throat). Inflammation Research 2012, 61, 1041–1052. [Google Scholar] [CrossRef]
- Ghimire, S.; Sharma, S.; Patel, A.; Budhathoki, R.; Chakinala, R.; Khan, H.; Lincoln, M.; Georgeston, M. Diarrhea is associated with increased severity of disease in COVID-19: systemic review and metaanalysis. SN Comprehensive Clinical Medicine 2021, 3, 28–35. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Torres-Macho, J.; Guijarro, C.; Martín-Guerrero, J.D.; Pellicer-Valero, O.J.; Plaza-Manzano, G. Trajectory of gastrointestinal symptoms in previously hospitalized COVID-19 survivors: The Long COVID Experience Multicenter Study. Viruses 2023, 15, 1134–1146. [Google Scholar] [CrossRef]
- Freire, M.P.; Oliveira, M.S.; Magri, M.M.C.; Tavares, B.M.; Marinho, I.; Nastri, A.C.D.S.S.; Busatto Filho, G.; Levin, A.S. Frequency and factors associated with hospital readmission after COVID-19 hospitalization: the importance of post-COVID diarrhea. Clinics 2022, 77, 100061–100067. [Google Scholar] [CrossRef]
- Levy, M.; Kolodziejczyk, A.A.; Thaiss, C.A.; Elinav, E. Dysbiosis and the immune system. Nature Reviews Immunology 2017, 17, 219–232. [Google Scholar] [CrossRef]
- Al-Jahdhami, I.; Al-Naamani, K.; Al-Mawali, A. The post-acute COVID-19 syndrome (long COVID). Oman medical journal 2021, 36, e220–e221. [Google Scholar] [CrossRef]
- Teo, J. Early detection of silent hypoxia in Covid-19 pneumonia using smartphone pulse oximetry. Journal of medical systems 2020, 44, 134–135. [Google Scholar] [CrossRef]
- Grewal, J.S.; Carlsten, C.; Johnston, J.C.; Shah, A.S.; Wong, A.W.; Ryerson, C. Post-COVID dyspnea: prevalence, predictors, and outcomes in a longitudinal, prospective cohort. BMC Pulmonary Medicine 2023, 23, 84–92. [Google Scholar] [CrossRef]
- Joli, J.; Buck, P.; Zipfel, S.; Stengel, A. Post-COVID-19 fatigue: A systematic review. Frontiers in Psychiatry 2022, 13, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Rudroff, T.; Fietsam, A.C.; Deters, J.R.; Bryant, A.D.; Kamholz, J. Post-COVID-19 fatigue: potential contributing factors. Brain sciences 2020, 10, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Shaik, R.; Ahmad, R.; Yusuf, M.; Khan, M.; Almutairi, A.; Alghuyaythat, W.; Almutairi, S. " LONG COVID": an insight. European Review for Medical & Pharmacological Sciences 2021, 25, 5561–5577. [Google Scholar]
- Townsend, L.; Dowds, J.; O’Brien, K.; Sheill, G.; Dyer, A.H.; O’Kelly, B.; Hynes, J.P.; Mooney, A.; Dunne, J.; Ni Cheallaigh, C. Persistent poor health after COVID-19 is not associated with respiratory complications or initial disease severity. Annals of the American Thoracic Society 2021, 18, 997–1003. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. Jama 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Jacobs, L.G.; Gourna Paleoudis, E.; Lesky-Di Bari, D.; Nyirenda, T.; Friedman, T.; Gupta, A.; Rasouli, L.; Zetkulic, M.; Balani, B.; Ogedegbe, C. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PloS one 2020, 15, 1–14. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Palacios-Cena, D.; Gomez-Mayordomo, V.; Palacios-Cena, M.; Rodriguez-Jimenez, J.; de-la-Llave-Rincón, A.I.; Velasco-Arribas, M.; Fuensalida-Novo, S.; Ambite-Quesada, S.; Guijarro, C. Fatigue and dyspnoea as main persistent post-COVID-19 symptoms in previously hospitalized patients: related functional limitations and disability. Respiration 2022, 101, 132–141. [Google Scholar] [CrossRef]
- Rai, D.K.; Sharma, P.; Karmakar, S.; Thakur, S.; Ameet, H.; Yadav, R.; Gupta, V.B. Approach to post COVID-19 persistent cough: A narrative review. Lung India 2023, 40, 149–154. [Google Scholar] [CrossRef]
- Naik, S.; Haldar, S.N.; Soneja, M.; Mundadan, N.G.; Garg, P.; Mittal, A.; Desai, D.; Trilangi, P.K.; Chakraborty, S.; Begam, N.N. Post COVID-19 sequelae: A prospective observational study from Northern India. Drug discoveries & therapeutics 2021, 15, 254–260. [Google Scholar]
- Dennis, A.; Wamil, M.; Alberts, J.; Oben, J.; Cuthbertson, D.J.; Wootton, D.; Crooks, M.; Gabbay, M.; Brady, M.; Hishmeh, L. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ open 2021, 11, e048391–e048402. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent symptoms in patients after acute COVID-19. Jama 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Kayaaslan, B.; Eser, F.; Kalem, A.K.; Kaya, G.; Kaplan, B.; Kacar, D.; Hasanoglu, I.; Coskun, B.; Guner, R. Post-COVID syndrome: A single-center questionnaire study on 1007 participants recovered from COVID-19. Journal of medical virology 2021, 93, 6566–6574. [Google Scholar] [CrossRef]
- Tana, C.; Bentivegna, E.; Cho, S.-J.; Harriott, A.M.; García-Azorín, D.; Labastida-Ramirez, A.; Ornello, R.; Raffaelli, B.; Beltrán, E.R.; Ruscheweyh, R. Long COVID headache. The journal of headache and pain 2022, 23, 93–104. [Google Scholar] [CrossRef]
- Gómez-Dabó, L.; Melgarejo-Martínez, L.; Caronna, E.; Pozo-Rosich, P. Headache in COVID-19 and Long COVID: to Know Facts for Clinical Practice. Current Neurology and Neuroscience Reports 2023, 23, 551–560. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Navarro-Santana, M.; Gómez-Mayordomo, V.; Cuadrado, M.L.; García-Azorín, D.; Arendt-Nielsen, L.; Plaza-Manzano, G. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature. European journal of neurology 2021, 28, 3820–3825. [Google Scholar] [CrossRef]
- Garcia-Azorin, D.; Layos-Romero, A.; Porta-Etessam, J.; Membrilla, J.A.; Caronna, E.; Gonzalez-Martinez, A.; Mencia, Á.S.; Segura, T.; Gonzalez-García, N.; Díaz-de-Terán, J. Post-COVID-19 persistent headache: a multicentric 9-months follow-up study of 905 patients. Cephalalgia 2022, 42, 804–809. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: major findings, mechanisms and recommendations. Nature reviews. Microbiology 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Cancela-Cilleruelo, I.; Moro-López-Menchero, P.; Rodríguez-Jiménez, J.; Gómez-Mayordomo, V.; Torres-Macho, J.; Pellicer-Valero, O.J.; Martín-Guerrero, J.D.; Hernández-Barrera, V.; Arendt-Nielsen, L. Prevalence of musculoskeletal post-COVID pain in hospitalized COVID-19 survivors depending on infection with the historical, alpha or delta SARS-CoV-2 variant. Biomedicines 2022, 10, 1951–1960. [Google Scholar] [CrossRef]
- Neto, R.B.D.; Reis, L.F.F.; Ferreira, A.d.S.; Alexandre, D.J.d.A.; Almeida, R.S.d. Hospital admission is associated with disability and late musculoskeletal pain in individuals with long COVID. Frontiers in Rehabilitation Sciences 2023, 4, 1186499–1186506. [Google Scholar] [CrossRef]
- Steinmetz, A.; Gross, S.; Lehnert, K.; Lücker, P.; Friedrich, N.; Nauck, M.; Bahlmann, S.; Fielitz, J.; Dörr, M. Longitudinal clinical features of post-COVID-19 patients—symptoms, fatigue and physical function at 3-and 6-month follow-up. Journal of Clinical Medicine 2023, 12, 3966–3980. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-Penas, C.; Cancela-Cilleruelo, I.; Moro-López-Menchero, P.; Rodríguez-Jiménez, J.; Pellicer-Valero, O.J.; Martín-Guerrero, J.D.; Arendt-Nielsen, L. Exploring the trajectory curve of long-term musculoskeletal post-COVID pain symptoms in hospitalized COVID-19 survivors: a multicenter study. Pain 2023, 164, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Karaarslan, F.; Demircioğlu Güneri, F.; Kardeş, S. Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19: prospective follow-up by phone interviews. Rheumatology international 2021, 41, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Teodoro, T.; Chen, J.; Gelauff, J.; Edwards, M.J. Functional neurological disorder in people with long COVID: A systematic review. European Journal of Neurology 2023, 30, 1505–1514. [Google Scholar] [CrossRef]
- Guo, P.; Benito Ballesteros, A.; Yeung, S.P.; Liu, R.; Saha, A.; Curtis, L.; Kaser, M.; Haggard, M.P.; Cheke, L.G. COVCOG 2: cognitive and memory deficits in long COVID: a second publication from the COVID and cognition study. Frontiers in aging neuroscience 2022, 14, 1–21. [Google Scholar] [CrossRef]
- Irisson-Mora, I.; Salgado-Cordero, A.M.; Reyes-Varón, E.; Cataneo-Piña, D.J.; Fernández-Sánchez, M.; Buendía-Roldán, I.; Salazar-Lezama, M.A.; Health, O.; Consortium, P.M. Comparison between the persistence of post COVID-19 symptoms on critical patients requiring invasive mechanical ventilation and non-critical patients. PloS one 2022, 17, e0273041–e0273057. [Google Scholar] [CrossRef]
- Taylor, R.R.; Trivedi, B.; Patel, N.; Singh, R.; Ricketts, W.M.; Elliott, K.; Yarwood, M.; White, V.; Hylton, H.; Allen, R. Post-COVID symptoms reported at asynchronous virtual review and stratified follow-up after COVID-19 pneumonia. Clinical Medicine 2021, 21, e384–e391. [Google Scholar] [CrossRef]
- Mandal, S.; Barnett, J.; Brill, S.E.; Brown, J.S.; Denneny, E.K.; Hare, S.S.; Heightman, M.; Hillman, T.E.; Jacob, J.; Jarvis, H.C.; et al. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2021, 76, 396–398. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Florencio, L.L.; Cuadrado, M.L.; Plaza-Manzano, G.; Navarro-Santana, M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. European journal of internal medicine 2021, 92, 55–70. [Google Scholar] [CrossRef]
- Yuan, N.; Lv, Z.-H.; Sun, C.-R.; Wen, Y.-Y.; Tao, T.-Y.; Qian, D.; Tao, F.-P.; Yu, J.-H. Post-acute COVID-19 symptom risk in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Frontiers in Public Health 2023, 11, 1112383–1112392. [Google Scholar] [CrossRef]
- Pérez-González, A.; Araújo-Ameijeiras, A.; Fernández-Villar, A.; Crespo, M.; Poveda, E. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Scientific reports 2022, 12, 3369–3376. [Google Scholar] [CrossRef] [PubMed]
- Maglietta, G.; Diodati, F.; Puntoni, M.; Lazzarelli, S.; Marcomini, B.; Patrizi, L.; Caminiti, C. Prognostic factors for post-COVID-19 syndrome: a systematic review and meta-analysis. Journal of clinical medicine 2022, 11, 1541–1555. [Google Scholar] [CrossRef] [PubMed]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.m. Attributes and predictors of long COVID. Nature medicine 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Augustin, M.; Schommers, P.; Stecher, M.; Dewald, F.; Gieselmann, L.; Gruell, H.; Horn, C.; Vanshylla, K.; Di Cristanziano, V.; Osebold, L. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. The Lancet Regional Health–Europe 2021, 6, 100122–100129. [Google Scholar] [CrossRef]
- Fedorowski, A.; Fanciulli, A.; Raj, S.R.; Sheldon, R.; Shibao, C.A.; Sutton, R. Cardiovascular autonomic dysfunction in post-COVID-19 syndrome: a major health-care burden. Nature Reviews Cardiology 2024, 21, 379–395. [Google Scholar] [CrossRef]
- Choutka, J.; Jansari, V.; Hornig, M.; Iwasaki, A. Unexplained post-acute infection syndromes. Nature Medicine 2022, 28, 911–923. [Google Scholar] [CrossRef]
- Daugherty, S.E.; Guo, Y.; Heath, K.; Dasmariñas, M.C.; Jubilo, K.G.; Samranvedhya, J.; Lipsitch, M.; Cohen, K. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ 2021, 373, 1098–1109. [Google Scholar] [CrossRef]
- Tleyjeh, I.M.; Saddik, B.; AlSwaidan, N.; AlAnazi, A.; Ramakrishnan, R.K.; Alhazmi, D.; Aloufi, A.; AlSumait, F.; Berbari, E.; Halwani, R. Prevalence and predictors of Post-Acute COVID-19 Syndrome (PACS) after hospital discharge: A cohort study with 4 months median follow-up. PloS one 2021, 16, e0260568–e0260582. [Google Scholar] [CrossRef]
| MG (A, n = 40) |
WIMV (B, n = 40) |
IMV (C, n =13) |
RG (D, n = 40) |
p | |
|---|---|---|---|---|---|
| Age (years) | 43.9 ± 15.5 | 52.8 ± 11.2 | 52.1 ± 12.2 | 40.4 ± 12.4 | A-B,C-D,A,C,B-D |
| Height (cm) | 164.9 ± 7.4 | 167.5 ± 10.6 | 164.9 ± 12.0 | 164.2 ± 8.8 | A,B,C,D,A,C,B,D |
| Weight (kg) | 76.3 ± 16.1 | 83.8 ± 15.7 | 92.5 ± 22.2 | 74.9 ± 14.0 | A-B,C-D,A-C,B-D |
| BMI (kg/m2) | 28.1 ± 6.1 | 29.9 ± 5.2 | 33.9 ± 6.2 | 27.8 ± 4.6 | A,B-C-D,A-C-B,D |
| Gender (F/M) | (29/11) | (21/19) | (7/6) | (29/11) | - |
| MG n (%) |
WIMV n (%) |
IMV n (%) |
RG n (%) |
|
|---|---|---|---|---|
| Current Smoker | 1 (2.5) | 0 (0) | 1 (7.7) | 2 (5.0) |
| Former Smoker | 4 (10.0) | 13 (32.5) | 2 (15.4) | 3 (7.5) |
| Overweight | 15 (37.5) | 15 (37.5) | 1 (7.7) | 14 (35.0) |
| Obesity | 10 (25.0) | 15 (37.5) | 8 (61.5) | 14 (35.0) |
| Severe obesity (BMI ≥ 40.0) |
2 (5.0) | 3 (7.5) | 3 (23.1) | 0 (0) |
| Diabetes Mellitus | 1 (2.5) | 10 (25.0) | 4 (30.7) | 2 (5.0) |
| Prediabetes | 2 (5.0) | 2 (5.0) | 0 (0) | 0 (0) |
| Arterial Hypertension | 8 (20.0) | 17 (42.5) | 8 (61.5) | 6 (15.0) |
| Cardiomegaly | 1 (2.5) | 0 (0) | 1 (7.69) | 0 (0) |
| Hypercholesterolemia | 3 (7.5) | 0 (0) | 0 (0) | 0 (0) |
| COPD (pulmonary emphysema and chronic bronchitis) | 0 (0) | 1 (2.5) | 0 (0) | 1 (2.5) |
| Asthma | 2 (5.0) | 4 (10.0) | 0 (0) | 3 (7.5) |
| Home O2 dependence | 0 (0) | 0 (0) | 1 (7.7) | 0 (0) |
| Anxiety | 0 (0) | 0 (0) | 0 (0) | 4 (10.0) |
| Depression | 0 (0) | 1 (2.5) | 1 (7.7) | 1 (2.5) |
| Used Hydroxychloroquine | 0 (0) | 2 (5.0) | 1 (7.7) | 1 (2.5) |
| Used Azithromycin | 11 (27.5) | 18 (45.0) | 7 (53.8) | 13 (32.5) |
| Used Ivermectin | 4 (10.0) | 9 (22.5) | 3 (23.1) | 3 (7.5) |
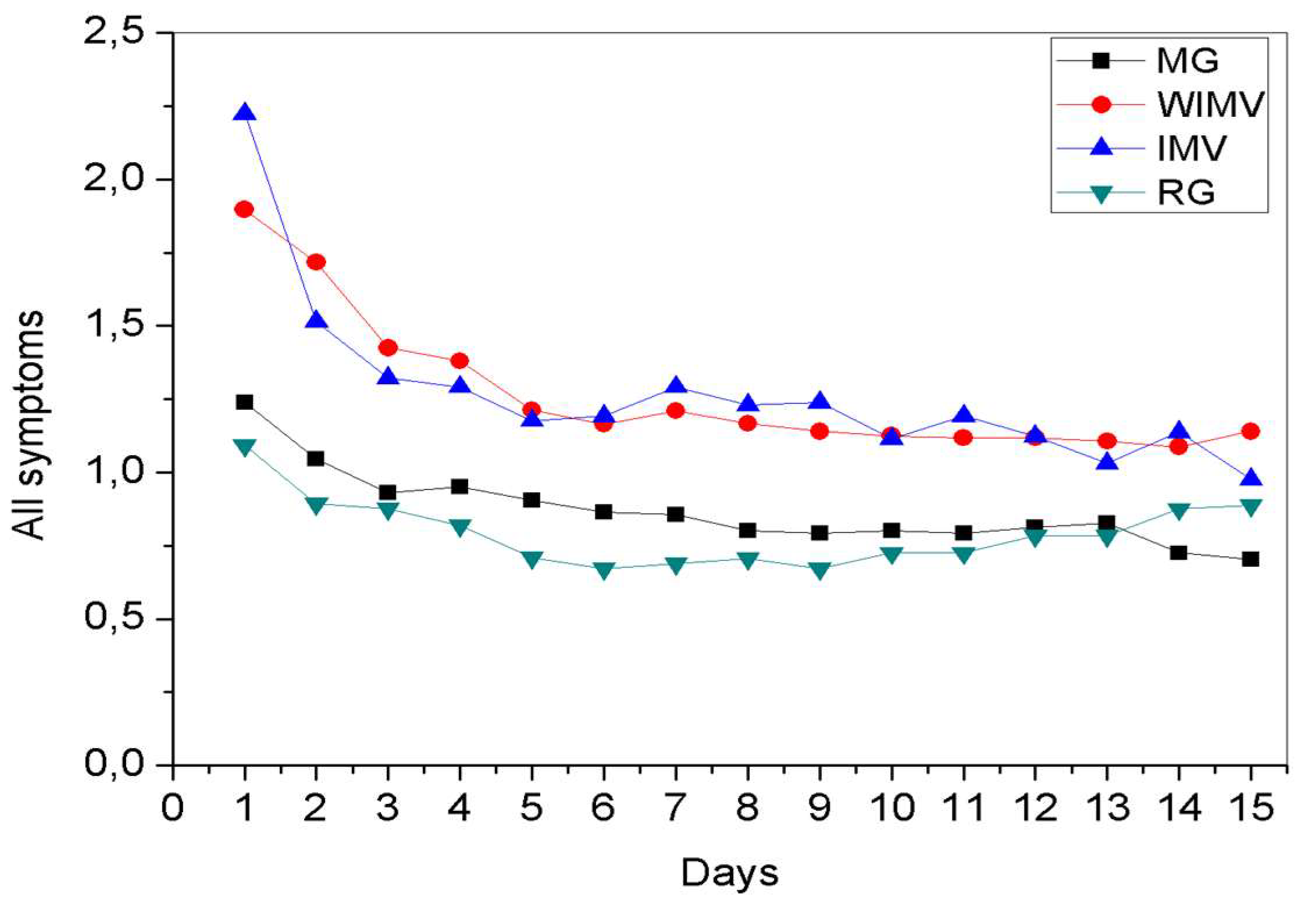
| MG | WIMV | IMV | RG | |
|---|---|---|---|---|
| Shortness of breath | 1.12 ± 2.26 | 1.67 ± 2.01 | 1.47 ± 1.93 | 1.07 ± 2.12 |
| Fatigue | 1.72 ± 2.61 | 2.92 ± 2.60 | 3.28 ± 2.31 | 1.92 ± 2.62 |
| Fever | 0.15 ± 0.57 | 0.30 ± 0.80 | 0.16 ± 0.57 | 0.11 ± 0.54 |
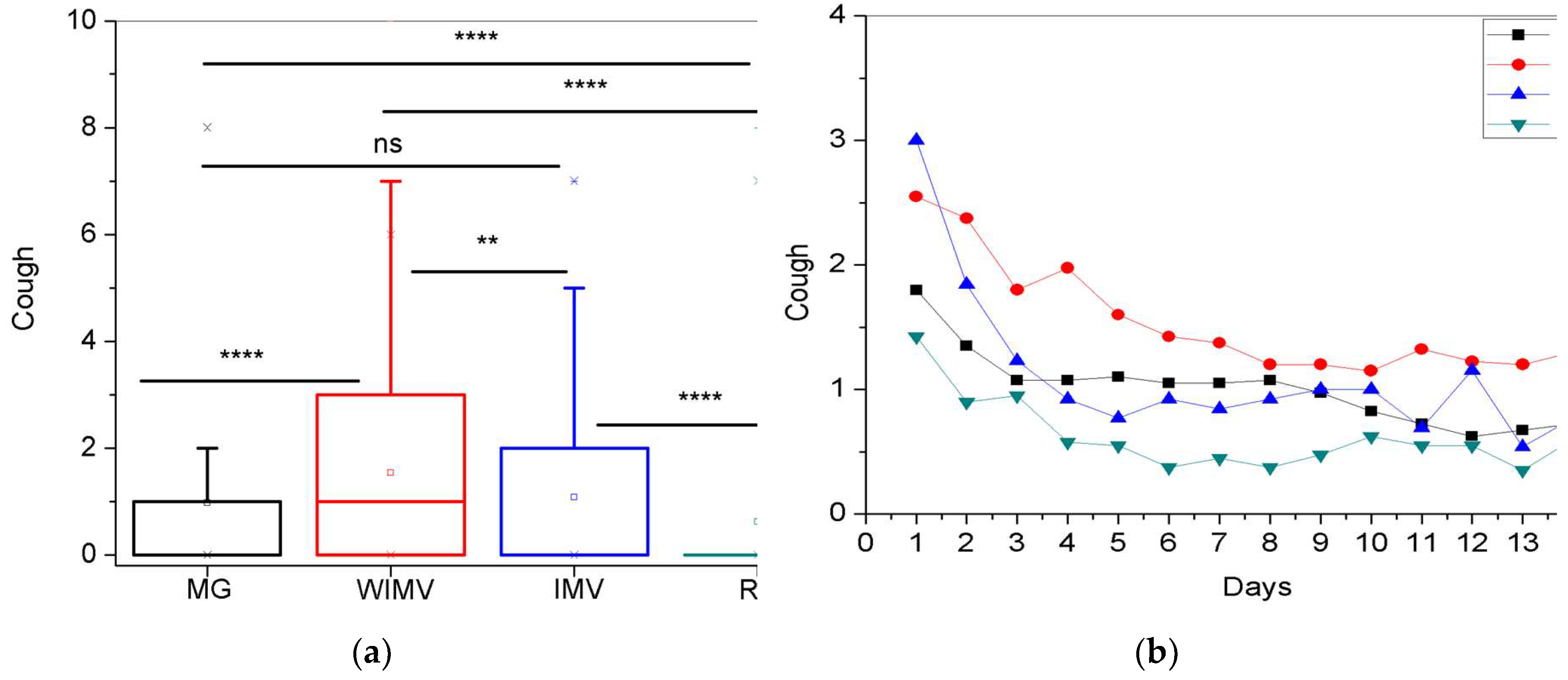
| Cough | 0.98 ± 1.75 | 1.54 ± 1.90 | 1.08 ± 1.65 | 0.62 ± 1.50 |
| Expectoration | 0.48 ± 1.13 | 0.63 ± 1.22 | 0.61 ± 1.37 | 0.58 ± 1.58 |
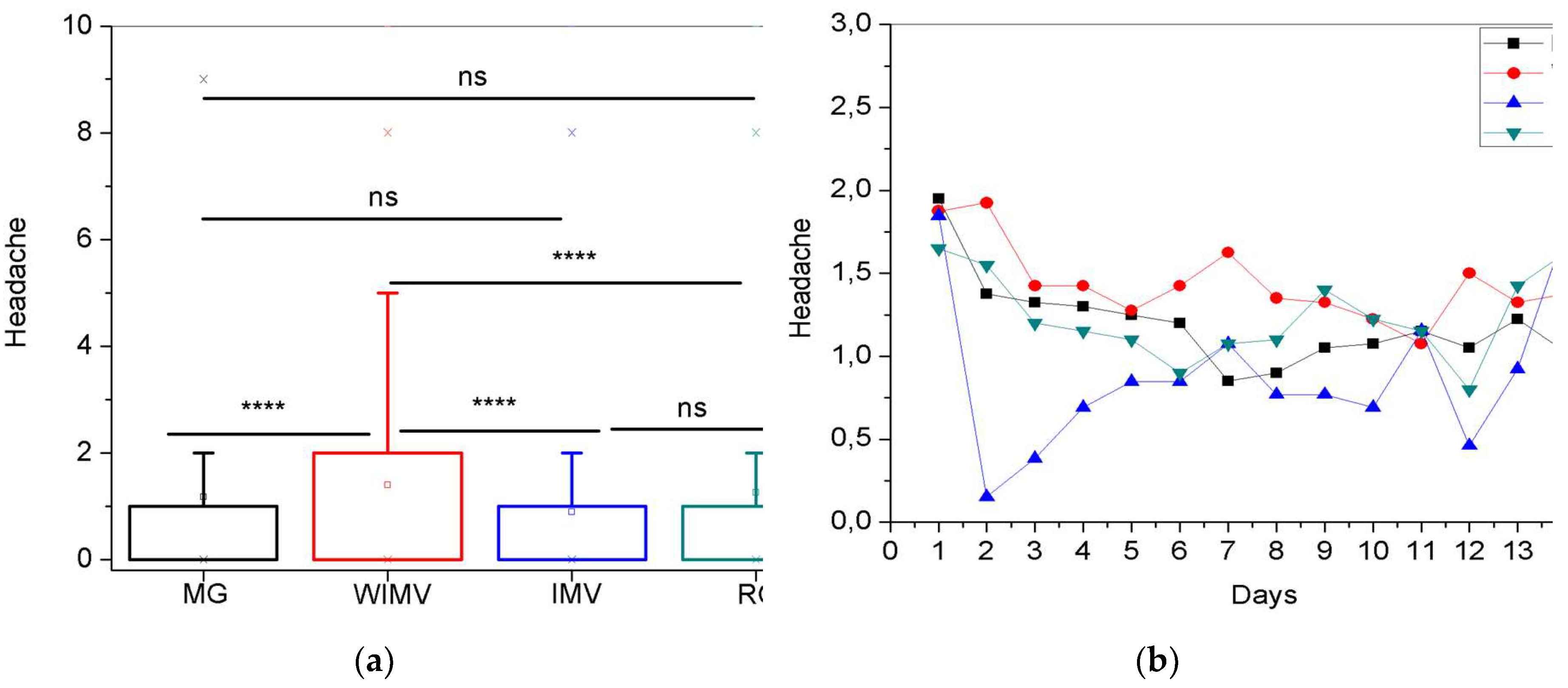
| Headache | 1.18 ± 2.44 | 1.40 ± 2.00 | 0.89 ± 1.92 | 1.25 ± 2.37 |
| Sore throat | 0.29 ± 0.89 | 0.41 ± 0.91 | 0.43 ± 1.20 | 0.21 ± 0.87 |
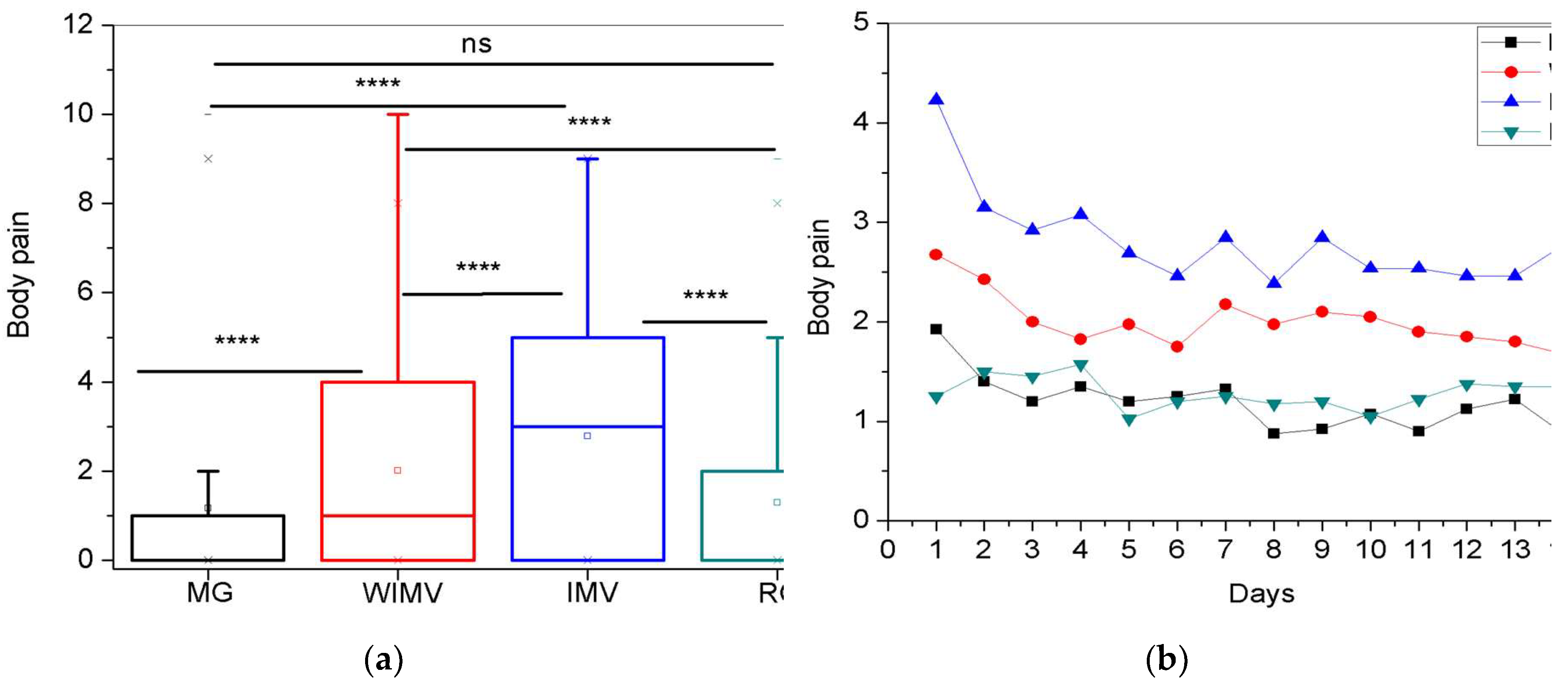
| Body pain | 1.16 ± 1.22 | 2.01 ± 2.32 | 2.77 ± 2.43 | 1.29 ± 2.19 |
| Diarrhea | 0.19 ± 0.87 | 0.40 ± 1.06 | 0.14 ± 0.61 | 0.16 ± 0.70 |
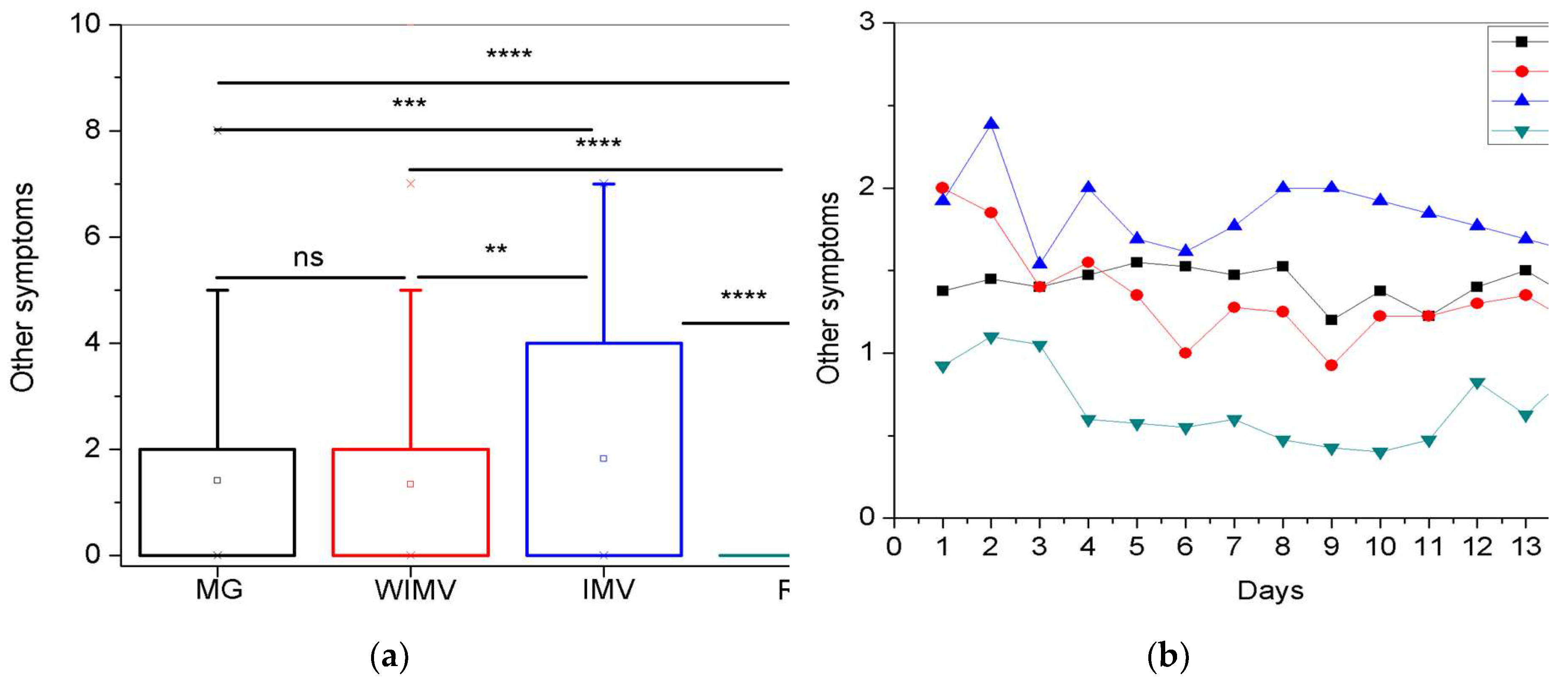
| Other symptoms | 1.41 ± 2.44 | 1.34 ± 2.07 | 1.83 ± 2.21 | 0.70 ± 2.02 |
| n (%) | |
|---|---|
| Memory lapse | 14 (10.5) |
| Tachycardia | 7 (5.26) |
| Tingling in limbs | 4 (3.0) |
| Radiating pain | 3 (2.25) |
| Anxiety | 3 (2.25) |
| Chest pressure | 3 (2.25) |
| Sensitive smell | 2 (1.50) |
| Weakness | 2 (1.50) |
| Arterial Hypertension | 2 (1.50) |
| Anosmia | 2 (1.50) |
| Hair loss | 2 (1.50) |
| Dizziness | 2 (1.50) |
| Nasal congestion and runny nose | 2 (1.50) |
| Sneezing | 1 (0.75) |
| Tremors in limbs | 1 (0.75) |
| Eye pain | 1 (0.75) |
| Ear blockage | 1 (0.75) |
| Testicular inflammation | 1 (0.75) |
| Wart | 1 (0.75) |
| Colic | 1 (0.75) |
| Reflux | 1 (0.75) |
| Nausea | 1 (0.75) |
| Insomnia | 1 (0.75) |
| No other symptoms | 75 (56.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





