Submitted:
15 April 2025
Posted:
15 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
- -
- Had a confirmed diagnosis of obstructive disorder of the major salivary glands (parotid or submandibular);
- -
- Had complete demographic and clinical documentation, including sex, age, affected gland, diagnostic approach, treatment method, clinical evolution, and any complications.
- -
- Had systemic or locoregional conditions contraindicating sialendoscopy, such as hematologic disorders, coagulopathies, severe cardiovascular diseases, or systemic infections;
- -
- Presented with acute suppurative sialadenitis or other high-risk comorbidities that significantly increased the potential for intra- or post-procedural complications.
2.2. Data Collection and Analysis
2.3. Statistical Analysis
3. Results
3.1. Gland Involvement
3.2. Imaging Investigations
3.3. Diagnosis and Pathology Distribution
3.4. Salivary Calculus Characteristics
3.5. Anesthesia
3.6. Therapeutic Interventions
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CBCT | Cone-beam computed tomography |
| Medical CT | Medical computed tomography |
| MRI | Magnetic resonance imaging |
| SD | Standard deviation |
References
- Karwowska, N.N.; Turner, M.D. Etiology, diagnosis, and surgical management of obstructive salivary gland disease. Front. Oral Maxillofac. Med. 2021, 3, 17. [Google Scholar] [CrossRef]
- Subha, S.T.; Osman, M.; Narayanan, P. Obstructive Salivary Gland Disorders - A Malaysian Patient Series. Int. Arch. Otorhinolaryngol. 2024, 28, e608–e613. [Google Scholar] [CrossRef] [PubMed]
- Capaccio, P.; Torretta, S.; Ottaviani, F.; Sambataro, G.; Pignataro, L. Modern management of obstructive salivary diseases L’attuale orientamento terapeutico nelle patologie ostruttive salivari. Otorhinolaryngol. Ital. 2007, 27, 161–172. [Google Scholar]
- Wang, Y.-H.; Chen, Y.-T.; Chiu, Y.-W.; Yu, H.-C.; Chang, Y.-C. Time trends in the prevalence of diagnosed sialolithiasis from Taiwanese nationwide health insurance dental dataset. J. Dent. Sci. 2019, 14, 365–369. [Google Scholar] [CrossRef]
- Sánchez Barrueco, A.; Alcalá Rueda, I.; Ordoñez González, C.; Sobrino Guijarro, B.; Santillán Coello, J.; Tapia, G.D.; Guerra Gutiérrez, F.; Campos González, A.; Brenna, A.; Cenjor Españo, C.; et al. Transoral removal of submandibular hilar lithiasis: results on the salivary duct system, glandular parenchyma, and quality-of-life recovery. Eur. Arch. Oto-Rhino-Laryngology 2023, 280, 5031–5037. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.B.; Vissink, A.; Firth, N. Salivary Gland Disorders and Diseases. In Contemporary Oral Medicine; Springer International Publishing: Cham, 2019; pp. 1437–1521. ISBN 978-3-319-72303-7. [Google Scholar]
- Capaccio, P.; Gaffuri, M.; Canzi, P.; Pignataro, L. Recurrent obstructive salivary disease after sialendoscopy. A narrative literature review. Acta Otorhinolaryngol. Ital. 2023, 43, S95. [Google Scholar] [CrossRef]
- Filipov, I.; Cristache, C.M.; Săndulescu, M. Minimally-invasive definitive treatment of recurrent sialadenitis due to obstructive sialolithiasis - a case report. Germs 2023, 13, 288–291. [Google Scholar] [CrossRef]
- Singh, P.P.; Gupta, V. Sialendoscopy: Introduction, Indications and Technique. Indian J. Otolaryngol. Head Neck Surg. 2013, 66, 74. [Google Scholar] [CrossRef]
- Gundlach, P.; Hopf, J.; Linnarz, M. Introduction of a new diagnostic procedure: salivary duct endoscopy (sialendoscopy) clinical evaluation of sialendoscopy, sialography, and X-ray imaging. Endosc. Surg. Allied Technol. 1994, 2, 294–296. [Google Scholar]
- Konigsberger, R.; Feyh, J.; Goetz, A.; Schilling, V.; Kastenbauer, E. [Endoscopic controlled laser lithotripsy in the treatment of sialolithiasis]. Laryngorhinootologie. 1990, 69, 322–323. [Google Scholar] [CrossRef]
- Katz, P. [Endoscopy of the salivary glands]. Ann. Radiol. (Paris). 1991, 34, 110–113. [Google Scholar] [PubMed]
- Iro, H.; Zenk, J.; Escudier, M.P.; Nahlieli, O.; Capaccio, P.; Katz, P.; Brown, J.; Mcgurk, M. Outcome of minimally invasive management of salivary calculi in 4,691 patients. Laryngoscope 2009, 119, 263–268. [Google Scholar] [CrossRef]
- Cox, D.; Chan, L.; Veivers, D. Prognostic factors for therapeutic sialendoscopy. J. Laryngol. Otol. 2018, 132, 275–278. [Google Scholar] [CrossRef]
- Al-Abri, R.; Marchal, F. New era of Endoscopic Approach for Sialolithiasis: Sialendoscopy. Sultan Qaboos Univ. Med. J. 2010, 10, 382. [Google Scholar] [CrossRef]
- Koch, M.; Mantsopoulos, K.; Müller, S.; Sievert, M.; Iro, H. Treatment of Sialolithiasis: What Has Changed? An Update of the Treatment Algorithms and a Review of the Literature. J. Clin. Med. 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Keshet, N.; Aricha, A.; Friedlander-Barenboim, S.; Aframian, D.J.; Nadler, C. Novel parotid sialo-cone-beam computerized tomography features in patients with suspected Sjogren’s syndrome. Oral Dis. 2019, 25, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Thomas, W.W.; Douglas, J.E.; Rassekh, C.H. Accuracy of Ultrasonography and Computed Tomography in the Evaluation of Patients Undergoing Sialendoscopy for Sialolithiasis. Otolaryngol. Head. Neck Surg. 2017, 156, 834–839. [Google Scholar] [CrossRef]
- Bertin, H.; Bonnet, R.; Le Thuaut, A.; Huon, J.F.; Corre, P.; Frampas, E.; Langlois, E.M.; Chesneau, A.S.D. A comparative study of three-dimensional cone-beam CT sialography and MR sialography for the detection of non-tumorous salivary pathologies. BMC Oral Health 2023, 23, 463. [Google Scholar] [CrossRef]
- Capaccio, P.; Torretta, S.; Pignataro, L.; Koch, M. Salivary lithotripsy in the era of sialendoscopy. Acta Otorhinolaryngol. Ital. 2017, 37, 113–121. [Google Scholar] [CrossRef]
- Strychowsky, J.E.; Sommer, D.D.; Gupta, M.K.; Cohen, N.; Nahlieli, O. Sialendoscopy for the management of obstructive salivary gland disease: a systematic review and meta-analysis. Arch. Otolaryngol. Head. Neck Surg. 2012, 138, 541–547. [Google Scholar] [CrossRef]
- Filipov, I.; Chirila, L.; Sandulescu, M.; Cristache, G.; Cristache, C.M. Clinical Efficacy and Outcomes of Electro-Pneumatic Intracorporeal Lithotripsy in the Management of Sialolithiasis. OTO Open 2025, 9, e70080. [Google Scholar] [CrossRef]
- Koch, M.; Iro, H. Salivary duct stenosis: diagnosis and treatment. Acta Otorhinolaryngol. Ital. 2017, 37, 132. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.; Khorate, M.M.; Chinam, N. Efficacy of sialendoscopy in treatment of obstructive salivary gland diseases: A systematic review and meta-analysis. J. Oral Maxillofac. Surgery, Med. Pathol. 2024, 36, 570–578. [Google Scholar] [CrossRef]
- Gallo, A.; Benazzo, M.; Capaccio, P.; De Campora, L.; De Vincentiis, M.; Fusconi, M.; Martellucci, S.; Paludetti, G.; Pasquini, E.; Puxeddu, R.; et al. Sialoendoscopy: state of the art, challenges and further perspectives. Round Table, 101st SIO National Congress, Catania 2014. Acta Otorhinolaryngol. Ital. 2015, 35, 217. [Google Scholar] [PubMed]
- Vanden Daele, A.; Drubbel, J.; Van Lierde, C.; Meulemans, J.; Delaere, P.; Vander Poorten, V. Long-term outcome of a cohort of 272 patients undergoing sialendoscopy. Clin. Otolaryngol. 2022, 47, 138–145. [Google Scholar] [CrossRef]
- Kallas-Silva, L.; Azevedo, M.F.D.; de Matos, F.C.M.; Petrarrolha, S.P.; Dedivitis, R.A.; Kulcsar, M.A.V.; Matos, L.L. Sialendoscopy for treatment of major salivary glands diseases: a comprehensive analysis of published systematic reviews and meta-analyses. Brazilian Journal of Otorhinolaryngology, 2023; 89, 101293. [Google Scholar] [CrossRef]
- Kroll, T.; May, A.; Wittekindt, C.; Kähling, C.; Sharma, S.J.; Howaldt, H.P.; Klussmann, J.P.; Streckbein, P. Cone beam computed tomography (CBCT) sialography--an adjunct to salivary gland ultrasonography in the evaluation of recurrent salivary gland swelling. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 771–775. [Google Scholar] [CrossRef]
- Avishai, G.; Ben-Zvi, Y.; Ghanaiem, O.; Chaushu, G.; Gilat, H. Sialolithiasis—Do Early Diagnosis and Removal Minimize Post-Operative Morbidity? Medicina (B. Aires). 2020, 56, 332. [Google Scholar] [CrossRef]
- Lustmann, J.; Regev, E.; Melamed, Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int. J. Oral Maxillofac. Surg. 1990, 19, 135–138. [Google Scholar] [CrossRef]
- Borner, U.; Anschuetz, L.; Caversaccio, M.; von Werdt, M.; Panosetti, E.; Keghian, J.; Remacle, M. A Retrospective Analysis of Multiple Affected Salivary Gland Diseases: Diagnostic and Therapeutic Benefits of Interventional Sialendoscopy. Ear. Nose. Throat J. 2024, 103. [Google Scholar] [CrossRef]
- Agrawal, A.T.; Hande, A.; Reche, A.; Paul, P. Appraisal of Saliva and Its Sensory Perception in Reproductive Transitions of Women: A Review. Cureus 2022, 14, e31614. [Google Scholar] [CrossRef]
- Escudier, M.P.; McGurk, M. Symptomatic sialoadenitis and sialolithiasis in the English population, an estimate of the cost of hospital treatment. Br. Dent. J. 1999, 186, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Pachisia, S.; Mandal, G.; Sahu, S.; Ghosh, S. Submandibular Sialolithiasis: A Series of Three Case Reports with Review of Literature. Clin. Pract. 2019, Vol. 9, Page 1119 2019, 9, 1119. [Google Scholar] [CrossRef]
- Drage, N.A.; Brown, J.E.; Makdissi, J.; Townend, J. Migrating salivary stones: Report of three cases. Br. J. Oral Maxillofac. Surg. 2005, 43, 180–182. [Google Scholar] [CrossRef]
- Duong, L.T.; Kakiche, T.; Ferré, F.; Nawrocki, L.; Bouattour, A. Management of anterior submandibular sialolithiasis. J. Oral Med. Oral Surg. 2019, 25, 16. [Google Scholar] [CrossRef]
- Gaudino, C.; Cassoni, A.; Pisciotti, M.L.; Pucci, R.; Veneroso, C.; Di Gioia, C.R.T.; De Felice, F.; Pantano, P.; Valentini, V. High Field MRI in Parotid Gland Tumors: A Diagnostic Algorithm. Cancers (Basel). 2024, 17. [Google Scholar] [CrossRef]
- Koch, M.; Schapher, M.; Mantsopoulos, K.; von Scotti, F.; Goncalves, M.; Iro, H. Multimodal treatment in difficult sialolithiasis: Role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope 2018, 128, E332–E338. [Google Scholar] [CrossRef] [PubMed]
- Jokela, J.; Tapiovaara, L.; Lundberg, M.; Haapaniemi, A.; Bäck, L.; Saarinen, R. A Prospective Observational Study of Complications in 140 Sialendoscopies. Otolaryngol. Head. Neck Surg. 2018, 159, 650–655. [Google Scholar] [CrossRef]
- de Paiva Leite, S.; de Oliveira, M.M.R.; Ahmad, Z.; Morton, R.P. Impact on quality of life in obstructive sialadenitis predicting outcomes after sialendoscopy. Am. J. Otolaryngol. 2022, 43. [Google Scholar] [CrossRef] [PubMed]
- Terhaard, C. Salivary Glands and Quality of Life BT - Functional Preservation and Quality of Life in Head and Neck Radiotherapy. In; Harari, P.M., Connor, N.P., Grau, C., Eds.; Springer Berlin Heidelberg: Berlin, Heidelberg, 2009; pp. 89–101. ISBN 978-3-540-73232-7. [Google Scholar]
- Bawazeer, N.; Carvalho, J.; Djennaoui, I.; Charpiot, A. Sialendoscopy under conscious sedation versus general anesthesia. A comparative study. Am. J. Otolaryngol. 2018, 39, 754–758. [Google Scholar] [CrossRef]
- Trujillo, O.; Drusin, M.A.; Pagano, P.P.; Askin, G.; Rahmati, R. Evaluation of Monitored Anesthesia Care in Sialendoscopy. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 769. [Google Scholar] [CrossRef]
- Nahlieli, O.; Shacham, R.; Shlesinger, M.; Eliav, E. Juvenile recurrent parotitis: a new method of diagnosis and treatment. Pediatrics 2004, 114, 9–12. [Google Scholar] [CrossRef] [PubMed]
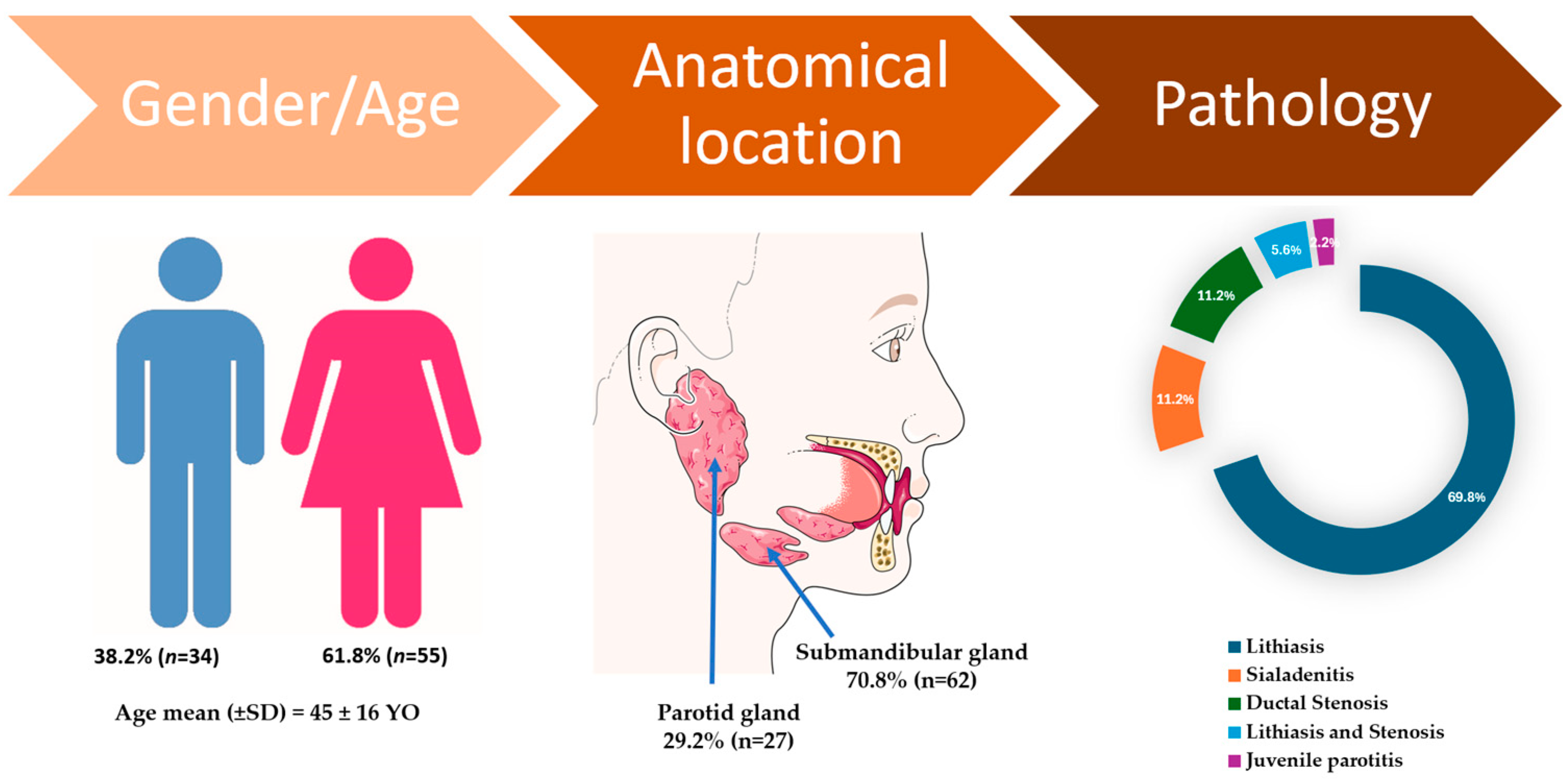


| Variable | Female (n=55) | Male (n=34) | P-value | Parotid | Submandibular | P-value | Total (n=89) |
|---|---|---|---|---|---|---|---|
| Age (mean ± SD) | 43.7±17.0 | 46.2±14.8 | 0.46 | 41.89±16.50 | 45.85±15.96 | 0.29 | 45 ± 16 |
| Gland involved | |||||||
| Parotid | 18 (32.7%) | 9 (26.5%) | 0.67 | 27 (29.2%) | - | - | 27 (29.2%) |
| Submandibular | 37 (67.3%) | 25 (73.5%) | 0.67 | - | 62 (70.8%) | - | 62 (70.8%) |
| Calculus size (mm) | 7.19±4.17 | 6.80±5.24 | 0.75 | 5.07±1.82 | 7.57±4.92 | 0.00* | 7.04±4.56 |
| Pathology | |||||||
| Lithiasis | 38 (69.1%) | 24 (70.6%) | 1.00 | 10 (37.1%) | 52 (83.9%) | 0.00* | 64 (69.8%) |
| Sialadenitis | 7 (12.7%) | 3 (8.8%) | 0.83 | 5 (18.5%) | 5 (8.1%) | 0.28 | 10 (11.2%) |
| Ductal Stenosis | 6 (10.9%) | 4 (11.8%) | 1.00 | 6 (22.2%) | 4 (6.5%) | 0.07 | 10 (11.2%) |
| Lithiasis and stenosis | 4 (7.3%) | 1 (2.9%) | 0.69 | 4 (14.8%) | 1 (1.5%) | 0.05* | 5 (5.6%) |
| Juvenile parotitis | 0 | 2 (5.9%) | 0.28 | 2 (7.4%) | 0 | - | 2 (2.2%) |
| Imaging Investigations | |||||||
| Ultrasound | 47 (85.5%) | 30 (88.2%) | 0.96 | 25 (92.59%) | 52 (83.87%) | 0.44 | 77(86.5%) |
| CBCT | 34 (61.8%) | 20 (58.8%) | 0.95 | 8 (29.6%) | 46 (74.19%) | 0.00* | 54 (60.7%) |
| Medical CT | 2 (3.6%) | 4 (11.8%) | 0.29 | 5 (18.52%) | 1 (1.61%) | 0.01* | 6 (6.7%) |
| MRI | 3 (5.5%) | 2 (5.9%) | 1.0 | 2 (3.23%) | 0.32 | 5 (5.6%) | |
| CBCT Sialography | 2 (3.6%) | 1 (2.9%) | 1.0 | 2 (7.40%) | 1 (1.61%) | 0.45 | 3 (3.4%) |
| Anesthesia | |||||||
| Local | 53 (96.4%) | 30 (88.2%) | 0.29 | 27 (100%) | 56 (90.32%) | 0.22 | 83 (93.26%) |
| General | 2 (3.6%) | 4 (11.8%) | 0.29 | 0 | 6 (9.68%) | 0.22 | 6 (6.74%) |
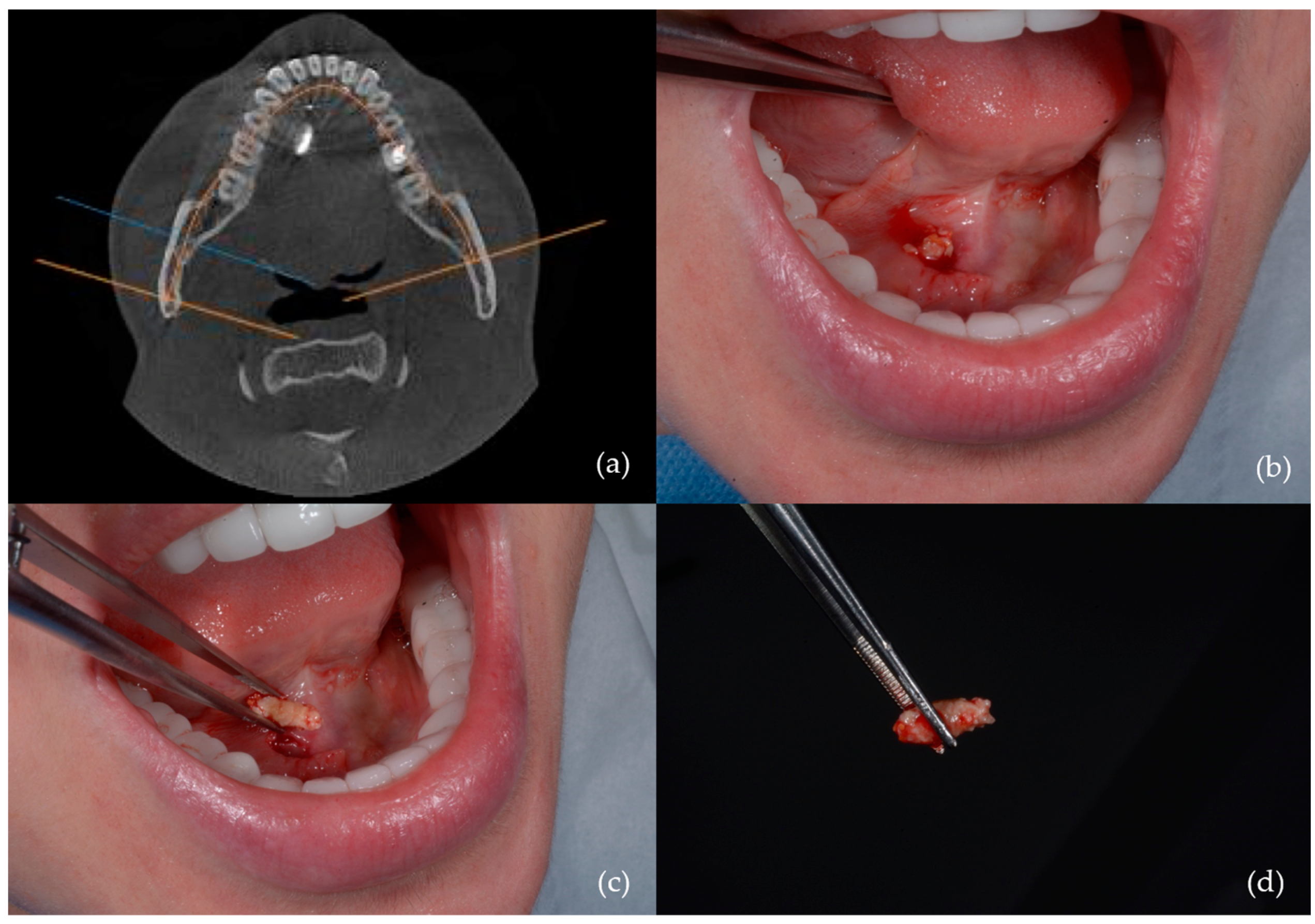
| Therapeutic Interventions | |||||||
| Transoral sialolithotomy | 19 (34.5%) | 10 (29.4%) | 0.79 | 0 | 29 (8.06%) | 0.46 | 29 (32.6%) |
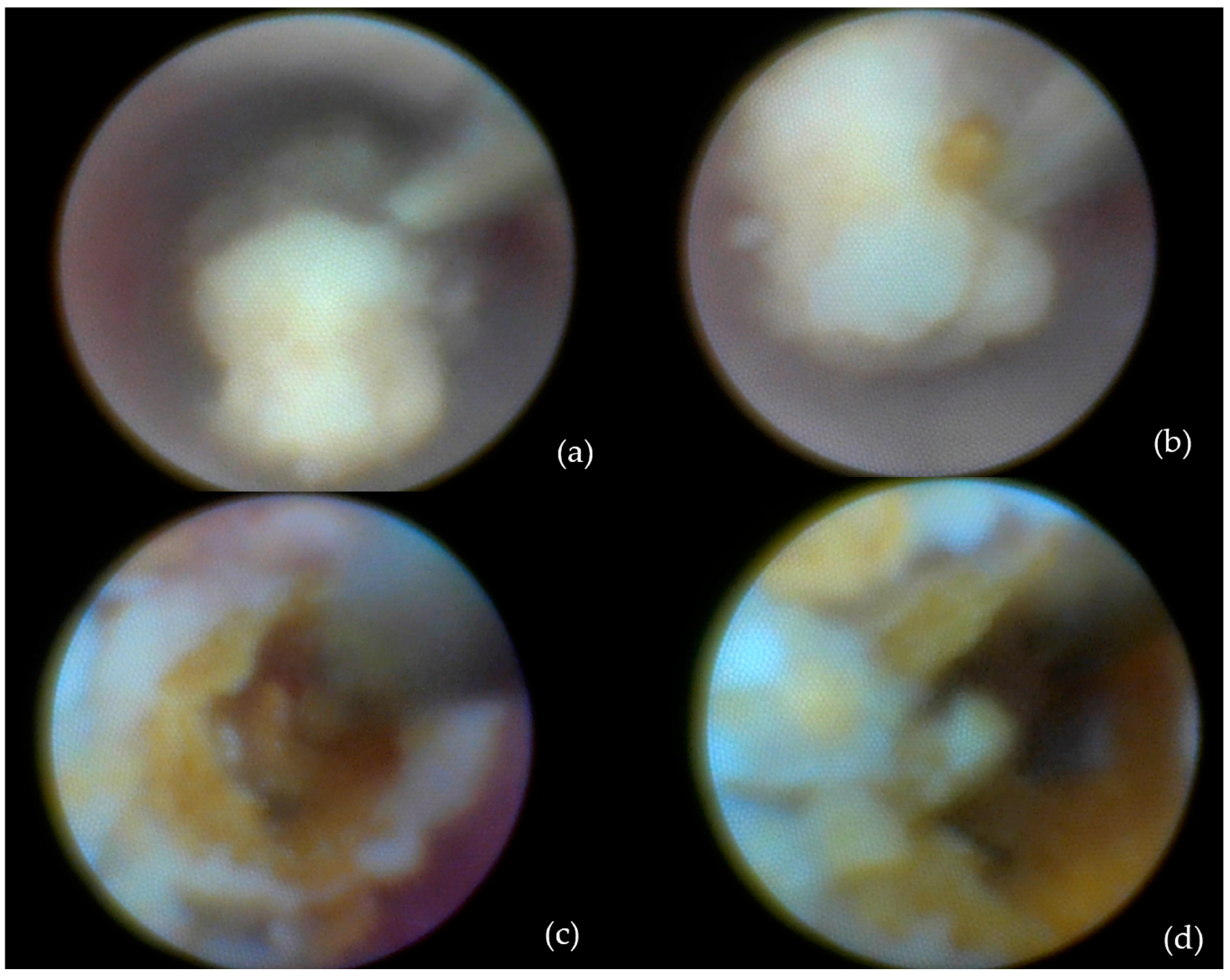
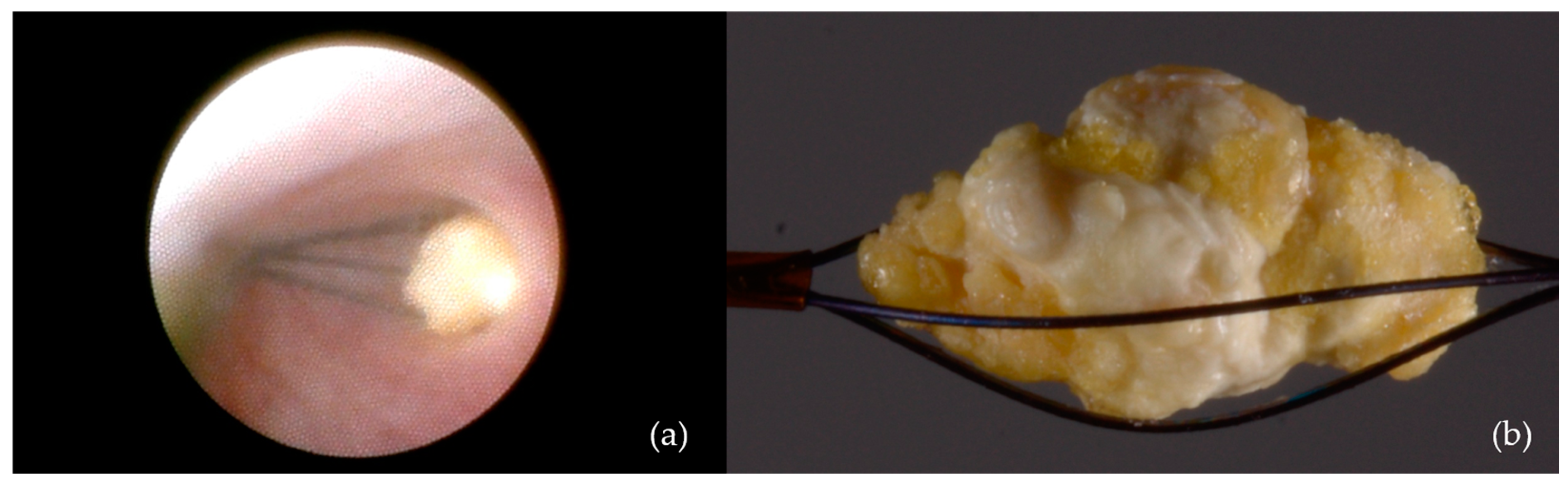
| Intracorporeal lithotripsy | 18 (32.7%) | 11 (32.4%) | 1.0 | 12 (44.4%) | 17 (27.42%) | 0.18 | 29 (32.6%) |
| Dormia basket extraction | 6 (10.9%) | 2 (5.9%) | 0.67 | 3 (11.11%) | 5 (8.06%) | 0.95 | 8 (9.0%) |
| Ductal dilation and stenting | 4 (7.3%) | 3 (8.8%) | 1.0 | 4 (14.81%) | 3 (4.84%) | 0.24 | 7 (7.9%) |
| Submandibulectomy | 1 (1.8%) | 4 (11.8%) | 0.13 | 0 | 5 (46.77%) | 0.31 | 5 (5.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





