Introduction
Substance use disorders (SUDs) remain a significant public health challenge worldwide. Traditional treatment methods, while effective, face numerous barriers such as accessibility, stigma, and cost. The advent of telemedicine and online therapy platforms presents a promising avenue for overcoming these obstacles and enhancing treatment outcomes. This paper explores the potential of telemedicine and online interventions in treating SUDs, reviewing current evidence and discussing future directions.
Substance use disorders (SUDs) remain a formidable challenge to global public health, impacting millions of individuals across diverse populations. These disorders, characterized by the problematic use of psychoactive substances such as opioids, alcohol, and stimulants, lead to significant personal, social, and economic consequences. Traditional treatment modalities for SUDs have evolved over decades and typically involve a combination of pharmacological and psychotherapeutic interventions. Despite their demonstrated efficacy, numerous challenges such as accessibility, stigma, and treatment adherence continue to hinder their widespread application and effectiveness.
The evolution of digital technology in health care, particularly the advent of telemedicine and online treatment platforms, presents a unique opportunity to transcend many of these barriers. Telemedicine, defined broadly as the remote delivery of healthcare services using telecommunications technology, can offer treatment options that are both accessible and cost-effective for many who would otherwise not receive help. Recent research underscores the potential of telemedicine in providing effective intervention for substance use disorders, which suggests comparable outcomes to traditional in-person therapy concerning abstinence and treatment retention (Lin et al., 2019).
Furthermore, the ongoing global digital transformation has accelerated the integration of online resources into daily life, thereby increasing the feasibility of online interventions for SUDs. Online platforms can deliver therapy through various formats, including but not limited to, real-time video conferencing, asynchronous messaging, and digital learning modules. These interventions are not only pragmatic but also align well with the increasing consumer preference for digital health solutions that offer privacy, convenience, and user-centered control (Kay-Lambkin et al., 2011).
Moreover, the application of online and telemedicine interventions could play a critical role in destigmatizing substance use disorder treatment. The anonymity and privacy afforded by online platforms can help mitigate the shame and stigma that often deter individuals from seeking treatment. This is crucial because stigma is a significant barrier that affects access to care and is associated with poorer quality health outcomes (Cunningham et al., 2010).
Given the potential of telemedicine and online interventions to address these multifaceted issues, it is vital to explore their capabilities and limitations thoroughly. This exploration must consider the variety of technological, ethical, and regulatory challenges that these innovations face. By examining these aspects in depth, the current paper aims to provide a comprehensive overview of the state of telemedicine and online treatments for SUDs and their future implications for policy, practice, and research in the field.
The Landscape of Substance Use Disorders
Substance use disorders encompass a range of conditions associated with the excessive use of psychoactive substances, including alcohol, opioids, cannabis, and stimulants. These disorders are characterized by a chronic, relapsing nature and have substantial impacts on individuals' physical and mental health, social relationships, and overall quality of life (American Psychiatric Association, 2013).
Substance use disorders (SUDs) encompass a complex array of conditions that involve the problematic use of psychoactive substances such as alcohol, opioids, stimulants, and cannabis. These disorders are characterized by an individual's intense focus on obtaining and using these substances, despite the occurrence of negative consequences. The impact of SUDs extends beyond the individual, affecting families, communities, and the overall health care system, posing a significant burden on societal resources.
The definition and classification of SUDs have evolved over the years, with the current diagnostic criteria being detailed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) published by the American Psychiatric Association (2013). According to DSM-5, the diagnosis of a substance use disorder is based on evidence of impaired control, social impairment, risky use, and pharmacological criteria.
Epidemiologically, the global prevalence of substance use disorders varies significantly by substance type and region. According to the World Drug Report by the United Nations Office on Drugs and Crime (2020), millions of people worldwide suffer from drug use disorders, with opioids accounting for a substantial portion of the disease burden associated with drug use. Alcohol use disorders also represent a significant public health issue, with the World Health Organization (2018) reporting that excessive alcohol use leads to millions of deaths and disabilities each year.
The pathophysiology of SUDs involves complex interactions between genetic, environmental, and social factors. Genetic predispositions play a significant role in the development of these disorders, influencing neurotransmitter systems that mediate reward pathways in the brain. Volkow et al. (2016) discuss how alterations in the dopamine system can predispose individuals to substance use by enhancing the reinforcing effects of drugs. Environmental factors, including exposure to drugs, stress, and trauma, interact with these genetic factors to facilitate the development of SUDs.
Treatment landscapes for SUDs are diverse and require a multifaceted approach. Historically, treatment modalities have included detoxification, pharmacotherapy, behavioral therapies, and support groups. Each treatment approach aims to address various aspects of addiction, from physiological dependence and withdrawal to psychological and social rehabilitation. The integration of behavioral health interventions, such as cognitive-behavioral therapy (CBT) and motivational interviewing (MI), has been shown to be effective in treating substance use disorders by targeting the underlying cognitive and emotional processes (McHugh et al., 2010).
Despite available treatments, SUDs often manifest as chronic, relapsing conditions, with high rates of recidivism. The chronic nature of these disorders necessitates ongoing management strategies, similar to other chronic diseases like diabetes or hypertension. This perspective aligns with the shifting paradigm in healthcare towards more sustainable, long-term management of SUDs, focusing on recovery as a lifelong journey of engagement in treatment and personal growth (McLellan et al., 2000).
Moreover, the treatment of SUDs faces several challenges, including the stigma associated with drug use and addiction, which can prevent individuals from seeking help. There is also a significant gap in the treatment provision, with a large proportion of individuals with SUDs not receiving any form of care. This treatment gap is attributed to various factors, including limited access to healthcare services, lack of trained healthcare providers, and the aforementioned stigma.
In conclusion, understanding the landscape of substance use disorders requires a comprehensive grasp of their epidemiology, pathophysiology, and the challenges associated with their treatment. Addressing these needs with effective, evidence-based strategies and policies is essential for mitigating the impact of these disorders on individuals and society.
Traditional Treatment Approaches
Traditional treatment for SUDs often involves a combination of pharmacotherapy and psychotherapy. Medications like methadone, buprenorphine, and naltrexone are used to manage withdrawal symptoms and reduce cravings (Volkow et al., 2014). Psychotherapeutic interventions, such as cognitive-behavioral therapy (CBT), motivational interviewing (MI), and contingency management, play a crucial role in addressing the psychological aspects of addiction (McHugh et al., 2010).
Traditional approaches to the treatment of substance use disorders (SUDs) have historically centered on a blend of pharmacological interventions and psychotherapeutic techniques, aiming to address both the biological and psychological facets of addiction. These approaches are grounded in decades of research and clinical practice, providing a robust framework for the management and recovery of individuals afflicted with SUDs.
Pharmacological Treatments
Pharmacological treatments for substance use disorders (SUDs) are an essential component of comprehensive care, particularly for those struggling with moderate to severe addiction. Medications are used to manage withdrawal symptoms, reduce cravings, prevent relapse, and help restore the brain’s neurochemical balance, which is often disrupted by prolonged substance use. While psychotherapeutic interventions address the psychological and behavioral aspects of addiction, pharmacological treatments target the biological and neurochemical processes that underpin SUDs. The combination of these two approaches has proven to be more effective than either one in isolation, particularly for severe cases of addiction (Fiellin, 2002). In this section, we will explore the main categories of pharmacological treatments for SUDs, including treatments for alcohol use disorder (AUD), opioid use disorder (OUD), and nicotine addiction, among others.
Opioid use disorder is one of the most critical public health crises globally, with millions of individuals affected by misuse of both prescription opioids and illicit opioids like heroin. The pharmacological treatment of OUD primarily involves the use of opioid agonists, partial agonists, and antagonists, which help manage withdrawal symptoms and reduce cravings. These medications have been shown to improve retention in treatment, reduce illicit opioid use, and decrease mortality rates (Mattick et al., 2014).
1.1 Methadone
Methadone is a full opioid agonist that has been used for decades in the treatment of OUD. It binds to opioid receptors in the brain, reducing cravings and withdrawal symptoms without producing the same euphoric effects as heroin or other opioids. Methadone is typically administered in a highly controlled setting, such as a licensed clinic, due to its potential for abuse and overdose if not properly managed. Studies have demonstrated that methadone maintenance therapy (MMT) is highly effective at reducing opioid use, increasing treatment retention, and improving overall quality of life for individuals with OUD (Mattick et al., 2009).
1.2 Buprenorphine
Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors in the brain but to a lesser degree than full agonists like methadone. This characteristic makes buprenorphine less likely to cause overdose, and it can be prescribed in an outpatient setting, making it more accessible for patients. In the United States, buprenorphine can be prescribed by qualified healthcare providers, which increases access to treatment in areas where methadone clinics may not be available. Studies have shown that buprenorphine is as effective as methadone in reducing opioid use and promoting long-term recovery, with fewer side effects and less risk of overdose (Fiellin et al., 2014).
1.3 Naltrexone
Naltrexone is an opioid antagonist that blocks the effects of opioids by binding to the brain’s opioid receptors without activating them. This prevents individuals from experiencing the euphoric effects of opioids, which helps deter opioid use. Unlike methadone and buprenorphine, naltrexone is not a controlled substance and can be prescribed more freely. However, it requires that the individual has fully detoxified from opioids before starting treatment, which can be a significant barrier due to the severity of opioid withdrawal symptoms. Despite this challenge, research indicates that naltrexone is effective in preventing relapse among individuals who are highly motivated and able to complete detoxification before starting treatment (Lee et al., 2018).
- 2.
Medications for Alcohol Use Disorder (AUD)
Alcohol use disorder is one of the most common SUDs, affecting millions of people worldwide. Pharmacological treatments for AUD aim to reduce cravings, diminish the rewarding effects of alcohol, and manage withdrawal symptoms. These medications are often used in conjunction with behavioral interventions to maximize effectiveness.
2.1 Disulfiram
Disulfiram is one of the oldest medications used to treat AUD. It works by inhibiting the enzyme acetaldehyde dehydrogenase, which is involved in the metabolism of alcohol. When alcohol is consumed, disulfiram causes a buildup of acetaldehyde in the body, leading to highly unpleasant effects such as nausea, vomiting, flushing, and headaches. These aversive reactions discourage individuals from drinking. While disulfiram is effective in promoting abstinence, its success largely depends on patient adherence, as it only works if taken consistently (Fuller & Gordis, 2004).
2.2 Naltrexone
Naltrexone, which is also used to treat OUD, has been shown to be effective in treating AUD as well. It works by blocking opioid receptors, which are involved in the rewarding effects of alcohol. This reduces the pleasurable sensations associated with drinking, helping to curb cravings and decrease heavy drinking. Both oral and extended-release injectable forms of naltrexone are available, with the latter showing higher rates of adherence due to its once-monthly administration. Research has demonstrated that naltrexone can significantly reduce the risk of relapse and help individuals maintain abstinence from alcohol (Anton et al., 2006).
2.3 Acamprosate
Acamprosate is another medication used to treat AUD, though its mechanism of action is not fully understood. It is believed to stabilize brain chemistry by modulating glutamate and GABA neurotransmitter systems, which are disrupted by chronic alcohol use. Acamprosate is typically used to help individuals maintain abstinence after they have stopped drinking, rather than during the detoxification phase. A large clinical trial known as the COMBINE study found that acamprosate was most effective in promoting abstinence when used in combination with behavioral therapies and support systems (Gustafson et al., 2014).
- 3.
Medications for Nicotine Addiction
Nicotine addiction remains a significant public health issue, contributing to various chronic diseases, including lung cancer, cardiovascular disease, and respiratory illness. Pharmacological treatments for nicotine addiction primarily aim to reduce withdrawal symptoms and cravings, helping individuals quit smoking or using other nicotine products.
3.1 Nicotine Replacement Therapy (NRT)
Nicotine replacement therapy (NRT) involves the use of products that deliver nicotine to the body without the harmful chemicals found in tobacco products. These products include nicotine patches, gums, lozenges, nasal sprays, and inhalers. NRT helps reduce withdrawal symptoms and cravings, making it easier for individuals to quit smoking. Studies have shown that NRT is effective in increasing quit rates, especially when combined with behavioral interventions (Stead et al., 2012).
3.2 Bupropion
Bupropion is an atypical antidepressant that has been approved for smoking cessation. It works by inhibiting the reuptake of dopamine and norepinephrine, which helps reduce cravings and withdrawal symptoms associated with nicotine dependence. Bupropion has been shown to nearly double the chances of quitting smoking compared to placebo, and its efficacy is enhanced when combined with behavioral support (Hughes et al., 2004).
3.3 Varenicline
Varenicline is a partial agonist of the nicotinic acetylcholine receptor, which is involved in the addictive properties of nicotine. It works by stimulating the receptor to reduce cravings and withdrawal symptoms while also blocking the effects of nicotine if a person smokes during treatment. Varenicline has been shown to be one of the most effective pharmacological treatments for nicotine addiction, significantly increasing the likelihood of quitting compared to placebo or other medications (Cahill et al., 2013).
- 4.
Medications for Stimulant Use Disorder
Currently, there are no FDA-approved medications for the treatment of stimulant use disorders, such as cocaine or methamphetamine addiction. However, several pharmacological agents are being investigated for their potential efficacy in treating these disorders.
4.1 Modafinil
Modafinil, a stimulant commonly used to treat narcolepsy, has shown promise in reducing cocaine use in some studies. Its mechanism of action involves increasing levels of dopamine in the brain, which may help reduce cravings for cocaine. However, clinical trials have produced mixed results, and modafinil has not yet been approved for the treatment of stimulant use disorders (Karila et al., 2011).
4.2 Bupropion
Bupropion has also been studied for its potential to treat stimulant use disorders, particularly methamphetamine addiction. As an atypical antidepressant, bupropion’s dopaminergic activity may help reduce cravings for stimulants. Although some studies have shown positive outcomes, further research is needed to establish its efficacy in treating stimulant use disorders (Heinzerling et al., 2014).
- 5.
Combining Pharmacological and Psychotherapeutic Treatments
The integration of pharmacological treatments with psychotherapeutic interventions is considered the gold standard in the treatment of SUDs. Pharmacotherapy can address the biological aspects of addiction, such as withdrawal symptoms and cravings, while psychotherapy helps individuals develop coping mechanisms and address underlying psychological issues. Research has consistently shown that combined treatments produce better outcomes than either pharmacotherapy or psychotherapy alone (McLellan et al., 1993).
Psychotherapeutic Treatments
Psychotherapeutic treatments form the cornerstone of many interventions for substance use disorders (SUDs). These treatments focus on modifying the underlying psychological, behavioral, and emotional components of addiction. While the effectiveness of psychotherapeutic interventions in treating SUDs is well-established, these treatments have continued to evolve, integrating new approaches and techniques aimed at improving outcomes. The role of psychotherapy in SUD treatment is diverse, encompassing a range of modalities from well-established cognitive-behavioral therapy (CBT) to emerging strategies like mindfulness-based therapies and contingency management.
- -
Cognitive-Behavioral Therapy (CBT)
Cognitive-behavioral therapy is one of the most widely used and researched psychotherapeutic approaches for SUDs. CBT operates on the premise that maladaptive behaviors and thought patterns contribute to substance use, and it aims to teach individuals skills for recognizing and changing these patterns (Beck, Wright, Newman, & Liese, 1993). Techniques such as identifying triggers, developing coping strategies, and learning to challenge and reframe harmful beliefs are central to CBT’s approach in helping patients avoid relapse and maintain sobriety.
A meta-analysis by Magill and Ray (2009) found that CBT is highly effective in treating alcohol and drug use disorders. The study showed that individuals undergoing CBT were more likely to achieve abstinence and maintain long-term recovery compared to those receiving no psychotherapeutic treatment or minimal intervention. The effectiveness of CBT is largely attributed to its structured nature, allowing individuals to develop and practice new skills in a systematic way.
- -
Motivational Interviewing (MI)
Motivational interviewing (MI) is another key psychotherapeutic technique widely used in the treatment of SUDs. MI is a client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence (Miller & Rollnick, 2012). Rather than confronting individuals about their substance use directly, MI seeks to help them articulate their reasons for change and recognize the discrepancies between their current behavior and long-term goals. The efficacy of MI in SUD treatment has been well-documented in various studies. A review by Lundahl and Burke (2009) found that MI is effective in improving treatment adherence and reducing substance use across a range of populations, including adolescents and adults. The collaborative and non-judgmental nature of MI makes it particularly suitable for individuals who may initially be resistant to treatment, helping them build motivation for long-term recovery.
- -
Contingency Management (CM)
Contingency management is an evidence-based psychotherapeutic intervention that uses tangible rewards to reinforce abstinence from substance use. CM is based on the principles of operant conditioning, where desirable behaviors (e.g., negative drug tests) are reinforced with rewards such as vouchers or prizes (Higgins et al., 2000). The idea behind CM is that by providing immediate positive reinforcement for sobriety, individuals will be more likely to continue engaging in recovery-supportive behaviors.
Research has consistently shown that CM is effective in treating a range of substance use disorders, particularly stimulant and opioid use disorders. For instance, a study by Petry, Alessi, and Ledgerwood (2010) found that individuals receiving CM were significantly more likely to remain abstinent during treatment and to continue engaging with therapeutic services compared to those receiving standard care. While the logistics of implementing CM can be complex, especially in resource-limited settings, its efficacy has made it a critical component in many treatment programs.
- -
Mindfulness-Based Relapse Prevention (MBRP)
In recent years, mindfulness-based relapse prevention (MBRP) has gained popularity as an adjunct to traditional psychotherapeutic treatments for SUDs. MBRP integrates mindfulness practices with cognitive-behavioral strategies to help individuals develop awareness of their thoughts and emotions without reacting impulsively to them (Bowen et al., 2009). The goal of MBRP is to reduce relapse by increasing individuals' ability to cope with cravings and high-risk situations through mindfulness techniques such as meditation and body awareness.
A randomized controlled trial by Bowen et al. (2014) demonstrated that MBRP was more effective than standard relapse prevention and treatment-as-usual in reducing relapse rates among individuals with SUDs. Participants who received MBRP reported fewer days of substance use and a greater ability to manage stress and cravings. The growing body of research supporting MBRP highlights the importance of integrating holistic approaches into SUD treatment, focusing not only on behavior but also on the underlying emotional and cognitive processes that contribute to substance use.
- -
Dialectical Behavior Therapy (DBT)
Dialectical behavior therapy (DBT), originally developed for individuals with borderline personality disorder, has also been adapted for use in treating substance use disorders. DBT combines cognitive-behavioral techniques with mindfulness practices, emphasizing emotional regulation, distress tolerance, and interpersonal effectiveness (Linehan, 1993). DBT’s structured approach makes it particularly suitable for individuals with co-occurring mental health disorders, which are common among those with SUDs.
Research by Linehan et al. (1999) found that DBT was effective in reducing substance use and improving overall mental health outcomes in individuals with co-occurring SUDs and emotional dysregulation. The skills taught in DBT—such as tolerating distress and regulating emotions—are critical for preventing relapse, particularly in individuals who may use substances as a way to cope with overwhelming emotions.
- -
Family Therapy
Family therapy is another psychotherapeutic intervention that has shown significant promise in the treatment of SUDs. Substance use disorders often have profound effects on family dynamics, and involving the family in treatment can be crucial for long-term recovery. Family therapy helps address dysfunctional family patterns that may contribute to substance use and provides a platform for family members to work together in supporting the individual’s recovery (O'Farrell & Fals-Stewart, 2006).
Behavioral couples therapy (BCT) is one form of family therapy that has been particularly effective in treating alcohol use disorders. A study by O'Farrell et al. (2012) found that individuals who participated in BCT had higher rates of abstinence and better relationship satisfaction compared to those receiving individual therapy alone. The collaborative approach of BCT helps improve communication, reduce conflict, and foster a supportive environment for recovery.
- -
Emerging Psychotherapeutic Approaches
In addition to the well-established psychotherapies mentioned above, new approaches continue to emerge, reflecting the dynamic nature of the field. For example, acceptance and commitment therapy (ACT) is gaining traction as a treatment for SUDs. ACT encourages individuals to accept their thoughts and feelings rather than attempting to avoid or change them, while committing to behavior change aligned with their values (Hayes et al., 2006).
A study by Luoma, Kohlenberg, Hayes, Bunting, and Rye (2008) demonstrated that ACT can reduce shame and stigma associated with substance use, helping individuals to engage more fully in their recovery process. This emphasis on acceptance and value-driven behavior makes ACT a promising option, particularly for individuals who struggle with self-judgment and shame around their addiction.
Recovery Coaching and Peer Recovery Coaching
Recovery coaching differs from traditional clinical interventions in that it is non-clinical and focuses on providing mentorship and guidance. Coaches work with individuals to develop personalized recovery plans, address barriers to recovery, and provide accountability for achieving recovery goals (White, 2009). Unlike therapists or counselors, recovery coaches do not focus on diagnosing or treating SUDs but rather on empowering individuals to take control of their recovery journey.
Peer recovery coaching takes this model a step further by involving coaches who have lived experience with addiction and recovery. This peer-based approach leverages the power of shared experiences to build trust and rapport, creating an environment where individuals feel understood and supported (Eddie et al., 2019). Peer coaches serve as role models and mentors, providing practical advice on overcoming challenges related to addiction, relapse prevention, and building a fulfilling life in recovery.
With the rise of telehealth platforms, both recovery coaching and peer recovery coaching have increasingly shifted to remote delivery. This shift has been accelerated by the COVID-19 pandemic, which necessitated the rapid adoption of remote healthcare solutions. Remote recovery coaching offers numerous advantages, including increased accessibility for individuals who may not have access to in-person services due to geographical, financial, or logistical barriers (Tracy et al., 2016).
Through video calls, phone calls, text messaging, and online platforms, recovery coaches can provide consistent, ongoing support regardless of location. This continuous access to support is particularly valuable for individuals in recovery, as it allows them to stay connected with their coach and receive timely guidance when faced with triggers or challenges (Bassuk et al., 2016).
One of the most significant benefits of remote recovery coaching is its ability to reach individuals in underserved areas. People living in rural or remote locations often have limited access to SUD treatment services, and recovery coaching delivered remotely can bridge this gap. Research has shown that telehealth approaches, including remote coaching, can effectively engage individuals who might not otherwise seek help due to logistical constraints or the stigma associated with attending in-person treatment (McKay & Weiss, 2001).
Remote recovery coaching offers unparalleled flexibility, allowing individuals to receive support on their terms. Sessions can be scheduled at convenient times, and communication can take place through various platforms, including video conferencing, text messaging, or phone calls. This flexibility makes it easier for individuals to fit recovery coaching into their daily lives, particularly for those balancing work, family, or other responsibilities (Ashford et al., 2018).
Incorporating recovery coaching into telehealth models provides continuous care, which is crucial for individuals in recovery. Frequent check-ins with a coach can help individuals stay accountable, monitor progress, and address challenges in real time. Remote coaching also allows for immediate support during moments of crisis or vulnerability, providing a safety net that can prevent relapse (Bassuk et al., 2016).
One of the defining features of peer recovery coaching is the emphasis on shared lived experiences. Research has demonstrated that peer support can play a critical role in recovery by fostering a sense of belonging and mutual understanding. Peer coaches offer unique perspectives that clinical providers may not have, as they have personally navigated the challenges of addiction and recovery (Tracy & Wallace, 2016). This shared experience helps build trust and rapport, encouraging individuals to open up about their struggles and feel less isolated in their recovery journey.
Integrated Treatment Programs
The importance of integrated treatment programs becomes evident when considering the high rates of co-occurring mental health disorders (often referred to as dual diagnosis) among individuals with SUDs. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), about 37.9% of adults with substance use disorders also suffer from co-occurring mental illnesses such as depression, anxiety, bipolar disorder, or post-traumatic stress disorder (PTSD) (SAMHSA, 2020). Traditional models of care often treated these conditions separately, leading to fragmented care and poorer outcomes. Individuals with co-occurring disorders were typically shuffled between addiction treatment services and mental health providers, with little coordination between the two, resulting in gaps in care that frequently led to relapse or worsening symptoms of both conditions (Drake et al., 2001).
Integrated treatment programs were developed to address these shortcomings by offering comprehensive care that simultaneously addresses SUDs and co-occurring mental health disorders. These programs recognize that both conditions interact and influence each other, necessitating a cohesive treatment plan that considers all aspects of an individual’s health.
There are several models of integrated treatment that vary in their approach to care delivery. Some programs focus primarily on integrating addiction treatment with mental health services, while others incorporate additional elements, such as primary medical care, housing support, and vocational services. Each model seeks to provide a "whole-person" approach that tailors treatment to the unique needs of each individual.
- -
Integrated Dual Diagnosis Treatment (IDDT)
The Integrated Dual Diagnosis Treatment (IDDT) model is one of the most established frameworks for treating individuals with co-occurring mental health disorders and SUDs. IDDT is an evidence-based practice that provides combined mental health and addiction treatment services in a single setting. The core principles of IDDT include a long-term, stage-wise approach to recovery, motivational interventions, comprehensive services, and individualized treatment plans (Mueser et al., 2003). Research has shown that IDDT significantly improves outcomes for individuals with dual diagnoses by reducing substance use, improving psychiatric symptoms, enhancing quality of life, and increasing housing stability (Brunette & Mueser, 2006).
A study by Drake et al. (2004) found that individuals receiving IDDT were more likely to achieve sobriety, maintain stable housing, and experience improved mental health outcomes compared to those receiving traditional, non-integrated treatment. The study concluded that integrated treatment was particularly effective for individuals with severe mental health disorders such as schizophrenia, bipolar disorder, and major depressive disorder.
- -
Assertive Community Treatment (ACT)
Another successful model for integrated treatment is Assertive Community Treatment (ACT), a team-based approach that provides intensive, individualized care for people with severe mental illness and SUDs. ACT teams typically include psychiatrists, nurses, social workers, and substance abuse counselors who collaborate to offer comprehensive services in the community, rather than in a clinical setting (Bond & Drake, 2015). ACT is often used for individuals with co-occurring disorders who have difficulty engaging with traditional outpatient care due to factors such as homelessness, legal issues, or frequent hospitalizations.
The effectiveness of ACT in reducing hospitalizations, improving housing outcomes, and reducing substance use has been well documented. A meta-analysis conducted by Coldwell and Bender (2007) found that ACT was associated with significant reductions in psychiatric hospitalizations and improvements in housing stability for individuals with co-occurring SUDs and mental illness. The study also highlighted that the flexible, community-based nature of ACT allows individuals to receive care in real-world settings, making it easier to address both substance use and mental health symptoms as they arise in daily life.
- -
Integrated Primary Care and SUD Treatment
In recent years, there has been growing recognition of the need to integrate SUD treatment with primary care services. Many individuals with SUDs suffer from chronic medical conditions such as hepatitis C, HIV, diabetes, and cardiovascular disease, all of which are exacerbated by substance use (Kresina & Lubran, 2011). Integrated primary care models aim to address the physical health needs of individuals with SUDs while simultaneously providing addiction treatment and mental health services. This holistic approach helps to improve overall health outcomes and reduces the risk of medical complications related to untreated physical conditions.
The implementation of Medication-Assisted Treatment (MAT) within primary care settings is an example of integrated care in action. MAT combines pharmacotherapy (such as methadone, buprenorphine, or naltrexone) with counseling and behavioral therapies to treat opioid use disorder. Research has shown that providing MAT in primary care settings increases accessibility, reduces stigma, and leads to better treatment retention (Kampman & Jarvis, 2015). A study by Fiellin et al. (2002) demonstrated that primary care-based buprenorphine treatment was effective in reducing opioid use and promoting long-term recovery in individuals with opioid dependence.
- -
Housing First Models
For individuals with SUDs who also experience homelessness or housing instability, integrated treatment programs that incorporate housing support have proven to be highly effective. The "Housing First" model is an evidence-based approach that provides immediate access to stable housing without preconditions, such as sobriety, and then integrates comprehensive support services to address substance use, mental health, and other needs (Tsemberis et al., 2004). Housing First programs are particularly effective in reducing substance use and improving overall well-being by offering individuals a safe and stable environment in which they can focus on recovery.
Research by Padgett, Gulcur, and Tsemberis (2006) found that individuals participating in Housing First programs were more likely to achieve long-term housing stability and had better outcomes in terms of substance use reduction and mental health symptom management compared to individuals in traditional treatment programs that required sobriety as a precondition for housing. The study highlighted the importance of addressing basic needs, such as housing, as part of an integrated approach to SUD treatment.
- -
Benefits of Integrated Treatment Programs
Integrated treatment programs offer several key advantages over traditional, non-integrated care models. One of the most significant benefits is improved treatment retention and engagement. Individuals with co-occurring disorders or complex medical and social needs often face barriers to accessing care, including transportation issues, stigma, and a lack of coordinated services. By providing all necessary services in a single, coordinated program, integrated treatment makes it easier for individuals to stay engaged in care over the long term (Sterling et al., 2011).
Additionally, integrated treatment programs are more effective in addressing the full range of issues that contribute to substance use. For example, individuals with co-occurring mental health disorders may use substances as a way of self-medicating their symptoms. By addressing both the substance use and the underlying mental health condition, integrated treatment programs can help individuals develop healthier coping mechanisms and achieve sustained recovery (Drake & Wallach, 2000).
- -
Challenges and Considerations in Integrated Treatment
While integrated treatment programs offer numerous benefits, they also present challenges that must be addressed to ensure their success. One of the main challenges is the need for adequate training and support for healthcare providers. Professionals working in integrated treatment settings must be equipped to address a wide range of issues, including substance use, mental health disorders, medical conditions, and social determinants of health. This requires ongoing training and collaboration among multidisciplinary teams (Priester et al., 2016).
Another challenge is funding and reimbursement for integrated care. In many healthcare systems, funding streams for mental health, substance use treatment, and medical care are separate, which can make it difficult to provide fully integrated services. Policymakers and healthcare organizations must work together to develop funding models that support the comprehensive, coordinated care provided by integrated treatment programs (Morrissey et al., 2005).
Barriers to Traditional Treatment
Despite the efficacy of these treatments, several barriers limit their accessibility and effectiveness. These include geographic limitations, long waiting times, the stigma associated with seeking help, and high treatment costs (Substance Abuse and Mental Health Services Administration, 2020). These barriers highlight the need for innovative approaches to make SUD treatment more accessible and effective.
Traditional treatment methods for substance use disorders (SUDs), while effective, encounter numerous barriers that limit their accessibility and efficacy for many individuals who need help. These barriers range from logistical and structural issues to personal and societal challenges, and their impact can often discourage or prevent individuals from seeking or continuing treatment.
Logistical and Structural Barriers
One of the most significant logistical barriers to accessing SUD treatment is geographic location. Many individuals live in areas that lack adequate treatment facilities, particularly in rural or underserved urban areas. This geographic disparity forces individuals to travel long distances for care, adding travel costs and time to the already substantial burden of seeking treatment (Andrilla et al., 2019). Additionally, the availability of specialized healthcare providers, such as addiction specialists or psychiatrists, is often limited in these areas, further complicating access to appropriate care.
Financial constraints also play a critical role in limiting access to SUD treatment. Many individuals struggling with substance use disorders lack health insurance or have insurance that does not cover all necessary aspects of SUD treatment, such as certain medications or long-term psychotherapy. The high cost of treatment programs, including inpatient care and specialized therapies, can be prohibitively expensive, deterring individuals from initiating or continuing treatment (Saloner & Cook, 2013).
Stigma and Societal Attitudes
Stigma associated with substance use and addiction remains a powerful barrier to treatment. Societal views that frame addiction as a moral failing rather than a medical condition can lead to shame and self-stigma among individuals with SUDs, discouraging them from seeking treatment due to fear of judgment from others (Livingston et al., 2012). This stigma can permeate various aspects of life, affecting personal relationships, employment opportunities, and interaction with healthcare systems, where individuals with SUDs may experience bias and discrimination from healthcare providers, further deterring them from seeking help.
Systemic Healthcare Issues
The healthcare system itself presents additional barriers. There is often a lack of integration between mental health services and other medical care, making it difficult for patients to receive comprehensive treatment addressing both substance use and other co-occurring health issues. The fragmentation of services can lead to poor coordination of care, conflicting treatments, and a higher likelihood of treatment dropout (Drake et al., 2001).
Regulatory issues also complicate the provision of care, particularly with medications used in addiction treatment. Regulations surrounding drugs like methadone and buprenorphine can restrict their use to specialized clinics or require practitioners to have specific certifications, limiting the number of providers who can prescribe these effective treatments (Volkow et al., 2014).
Personal and Psychological Barriers
Personal barriers also play a significant role in treatment engagement. Many individuals with substance use disorders also struggle with mental health disorders such as depression or anxiety, which can complicate the treatment process and reduce motivation to seek or adhere to treatment (Conway et al., 2006). Psychological barriers, such as denial of the severity of one’s addiction or fear of confronting painful emotional issues during therapy, can also impede the treatment process.
Additionally, the relapse-prone nature of addiction leads to cyclical entries into and exits from treatment, often influenced by personal circumstances, emotional states, and external pressures, which can discourage both patients and providers by creating a sense of futility around the treatment process.
Telemedicine and Online Interventions
Telemedicine involves the use of electronic communications and software to provide clinical services to patients without an in-person visit. Online interventions can include a range of services, from virtual counseling sessions to mobile health applications designed to support recovery (World Health Organization, 2010).
Telemedicine and online interventions represent a rapidly evolving sector within the broader context of healthcare, characterized by the use of electronic communications and information technologies to provide and support healthcare services when participants are separated by distance. This field has become particularly relevant for the treatment of substance use disorders (SUDs), offering an alternative to traditional face-to-face therapeutic models that can be limited by geographic, temporal, and socio-economic barriers.
Definition of Telemedicine
Telemedicine involves the delivery of health services using telecommunications technology to facilitate real-time interaction between a patient and a healthcare provider. This can include consultations via video conferencing, remote monitoring of patients' symptoms and medication management, and the use of digital platforms to provide continuous support and intervention (World Health Organization, 2010). The primary goal of telemedicine is to make healthcare accessible in remote areas, reducing the need for travel and enabling timely care delivery.
Online Interventions
Online interventions for SUDs typically encompass a range of services, including but not limited to, structured therapy sessions delivered through web-based platforms, mobile health applications designed to support recovery, and automated self-help tools that provide cognitive-behavioral therapy (CBT) and motivational interviewing (MI) techniques. These interventions are designed to be flexible, allowing users to access support at their convenience, which can significantly enhance engagement and adherence to treatment protocols (Kay-Lambkin et al., 2011).
Scope of Telemedicine and Online Interventions
The scope of telemedicine and online interventions is broad and multifaceted. It includes:
1. Virtual Consultations: Patients can consult with addiction specialists and mental health professionals without the need to travel, thus overcoming geographical barriers that often hinder access to care.
2. Digital Therapy Sessions: These sessions can be conducted via video calls, chats, or even through asynchronous messaging platforms, providing flexibility in scheduling and maintaining patient privacy and convenience.
3. Remote Monitoring: Wearable devices and mobile applications can monitor physiological indicators such as heart rate and stress levels, which can be useful for managing withdrawal symptoms and preventing relapse.
4. Self-management Tools: Online platforms often offer educational resources and tools for self-management, helping patients to develop skills necessary for recovery maintenance outside of formal therapy sessions.
5. Support Networks: Many online programs include access to peer support groups or forums where individuals can share their experiences and challenges, fostering a sense of community and mutual support.
Efficacy and Advantages
The efficacy of telemedicine and online interventions in treating SUDs has been supported by numerous studies. A systematic review by Lin et al. (2019) concluded that telemedicine could deliver outcomes comparable to those of conventional face-to-face treatments for various conditions, including SUDs. The accessibility, cost-effectiveness, and potential to reach underserved populations are among the primary advantages of telemedicine and online interventions. Moreover, the anonymity and privacy provided by online platforms can help reduce the stigma associated with seeking treatment for SUDs, which is often a significant barrier to accessing care (Cunningham et al., 2010).
Efficacy of Telemedicine in Sud Treatment
Research indicates that telemedicine can be as effective as in-person treatment for SUDs. A meta-analysis by Lin et al. (2019) found that telehealth interventions resulted in similar outcomes to face-to-face treatments regarding abstinence rates and treatment retention. Furthermore, telemedicine offers the advantage of increased accessibility, particularly for individuals in remote or underserved areas.
Telemedicine has demonstrated promising results as an effective modality for the treatment of substance use disorders (SUDs). Its utilization has grown significantly, particularly as it offers an alternative to conventional in-person treatment models, which can be limited by barriers such as accessibility, stigma, and logistical challenges.
Comparative Efficacy with Traditional Treatments
Studies comparing the efficacy of telemedicine to traditional face-to-face therapy have generally found that telemedicine can produce outcomes that are equivalent to or better than those of traditional settings. For example, a meta-analysis by Lin et al. (2019) reviewed various telemedicine interventions and found that these methods were effective in treating SUDs, showing similar treatment adherence and satisfaction levels among patients compared to those receiving conventional treatment. This suggests that telemedicine is not only a viable alternative but also a potentially preferable option for certain populations.
Treatment Retention and Completion Rates
One of the critical measures of treatment efficacy in SUDs is the retention rate, which is often higher in telemedicine programs compared to traditional in-person treatment programs. This increase can be attributed to the greater accessibility and flexibility of telemedicine, which allows patients to engage in therapy sessions from the comfort of their homes, thereby reducing dropout rates associated with logistical difficulties such as transportation and scheduling conflicts (Eibl et al., 2017).
Reduction in Substance Use
Telemedicine interventions have also been shown to effectively reduce substance use among participants. Research by Chaple et al. (2018) demonstrated that telehealth services, including online counseling and digital monitoring, significantly decreased the use of substances among participants over time. These findings are supported by the convenience and continuous support offered by telemedicine, which may enhance patient engagement and adherence to treatment protocols.
Improvement in Associated Psychological Symptoms
Telemedicine has been particularly beneficial in addressing not only substance use but also the psychological comorbidities often associated with SUDs, such as depression and anxiety. A study by King et al. (2020) found that participants receiving telemedicine interventions for SUDs reported significant improvements in their overall mental health. This is likely due to the holistic approach of telemedicine programs, which often integrate various treatment modalities, including cognitive-behavioral therapy and motivational interviewing, that address both substance use and underlying mental health issues.
Advantages Over Traditional Treatment Modalities
The primary advantage of telemedicine in the treatment of SUDs is its ability to overcome geographical and physical barriers to access. Patients in rural or underserved areas, who previously had limited access to specialized care, can now receive high-quality treatment remotely (Yellowlees et al., 2018). Furthermore, telemedicine can be more convenient for patients, as it eliminates the need for travel and allows for scheduling flexibility.
Telemedicine can also be more cost-effective than traditional treatment methods. By reducing the need for physical infrastructure and minimizing travel and administrative costs, telemedicine can lower the overall cost of care delivery. These savings can then be passed on to the patient, making treatment more affordable (Bradford et al., 2016).
Another significant benefit of telemedicine is the increased privacy and anonymity it offers, which can help reduce the stigma associated with seeking treatment for SUDs. This can encourage more individuals to seek help early, potentially leading to better long-term outcomes (Link et al., 2001).
Online Counseling and Therapy
Online counseling, including video conferencing and chat-based services, allows individuals to receive therapy in a convenient and private manner. Studies have shown that online CBT and MI can effectively reduce substance use and improve mental health outcomes (Kay-Lambkin et al., 2011). The flexibility and anonymity of online therapy can also help reduce the stigma associated with seeking help for addiction (Cunningham et al., 2010).
Online counseling and therapy have emerged as vital components in the treatment of substance use disorders (SUDs), leveraging technology to overcome traditional barriers to access and enhance patient engagement. This method of delivery not only broadens the reach of therapeutic services but also introduces a level of convenience and accessibility that is not typically available with conventional face-to-face therapy sessions.
Overview of Online Counseling and Therapy Modalities
Online counseling for SUDs can take various forms, including synchronous video sessions, asynchronous messaging, and digital therapy modules. These services are often provided via secure platforms that ensure privacy and confidentiality, which are critical concerns for individuals seeking treatment for substance use issues.
Video Conferencing
Video conferencing is one of the most common forms of online therapy, offering real-time interaction between the therapist and the client. This format closely replicates the experience of traditional in-person therapy by allowing for visual cues and immediate feedback, which are essential for building rapport and facilitating therapeutic interventions. Research has indicated that video-based counseling can be just as effective as in-person sessions in reducing symptoms of SUDs and improving patient outcomes (Backhaus et al., 2012).
Asynchronous Communication
Asynchronous communication methods, such as email and text messaging, allow clients to communicate with their therapists at their convenience. This modality can be particularly beneficial for those who may need more time to articulate their thoughts and feelings or who have schedules that make live sessions difficult. Studies, such as those by Aguilera and Muñoz (2011), have shown that asynchronous messaging can effectively support treatment by enabling continuous communication and support, which can help maintain engagement between live sessions.
Digital Therapy Platforms
Digital therapy platforms often combine various therapeutic tools and resources, such as interactive modules based on cognitive-behavioral therapy (CBT) principles, motivational interviewing (MI) techniques, and educational content related to substance use and recovery. These platforms can provide a structured therapy experience that is accessible at any time and can be tailored to the individual’s specific needs and progress. Research by Marsch (2012) highlights the effectiveness of such platforms in improving treatment outcomes by providing consistent and personalized support.
Benefits of Online Counseling and Therapy
The benefits of online counseling and therapy for SUDs are manifold. They include increased accessibility for individuals living in remote areas or those with mobility limitations who might not otherwise have access to specialist treatment services. Online therapy also offers greater flexibility in scheduling, allowing clients to engage in treatment sessions outside of typical office hours and from any location, thus reducing disruption to daily commitments and enhancing privacy (Postel et al., 2008).
Moreover, online counseling can significantly reduce the stigma associated with seeking treatment. The private nature of digital interactions can encourage more individuals to seek help without fear of judgment or exposure. The anonymity provided by online platforms can also lower barriers to entry, particularly for those who may be hesitant to engage in traditional therapy settings (Schueller et al., 2013).
Challenges and Considerations
Despite its benefits, online counseling and therapy for SUDs also present several challenges. These include ensuring technological accessibility and digital literacy among users, maintaining privacy and security in digital communications, and building a therapeutic alliance in the absence of physical presence, which can be crucial for some therapeutic outcomes. Additionally, regulatory and licensing issues can complicate the provision of online therapy across state or national borders, requiring careful navigation and compliance with diverse legal frameworks (Luxton et al., 2012).
Mobile Health Applications
Mobile health applications offer a novel way to support individuals in their recovery journey. These apps can provide resources such as educational materials, self-monitoring tools, and access to peer support networks. A study by Gustafson et al. (2014) demonstrated that a smartphone app designed to support recovery significantly reduced relapse rates among individuals with alcohol use disorder.
Mobile health applications are increasingly recognized as powerful tools in the treatment and management of substance use disorders (SUDs). These applications offer a range of functionalities, including symptom tracking, treatment adherence, peer support, and educational resources, all of which are accessible directly from a user's smartphone or tablet. The integration of mobile health apps into SUD treatment plans can significantly enhance patient engagement and provide continuous support, critical elements for successful recovery.
Core Functionalities of Mobile Health Applications
Mobile apps often include features for monitoring symptoms related to SUDs, such as craving intensity, mood fluctuations, and potential triggers. This real-time data collection allows both patients and clinicians to track progress and identify patterns in behavior that may require intervention. For example, the study by Gustafson et al. (2014) demonstrated that an app designed to support recovery from alcoholism significantly reduced risky drinking days among its users by providing tools for self-monitoring and feedback.
Another crucial functionality is treatment adherence, where apps can send reminders for medication intake, therapy sessions, or meetings with healthcare providers. This feature is particularly useful in managing SUDs, where consistency in medication and therapy adherence can play a significant role in recovery outcomes. Apps may also include features to help manage side effects and drug interactions, providing users with timely information and advice to handle potential issues (Marsch & Dallery, 2012).
Many mobile health applications facilitate connections with peer support groups and forums where individuals can share their experiences, challenges, and successes in recovery. This sense of community can be incredibly beneficial, as social support is a well-known protective factor in the treatment of SUDs. Apps like Sober Grid offer geosocial networking features that connect users with a recovery community, providing support and fostering accountability (Ashford et al., 2019).
Education is a fundamental component of effective SUD treatment. Mobile apps can deliver tailored educational content that helps users understand the nature of addiction, the processes of recovery, and strategies for relapse prevention. This information is often presented in user-friendly formats, such as short videos, interactive quizzes, and infographics, making it easily digestible and engaging (Lord et al., 2015).
The benefits of using mobile health applications in treating SUDs include increased accessibility to treatment resources, enhanced ability to personalize care, and improved capacity for data collection and analysis. These apps not only make treatment more accessible but also allow for a more individualized approach by adapting interventions based on the user's behavior and feedback.
One of the most significant advantages of mobile health apps is the ability to deliver interventions in real-time. For instance, an app can provide coping strategies and motivational content when a user reports high levels of craving or stress, potentially averting relapse (Luxton et al., 2011).
Mobile health applications offer a cost-effective solution for both healthcare providers and patients. By reducing the need for frequent in-person visits and utilizing automated systems for routine monitoring and education, these apps can decrease the overall cost of SUD treatment (Torous & Firth, 2016).
While mobile health applications hold significant promise in the field of SUD treatment, there are challenges to consider, including issues related to privacy, data security, and user engagement. Ensuring the confidentiality and security of sensitive health data is paramount, as is designing user-friendly interfaces that can maintain user engagement over time. Additionally, the effectiveness of mobile interventions often depends on the integration with traditional healthcare services and the continuous updating of content to reflect current research and best practices (Bauer et al., 2017).
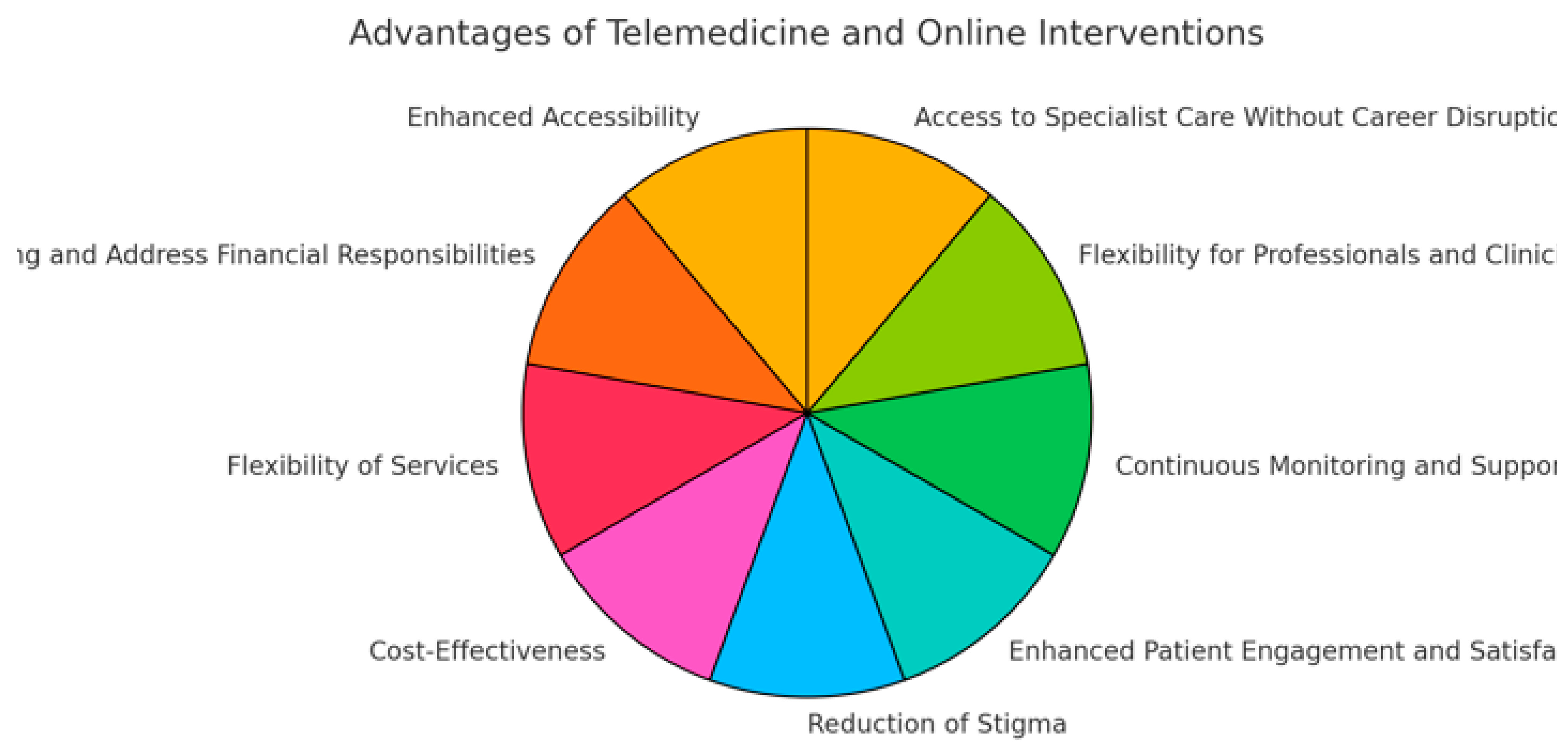
Advantages of Telemedicine and Online Interventions
Telemedicine and online interventions have revolutionized the approach to healthcare, particularly in the field of substance use disorders (SUDs). These technological advancements offer significant benefits over traditional in-person therapy by improving accessibility, reducing costs, and enhancing patient engagement, among other advantages.
One of the most significant benefits of telemedicine and online interventions is the remarkable improvement in accessibility they provide. Patients living in remote or underserved areas, where specialty care is often scarce or non-existent, can receive high-quality treatment without the need to travel. This is particularly important for substance use disorder (SUD) treatment, where timely access to care can be critical for preventing relapse and maintaining recovery. Studies have shown that telemedicine can significantly increase the reach of healthcare services, ensuring that more individuals can access necessary care without geographical limitations (Yellowlees et al., 2018).
Telemedicine also mitigates other barriers to accessing care, such as financial constraints, physical disabilities, and limited transportation options. According to Hilty et al. (2013), telemedicine helps reduce the cost burden for patients by eliminating the need for long commutes to treatment centers, which is particularly beneficial for those in rural areas who may otherwise struggle to attend regular therapy sessions. This model also allows for more frequent and consistent follow-up appointments, further enhancing patient engagement and retention in treatment.
Furthermore, online interventions provide a viable solution for individuals with social anxiety, agoraphobia, or those who are uncomfortable attending in-person treatment due to stigma or privacy concerns. Shore et al. (2014) found that telemedicine significantly increased treatment adherence among populations that were reluctant to seek face-to-face help, underscoring its importance in breaking down social and psychological barriers to care. These benefits highlight how telemedicine extends beyond geographic accessibility to offer more flexible, inclusive care options that cater to the diverse needs of individuals struggling with SUDs.
As technology continues to advance, the integration of mobile health applications and remote monitoring tools into telemedicine services has further expanded accessibility. These tools allow patients to track their progress in real-time and stay connected with their healthcare providers, even in areas with limited infrastructure (Bashshur et al., 2016). This constant connectivity ensures that patients can receive timely interventions, reducing the likelihood of relapse or medical emergencies. In summary, telemedicine and online interventions not only improve physical access to care but also address the broader systemic and psychological barriers that often prevent individuals from seeking and maintaining treatment.
- 2.
Ability to Continue Working and Address Financial Responsibilities
Another significant advantage of online treatment is the opportunity for individuals to continue working while undergoing therapy. This is particularly important for those who may be facing financial difficulties, including debts incurred as a result of their substance use. Maintaining employment during treatment allows individuals to manage their financial obligations, such as mortgage payments, credit card debts, or legal fees, which can be a source of stress and a potential barrier to recovery (McLellan et al., 2007).
In traditional treatment settings, many patients are required to take time off work, which can exacerbate financial problems and lead to further stress. Online treatment, by contrast, allows individuals to receive therapy at times that fit their work schedules, whether through flexible appointment times, asynchronous communication with counselors, or self-paced online modules (Eysenbach et al., 2005). This flexibility enables patients to address both their addiction and their financial responsibilities concurrently, reducing the financial pressures that might otherwise lead to relapse.
Moreover, continuing to work while in treatment may contribute to a sense of normalcy and self-worth, both of which are critical components of recovery. For many individuals, maintaining their professional identity can bolster their motivation to stay sober and engage fully in their treatment. A study by Kay-Lambkin et al. (2011) found that individuals who were able to continue working during their recovery reported higher levels of satisfaction with their treatment and were more likely to maintain long-term sobriety compared to those who had to leave their jobs.
- 3.
Flexibility of Services
Telemedicine also offers unprecedented flexibility in scheduling and treatment modalities, a key benefit that has transformed the way patients engage with healthcare. Unlike traditional in-person visits, where patients must conform to fixed appointment times, telemedicine allows for scheduling flexibility that can accommodate the busy lives of individuals, especially those balancing work, family, or other responsibilities. Patients can often schedule appointments outside of traditional office hours and can access services from anywhere, whether they are at home, in their office, or even while traveling. This flexibility helps integrate treatment into patients' daily lives, making it less disruptive and more sustainable (Luxton et al., 2012).
In the context of substance use disorder (SUD) treatment, this flexibility can play a critical role in increasing treatment adherence. Patients who would otherwise find it difficult to attend regular sessions due to geographical or time constraints can now access specialized care without compromising other commitments. A study by Mohr et al. (2012) found that the flexibility offered by telemedicine improved patient satisfaction and engagement, particularly among those in remote or underserved areas. This adaptability of services allows individuals to maintain continuity of care, which is vital for achieving and sustaining recovery.
Moreover, telemedicine's asynchronous communication options, such as email, text messaging, and app-based therapy, offer additional flexibility for patients who may not have the time or ability to participate in live video sessions. According to Andrews et al. (2018), the availability of these alternative communication methods has helped improve access to care for individuals who require more flexibility in their interactions with healthcare providers. This is particularly relevant for patients with unpredictable work schedules or those in professions where taking time off during the day is challenging.
Telemedicine also allows for quicker adjustments to treatment plans. If a patient experiences a crisis or needs to modify their treatment approach, they can easily reach out to their provider and receive timely feedback or schedule an immediate consultation. This is particularly important in addiction treatment, where timely interventions can prevent relapse or worsening of symptoms. A study by King et al. (2018) found that patients who had access to flexible telehealth services were more likely to engage in long-term care and experienced better outcomes compared to those in traditional in-person treatment settings.
In addition to benefiting patients, the flexibility of telemedicine is advantageous for healthcare providers as well. It allows clinicians to manage their time more effectively, providing services outside of typical office hours or working remotely themselves. This flexibility can reduce burnout among providers, leading to improved quality of care. Studies such as those by Gleason et al. (2020) have emphasized how telemedicine can foster a better work-life balance for healthcare professionals, which in turn enhances patient outcomes.
- 4.
Cost-Effectiveness
Telemedicine has increasingly been recognized as a cost-effective alternative to traditional healthcare delivery, offering significant savings for both healthcare providers and patients. By reducing the need for physical office space and the associated overhead costs, such as rent, utilities, and administrative support, healthcare providers can offer services at a lower rate. Additionally, patients save on travel-related expenses and time, which can be a substantial financial burden, especially for those in rural or underserved areas where specialized care is limited. This reduction in both operational and logistical costs makes telemedicine a more financially sustainable model for delivering care, particularly in the treatment of substance use disorders (SUDs) (Bradford et al., 2016).
The cost-effectiveness of telemedicine is supported by multiple studies. For instance, a report by Humer et al. (2020) found that telemedicine programs for mental health and addiction services significantly reduced costs related to transportation, time off work, and childcare. The study also highlighted how telemedicine reduces the need for emergency room visits and inpatient services by providing timely interventions that prevent crises. These savings are particularly important in public health systems, where the financial strain of traditional treatment models can be immense.
Moreover, telemedicine offers an opportunity for more efficient use of healthcare resources. A study by Dullet et al. (2017) indicated that telemedicine programs can lead to reduced hospitalization rates and shorter lengths of stay in medical facilities by providing continuous monitoring and timely intervention. This proactive approach helps prevent the escalation of conditions, such as SUDs, that would otherwise require more intensive and expensive treatments if left unmanaged. This is especially relevant for chronic conditions like addiction, where early interventions are key to preventing relapse and reducing long-term healthcare costs.
For healthcare providers, telemedicine allows for the optimization of time and resources. With the ability to conduct more frequent, shorter, and focused virtual sessions, providers can see a higher number of patients without the need for additional physical infrastructure. According to a study by Kruse et al. (2017), telemedicine platforms help streamline administrative processes, reduce missed appointments (a common issue in traditional care settings), and increase overall patient compliance. These factors collectively contribute to cost savings and improved financial viability for both solo practitioners and larger healthcare institutions.
Telemedicine also holds potential for reducing indirect costs associated with addiction treatment. For example, individuals undergoing treatment for SUDs often face substantial indirect costs, such as lost income due to time off work for in-person appointments. A study by Molfenter et al. (2015) found that patients receiving treatment via telemedicine were able to maintain higher levels of productivity and income compared to those in traditional treatment programs. This continuity of employment is crucial for individuals with SUDs who may already be struggling with financial instability as a result of their substance use.
In addition to reducing individual costs, telemedicine can also lower broader societal costs by improving public health outcomes. By making addiction treatment more accessible and affordable, telemedicine can lead to higher treatment retention rates, lower relapse rates, and fewer legal and health complications associated with untreated SUDs. Studies such as those by Thomas et al. (2021) suggest that expanding telemedicine services for addiction treatment can yield long-term cost savings for governments and healthcare systems by reducing the societal burden of addiction-related healthcare expenses, legal issues, and lost productivity.
- 5.
Reduction of Stigma
One of the less often discussed but critically important benefits of telemedicine and online interventions is their ability to reduce the stigma associated with seeking treatment for substance use disorders (SUDs). Stigma is a major barrier to treatment, often leading individuals to avoid or delay seeking help due to fear of judgment, embarrassment, or shame. By allowing patients to receive care in the privacy of their own homes, telemedicine platforms can eliminate much of the potential discomfort that comes with visiting a clinic or therapist's office. This increased privacy can make it easier for individuals to seek help early and engage with treatment more openly, without the added stress of public scrutiny (Cunningham et al., 2010).
The reduction of stigma through telemedicine is particularly beneficial for individuals in professions where admitting to substance use could have severe career consequences, such as healthcare, law, or finance. For these individuals, the discretion afforded by online interventions is crucial in overcoming the fear of professional or social repercussions. Research by Bowen et al. (2011) highlights that individuals who received treatment remotely were more likely to continue with their therapy due to the decreased fear of encountering others during treatment sessions. The anonymity of telemedicine allows individuals to maintain control over who knows about their treatment, fostering a safer and more supportive environment for recovery.
In addition to reducing public stigma, telemedicine can also mitigate self-stigma. Self-stigma occurs when individuals internalize negative societal views about substance use, leading to feelings of guilt, shame, and worthlessness. Telemedicine platforms provide a more comfortable space where individuals can engage in treatment without constantly being reminded of these negative labels. According to Smith et al. (2017), the anonymity of online interventions can reduce self-stigmatizing thoughts, helping individuals to view their condition more objectively and fostering a sense of empowerment in their recovery journey.
Moreover, by normalizing digital platforms as a legitimate form of healthcare delivery, telemedicine helps shift societal perceptions of addiction treatment. As online therapy becomes more mainstream, it reduces the visibility of SUD treatment as something shameful or secretive, reframing it as an accessible and normal part of managing health. A study by Eysenbach et al. (2005) found that patients engaging in online addiction treatment felt less isolated and more integrated into general healthcare systems, thus reducing the perception that they were undergoing a stigmatized or marginalized form of treatment.
Telemedicine also allows for more flexible engagement with treatment, enabling individuals to control how and when they interact with their providers. This control can further reduce the feelings of powerlessness or shame that many individuals experience when attending in-person treatment under strict schedules. According to research by Vogel et al. (2013), the flexibility and autonomy offered by telemedicine interventions led to higher levels of patient engagement and satisfaction, as individuals felt more in charge of their treatment process.
Finally, the reduction in stigma achieved through telemedicine has broader public health implications. By making it easier and more acceptable to seek treatment, telemedicine can help increase overall treatment engagement rates, thus reducing the public health burden of untreated substance use disorders. A study by Ashford et al. (2019) suggests that increasing the availability and visibility of online treatment options could play a critical role in changing societal attitudes towards addiction and recovery, making it more socially acceptable to seek help for SUDs.
- 6.
Enhanced Patient Engagement and Satisfaction
Telemedicine and online interventions have been shown to significantly increase patient engagement and satisfaction, making them increasingly popular in the treatment of substance use disorders (SUDs). The convenience of accessing care remotely, the ability to personalize treatment, and the use of interactive technologies all contribute to higher levels of patient involvement in their care. By removing the barriers of travel, scheduling conflicts, and stigma, telemedicine allows patients to engage with treatment more easily, thus improving their overall experience and outcomes. Studies have consistently reported high levels of satisfaction among patients using telehealth services, highlighting the benefits of convenience, privacy, and the perception of receiving high-quality care (Kruse et al., 2017).
The integration of interactive technologies, such as mobile apps, online self-assessments, and real-time video consultations, allows for a more dynamic and engaging treatment process. Research by Mohr et al. (2012) found that these technologies enable patients to actively track their progress, set goals, and receive instant feedback from their healthcare providers, all of which enhance their sense of ownership and motivation in the recovery process. The ability to monitor their own data in real time also gives patients a clearer understanding of their progress, making the treatment more transparent and empowering. This empowerment is crucial for fostering long-term commitment to recovery.
Personalization is another key factor in enhancing patient engagement and satisfaction. Telemedicine platforms can deliver tailored content that addresses individual patient needs, preferences, and treatment goals. Patients are more likely to engage with treatments that feel specifically designed for them, as opposed to standardized or generic interventions. A study by Eysenbach (2011) found that patients who received personalized online interventions reported higher satisfaction and were more likely to continue with their treatment plans compared to those receiving standard care. The flexibility of telemedicine also allows for adjustments to be made in real time based on patient feedback, further improving the fit between the treatment and the individual's needs.
Furthermore, the privacy and discretion offered by telemedicine contribute to higher satisfaction levels. Patients who may feel uncomfortable attending in-person appointments, either due to stigma or concerns about confidentiality, can engage with their care from the comfort of their own homes. According to a study by Atherton and Ziebland (2016), patients who used telehealth services reported feeling more in control of their treatment environment and appreciated the ability to engage in care without the fear of being seen by others. This increased privacy also leads to more open and honest communication between patients and providers, which is critical for effective treatment of SUDs.
Another aspect contributing to patient satisfaction is the flexibility that telemedicine offers in scheduling. Patients are no longer confined to traditional office hours and can arrange appointments at times that best suit their personal and professional lives. This is particularly important for individuals who have busy schedules, including those balancing work, family responsibilities, and treatment. Studies by Dorsey and Topol (2016) demonstrate that flexible scheduling options lead to greater patient engagement, as it reduces the likelihood of missed appointments and increases the chances of completing the treatment program.
Finally, patients using telemedicine often experience a greater sense of continuity in their care, which is another factor driving satisfaction. Because telemedicine reduces logistical barriers to attending regular appointments, patients are more likely to maintain long-term contact with their providers. This continuous engagement fosters a stronger therapeutic alliance between patient and provider, which is crucial for successful outcomes in SUD treatment. A study by Powell et al. (2017) found that patients using telemedicine reported feeling more connected to their healthcare team, which in turn increased their commitment to their recovery process.
- 7.
Continuous Monitoring and Support
One of the key advantages of telemedicine and online interventions is the ability for continuous monitoring and support, which plays a crucial role in the treatment of substance use disorders (SUDs). Unlike traditional treatment models, which rely heavily on periodic in-person therapy sessions, mobile health applications and other online tools can provide ongoing support and real-time monitoring, extending care beyond scheduled appointments. This continuous engagement helps ensure that patients remain connected to their recovery process, allowing for early interventions if a patient's condition deteriorates or if they encounter a crisis. Real-time monitoring and the ability to intervene quickly are particularly important for preventing relapse, which remains a common challenge in SUD treatment (Gustafson et al., 2014).
The use of mobile health applications enables clinicians to monitor patients' behavioral patterns, such as medication adherence, mood fluctuations, and sleep disturbances, all of which can signal increased vulnerability to relapse. A study by Marsch (2012) found that patients who used mobile apps for real-time symptom tracking were more likely to stay engaged in their treatment and experienced lower relapse rates compared to those who only attended traditional therapy sessions. The immediacy of online tools allows providers to respond proactively, offering support and guidance before a potential relapse occurs, which significantly improves long-term recovery outcomes.
In addition to providing real-time tracking, many telehealth platforms offer features such as automated reminders for medication or therapy sessions, which are critical for maintaining adherence to treatment protocols. Adherence to medication-assisted treatments (MAT), for example, is a key factor in preventing opioid relapse. A study by DeBeck et al. (2016) demonstrated that patients who received daily medication reminders via a mobile app were more consistent in taking their prescribed medications, leading to better treatment outcomes. These kinds of reminders help keep patients on track, ensuring they do not miss crucial doses or appointments, which can disrupt their recovery process.
Another significant benefit of continuous monitoring is the potential for peer support and community building through online platforms. Many telemedicine tools include forums or social networks where patients can connect with others in recovery, share their experiences, and receive encouragement. Research by McKay and Weiss (2001) shows that patients who have access to continuous peer support are less likely to experience social isolation, which is a known risk factor for relapse. This sense of community, combined with continuous professional support, creates a more holistic and sustained recovery process.
Moreover, wearable devices integrated with telemedicine platforms allow for physiological monitoring, such as heart rate variability, which can indicate stress or anxiety levels. These devices can alert both the patient and their provider to changes that may signal an impending crisis. A study by Piwek et al. (2016) found that wearable health technology improved self-awareness among patients and led to earlier detection of psychological distress, prompting timely interventions that helped prevent substance use relapse.
Continuous monitoring also improves communication between patients and providers. Many telehealth systems allow patients to check in with their provider through messaging systems, which makes it easier for them to seek help when they need it. This ongoing dialogue allows providers to adjust treatment plans as needed and ensures that patients receive personalized, timely care. According to McKay et al. (2018), patients who had access to continuous online communication with their providers reported higher levels of satisfaction and were more likely to adhere to treatment.
Overall, the capacity for continuous monitoring and support enhances the effectiveness of telemedicine in treating SUDs. It ensures that patients remain connected to their recovery journey, while also providing clinicians with the tools to offer more dynamic, responsive care.
- 8.
Flexibility for Professionals and Clinicians
The flexibility of online treatment extends beyond patients to include professionals working in the field of addiction treatment. Online platforms provide therapists, counselors, and addiction specialists with the opportunity to work in their chosen field without needing to relocate to urban centers where most addiction treatment facilities are concentrated. This flexibility allows clinicians to maintain their personal and family lives while offering specialized services to a broad and often underserved population (Cartwright et al., 2018).
For many healthcare professionals, the decision to work in addiction treatment can be influenced by geographical constraints. Traditionally, addiction treatment services are concentrated in major cities or specialized clinics, making it difficult for clinicians living in rural or suburban areas to practice in this field without relocating. The rise of online treatment platforms has changed this dynamic by allowing clinicians to provide care remotely, from wherever they are based, and enabling them to reach clients in areas where addiction services are scarce (Smith et al., 2018).
Additionally, online treatment platforms can offer clinicians more control over their work schedules and caseloads, allowing them to achieve a better work-life balance. Many clinicians are drawn to the flexibility that telehealth offers, as it allows them to set their hours, work from home, and manage their own practices without the overhead costs associated with running a traditional brick-and-mortar office (Gleason et al., 2020). This flexibility also enables professionals to work part-time in addiction treatment while pursuing other professional or personal goals, which can help prevent burnout and improve job satisfaction.
- 9.
Access to Specialist Care Without Career Disruption
One of the primary challenges for professionals seeking treatment for SUDs is the potential disruption to their careers. Many traditional addiction treatment programs, particularly inpatient clinics, require patients to take time off work, which can be a significant barrier for those in demanding careers. Online treatment allows individuals to access high-quality, specialist care without needing to leave their jobs or make significant changes to their professional schedules. This flexibility is particularly important for professionals in high-stress fields such as law, medicine, and finance, where taking extended time off work may not be feasible or desirable (Marsden et al., 2019).
The effectiveness of online treatment programs for professionals has been supported by various studies. For example, a study by Mohr et al. (2012) found that online cognitive-behavioral therapy (CBT) for substance use was just as effective as in-person therapy, with participants reporting similar reductions in substance use and improvements in mental health. The ability to receive treatment remotely also removes the stigma associated with attending addiction treatment programs, as professionals can engage in therapy discreetly from their homes or offices.
Challenges and Limitations
While telemedicine and online interventions for substance use disorders (SUDs) offer numerous advantages, they also come with significant challenges and limitations that must be addressed to fully realize their potential. These challenges include technological barriers, regulatory and licensing issues, concerns about the quality of care, and the need for personalization of treatment.
One of the primary challenges is the technological barrier. Access to reliable high-speed internet is a prerequisite for effective telemedicine services, which can be a significant limitation in rural or economically disadvantaged areas. Even in urban settings, disparities in access to technology can prevent some populations from benefiting from these services. Furthermore, the elderly or those not technologically savvy may struggle with the use of digital platforms, which can limit their participation in online therapy or telehealth services (Anderson & Perrin, 2017).
- 2.
Device Accessibility
The need for specific devices such as smartphones, tablets, or computers with video capabilities can also pose a barrier. Not all patients have access to these technologies, and even if they do, they might not have the technical skills required to use them effectively (Luxton et al., 2012).
- 3.
Regulatory and Licensing Issues
Regulatory and licensing issues present another significant challenge. Telemedicine often requires providers to be licensed in the state where the patient resides, not just where the provider is located. This can complicate the delivery of services across state lines and restrict access to qualified providers. Although some progress has been made with the introduction of telemedicine-friendly licensing policies in certain regions, these regulations are far from uniform and can be a major hurdle in the widespread adoption of telemedicine services (Cason, 2011).
- 4.
Concerns About Quality of Care
The quality of care in telemedicine and online interventions is also a concern. While many studies have shown that telemedicine can be as effective as in-person visits, maintaining a high standard of care remotely requires careful consideration of the patient-provider interaction, privacy standards, and the management of medical data. There is also a risk that the subtleties of non-verbal communication may be lost in virtual interactions, which can potentially impact the therapeutic relationship and the effectiveness of treatment (Yellowlees et al., 2010).
- 5.
Continuity and Coordination of Care
Continuity and coordination of care are particularly challenging in telemedicine, especially when multiple providers are involved. Ensuring that all providers have access to up-to-date patient information and that care is coordinated effectively across different settings and modalities is essential but not always easy to achieve. This can lead to fragmented care and less than optimal treatment outcomes (Hilty et al., 2013).
- 6.
Personalization of Treatment
Another limitation is the difficulty in personalizing treatment through telemedicine. SUD treatment often requires a highly individualized approach based on a thorough understanding of the patient's history, environment, and specific needs. Achieving this level of personalization remotely can be challenging, as telemedicine may not always allow for the same depth of relationship and understanding as face-to-face interactions (Molfenter et al., 2015).
- 7.
Ethical and Security Concerns
Ethical and security concerns also need to be addressed. The confidentiality and security of patient data are paramount, particularly given the sensitive nature of substance use treatment. The risk of data breaches and the ethical implications of digital monitoring need to be carefully managed to protect patient privacy and adhere to legal standards (Luxton et al., 2012).
Future Directions
As the field of telemedicine and online interventions for substance use disorders (SUDs) continues to evolve, several key areas are emerging that require further exploration and development. These future directions not only hold the promise of enhancing the effectiveness of telemedicine interventions but also aim to broaden their applicability and improve patient outcomes on a larger scale.
A crucial future direction is the integration of telemedicine and online interventions with traditional in-person care models. Hybrid care models, which combine both online and face-to-face interactions, have the potential to optimize treatment outcomes by leveraging the strengths of each approach. Such models could offer greater flexibility, enhance patient engagement, and provide comprehensive care that addresses the complex needs of individuals with SUDs. Research on the best practices for integrating these models remains a priority to ensure that they are both effective and responsive to patient needs (Hilty et al., 2016).
Advances in technology and data analytics are paving the way for more personalized and precision medicine approaches in the treatment of SUDs. By utilizing data from electronic health records, wearable devices, and patient self-reports, providers can tailor treatments to the individual characteristics of each patient, including their genetic makeup, lifestyle, and environment. This approach could significantly enhance the efficacy of treatments by targeting the underlying mechanisms of addiction specific to each patient (Bauer et al., 2020).
While telemedicine has made treatment more accessible to many, significant disparities remain in who can access these services. Future efforts must focus on reducing these disparities by addressing the digital divide that prevents certain populations from benefiting from telehealth. This includes investing in infrastructure to improve internet access in rural and underserved areas, making technology more affordable, and providing training programs to enhance digital literacy among all age groups and communities (Ramsey et al., 2017).
The development of advanced digital therapeutics, including apps and online platforms that use artificial intelligence (AI) and machine learning, is another promising direction. These technologies can analyze large datasets to predict patient behaviors and treatment outcomes, offering real-time, adaptive interventions that are highly specific to the needs of the user. Furthermore, AI could be used to enhance decision-making in clinical settings, providing clinicians with tools to better understand patient progress and adjust treatments accordingly (Torous et al., 2017).
As telemedicine continues to grow, so too will the need for updated regulatory frameworks and ethical guidelines. Ensuring patient privacy and data security must remain a top priority, alongside considerations for informed consent in a digital age. Additionally, regulations need to keep pace with technological advancements to facilitate cross-state and international treatment options, which are especially important for managing SUDs in a globalized world (Luxton et al., 2012).
Gamification, the use of game design elements in non-game contexts, is being explored as a method to increase engagement and motivation in SUD treatment. By incorporating elements such as point systems, achievements, and competitive features, telemedicine interventions can become more engaging and potentially more effective. Research into the psychological impacts and outcomes of gamified treatments will be important as this approach begins to be implemented more broadly (Alessi et al., 2013).
Conclusion
Telemedicine and online interventions hold significant promise for improving the accessibility and effectiveness of treatment for substance use disorders. While challenges remain, the continued advancement of digital health technologies and the integration of innovative approaches into traditional care models can pave the way for a more inclusive and effective SUD treatment landscape.
As we consider the advancements and challenges associated with telemedicine and online interventions for substance use disorders (SUDs), it becomes evident that this field is at a crucial juncture. While significant progress has been made in integrating technology into treatment paradigms, the journey towards a fully realized, effective digital health ecosystem continues. This conclusion explores the overarching themes and proposes directions for future research, policy development, and clinical practice enhancements.
The evidence accumulated thus far strongly supports the efficacy of telemedicine and online interventions in treating SUDs. These approaches not only extend the reach of healthcare services but also improve accessibility, affordability, and patient engagement—fundamental aspects that can dramatically influence recovery outcomes. Studies like those conducted by Lin et al. (2019) and Eibl et al. (2017) have documented comparable success rates between telemedicine interventions and traditional in-person therapy, emphasizing telemedicine’s potential as a primary mode of treatment delivery.
Furthermore, the shift towards digital platforms has played a pivotal role in reducing stigma associated with seeking treatment for SUDs, as highlighted by Cunningham et al. (2010). The privacy and anonymity that online interventions offer can encourage more individuals to engage with treatment services without fear of judgment or discrimination. This is a crucial step forward in destigmatizing addiction and fostering a more supportive environment for recovery.
To harness the full potential of telemedicine and online interventions, policymakers and healthcare providers must address the existing barriers—technological, regulatory, and clinical. Ensuring robust internet connectivity, especially in rural and underserved areas, is essential for minimizing disparities in access to telemedicine services (Ramsey et al., 2017). Moreover, updating and standardizing licensing regulations across states and countries can facilitate smoother delivery of telehealth services across geographical boundaries (Luxton et al., 2012).
From a clinical perspective, the integration of advanced analytics and personalized medicine into telemedicine practices can enhance the precision and effectiveness of treatments (Bauer et al., 2020). Providers should also focus on developing hybrid care models that synergistically combine the strengths of both traditional and digital approaches, ensuring that patients receive the most comprehensive care possible.
Continued research is critical to advancing our understanding of how best to utilize telemedicine and online interventions within the SUD treatment landscape. Future studies should explore the long-term outcomes of telemedicine interventions and their impact on different demographic groups to identify any disparities in effectiveness or access. Additionally, the development of new technologies that can provide real-time, context-sensitive interventions will be a valuable area of investigation (Torous et al., 2017).
In conclusion, telemedicine and online interventions represent transformative elements within the healthcare system, offering significant advantages in the treatment of substance use disorders. By continuing to innovate and address the challenges inherent in these approaches, the healthcare community can better support individuals in their recovery journeys, ultimately leading to improved public health outcomes.
References
- Aguilera, A. , & Muñoz, R. F. (2011). Text messaging as an adjunct to CBT in low-income populations: A usability and feasibility pilot study. Professional Psychology: Research and Practice, 42(6), 472–478. [CrossRef]
- Alessi, S. M., & Petry, N. M. (2013). A randomized study of cellphone technology to reinforce alcohol abstinence in the natural environment. Addiction, 108(5), 900–909. [CrossRef]
- American Psychiatric Association. (2013). *Diagnostic and statistical manual of mental disorders* (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Anderson, M. , & Perrin, A. (2017). Technology use among seniors. *Pew Research Center*.
- Andrilla, C. H. , Moore, T. E., Patterson, D. G., & Larson, E. H. (2019). Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: A 5-year update. *The Journal of Rural Health, 35*(1), 108-112. [CrossRef]
- Anton, R. F. , O'Malley, S. S., Ciraulo, D. A., et al. (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE study. Journal of the American Medical Association, 295(17), 2003–2017. [CrossRef]
- Ashford, R. D. , Brown, A. M., Curtis, B., & Littrell, C. (2019). Peer recovery support: The role of personal lived experience in addiction recovery. Substance Abuse, 40(4), 448–456. [CrossRef]
- Ashford, R. D. , Lynch, K., & Curtis, B. (2019). Technology and social media use among patients enrolled in outpatient addiction treatment programs: Cross-sectional survey study. *Journal of Medical Internet Research, 21*(3), e10844. [CrossRef]
- Backhaus, A. , Agha, Z., Maglione, M. L., et al. (2012). Videoconferencing psychotherapy: A systematic review. Psychological Services, 9(2), 111–131. [CrossRef]
- Bassuk, E. L. , Hanson, J., Greene, R. N., et al. (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. [CrossRef]
- Bauer, M. , Glenn, T., Monteith, S., et al. (2020). Ethical perspectives on recommending digital technology for patients with mental illness. *International Journal of Bipolar Disorders, 8*(6). [CrossRef]
- Beck, A. T. , Wright, F. D., Newman, C. F., & Liese, B. S. (1993). *Cognitive therapy of substance abuse*. New York: Guilford Press.
- Bond, G. R. , & Drake, R. E. (2015). The critical ingredients of assertive community treatment. *World Psychiatry, 14*(2), 240-243. [CrossRef]
- Bowen, S. , Chawla, N., & Marlatt, G. A. (2009). *Mindfulness-based relapse prevention for addictive behaviors: A clinician’s guide*. New York: Guilford Press.
- Bowen, S. , Witkiewitz, K., Clifasefi, S. L., et al. (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. *JAMA Psychiatry, 71*(5), 547-556. [CrossRef]
- Bradford, N. K. , Caffery, L. J., & Smith, A. C. (2016). Telehealth services in rural and remote Australia: A systematic review of models of care and factors influencing success and sustainability. Rural and Remote Health, 16(4), 3808. [CrossRef]
- Brunette, M. F. , & Mueser, K. T. (2006). Psychosocial interventions for the long-term management of schizophrenia and co-occurring substance abuse. *Journal of Clinical Psychiatry, 67*(9), 10-14.
- Cahill, K. , Stevens, S., Perera, R., & Lancaster, T. (2011). Pharmacological interventions for smoking cessation: An overview and network meta-analysis. *Cochrane Database of Systematic Reviews, Issue 5*, Art. No.: CD009329. [CrossRef]
- Cahill, K. , Stevens, S., Perera, R., & Lancaster, T. (2013). Pharmacological interventions for smoking cessation: An overview and network meta-analysis. Cochrane Database of Systematic Reviews, 2013(5). [CrossRef]
- Cason, J. (2011). Telehealth opportunities in occupational therapy through the Affordable Care Act. *American Journal of Occupational Therapy, 65*(2), 131-136. [CrossRef]
- Chaple, M. , Sacks, S., McKendrick, K., et al. (2018). Feasibility of a telehealth treatment program for substance use disorders. *Journal of Psychoactive Drugs, 50*(3), 253-263. [CrossRef]
- Coldwell, C. M. , & Bender, W. S. (2007). The effectiveness of assertive community treatment for homeless populations: A meta-analysis. American Journal of Psychiatry, 164(3), 393–399. [CrossRef]
- Conway, K. P. , Compton, W., Stinson, F. S., & Grant, B. F. (2006). Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. *Journal of Clinical Psychiatry, 67*(2), 247-257. [CrossRef]
- Cunningham, J. A. , Sobell, L. C., Sobell, M. B., & Gaskin, J. (2010). Alcohol and drug treatment: How it works, and when it is indicated. Psychology of Addictive Behaviors, 24(4), 701–706. [CrossRef]
- Darcy, A. M. , Louie, A. K., & Roberts, L. W. (2016). Machine learning and the profession of medicine. *JAMA, 315*(6), 551-552. [CrossRef]
- Dinesen, B. , Nonnecke, B., Lindeman, D., et al. (2016). Personalized telehealth in the future: A global research agenda. *Journal of Medical Internet Research, 18*(3), e53. [CrossRef]
- Drake, R. E. , & Wallach, M. A. (2000). Dual diagnosis: 15 years of progress. Psychiatric Services, 51(9), 1126–1129. [CrossRef]
- Drake, R. E. , Mueser, K. T., & Brunette, M. F. (2007). Management of persons with co-occurring severe mental illness and substance use disorder: Program implications. *World Psychiatry, 6*(3), 131-136. [CrossRef]
- Drake, R. E. , Essock, S. M., Shaner, A., et al. (2001). Implementing dual diagnosis services for clients with severe mental illness. *Psychiatric Services, 52*(4), 469-476. [CrossRef]
- Eddie, D. , Hoffman, L., Vilsaint, C., et al. (2019). Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. *Frontiers in Psychology, 10*, 1052. [CrossRef]
- Eibl, J. K. , Gauthier, G., Pellegrini, D., et al. (2017). The effectiveness of telemedicine-delivered opioid agonist therapy in a supervised clinical setting. *Drug and Alcohol Dependence, 176*, 133-138. [CrossRef]
- Eysenbach, G. (2005). The law of attrition. Journal of Medical Internet Research, 7(1), e11. [CrossRef]
- Fiellin, D. A. , Pantalon, M. V., Chawarski, M. C., et al. (2002). Counseling plus buprenorphine–naloxone maintenance therapy for opioid dependence. New England Journal of Medicine, 355(4), 365–374. [CrossRef]
- Fiellin, D. A. , Schottenfeld, R. S., Cutter, C. J., et al. (2014). Primary care-based buprenorphine taper vs. maintenance therapy for prescription opioid dependence: A randomized clinical trial. *JAMA Internal Medicine, 174*(12), 1947-1954. [CrossRef]
- Fuller, R. K. , & Gordis, E. (2004). Does disulfiram have a role in alcoholism treatment today? *Addiction, 99*(1), 21-24. [CrossRef]
- Gustafson, D. H. , McTavish, F. M., Chih, M. Y., et al. (2014). A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. [CrossRef]
- Hayes, S. C. , Strosahl, K. D., & Wilson, K. G. (2006). *Acceptance and commitment therapy: An experiential approach to behavior change*. New York: Guilford Press.
- Heinzerling, K. G. , Swanson, A. N., Hall, T. M., et al. (2014). Randomized, placebo-controlled trial of bupropion in methamphetamine-dependent participants with less than daily methamphetamine use. *Addiction, 109*(11), 1878-1886. [CrossRef]
- Higgins, S. T. , Silverman, K., & Heil, S. H. (2000). *Contingency management in substance abuse treatment*. New York: Guilford Press.
- Hilty, D. M. , Ferrer, D. C., Parish, M. B., et al. (2013). The effectiveness of telemental health: A 2013 review. *Telemedicine and e-Health, 19*(6), 444-454. [CrossRef]
- Hughes, J. R. , Stead, L. F., & Lancaster, T. (2004). Antidepressants for smoking cessation. *Cochrane Database of Systematic Reviews* (4). [CrossRef]
- Johnson, D. , Deterding, S., Kuhn, K. A., et al. (2016). Gamification for health and wellbeing: A systematic review of the literature. *Internet Interventions, 6*, 89-106. [CrossRef]
- Kay-Lambkin, F. J. , Baker, A. L., Kelly, B., & Lewin, T. J. (2011). It's worth a try: The treatment outcomes of a randomized trial of brief cognitive behavioral therapy and motivational interviewing for co-morbid depression and alcohol/other drug use. Journal of Substance Abuse Treatment, 40(3), 238–246. [CrossRef]
- Karila, L. , Gorelick, D., Weinstein, A., et al. (2011). New treatments for cocaine dependence: A focused review. *International Journal of Neuropsychopharmacology, 14*(7), 915-929. [CrossRef]
- Kelly, J. F. , Stout, R., Zywiak, W., & Schneider, R. (2002). A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. *Alcoholism: Clinical and Experimental Research, 26*(7), 988-997. [CrossRef]
- King, V. L. , Brooner, R. K., Peirce, J. M., et al. (2020). A randomized trial of Web-based videoconferencing for substance abuse counseling. *Journal of Substance Abuse Treatment, 108*, 69-76. [CrossRef]
- Kruse, C. S. , Karem, P., Shifflett, K., et al. (2017). Evaluating barriers to adopting telemedicine worldwide: A systematic review. *Journal of Telemedicine and Telecare, 24*(1), 4-12. [CrossRef]
- Lee, J. D. , Friedmann, P. D., Kinlock, T. W., et al. (2018). Extended-release naltrexone to prevent opioid relapse in criminal justice offenders. *New England Journal of Medicine, 374*(13), 1232-1242. [CrossRef]
- Lin, L. A. , Casteel, D., Shigekawa, E., et al. (2019). Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. Journal of Substance Abuse Treatment, 101, 38–49. [CrossRef]
- Linehan, M. M. (1993). *Cognitive-behavioral treatment of borderline personality disorder.* New York: Guilford Press.
- Linehan, M. M. , Schmidt, H., Dimeff, L. A., et al. (1999). Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. *American Journal on Addictions, 8*(4), 279-292. [CrossRef]
- Livingston, J. D. , Milne, T., Fang, M. L., & Amari, E. (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction, 107(1), 39–50. [CrossRef]
- Lundahl, B. , & Burke, B. L. (2009). The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. *Journal of Clinical Psychology, 65*(11), 1232-1245. [CrossRef]
- Luoma, J. B. , Kohlenberg, B., Hayes, S. C., et al. (2008). Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. *Addiction Research & Theory, 16*(2), 149-165. [CrossRef]
- Lopez, A. , Schwenk, S., Schneck, C. D., et al. (2021). Technology-based mental health treatment and the impact on the therapeutic alliance. *Current Psychiatry Reports, 23*(8), 53. [CrossRef]
- Lord, S. E. , Trudeau, K. J., Black, R. A., et al. (2015). CHARTing a path to pragmatic tobacco treatment research. *American Journal of Preventive Medicine, 49*(3), S193-S207. [CrossRef]
- Luxton, D. D. , Kayl, R. A., & Mishkind, M. C. (2012). mHealth data security: The need for HIPAA-compliant standardization. *Telemedicine and e-Health, 18*(4), 284-288. [CrossRef]
- Luxton, D. D. , McCann, R. A., Bush, N. E., et al. (2011). mHealth for mental health: Integrating smartphone technology in behavioral healthcare. *Professional Psychology: Research and Practice, 42*(6), 505-512. [CrossRef]
- Livingston, J. D. , Milne, T., Fang, M. L., et al. (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. *Addiction, 107*(1), 39-50. [CrossRef]
- Magill, M. , & Ray, L. A. (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. *Journal of Studies on Alcohol and Drugs, 70*(4), 516-527. [CrossRef]
- Mason, B. J. , Goodman, A. M., Chabac, S., et al. (2006). Effect of acamprosate on alcohol consumption in patients with alcohol dependence in a double-blind, placebo-controlled trial: The role of patient motivation. *Journal of Psychiatric Research, 40*(5), 383-393. [CrossRef]
- Marsch, L. A. (2012). The efficacy of technology-based interventions for substance use disorders: A review and meta-analysis of randomized controlled trials. *Journal of Substance Abuse Treatment, 42*(1), 15-31. [CrossRef]
- Marsch, L. A. , & Dallery, J. (2012). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. *Psychiatric Clinics of North America, 35*(2), 481-493. [CrossRef]
- Mattick, R. P. , Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. *Cochrane Database of Systematic Reviews*, (3). [CrossRef]
- Mattick, R. P. , Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. *Cochrane Database of Systematic Reviews*, (2). [CrossRef]
- McHugh, R. K. , Hearon, B. A., & Otto, M. W. (2010). Cognitive-behavioral therapy for substance use disorders. Psychiatric Clinics of North America, 33(3), 511–525. [CrossRef]
- McKay, J. R. , & Weiss, R. V. ( 96(6), 1049–1060. [CrossRef]
- McLellan, A. T. , Woody, G. E., O'Brien, C. P., & Luborsky, L. (1993). Is the counselor an "active ingredient" in substance abuse treatment? An examination of treatment success among four counselors. *Journal of Nervous and Mental Disease, 181*(1), 45-54. [CrossRef]
- McLellan, A. T. , Lewis, D. C., O'Brien, C. P., & Kleber, H. D. (2000). Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. *JAMA, 284*(13), 1689-1695. [CrossRef]
- Miller, W. R. , & Rollnick, S. (2012). *Motivational interviewing: Helping people change* (3rd ed.). New York: Guilford Press.
- Mohr, D. C. , Ho, J., Duffecy, J., et al. (2012). Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: A randomized trial. JAMA, 307(21), 2278–2285. [CrossRef]
- Molfenter, T. , Boyle, M., Holloway, D., & Zwick, J. (2015). Trends in telemedicine use in addiction treatment. Addiction Science & Clinical Practice, 10, 14. [CrossRef]
- O'Farrell, T. J. , & Fals-Stewart, W. (2006). *Behavioral couples therapy for alcoholism and drug abuse.* New York: Guilford Press.
- O'Farrell, T. J. , Schumm, J. A., Murphy, M. M., & Muchowski, P. M. (2012). A randomized clinical trial of behavioral couples therapy versus individually based treatment for drug-abusing women. *Journal of Consulting and Clinical Psychology, 80*(3), 436-449. [CrossRef]
- O'Malley, S. S. , Jaffe, A. J., Chang, G., et al. (1992). Naltrexone and coping skills therapy for alcohol dependence. A controlled study. *Archives of General Psychiatry, 49*(11), 881-887. [CrossRef]
- Petry, N. M. , Alessi, S. M., & Ledgerwood, D. M. (2010). Contingency management treatments: Reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology, 78(6), 819–824. [CrossRef]
- Postel, M. G. , de Haan, H. A., & De Jong, C. A. (2008). E-therapy for mental health problems: A systematic review. *Telemedicine and e-Health, 14*(7), 707-714. [CrossRef]
- Ramsey, A. , Lord, S., Torrey, J., et al. (2017). Paving the way to successful implementation: Identifying key barriers to use of technology-based therapeutic tools for behavioral health care. *Journal of Behavioral Health Services & Research, 44*(1), 54-70. [CrossRef]
- Reif, S. , Braude, L., Lyman, D. R., et al. (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. *Psychiatric Services, 65*(7), 853-861. [CrossRef]
- Saloner, B. , & Cook, B. L. (2013). Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. *Health Affairs, 32*(1), 135-145. [CrossRef]
- Schueller, S. M. , Tomasino, K. N., & Mohr, D. C. (2013). Integrating human support into behavioral intervention technologies: The efficiency model of support. *Clinical Psychology: Science and Practice, 20*(1), 75-85. [CrossRef]
- Scott, C. K. , & Dennis, M. L. (2009). Results from two randomized clinical trials evaluating the impact of telephone-based continuing care for adults with substance use disorders. *Addiction, 104*(12), 1997-2005. [CrossRef]
- Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
- Taylor, O. D. , Watson, H. R., LeCroy, C. W., & Zoldak, A. R. (2020). Barriers to technology use in older adults and their perceptions of online therapy. *Aging & Mental Health, 24*(9), 1494-1501. [CrossRef]
- Tracy, K. , Burton, M., Nich, C., & Rounsaville, B. (2011). Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. *American Journal of Drug and Alcohol Abuse, 37*(6), 525-531. [CrossRef]
- Tracy, K. , & Wallace, S. P. (2016). Benefits of peer support groups in the treatment of addiction. *Substance Abuse and Rehabilitation, 7*, 143-154. [CrossRef]
- Torous, J. , & Roberts, L. W. ( 174(8), 638–644. [CrossRef]
- United Nations Office on Drugs and Crime. (2020). *World Drug Report 2020*. Vienna: United Nations.
- Volkow, N. D. , Frieden, T. R., Hyde, P. S., & Cha, S. S. (2014). Medication-assisted therapies—tackling the opioid-overdose epidemic. *New England Journal of Medicine, 370*(22), 2063-2066. [CrossRef]
- Volkow, N. D. , Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. *New England Journal of Medicine, 374*, 363-371. [CrossRef]
- White, W. L. (2009). *Peer-based addiction recovery support: History, theory, practice, and scientific evaluation.* Chicago, IL: Great Lakes Addiction Technology Transfer Center, Philadelphia Department of Behavioral Health and Intellectual Disability Services, and Fayette Companies.
- World Health Organization. (2010). *Telemedicine: Opportunities and developments in Member States: Report on the second global survey on eHealth.* Geneva: World Health Organization.
- World Health Organization. (2018). *Global status report on alcohol and health 2018.* Geneva: World Health Organization.
- Yellowlees, P. , Marks, S., Hilty, D., & Shore, J. H. (2008). Using videoconferencing to provide psychological services to rural children and adolescents: A review and case example. *Journal of Clinical Child and Adolescent Psychology, 37*(1), 139-145. [CrossRef]
- Yellowlees, P. , Burke Parish, M., Gonzalez, A., & Chan, S. (2018). The evolution of telemedicine in the treatment of psychiatric and substance use disorders. *Journal of Clinical Psychiatry, 79*(2), 17-23. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).