Submitted:
19 February 2025
Posted:
20 February 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Participants and Procedures
2.3. Measures
2.3.1. Past-Year Receipt of Substance Use Treatment
2.3.2. Substance Use Treatment-Seeking vs. not Seeking
2.3.3. Past-Year SUD
2.3.4. SUD Severity
2.3.5. Problem self-Perception
2.3.6. Past-Year Mental Illness Severity and Mental Health Treatment Use
2.3.7. Predisposing Factors
2.3.8. Enabling Factors
2.4. Analysis
3. Results
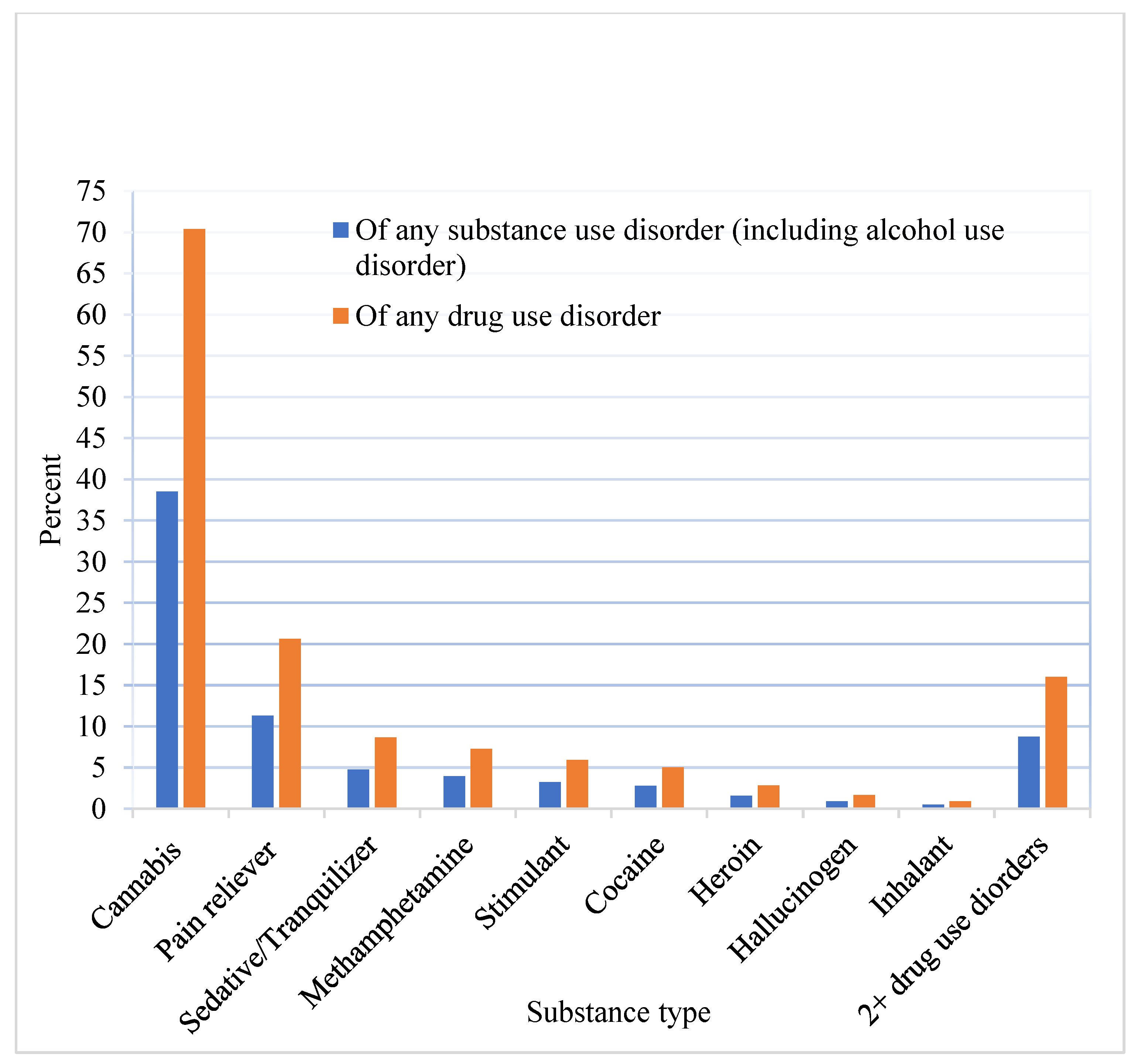
3.1. Prevalence of Past-Year SUD and Treatment Receipt
3.2. Characteristics of SUD Treatment Users and Non-Users
3.3. Treatment Non-Users: Comparison between Treatment Seekers and Non-Seekers
3.4. Associations of Treatment Use with SUD Symptom Severity, Problem Self-Perception, Comorbid Mental Illness, and Mental Health Treatment
3.5. Correlates of Treatment-Seeking Among Treatment Non-Users
3.6. Personal and Environmental/Structural Reasons for Treatment Non-Use Among Treatment Seekers
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association, Washington, DC, USA. 2013. [CrossRef]
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2023 National Survey on Drug Use and Health (HHS Publication No. PEP24-07-021, NSDUH Series H-59). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 2024. https://www.samhsa.gov/data/report/2023-nsduh-annual-national-report (accessed on October 20, 2024).
- Garnett, M. F.; Miniño, A. M. Drug overdose deaths in the United States, 2003–2023. NCHS Data Brief, no 522. Hyattsville, MD: National Center for Health Statistics. 2024. [CrossRef]
- Spencer, M. R.; Garnett, M. F.; Miniño, A. M. Drug overdose deaths in the United States, 2002-2022. NCHS Data Brief, no 491. Hyattsville, MD: National Center for Health Statistics. 2024. [CrossRef]
- Bastos Maia, M.; Martins, P. M.; Figueiredo-Braga, M. Outcomes and challenges of motivational interviewing in dual diagnosis treatment - A systematic review. J. Dual Diagn. 2025, 21(1), 56–69. [Google Scholar] [CrossRef] [PubMed]
- Kline-Simon, A. H.; Palzes, V. A.; Chi, F. W.; Satre, D. D.; Weisner, C.; Sterling, S. A. Was receipt of any specialty alcohol treatment during the pandemic effective at reducing drinking for patients with or at risk of AUD? J. Subst. Use Addict. Treat. 2025, 168, 209531. [Google Scholar] [CrossRef] [PubMed]
- Mateu-Mollá, J. , Pérez-Gálvez, B., & Villanueva-Blasco, V. J. Pharmacological treatment for substance use disorder: A systematic review. Addict. Behav. 2025, 163, 108242 . [Google Scholar] [CrossRef]
- Morse, A. K.; Askovic, M.; Sercombe, J.; Dean, K.; Fisher, A.; Marel, C.; Chatterton, M. L.; Kay-Lambkin, F.; Barrett, E.; Sunderland, M.; Harvey, L.; Peach, N.; Teesson, M.; Mills, K. L. A systematic review of the efficacy, effectiveness and cost-effectiveness of workplace-based interventions for the prevention and treatment of problematic substance use. Front. Public Health. 2022, 10, 1051119. [Google Scholar] [CrossRef] [PubMed]
- Morse, A. K.; Sercombe, J.; Askovic, M.; Fisher, A.; Marel, C.; Chatterton, M. L.; Kay-Lambkin, F.; Barrett, E.; Sunderland, M.; Harvey, L.; Peach, N.; Teesson, M.; Mills, K. L. Systematic review of the efficacy, effectiveness, and cost-effectiveness of stepped-care interventions for the prevention and treatment of problematic substance use. J. Subst. Abuse Treat. 2023, 144, 108928. [Google Scholar] [CrossRef]
- O'Leary, C.; Ralphs, R.; Stevenson, J.; Smith, A.; Harrison, J.; Kiss, Z.; Armitage, H. The effectiveness of abstinence-based and harm reduction-based interventions in reducing problematic substance use in adults who are experiencing homelessness in high-income countries: A systematic review and meta-analysis: A systematic review. Campbell Syst. Rev. 2024, 20(2), e1396. [Google Scholar] [CrossRef]
- Choi, N. G.; DiNitto, D. M.; Marti, C. N. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014, 145, 113–120. [Google Scholar] [CrossRef]
- Edmonds, A. T.; Bensley, K. M.; Hawkins, E. J.; Williams, E. C. Geographic differences in receipt of addictions treatment in a national sample of patients with alcohol use disorders from the U.S. Veterans Health Administration. S. Veterans Health Administration. Subst. Abus. 2021, 42(4), 559–568. [Google Scholar] [CrossRef]
- Dhinsa, J.; Roman-Urrestarazu, A.; van Kessel, R.; Humphreys, K. Understanding predictors of mental health and substance use treatment utilization among US adults: A repeated cross-sectional study. Glob. Epidemiol. 2023, 5, 100109.1. [CrossRef]
- Han, B.; Compton, W. M.; Blanco, C.; Colpe, L. J. Prevalence, treatment, and unmet treatment needs Of US adults with mental health and substance use disorders. Health Aff. (Millwood), 2017, 36(10), 1739–1747. [CrossRef]
- Lin, L. A.; Bohnert, A. S. B.; Blow, F. C.; Gordon, A. J.; Ignacio, R. V.; Kim, H. M.; Ilgen, M. A. Polysubstance use and association with opioid use disorder treatment in the US Veterans Health Administration. Addiction (Abingdon, England), 2021, 116(1), 96–104. [CrossRef]
- Park-Lee, E.; Lipari, R. N.; Hedden, S. L.; Kroutil, L. A.; Porter, J. D. Receipt of services for substance use and mental health issues among adults: Results from the 2016 National Survey on Drug Use and Health. In CBHSQ Data Review. (pp. 1–35). Substance Abuse and Mental Health Services Administration (US). 2017.
- Priester, M. A.; Browne, T.; Iachini, A.; Clone, S.; DeHart, D.; Seay, K. D. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: An integrative literature review. J. Subst. Abuse Treat. 2016, 61, 47–59. [Google Scholar] [CrossRef]
- Romo, E.; Ulbricht, C. M.; Clark, R. E.; Lapane, K. L. Correlates of specialty substance use treatment among adults with opioid use disorders. Addict. Behav. 2018, 86, 96–103. [Google Scholar] [CrossRef]
- Bhondoekhan, F.; Li, Y.; Hallowell, B. D.; Mahoney, L.; Daly, M. M.; Goulet, J.; Beaudoin, F. L.; Chambers, L. C.; Marshall, B. D. L. Engagement in substance use disorder treatment after an emergency department visit among persons at high risk of opioid overdose: A prediction analysis. Drug Alcohol Depend. Rep. 2024, 13, 100287. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.; Meurk, C.; Sara, G. E.; Heffernan, E. Comprehensive care processes for substance use disorders in adult mental health services: A systematic review. Aust N Z J Psychiatry. 2025, 48674241312790. [CrossRef]
- Choi, N. G.; DiNitto, D. M. Characteristics of mental health and substance use service facilities for older adults: Findings from U.S. national surveys. Clin. Gerontol. 2022, 45(2), 338–350. [CrossRef]
- Choi, N. G.; DiNitto, D. M. Older marijuana users in substance abuse treatment: Treatment settings for marijuana-only versus polysubstance use admissions. J. Subst. Abuse Treat. 2019, 105, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J. F.; Hourani, L. L.; Heller, D. C. Predictors of treatment receipt among adults with a drug use disorder. Am. J. Drug Alcohol Abuse, 2004, 30(4), 841–869. [CrossRef]
- Fry, C. E.; Harris, J.; Burns, M. E. Changes in legal referrals to specialty substance use disorder treatment from 2015-2019. Health Justice, 2024, 12(1), 42. [CrossRef]
- Johnson, K.; Rigg, K. K.; Hopkins Eyles, C. Receiving addiction treatment in the US: Do patient demographics, drug of choice, or substance use disorder severity matter? Int. J. Drug Policy. 2020, 75, 102583. [Google Scholar] [CrossRef]
- Pasman, E.; Blair, L.; Solberg, M. A.; McCabe, S. E.; Schepis, T.; Resko, S. M. The substance use disorder treatment gap among US college students: Findings from the 2021 National Survey on Drug Use and Health. Drug Alcohol Depend. Rep. 2024, 12, 100279. [Google Scholar] [CrossRef]
- Choi, N. G.; Moore, J.; Choi, B. Y. Cannabis use disorder and substance use treatment among U.S. adults. J. Subst. Use Addict. Treat. 2024, 167, 209486. [Google Scholar] [CrossRef]
- Andersen, R. M. Revisiting the behavioral model and access to medical care: does it matter? J. Health Social Behav. 1995, 36(1), 1–10. [Google Scholar] [CrossRef]
- Andersen, R. M. National health surveys and the behavioral model of health services use. Med. Care. 2008, 46(7), 647–653. [Google Scholar] [CrossRef]
- Babitsch, B.; Gohl, D.; von Lengerke, T. Re-revisiting Andersen's Behavioral Model of Health Services Use: A systematic review of studies from 1998-2011. Psychosoc. Med. 2012, 9, Doc11. [Google Scholar] [CrossRef]
- Graham, A.; Hasking, P.; Brooker, J.; Clarke, D.; Meadows, G. Mental health service use among those with depression: An exploration using Andersen’s behavioral model of health service use. J. Affect. Disord. 2017, 208, 170–176. [Google Scholar] [CrossRef]
- Ober, A. J.; Watkins, K. E.; McCullough, C. M.; Setodji, C. M.; Osilla, K.; Hunter, S. B. Patient predictors of substance use disorder treatment initiation in primary care. J. Subst. Abuse Treat. 2018, 90, 64–72. [Google Scholar] [CrossRef]
- Denis, C. M.; Gelernter, J.; Hart, A. B.; Kranzler, H. R. Inter-observer reliability of DSM-5 substance use disorders. Drug Alcohol Depend. 2015, 153, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.; Shmulewitz, D.; Stohl, M.; Greenstein, E.; Roncone, S.; Aharonovich, E.; Wall, M. Test-retest reliability of DSM-5 substance disorder measures as assessed with the PRISM-5, a clinician-administered diagnostic interview. Drug Alcohol Depend. 2020, 216, 108294. [Google Scholar] [CrossRef] [PubMed]
- Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 2023. https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report.
- 2023 National Survey on Drug Use and Health (NSDUH): Methodological Summary and Definitions. Substance Abuse and Mental Health Services Administration. 2024. https://www.samhsa.gov/data/report/2023-methodological-summary-and-definitions.
- How can you safely ignore multicollinearity? 2012. https://statisticalhorizons.com/multicollinearity/ (accessed on October 1, 2024).
- Ignaszewski, M. J. The epidemiology of drug abuse. J. Clin. Pharmacol. 2021, 61 Suppl 2, S10–S17. [Google Scholar] [CrossRef]
- Straussner, S. L. A.; Fewell, C. H. A review of recent literature on the impact of parental substance use disorders on children and the provision of effective services. Curr. Opin. Psychiatry. 2018, 31(4), 363–367. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D. S.; O’Brien, C. P.; Auriacombe, M.; Borges, G.; Bucholz, K.; Budney, A.; Compton, W. M.; Crowley, T.; Ling, W.; Petry, N. M.; Schuckit, M.; Grant, B. F. DSM-5 criteria for substance use disorders: recommendations and rationale. Am. J. Psychiatry 2013, 170, 834–851. [Google Scholar] [CrossRef]
- Moore, K. E.; Oberleitner, L.; Pittman, B. P.; Roberts, W.; Verplaetse, T. L.; Hacker, R. L.; Peltier, M. R.; McKee, S. A. The prevalence of substance use disorders among community-based adults with legal problems in the U.S. Addict. Res. Theory. 2020, 28(2), 165–172. [Google Scholar] [CrossRef]
- Moeller, S. J.; Goldstein, R. Z. Impaired self-awareness in human addiction: deficient attribution of personal relevance. Trends Cogn. Sci 2014, 18, 635–641. [Google Scholar] [CrossRef]
- Moeller, S. J.; Kundu, P.; Bachi, K.; Maloney, T.; Malaker, P.; Parvaz, M. A.; Alia-Klein, N.; London, E. D.; Goldstein, R. Z. Self-awareness of problematic drug use: Preliminary validation of a new fMRI task to assess underlying neurocircuitry. Drug Alcohol Depend. 2020, 209, 107930. [Google Scholar] [CrossRef]
- Lindgren, K. P.; Neighbors, C.; Gasser, M. L.; Ramirez, J. J.; Cvencek, D. A review of implicit and explicit substance self-concept as a predictor of alcohol and tobacco use and misuse. Am. J. Drug Alcohol Abuse. 2017, 43(3), 237–246. [Google Scholar] [CrossRef]
- Bonnet, U.; Specka, M.; Soyka, M.; Alberti, T.; Bender, S.; Grigoleit, T.; Hermle, L.; Hilger, J.; Hillemacher, T.; Kuhlmann, T.; Kuhn, J.; Luckhaus, C.; Lüdecke, C.; Reimer, J.; Schneider, U.; Schroeder, W.; Stuppe, M.; Wiesbeck, G. A.; Wodarz, N.; McAnally, H.; … Scherbaum, N. Ranking the harm of psychoactive drugs including prescription analgesics to users and others - A perspective of German addiction medicine experts. Front. Psychiatry. 2020, 11, 592199. [Google Scholar] [CrossRef]
- Spencer, M. R.; Curtin, S. C.; Garnett, M. F. Alcohol-induced death rates in the United States, 2019–2020. NCHS Data Brief, no 448. Hyattsville, MD: National Center for Health Statistics. 2022. [CrossRef]
- Pinedo, M; Villatoro, A. P. The role of perceived treatment need in explaining racial/ethnic disparities in the use of substance abuse treatment services. J. Subst. Abuse Treat. 2020, 118, 108105. [Google Scholar] [CrossRef] [PubMed]
- Boucher, L. M.; Marshall, Z.; Martin, A.; Larose-Hébert, K.; Flynn, J. V.; Lalonde, C.; Pineau, D.; Bigelow, J.; Rose, T.; Chase, R.; Boyd, R.; Tyndall, M.; Kendall, C. Expanding conceptualizations of harm reduction: results from a qualitative community-based participatory research study with people who inject drugs. Harm Reduct. J. 2017, 14(1), 18. [Google Scholar] [CrossRef] [PubMed]
- Boucher, L. M.; Shoemaker, E. S.; Liddy, C. E.; Leonard, L.; MacPherson, P. A.; Presseau, J.; Martin, A.; Pineau, D.; Lalonde, C.; Diliso, N.; Lafleche, T.; Fitzgerald, M.; Kendall, C. E. “The Drug Use Unfortunately isn't all Bad”: Chronic disease self-management complexity and strategy among marginalized people who use drugs. Qual. Health Res. 2022, 32(6), 871–886. [Google Scholar] [CrossRef] [PubMed]
- Magwood, O.; Saad, A.; Ranger, D.; Volpini, K.; Rukikamirera, F.; Haridas, R.; Sayfi, S.; Alexander, J.; Tan, Y.; Pottie, K. Mobile apps to reduce depressive symptoms and alcohol use in youth: A systematic review and meta-analysis: A systematic review. Campbell Syst. Rev. 2024, 20(2), e1398. [Google Scholar] [CrossRef]
- Marino, E. N., Karns-Wright, T., Perez, M. C.,; Potter, J. S. Smartphone app-based contingency management and opioid use disorder treatment outcomes. JAMA Network Open 2024, 7, e2448405. [Google Scholar] [CrossRef]
- Kilian, C., Manthey, J., Carr, S., Hanschmidt, F., Rehm, J., Speerforck, S.,; Schomerus, G. Stigmatization of people with alcohol use disorders: An updated systematic review of population studies. Alcoholism, Clinical and Experimental Research, 2021; 45, 899–911. [Google Scholar] [CrossRef]
- El Hayek, S., Foad, W., de Filippis, R., Ghosh, A., Koukach, N., Mahgoub Mohammed Khier, A., Pant, S. B., Padilla, V., Ramalho, R., Tolba, H.,; Shalbafan, M. Stigma toward substance use disorders: a multinational perspective and call for action. Frontiers in Psychiatry 2024, 15, 1295818. [Google Scholar] [CrossRef]
- Cazalis, A., Lambert, L.,; Auriacombe, M. Stigmatization of people with addiction by health professionals: Current knowledge. A scoping review. Drug and Alcohol Dependence Reports 2023, 9, 100196. [Google Scholar] [CrossRef]
| Sample N | Population N (95% CI) in millions | % (95% CI) of all adult population | ||
| Alcohol or drug use disorder of all adult population | 19,555 | 46.4 (45.0 - 47.7) | 18.05 (17.63 - 18.46) | |
| Of adults with alcohol/drug use disorder | ||||
| Both alcohol and drug use disorder | 3,586 | 16.14 (15.27 - 17.04) | ||
| Alcohol use disorder, no drug use disorder | 8,166 | 45.29 (43-91 - 46.68) | ||
| Drug use disorder, no alcohol use disorder | 7,803 | 38.57 (37.47 - 39.69) | ||
| Substance use treatment among adults with alcohol/drug use disorder | ||||
| Received treatment | 2,766 | 6.7 (6.2 - 7.2) | 14.37 (13.45 - 15.33) | |
| Did not receive specialty treatment | 16,789 | 39.7 (38.5 - 40.9) | 85.63 (84.67 - 86.55) | |
| Among those who did not receive treatment and provided the reasons for treatment non-receipt | 16,416 | |||
| Did not seek treatment | 15,540 | 36.7 (35.7 - 37.7) | 94.55 (93.84 - 95.19) | |
| Sought or thought to get treatment but did not receive | 876 | 2.1 (1.8 - 2.4) | 5.45 (4.81 - 6.17) | |
| SUD treatment among those with AUD/DUD | Among treatment non-users | |||||||
| Received N=2,766 (14.37%) |
Did not receive N=16,789 (85.63%) |
P | Treatment seekers N=876 (5.45%) |
Treatment non-seeker N=15,540 (94.55%) |
P | |||
| Age group (%) | .002 | <.001 | ||||||
| 18-25 | 16.68 | 20.77 | 18.04 | 21.15 | ||||
| 26-34 | 20.36 | 23.39 | 35.87 | 22.72 | ||||
| 35-49 | 32.79 | 26.59 | 24.11 | 26.67 | ||||
| 50-64 | 23.08 | 19.79 | 18.19 | 19.82 | ||||
| 65+ | 7.08 | 9.46 | 3.79 | 9.64 | ||||
| Female (%) | 43.81 | 41.77 | .115 | 47.20 | 41.41 | .024 | ||
| Race/ethnicity (%) | .195 | .386 | ||||||
| Non-Hispanic White | 66.53 | 62.28 | 62.98 | 62.32 | ||||
| Non-Hispanic Black | 9.95 | 13.06 | 10.70 | 13.18 | ||||
| Hispanic | 16.50 | 17.27 | 16.73 | 17.27 | ||||
| Asian/Pacific Islander | 3.23 | 3.88 | 3.86 | 3.82 | ||||
| American Indian/Alaska Native | 0.91 | 0.71 | 0.99 | 0.70 | ||||
| Multi-racial | 2.89 | 2.80 | 4.74 | 2.71 | ||||
| Marital status (%) | <.001 | .154 | ||||||
| Married | 21.98 | 35.52 | 29.72 | 35.90 | ||||
| Widowed | 4.39 | 2.81 | 1.62 | 2.85 | ||||
| Divorced/separated | 24.93 | 14.63 | 15.04 | 14.45 | ||||
| Never married | 48.71 | 47.04 | 53.61 | 46.79 | ||||
| Residential area (%) | <.001 | .535 | ||||||
| Large metropolitan area | 56.0 | 50.07 | 58.49 | 55.87 | ||||
| Small metropolitan area | 33.02 | 33.95 | 32.16 | 33.17 | ||||
| Nonmetropolitan area | 10.98 | 15.98 | 9.36 | 10.96 | ||||
| Education (%) | <.001 | <.001 | ||||||
| < High school | 47.50 | 35.46 | 30.2 | 44.0 | ||||
| Some college/associate degree | 36.23 | 33.07 | 41.8 | 38.0 | ||||
| College degree | 16.28 | 31.47 | 28.0 | 18.0 | ||||
| Income (%) | <.001 | .761 | ||||||
| Below poverty | 28.17 | 16.71 | 18.25 | 16.63 | ||||
| Up to 2x poverty | 26.55 | 18.98 | 18.97 | 18.96 | ||||
| More than 2x poverty | 45.28 | 64.31 | 62.78 | 64.41 | ||||
| Any health insurance coverage (%) | 91.48 | 88.31 | .001 | 83.47 | 88.72 | .019 | ||
| Availability of workplace help with substance use problems (%) | 22.14 | 32.34 | <.001 | 31.03 | 33.02 | .526 | ||
| Parol or probation state (%) | 12.51 | 2.43 | <.001 | 3.79 | 2.41 | .299 | ||
| No. of chronic medical condition, M (SE) | 0.76 (0.03) | 0.59 (0.01) | <.001 | 0.59 (0.05) | 0.60 (0.01) | .807 | ||
| Types of substance use disorder (%) | <.001 | <.001 | ||||||
| Both alcohol and drug use disorder | 25.05 | 14.64 | 35.71 | 13.5 | ||||
| Alcohol, not drug, use disorder | 27.0 | 48.36 | 42.56 | 48.73 | ||||
| Drug, not alcohol, use disorder | 47.95 | 37.0 | 21.73 | 37.76 | ||||
| Alcohol use disorder (AUD) severity (%) | <.001 | <.001 | ||||||
| No AUD | 47.95 | 37.0 | 21.73 | 37.76 | ||||
| Mild | 15.37 | 39.43 | 16.27 | 40.92 | ||||
| Moderate | 10.29 | 13.69 | 15.38 | 13.66 | ||||
| Severe | 26.39 | 9.88 | 46.62 | 7.65 | ||||
| Drug use disorder (DUD) severity (%) | <.001 | <.001 | ||||||
| No DUD | 27.0 | 48.36 | 42.56 | 48.73 | ||||
| Mild | 27.79 | 31.05 | 13.19 | 32.06 | ||||
| Moderate | 15.78 | 11.98 | 10.88 | 12.02 | ||||
| Severe | 29.43 | 8.60 | 33.37 | 7.18 | ||||
| Problem self-perception (%) | 60.43 | 27.87 | <.001 | 81.71 | 25.36 | <.001 | ||
| Past-year mental illness (%) | <.001 | <.001 | ||||||
| None | 32.46 | 58.21 | 30.78 | 60.09 | ||||
| Mild | 19.73 | 16.36 | 21.77 | 15.84 | ||||
| Moderate | 18.82 | 12.26 | 16.66 | 11.76 | ||||
| Severe | 28.99 | 13.18 | 30.79 | 12.32 | ||||
| Receipt of mental health treatment receipt (%) | 74.18 | 30.80 | <.001 | 37.05 | 30.53 | .021 | ||
| Inpatient treatment | 17.18 | 1.47 | <.001 | 1.56 | 1.37 | |||
| Outpatient treatment | 60.84 | 17.86 | <.001 | 23.79 | 17.52 | |||
| Medication therapy | 51.24 | 22.80 | <.001 | 31.40 | 22.46 | |||
| Phone/video treatment | 46.06 | 18.44 | <.001 | 21.50 | 18.36 | |||
| Of those with any SUD | Among treatment non-users | ||
| Treatment users vs. Non-users aOR (95% CI) |
Treatment seekers vs. Non-seekers aOR (95% CI) |
||
| Age group: vs. 18-25 | |||
| 26-34 | 1.41 (1.13-1.76)** | 2.04 (1.48-2.82)*** | |
| 35-49 | 2.09 (1.65-2.65)*** | 1.38 (0.91-2.10) | |
| 50-64 | 2.09 (1.55-2.82)*** | 1.94 (1.07-3.54)* | |
| 65+ | 1.87 (1.12-3.10)* | 1.27 (0.52-3.10) | |
| Male vs. Female | 1.18 (1.01-1.39)* | 0.67 (0.51-0.88)** | |
| Race/ethnicity: vs. Non-Hispanic White | |||
| Non-Hispanic Black | 0.86 (0.68-1.07) | 0.95 (0.58-1.57) | |
| Hispanic | 1.01 (0.76-1.35) | 1.08 (0.73-1.60) | |
| Asian/Pacific Islander | 1.23 (0.54-2.77) | 1.00 (0.40-2.51) | |
| American Indian/Alaska Native | 0.95 (0.42-2.12) | 1.17 (0.52-2.48) | |
| Multi-racial | 0.88 (0.61-1.26) | 1.73 (0.97-3.09) | |
| Marital status: vs. Married | |||
| Widowed | 1.75 (1.03-2.97)* | 0.53 (0.17-1.63) | |
| Divorced/separated | 1.63 (1.26-2.10)*** | 0.91 (0.58-1.45) | |
| Never married | 1.36 (1.06-1.74)* | 1.00 (0.75-1.32) | |
| Residential area: vs. Large metropolitan area | |||
| Small metropolitan area | 0.92 (0.77-1.11) | 0.82 (0.60-1.14) | |
| Nonmetropolitan area | 1.12 (0.87-1.44) | 0.74 (0.50-1.09) | |
| Education: vs. < High school | |||
| Some college/associate degree | 0.80 (0.66-0.97)* | 1.23 (0.86-1.78) | |
| College degree | 0.48 (0.37-0.63)*** | 1.12 (0.76-1.65) | |
| Income: vs. Below poverty | |||
| Up to 2x poverty | 0.87 (0.69-1.10) | 0.73 (0.46-1.17) | |
| More than 2x poverty | 0.61 (0.48-0.78)*** | 0.77 (0.52-1.13) | |
| Any health insurance coverage | 1.46 (1.11-1.93)** | 0.71 (0.48-1.04) | |
| Availability of workplace help with substance use problems | 0.82 (0.65-1.04) | 0.98 (0.73-1.30) | |
| Parol or probation state | 3.31 (2.23-4.92)*** | 1.01 (0.37-2.72) | |
| No. of chronic medical condition, M (SE) | 0.97 (0.88-1.06) | 1.04 (0.88-1.22) | |
| Types of substance use disorder: vs. Alcohol, not drug, use disorder | |||
| Drug, not alcohol, use disorder | 1.87 (1.39-2.52)*** | 0.62 (0.38-1.02) | |
| Both alcohol and drug use disorder | 1.17 (0.84-1.63) | 0.72 (0.45-1.14) | |
| Alcohol use disorder (AUD) severity: vs. No AUD or mild AUD | |||
| Moderate | 1.63 (1.18-2.25)** | 1.95 (1.21-3.11)** | |
| Severe | 3.85 (2.82-5.26)*** | 7.07 (4.72-10.57)*** | |
| Drug use disorder (DUD) severity: vs. No DUD or mild severity | |||
| Moderate | 1.54 (1.20-1.97)** | 1.79 (1.09-2.96)* | |
| Severe | 2.81 (2.27-3.47)*** | 6.85 (4.30-10.91)*** | |
| Problem self-perception | 2.12 (1.74-2.58)*** | 6.47 (4.59-9.10)*** | |
| Past-year mental illness: No mental illness | |||
| Mild | 1.17 (0.91-1.50) | 1.86 (1.33-2.62)** | |
| Moderate | 1.08 (0.83-1.39) | 1.83 (1.17-2.86)** | |
| Severe | 1.06 (0.82-1.38) | 2.14 (1.39-3.29)** | |
| Receipt of mental health treatment | 6.07 (4.73-7.78)*** | 0.95 (0.69-1.31) | |
| Model statistics | N=19,548; Population N=46.4 million; Design df=50; F (34,17)=45.23; p <.001 |
N=16,410; Population N=38.8 million; Design df=50; F (34,17)=16.73; p <.001 |
|
| Sample N | Reason - Personal | % | Sample N | Reason – Environmental/Structural | % | |
|---|---|---|---|---|---|---|
| 864 | Thought could handle by self | 76.34 | 861 | The cost was too high | 47.96 | |
| 850 | Not ready to start treatment | 61.15 | 870 | Did not know where to go | 44.80 | |
| 852 | Not ready to stop/cut use | 53.95 | 852 | Not enough time for treatment | 41.62 | |
| 870 | Worried about what people would think/say | 43.51 | 820 | No health insurance | 38.49 | |
| 857 | Worried that the information would not be kept private | 34.50 | 774 | Health insurance did not cover | 36.97 | |
| 846 | Did not think treatment would help | 27.44 | 856 | Thought would lose job/home/child | 36.61 | |
| 858 | Afraid to be forced against the will | 24.21 | 838 | Could not find a preferred provider | 32.86 | |
| 855 | No one would care if I got better | 19.34 | 825 | No opening with preferred provider | 13.47 | |
| 856 | Family/friends /religion would not like | 17.10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





