1. Introduction
Ameloblastoma is a benign, locally aggressive epithelial odontogenic neoplasm, which reveals several different microscopic variants [1-3]. Mural ameloblastoma is a subtype of unicystic ameloblastoma characterized by the expansion or infiltration of tumor nodules into the fibrous wall of the cyst. The behavior of this subtype is highly aggressive, with a risk of recurrence comparable with that of conventional ameloblastoma. Consequently, the preferred treatment for unicystic mural ameloblastoma is broad resection of the tumor. In this case report we describe the successful conservative treatment of a unicystic mural ameloblastoma associated with an impacted tooth. The conservative treatment involved marsupialization, followed by the enucleation of the lesion and the reconstruction of the defect using xenograft bone material. Our cautious approach maintained the integrity of the inferior alveolar nerve and ensured proper mandibular function, leading to a favorable aesthetic result. The condition is categorized into three types; solid, cystic (uni-cystic), and peripheral. Unicystic ameloblastomas are seen more often in younger patients during the second decade of life. The posterior mandible is the most common location [4-5]. This paper presents a case of unicystic (mural) ameloblastoma located in the mandible of a 22-year-old woman.
2. Case Report:
A 22-year-old female patient reported to our outpatient department with a chief complaint of swelling in the lower right region of the body of the mandible for 4 years. Cone beam CT (CBCT) revealed the extent of the lesion and the loss of cortical bone on both the lingual and buccal sides, along with a thinning of the bone base. Furthermore, the inferior alveolar nerve (IAN) canal was affected and measured approximately 20.5*26.2 cm after previous marsupialization. The patient observed swelling and misalignment of the teeth in the lower right posterior area and reported experiencing pain in that same region. The pain was dull and aching, occurring intermittently, worsening during chewing and easing with rest. During the extraoral examination, a diffuse swelling was noted on the lower third of the face, extending to the right side, measuring about 4 × 4 cm. The skin over the swelling appeared normal, with no visible pulsations or discharge. On palpation, the swelling was firm. The preliminary diagnosis was an odontogenic dentigerous cyst or ameloblastoma. A small sample of the cyst wall was collected for histological analysis. The cystic membrane was marsupialized, and a tube was inserted into the cavity to ensure it remained open. In the first month after surgery, the surgical site was rinsed weekly, followed by monthly follow-up visits at the clinic. The histological report supported a diagnosis of mural unicystic ameloblastoma. The marsupialization procedure was kept in place for three years, during which the cortical rim of the mandibular canal remineralized, and new bone formation and cortical borders developed. A second surgery was scheduled, during which an envelope flap and bone removal—similar to the procedure for impacted tooth extraction—were performed to gain access to the lesion. This approach facilitated the enucleation of the ameloblastoma, involved scraping the bone walls to eliminate any potential ameloblastic infiltrates, and included extensive irrigation with garamycin antibiotics, followed by graft augmentation in the defect. The surgical specimen was sent for histological analysis, and the pathologist confirmed a diagnosis of UA with mural growth.
An panoramic view was conducted 9 months after the excision, showing nearly complete mineralization of the osteolytic area. Additionally, there was significant ossification of the mandibular angle. The patient was monitored for 18 months following surgery. An panoramic view revealed complete healing of the lesion, full ossification of the defect, no signs of recurrence, and preservation of the mandibular angle and ramus profile. Clinically, the treatment resulted in no deformity, no changes to the mandibular contour, and no functional issues. The patient remained symptom-free and showed no significant neurological damage to the inferior alveolar nerve (IAN). However, due to the aggressive nature of this subtype of UA and the potential for recurrence, the patient will continue to be closely monitored with long-term clinical and radiological follow-up. This ongoing supervision will include periodic imaging studies to assess any potential changes in the mandibular area, ensuring early detection of any issues that may arise. Additionally, the healthcare team will provide the patient with guidance on maintaining optimal oral hygiene and overall health to support long-term outcomes.
Figure 1.
OPG showing preoperative lesion related to Impacted lower 3rd molar tooth in right side of mandible.
Figure 1.
OPG showing preoperative lesion related to Impacted lower 3rd molar tooth in right side of mandible.
Figure 2.
OPG showing postoperative removal of Impacted lower 3rd molar tooth in right side of mandible and marsupialization.
Figure 2.
OPG showing postoperative removal of Impacted lower 3rd molar tooth in right side of mandible and marsupialization.
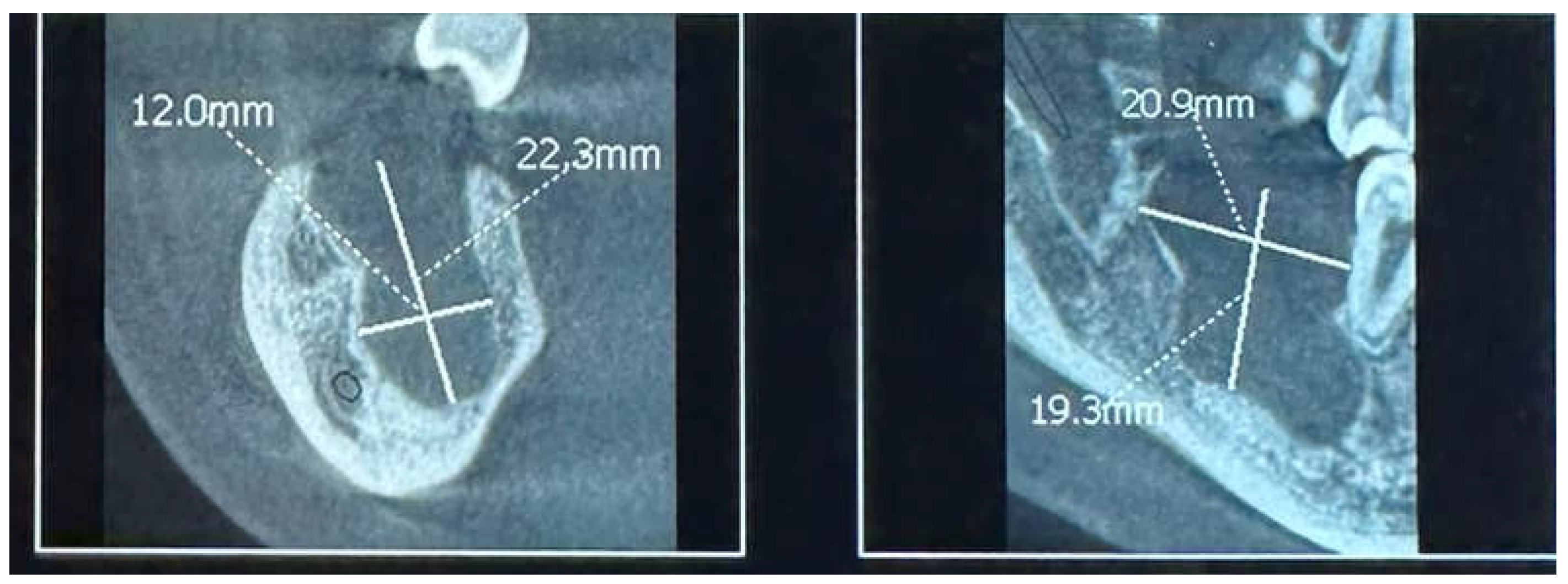
Figure 3.
CBCT showing postoperative 2 years of marsupialization.
Figure 3.
CBCT showing postoperative 2 years of marsupialization.
Figure 4.
Clinical photo showing preoperative of enucleation.
Figure 4.
Clinical photo showing preoperative of enucleation.
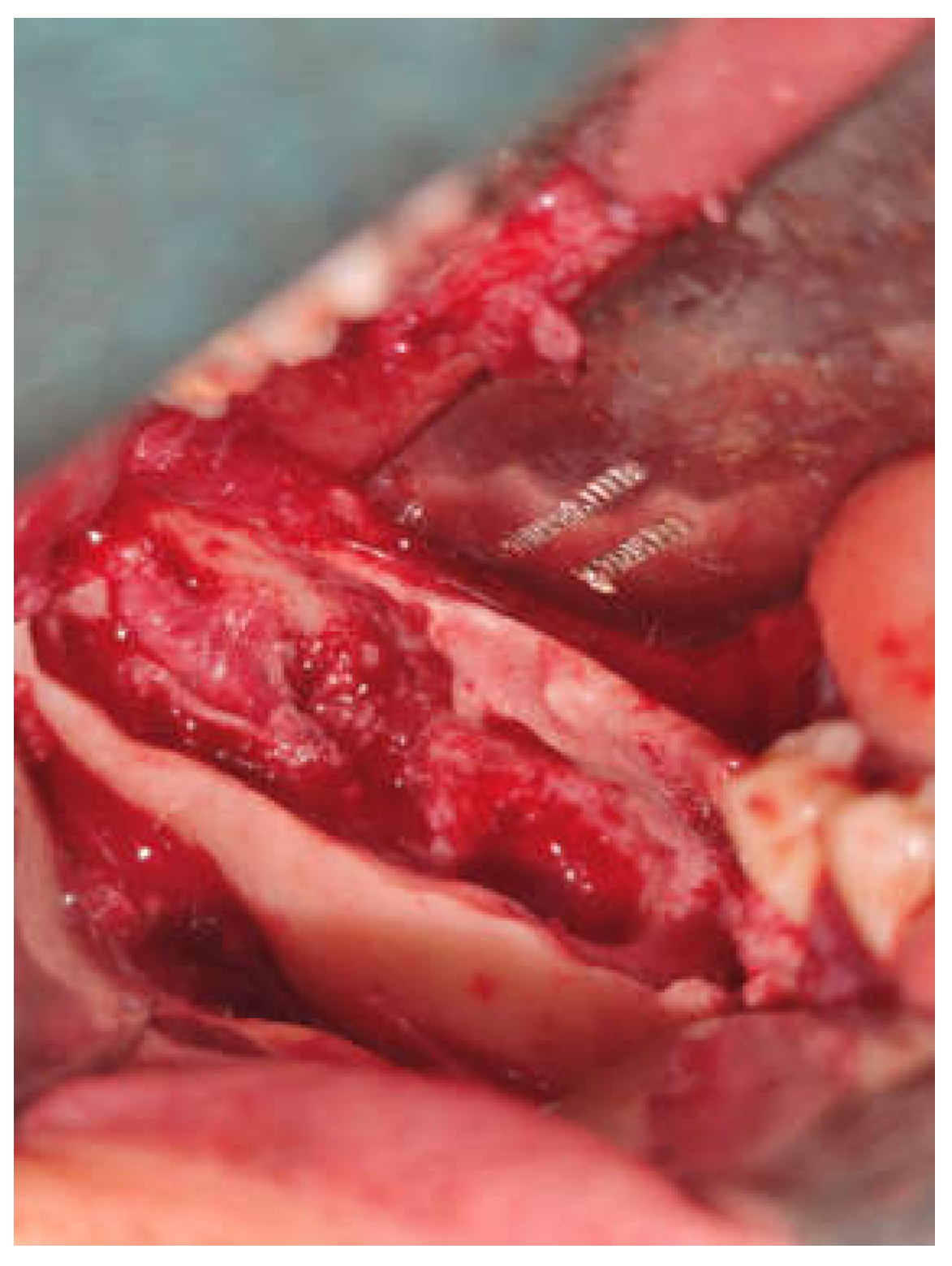
Figure 5.
Clinical photo showing flap design and exposure lesion.
Figure 5.
Clinical photo showing flap design and exposure lesion.
Figure 6.
Clinical photo showing lesion removal and preservation of IAN.
Figure 6.
Clinical photo showing lesion removal and preservation of IAN.
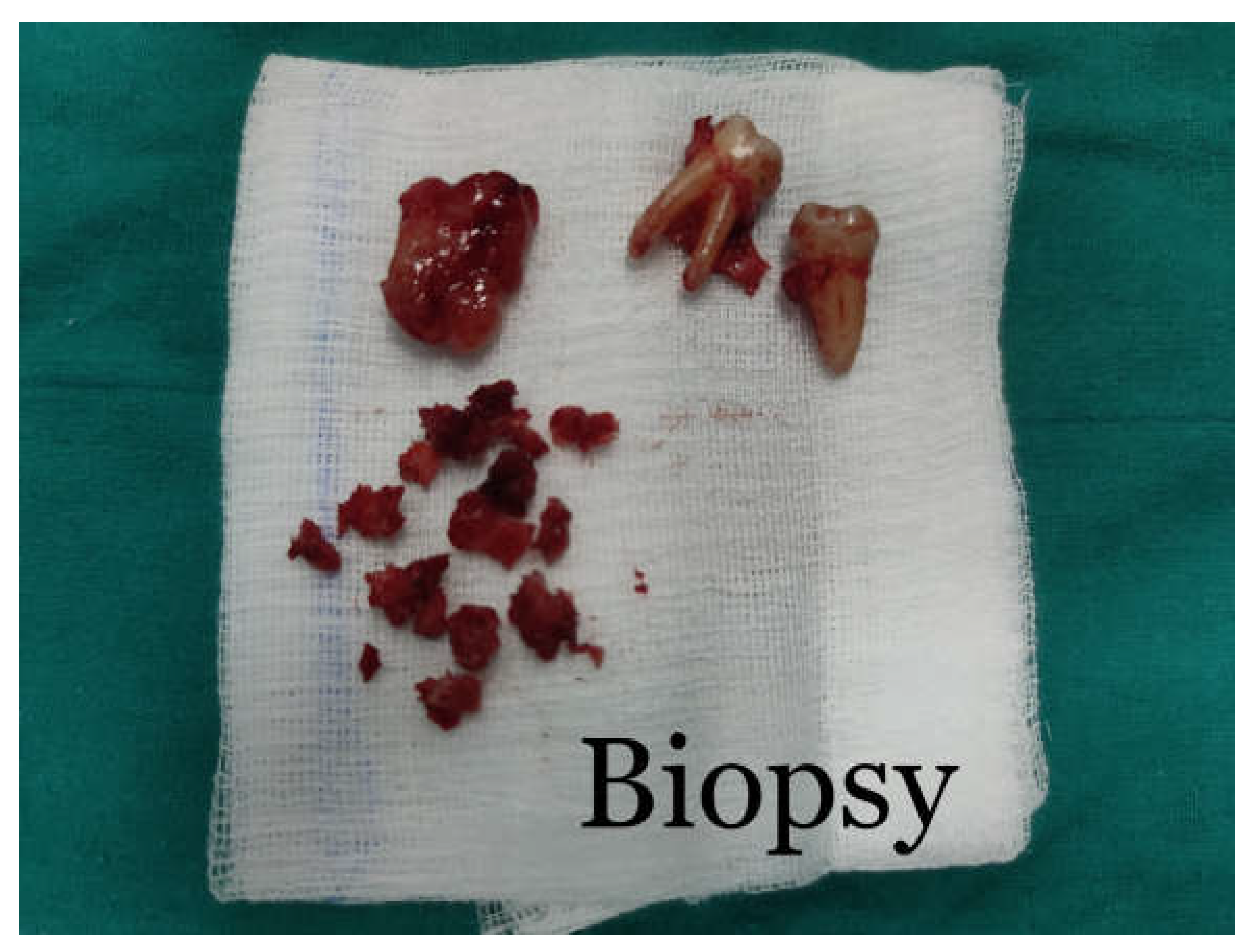
Figure 7.
Clinical photo showing excisional biopsy for histopathological examination.
Figure 7.
Clinical photo showing excisional biopsy for histopathological examination.
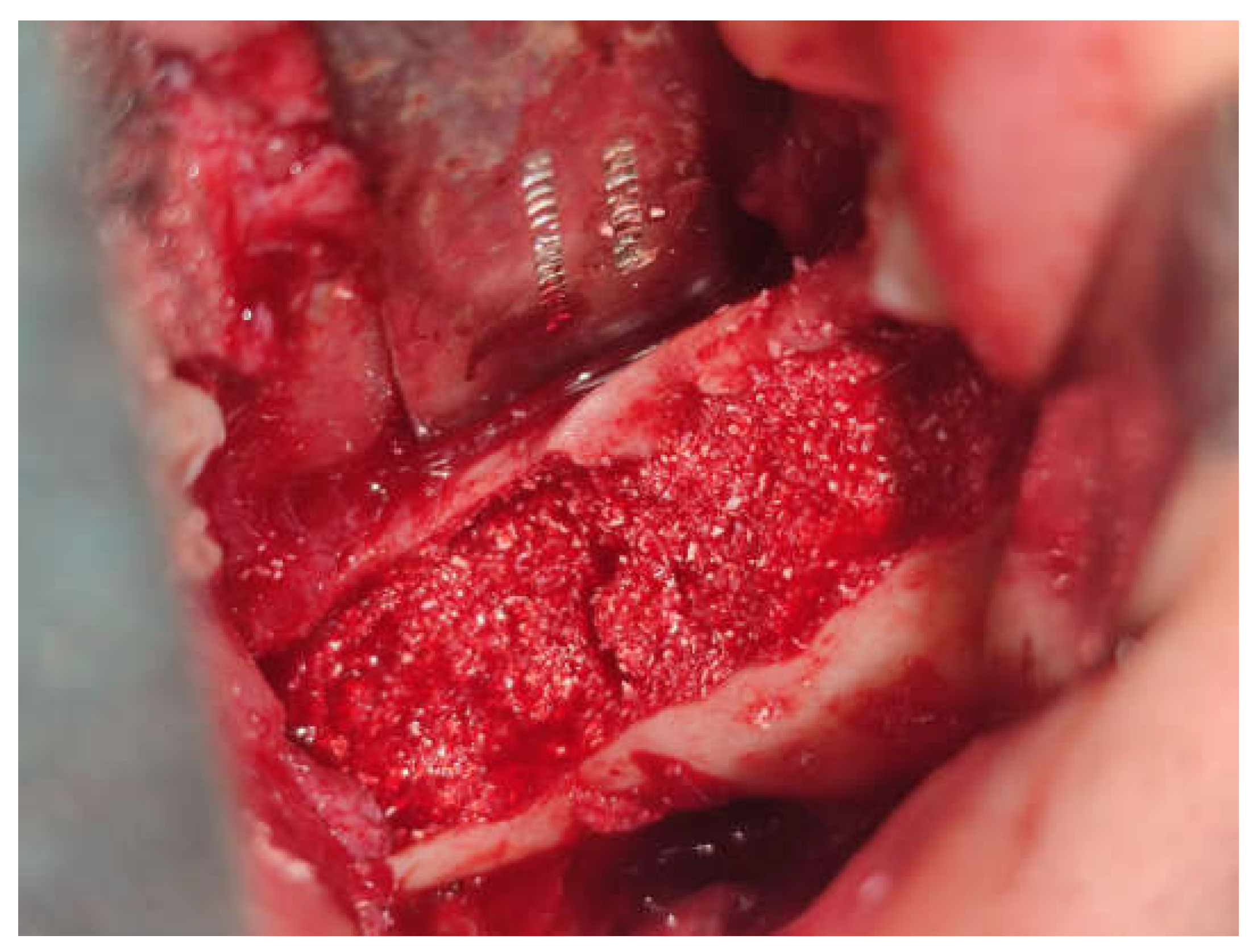
Figure 8.
Clinical photo showing bone graft in defect.
Figure 8.
Clinical photo showing bone graft in defect.
Figure 9.
OPG showing 2 years postoperative.
Figure 9.
OPG showing 2 years postoperative.
3. Discussion
According to the 2003 WHO classification system, ameloblastomas are categorized based on differences in biological behavior, treatment approaches, and recurrence rates into the following types: classic solid/multicystic ameloblastoma, unicystic ameloblastoma (UCA), peripheral ameloblastoma, and desmoplastic ameloblastoma, including hybrid lesions. UCA is a rare form, accounting for approximately 6% of all ameloblastomas. It typically occurs in younger individuals, often between 16 and 20 years of age, with nearly half of the cases presenting during the second decade of life, as seen in our case. Radiographically, UCAs exhibit two main patterns: unilocular and multilocular, with a clear preference for the unilocular configuration. This inclination is particularly pronounced in the dentigerous variant, which has a unilocular to multilocular ratio of 4.3:1, compared to a 1.1:1 ratio in the non-dentigerous type. Involvement of adjacent teeth frequently leads to varying degrees of root resorption. The differential diagnosis for large unilocular osteolytic lesions should consider UCA, keratocysts, and odontogenic cysts. However, a definitive diagnosis necessitates histopathological evaluation via biopsy. In this case, an incisional biopsy facilitated marsupialization of the lesion while awaiting histological confirmation. Marsupialization proves especially effective in the molar region and mandibular ramus, owing to the structural nature of the bone and surrounding anatomy. The healing potential depends on the patient's age, lesion location, surgical technique, and tumor growth patterns. Favorable outcomes rely heavily on new bone regeneration rates at the site of pathology. Histological examination revealed mural growth within the UCA. When managed exclusively by surgical enucleation or enucleation with curettage, mural ameloblastoma exhibits a recurrence rate of 35.7%. However, employing a radical approach significantly reduces recurrence risk. Surgical recommendations suggest maintaining at least a 1-cm safety margin to minimize risk further. In this case, the primary surgical goal was to preserve mandibular continuity. If discontinuity arises, patients may encounter issues like aesthetic deformities, facial asymmetry, limited mouth opening, difficulties with chewing, and a reduced quality of life. To prevent these complications, some experts recommend conservative management for patients who can commit to long-term follow-up. In this patient's treatment, a conservative approach was initially adopted to preserve the lower border of the mandible, reconstruct the vestibular and lingual cortical bone, and restore the cortical rim of the mandibular canal. Based on clinical experience, follow-up continues for as long as needed, irrespective of any surgical interventions. The follow-up protocol includes a CBCT scan conducted one year after surgery and annual orthopantomograms for up to five years. Any suspected recurrences should be evaluated with CBCT for a comprehensive assessment.
4. Conclusions
Mural ameloblastoma, while regarded as a variant of unicystic ameloblastoma (UA), exhibits an aggressiveness and recurrence rate comparable to conventional ameloblastoma (CA), often necessitating radical treatment. However, in certain cases, conservative approaches can serve as a viable alternative, allowing for the preservation of aesthetic functions and overall quality of life. These minimally invasive strategies necessitate active patient involvement and thorough radiographic monitoring. In the case presented, positive functional and aesthetic results were attained, with no indications of relapse noted two years after the surgery.
References
- Argyris PP, McBeain MJ, Rake A, Pambuccian SE, Gopalakrishnan R, Koutlas IG. Recurrent ameloblastoma of the mandible with unusual granular cell component. Int J Surg Pathol. 2015; 23: 298–304. [CrossRef]
- Matsushita Y, Fujita S, Kawasaki G, Hirota Y, Rokutanda S, Yamashita K, et al. Granular cell ameloblastoma: case report of particular ameloblastoma histologicallyresembling oncocytoma. Pathol Int. 2015; 65: 43–47. [CrossRef]
- Thillaikarasi R, Balaji J, Gupta B, Ilayarja V, Vani NV, Vidula B, et al. Cystic granular cell ameloblastoma. J Maxillofac Oral Surg. 2010; 9: 310–313. [CrossRef]
- Jain K, Sharma G, Kardam P, Mehendiratta M. Unicystic Ameloblastoma of Mandible with an Unusual Diverse His topathology: A Rare Case Report. J Clin Diagn Res. 2017; 11: ZD04-ZD05. [CrossRef]
- Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. Odontogenic cysts and tumors. 4rd ed. Philadelphia: Saunders; 2016. p. 654-660.
- Reichart P., A. and Philipsen H. P., Odontogenic Tumors and Allied Lesions, 2004, Quintessence, Hanover, Germany.
- Kumar K. R. K., George G. B., Padiyath S., and Rupak S., Mural unicystic ameloblastoma crossing the midline: a rare case report, International Journal of Odontostomatology. (2012) 6, no. 1, 97–103. [CrossRef]
- Gardner D., G. and Corio R. L., Plexiform unicystic ameloblastoma. A variant of ameloblastoma with a low-recurrence rate after enucleation, Cancer. (1984) 53, no. 8, 1730–1735, 2-s2.0-0021212883. [CrossRef]
- Eversole L., R. , Leider A. S., and Strub D., Radiographic characteristics of cystogenic ameloblastoma, Oral Surgery Oral Medicine and Oral Pathology. (1984) 57, no. 5, 572–577, 2-s2.0-0021236242. [CrossRef]
- Peter A., Reichart P. A., and Philipsen H. P., Unicystic ameloblastoma, Odontogenic Tumors and Allied Lesions, 2004, Quintessence, London, UK, 77–86, editorial and consensus conference held in Lyon, France (WHO,IARD) in July 2003 in conjunction with preparation of new WHO Blue Book, Pathology and genetics of tumors of head and neck.
- Kim J, Nam E, Yoon S. Conservative management (marsupialization) of unicystic ameloblastoma: literature review and a case report. Maxillofac Plast Reconstr Surg 2017 25;39(1):38. [CrossRef]
- Nakamura N, Higuchi Y, Tashiro H, Ohishi M. Marsupialization of cystic ameloblastoma: a clinical and histopathologic study of the growth characteristics before and after marsupialization. J Oral Maxillofac Surg 1995;53(7):748–54. [CrossRef]
- Li TJ, Wu YT, Yu SF, Yu GY. Unicystic ameloblastoma: a clinicopathologic study of 33 Chinese patients. Am J Surg Pathol 2000;24(10):1385–92.
- Ghandhi D, Ayoub AF, Pogrel MA, MacDonald G, Brocklebank LM, Moos KF. Ameloblastoma: a surgeon’s dilemma. J Oral Maxillofac Surg 2006;64(7):1010–4. [CrossRef]
- Giraddi GB, Arora K, Saifi AM. Ameloblastoma: a retrospective analysis of 31 cases. J Oral Biol Craniofac Res 2017;7(3):206–11. [CrossRef]
- Effiom OA, Ogundana OM, Akinshipo AO, Akintoye SO. Ameloblastoma: current etiopathological concepts and management. Oral Dis 2018;24:307–16. [CrossRef]
- Hammarfjord O, Roslund J, Abrahamsson P, Nilsson P, Thor A, Magnusson M, Kjeller G, Englesson-Sahlstr€om C, Strandkvist T, Warfvinge G, Krüger-Weiner C. Surgical treatment of recurring ameloblastoma, are the options? Br J Oral Maxillofac Surg 2013;51:762–6. [CrossRef]
- Hasegawa T, Imai Y, Takeda D, Yasuoka D, Ri S, Shigeta T, Minamikawa T, Shibuya Y, Komori T. Retrospective study of ameloblastoma: the possibility of conservative treatment. Kobe J Med Sci 2013;59(4):E112–21.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).