1. Introduction and Clinical Significance
Hyperattenuating contents in the gastrointestinal (GI) contents on CT examinations of the abdomen, pelvis, or chest are commonly encountered, and almost always due to the purposeful ingestion of an oral contrast agent, usually barium or iodine-based, employed to aid in detection of gastrointestinal disease. Other, less common, sources of high attenuation in the lumen of the bowel include orally administered medications, such as antacids, foreign objects, and medical devices. Lokelma (sodium zirconium cyclosilicate (SZC)), a compound used to treat hyperkalemia, has a hyperattenuating appearance on CT and radiography due to the presence of zirconium, a transition metal in the periodic table. We report a patient in which SZC was seen in the GI tract as hyperattenuating material on CT, and which was initially mistakenly diagnosed as an acute GI bleed in the cecum. This phenomenon, and potential pitfall, is not well known to radiologists, to our knowledge.
2. Case Presentation
Case
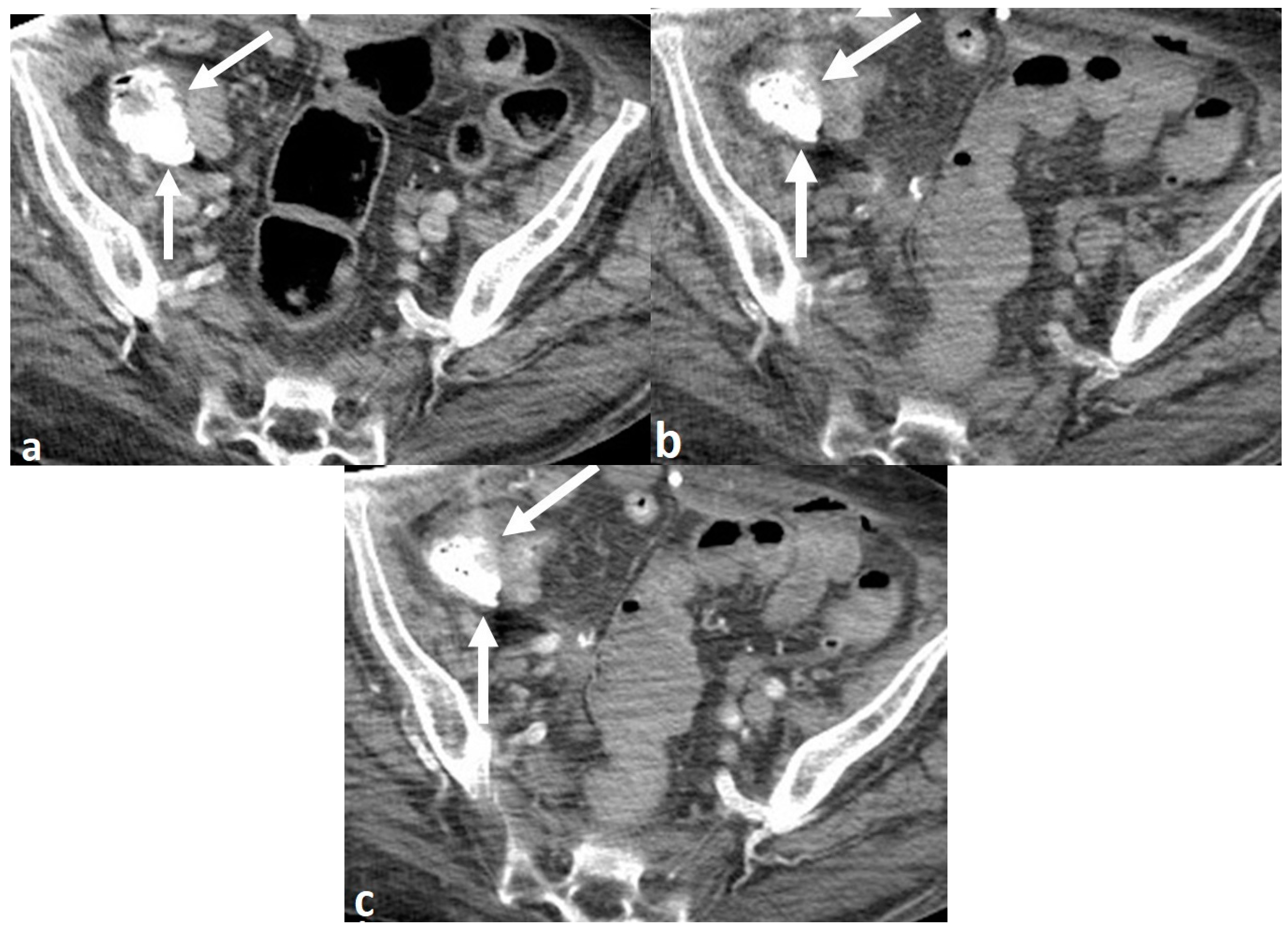
A 72-year-old woman with multiple medical conditions, including end-stage renal disease on hemodialysis, presented to the Emergency Department with rectal bleeding. The patient was found to be hyperkalemic on admission (potassium of 5.7). The patient underwent single-phase portal venous phase CT of the abdomen and pelvis, performed with intravenous contrast and without positive oral contrast. The scan showed hyperattenuating contents in the cecum, which was interpreted by the attending radiologist to be contrast extravasation from an active gastrointestinal (GI) bleed (
Figure 1A). There were no other acute or otherwise substantial findings on the scan, including no bowel wall thickening or mass. Based on this interpretation, a multi-phase CT angiogram of the abdomen and pelvis was performed the following day, in which similar intraluminal high density, measuring 1085 Hounsfield Units(HU), was seen in the cecum on the non-IV contrast enhanced series of the examination, performed prior to the administration of intravenous contrast, proving that this was not active bleeding (
Figure 1B,C). The arterial and venous phase series from the CT angiogram showed no contrast extravasation anywhere in the GI tract to suggest an acute GI bleed. Subsequent discussion with the clinical team caring for the patient revealed that the patient was being treated with SZC for her hyperkalemia, which explained the source of the hyperattenuating material in the bowel.
3. Discussion
Positive oral contrast agents used for X-ray or computed tomography (CT) are usually barium or iodine-based. Additionally, there are a wide spectrum of orally administered medications that are radiopaque on CT, including prescribed drugs, over-the-counter remedies, and multivitamins[
1,
2]. The hyperattenuating property of a drug can be due to a variety of substances, including but not limited to iodine, iron, bismuth, potassium, sulfur, aluminum, and calcium. Theoretically, any material containing a high atomic number element or with high mass density could be hyperattenuating. Rarely, hyperattenuating medications can be the source of misdiagnosis on radiography or CT, potentially being mistaken for gallstones, nephrolithiasis, gastric bleeding, and foreign objects[
3,
4,
5,
6,
7]. Sodium zirconium cyclosilicate (SZC) is a relatively new medication, approved by the United States Food and Drug Administration in 2018. While it has been shown to be hyperattenuating on various imaging modalities[
8,
9,
10,
11,
12], there is a paucity of literature and lack of knowledge among clinicians and radiologists regarding this fact.
Several recent case reports in the medical literature have shown SZC to be very dense on CT[
8,
9,
10,
11], with attenuation similar to routinely used barium and iodine based oral contrast agents, and iodine-based intravenous contrast. Additionally, since SZC is administered as a liquid suspension, it will have a more diffuse distribution in the bowel than pill-based medications, and thus can mimic oral contrast, although the quantity of SZC in the bowel would be expected to be less than that of a routine oral contrast preparation used for abdominal and pelvic CT examinations. Kolesnik et al. demonstrated high attenuation in vitro radiopacity of a solution of SZC and water on CT, with Hounsfield unit (HU) measurements ranging from 1040-1878 HU[
8]. McCarney et al. showed significant alterations of bone mineral density measurements on dual-energy X-ray absorptiometry (DXA) scan when scanning SZC solutions of varying concentrations with spine and body phantoms[
12]. However, none of these publications were in the imaging literature.
SZC has been shown to effectively treat hyperkalemia, with low risk of hypokalemia, and favorable tolerability and safety profiles compared to placebo. It is an inorganic, insoluble, non-polymer zirconium silicate compound that binds potassium and ammonium cations in the gastrointestinal tract in exchange for hydrogen and sodium cations, allowing for the excretion of potassium through the GI tract. The beneficial potassium-lowering effects can be utilized in patients with chronic kidney disease, heart failure, diabetes mellitus, and concomitant use of medications targeting the renin-angiotensin-aldosterone-system, and maintained for up to 12 months [
13]. It is not absorbed in the GI tract [
14].
The hyperattenuating effect of SZC is due to zirconium, which has an atomic number of 40. Higher atomic number elements have a greater number of electrons with which photons may interact, and a denser electron cloud, and therefore attenuate a higher proportion of the X-ray beam than lower atomic number elements. By way of comparison, the atomic numbers of barium and iodine are 56 and 53 respectively. Of note, the attenuation of SZC in the case patient was qualitatively similar to barium oral contrast and iodine-based oral and intravenous contrast agents on CT, and did not cause any noticeable beam hardening artifact from its opacity.
Although the general radiological community may not be familiar with the imaging appearance of zirconium, it is commonly used in dentistry in the form of zirconia, an oxidized form of zirconium, which has metal and non-metal properties and is the basis for ceramic based implants. The imaging appearance of zirconium and titanium-based implants, as well as their potential to cause image-degrading artifacts, is well documented in the dental literature.[
15,
16,
17]
The clinical utilization of SZC is on the rise, and radiologists are therefore more likely to encounter SZC in the GI tract on CT examinations. Knowledge regarding the imaging appearance of SZC is important, as it can be the cause of otherwise unexplained high attenuation in the GI tract on CT in a patient being treated for hyperkalemia. Moreover, SZC could potentially lead to misdiagnosis, as it initially did in our patient, in which the presence of SZC was mistaken for acute gastrointestinal hemorrhage. This is an important consideration in a patient in which a CT examination is performed only with intravenous contrast-enhanced images. A CT angiography performed for evaluation of acute GI bleeding typically consists of both non-enhanced and IV contrast-enhanced (usually arterial and more delayed phase) acquisitions. The non-enhanced series is essential to avoid misdiagnosis of commonly found hyperattenuating material, including surgical clips, suture, stents and residual oral contrast from prior CT scans, as active bleeding, as it effectively did in our patient.[
18] Alternatively, SZC may obscure the presence of intraluminal contrast extravasation in a patient experiencing acute GI bleeding. The high attenuation of SZC could also hinder evaluation of mural abnormalities of the intestine, such as perforation, enteritis, ischemia or neoplasm, or could be mistaken for an ingested foreign object.
4. Conclusion
We present a case of hyperattenuating contents in the GI tract on CT scan due to lokelma (sodium zirconium cyclosilicate), a relatively new potassium lowering agent. Recognition of SZC as a potential source for high density in the GI tract may help reduce confusion amongst clinicians and radiologists when seen on CT, and could potentially avoid non diagnostic or erroneous interpretations of CT scans for bowel related disease.
Author Contributions
Conceptualization, JJH.; methodology, JJH, JR; writing—original draft preparation, JR; review and editing, JJH, DSK.; supervision, JJH, DSK. All authors have read and agreed to the published version of the manuscript.
Funding
This paper received no external funding.
Institutional Review Board Statement
Ethical review and approval were not required because case reports are not considered research. The patient’s information has been de-identified.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations were used in this manuscript:
| CT |
Computed Tomography. |
| SZC |
Sodium Zirconium Cyclosilicate. |
| GI |
Gastrointestinal. |
| DXA |
Dual-energy X-ray absorptiometry. |
| HU |
Hounsfield Unit. |
References
- Savitt DL, Hawkins HH, Roberts JR. The radiopacity of ingested medications. Annals of emergency medicine. 1987, 16, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Chan YC, Lau FL, Chan JC, Hon TY. A study of drug radiopacity by plain radiography. Hong Kong Journal of Emergency Medicine. 2004, 11, 205–210. [Google Scholar] [CrossRef]
- Commandeur JP, Metwaly A, Büchler L, Speiser J, Brander L, Reintam Blaser A. A degrading potassium tablet mimicking active gastric bleeding in a computer tomographic investigation. Case Reports in Radiology. 2020, 2020, 9791519. [Google Scholar]
- Florez MV, Evans JM, Daly TR. The radiodensity of medications seen on x-ray films. InMayo Clinic Proceedings 1998 Jun 1 (Vol. 73, No. 6, pp. 516–519). Elsevier.
- Onal B, Citgez S, Tansu N, Talat Z, Oner A. Tablets of the potassium citrate may cause a stone-like image: a case report. Urological research. 2009, 37, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Schreuder MF, Kortmann BB, Cornelissen EA. A boy with radiopacities on his abdominal X-ray. Journal of Paediatrics and Child Health. 2013, 49, 420. [Google Scholar] [CrossRef] [PubMed]
- Khara HS, Diehl DL, Metwally MJ, Schwender BJ. Bismuth subsalicylate tablet masquerading as vanishing button battery in the stomach. Gastrointestinal Endoscopy. 2014, 79, 539–540. [Google Scholar] [CrossRef] [PubMed]
- Kolesnik M, Berezovsky D, Sayegh M, Samarneh M. Radiopacity of sodium zirconium cyclosilicate on CT imaging. CEN Case Reports. 2021, 10, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Kotake H, Matsuda T, Yazawa M. Opaque Densities in the GI Tract of a Patient Treated for Hyperkalemia. Kidney360 2023, 4, e861–e862. [Google Scholar] [CrossRef] [PubMed]
- Angioi A, Floris M, Lepori N, Cabiddu G, Pani A. Radiopacity of Sodium Zirconium Cyclosilicate in Computed Tomography: a case of a patient with Hyperkalemia and kidney disease. Renal Failure. 2023, 45, 2284839. [Google Scholar] [CrossRef] [PubMed]
- Boss R, Nguyen M, Wahi-Gururaj S. Lokelma's Interaction With Computed Tomography Angiography. Annals of Internal Medicine: Clinical Cases. 2023, 2, e230888. [Google Scholar]
- McCarney B, Binkley N, Krueger D. A newly recognized DXA confounder: the potassium-binding medication sodium zirconium cyclosilicate. Journal of Clinical Densitometry. 2021, 24, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Stavros, F, Yang, A, Leon, A, Nuttall, M, Rasmussen, HS. Characterization of structure and function of ZS-9, a K+ selective ion trap. PLoS ONE. 2014, 9, e114686. [Google Scholar]
- Hoy, S.M. Sodium zirconium cyclosilicate: a review in hyperkalaemia. Drugs 2018, 78, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Chen YW, Moussi J, Drury JL, Wataha JC. Zirconia in biomedical applications. Expert review of medical devices. 2016, 13, 945–963. [Google Scholar] [CrossRef] [PubMed]
- Smeets R, Schöllchen M, Gauer T, Aarabi G, Assaf AT, Rendenbach C, Beck-Broichsitter B, Semmusch J, Sedlacik J, Heiland M, Fiehler J. Artefacts in multimodal imaging of titanium, zirconium and binary titanium–zirconium alloy dental implants: an in vitro study. Dentomaxillofacial Radiology. 2017, 46, 20160267. [Google Scholar] [CrossRef] [PubMed]
- Fontenele RC, Nascimento EH, Vasconcelos TV, Noujeim M, Freitas DQ. Magnitude of cone beam CT image artifacts related to zirconium and titanium implants: impact on image quality. Dentomaxillofacial Radiology. 2018, 47, 20180021. [Google Scholar] [CrossRef] [PubMed]
- Guglielmo FF, Wells ML, Bruining DH, Strate LL, Huete Á, Gupta A, Soto JA, Allen BC, Anderson MA, Brook OR, Gee MS. Gastrointestinal bleeding at CT angiography and CT enterography: imaging atlas and glossary of terms. Radiographics. 2021, 41, 1632–1656. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).