1. Introduction
Cardiac surgery procedures are among the main treatments for cardiovascular disease patients, recognized as a crucial health problem with increased morbidity [
1]. Dyspnea is a cardinal clinical feature of post cardiac surgery patients and it can be the result of all the most important post-surgical complications, whether they are cardiac or pulmonary related. Patients who undergo cardiac surgery often develop heart failure, which is a major cause of morbidity and mortality in this setting: more than 20% of patients are expected to have acute cardiovascular dysfunction in the perioperative period of cardiac surgery [
2,
3]. On the other hand, a recent prospective multicenter study in 43 cardiac surgery Centers in 9 Countries provided data on the incidence of postoperative pulmonary complications occurred in 55% of patients, including pleural effusion (32%), respiratory failure (21%), atelectasia (16%), respiratory infection (9%), pneumothorax (4%), broncospasm (1%) and aspiration pneumonitis (1%) [
4].
Cardiac rehabilitation (CR) is the setting of a multidisciplinary approach for post cardiac surgery patients. On top of the multidisciplinary intervention, one of the major goals of CR is to solve any problem left over by surgery or post-surgical intensive care which may be evident either at rest or during exercise [
5]. As the main instrumental examinations in the CR setting, post-operative transthoracic echocardiographic examination (TTE) may immediately identify the causes of cardiovascular failure, including cardiac and valvular dysfunction as a consequence of heart or surgical failure [
3]. Moreover, focusing on functional limitation and symptoms during effort, the cardiopulmonary exercise test (CPET) allows measurement of metabolic, cardiovascular, ventilatory and gas exchange responses to progressive exercise and it can be particularly informative to identify the different components of dyspnea [
6]. Finally, crucial is the precise knowledge of the surgical technique to lead to a targeted clinical-instrumental evaluation in case of abnormal persistence of post-operative symptoms.
2. Case Description
A white 52-years-old non-smoker female patient, affected by mitral valve prolapse (MVP) known from the age of 14 years, due to an episode of palpitation, underwent an unscheduled TTE, demonstrating a left ventricular (LV) dimension at the upper limits of normality, a preserved LV ejection fraction (EF 60%), a MVP leading to severe mitral regurgitation, a mild-to-moderate tricuspid regurgitation and a systolic pulmonary artery pressure of 37 mmHg.
After a coronary angiography demonstrating absence of atherosclerotic lesions, the patient underwent a MV valvuloplasty (Physio II ring n° 38 + neochord on posterior mitral leaflet scallop P2 + posterior mitral leaflet radial plication) and a tricuspid valve valvuloplasty (Contour ring n° 32) through median sternotomy and MV exposure according to Guiraudon approach [
7]. An intraoperative transesophageal echocardiographic examination (TEE) control confirmed good surgery results.
In the post-operative period, first in the Cardiac Surgery Department and then in Rehabilitation Unit, the patient was apiretic without clinical signs of heart failure. The blood pressure values and the electrocardiogram were normal, showing sinus rhytm and heart rate equal to 70 beats/minute. However, she complained a persistent dyspnea during minimal effort with evidence of mild hypoxemia at rest (at blood gas analysis in room air, pH 7.46, oxygen partial pressure (pO
2) 58 mmHg, carbon dioxide partial pressure (pCO
2) 28 mmHg, oxygen saturation (SpO
2) 90%) and a marked drop in SpO
2 during minimum effort. Normal blood chemistry tests, except for the usual anemia seen in post-operative phase, without significant inflammation indices elevation were assessed. Normal spirometry data were detected. A chest radiography, confirmed by a chest computerized tomography scan, showed normal lung parenchyma and minimal bilateral pleural effusion (a thin flap of right anterior pneumothorax resolved at a subsequent early check). An incremental CPET, performed on a cycle ergometer, was early discontinued at low oxygen consumption (VO
2) and workload, due to a severe and progressive dyspnea and hypoxemia (SpO
2 progressively dropping to 80%), showing ventilation to carbon dioxide relationship slope (VE/VCO
2) at the upper limit of normal values and abnormal decrease of end-tidal partial pressure of carbon dioxide (PETCO
2) at peak exercise [
8] (
Table 1 – CPET 1 column), suggesting intracardiac shunt.
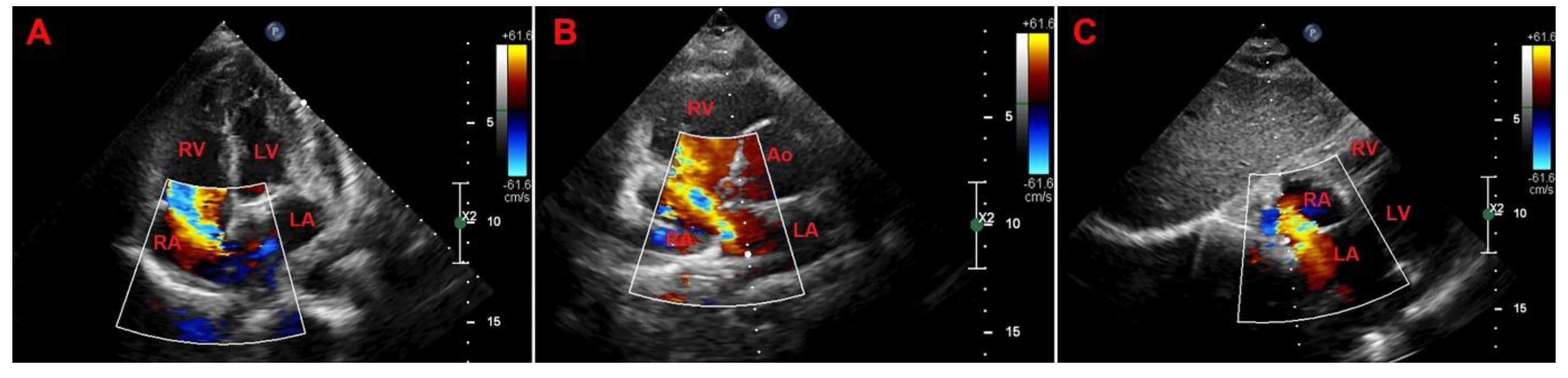
A TTE confirmed good surgical outcome showing mitral valvuloplasty with good leaflet dynamics with only minimal residual regurgitation and tricuspid valvuloplasty without residual regurgitation, normal LV with post-surgery septal dyskinesia, LVEF equal to 50%, normal atrial and right ventricle size with post-operative reduction of systolic longitudinal function and no pericardial effusion. Of note, TTE showed dilatation of inferior vena cava without collaps during breathing and a significant bi-directional shunt (left-to-right prevalent) due to a large ostium secundum type atrial septal defect (ASD)(diameter = 15 mm) with ratio between pulmonary (Qp) and systemic flow (Qs) equal to 1.5 in basal conditions (
Figure 1).
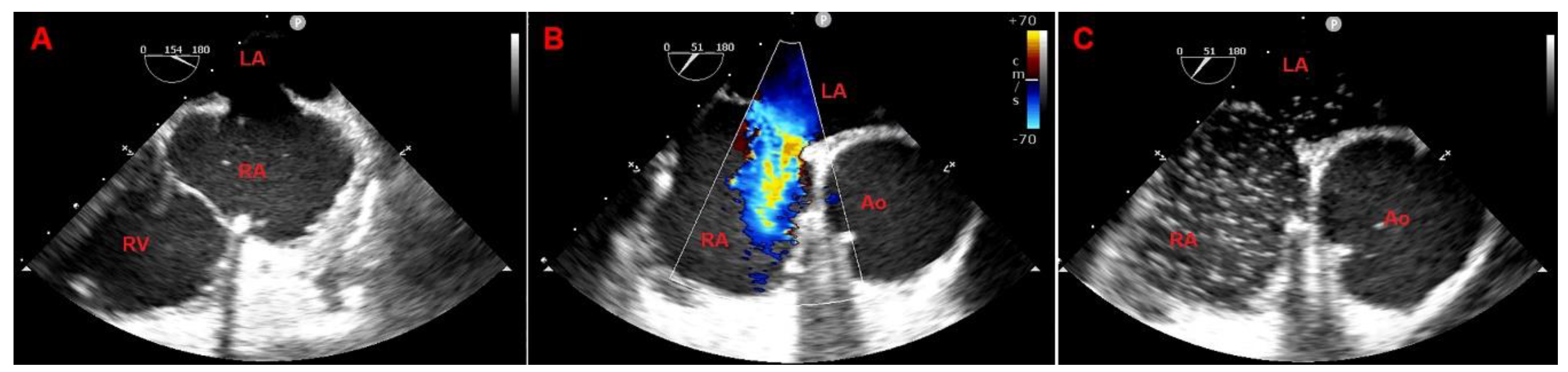
A following TEE confirmed the large ostium secundum type ASD (diameter = 15 mm; aortic rim 3 mm, posterior rim 11 mm, superior rim 12 mm, inferior rim 16 mm), leading to significant bi-directional shunt (left-to-right prevalent at color Doppler and right-to-left after saline infusion mixed with air (>25 microbubbles)), good mitral annulovalvuloplasty outcome (transmitral medium gradient = 2.6 mmHg) with mild-to-moderate residual central jet mitral regurgitation, good tricuspid annuloplasty outcome without evidence of residual tricuspid regurgitation (
Figure 2).
In agreement with cardiac surgeons, the patient underwent a second cardiac surgery through median sternotomy, during which a large opening of the interatrial septum due to the rupture of the suture thread was corrected.
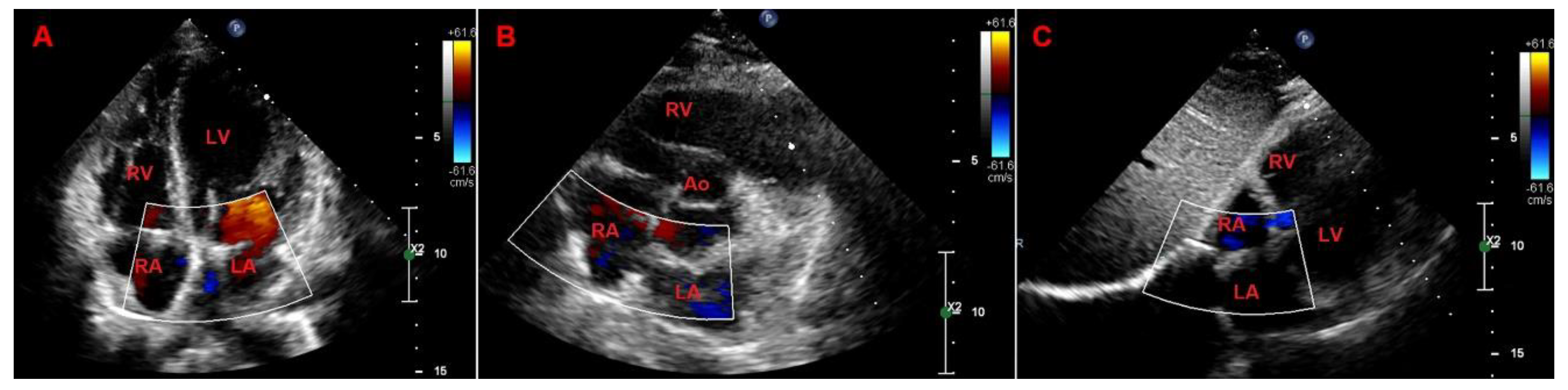
The post-operative phase was regular. The TTE showed a good outcome of mitral and tricuspid valve repair and a stable closure of the atrial septum (even when tested with microbubbles) (
Figure 3).
An incremental CPET was repeated to assess significant improvement of functional capacity without oxygen desaturation during effort and normal VE/VCO
2 and PETCO
2 during exercise (
Table 1).
The patient was finally discharged in subjective well-being.
3. Discussion
This case report describes an unusual cause of post cardiac surgery dyspnea and oxygen desaturation during effort.
Some important points emerged from this case:
- -
CR setting is an essential phase for the detection, the evaluation and the resolution of late post surgery complications
- -
second-level instrumental insights, namely experts performed TTE, TEE and CPET, are crucial to address and to resolve unusual post-surgery symptoms (the formers to find out anatomical defects and the latter to detect pathological gas exchange response to exercise)
- -
the detailed knowledge of surgical techniques can guide the diagnostic and therapeutic process in case of post-surgery symptoms.
CR Centers are recommended as the setting to provide multidisciplinary evidence-based secondary prevention therapies with supervised exercise training after cardiac surgery. The goals of CR are to optimize the recovery after a cardiovascular procedure, the functional capacity, the cardiovascular and psychological health and the quality of life. On enrollment, patients undergo a clinical and instrumental evaluation carried out by a trained and multidisciplinary CR team, leading to an in-depth evaluation and management of possible post-surgical complications [
5]. The possibility of an extended multidisciplinary clinical monitoring with second-level technologies in expert hands has allowed the recognition, the diagnosis and finally the referral to surgical treatment of the patient protagonist of the case report described.
In 1991 Guiraudon et al. published a paper about an extended vertical transatrial septal approach to either replacement or repair of the mitral valve apparatus [
7]. The “classical” approach is a left atrial incision within the right interatrial sulcus through a median sternotomy. According to the technique proposed by Guiraudon, the right atrium is opened longitudinally along the anterior segment of the atrioventricular fat pad and an extended vertical transseptal approach to the mitral valve is completed by a 1 to 2 cm vertical atrial septal incision through the fossa ovale (see Guiraudon’s paper for more surgical details). Atriotomies are finally closed using 3-0 monofilament running sutures starting at the lower end upward. Guiraudon’s technique was proposed to avoid distortion of the mitral valve apparatus and impairment of atrial functional anatomy. 34 consecutive patients (18 women and 16 men; age ranged from 26 to 79 years) treated using the extended vertical transseptal atrial approach were reported without bleeding or postoperative dehiscence such as an ASD. However, the latter could be a possible post-surgery complication of Guiraudon’s technique, crucial to keep in mind in these patients to correctly evaluate the post-surgical symptoms.
The interatrial septum is defined as a partition interposed between right and left atrium; the puncturing or the dissection of the interatrial septum could create a direct communication between the two atria. TTE is the primary means of establishing the diagnosis of an ASD. The role of imaging is to establish type, size and hemodynamic consequences including shunt direction, right heart volumes and function and pulmonary pressure. The ASD is classified in different types according to the seat of the defect: secundum ASD (located within the borders of the fossa ovalis), primum ASD (located near the origin of the tricuspid and mitral valve), sinus venosus ASD (located near the entry of the superior or inferior vena cava) and unroofed coronary sinus ASD (a communication between the left and the right atrium through the ostium of the coronary sinus) [
9]. In ostium secundum type ASD, it is possible to distinguish until 6 distinct rims listed in a clockwise direction: superior vena cava rim, aortic (anterior) rim, atrioventricular rim, inferior (vena cava) rim, posterior (posteroinferior and posterosuperior) rim. Multiple echocardiographic views are used to assess the presence and location of ASD and the hemodynamic impact of shunt. In the apical four-chamber views, since the atrial septum is parallel to the ultrasound beam, the central section of the atrial septum appears thin leading to false diagnosis of ASD. Therefore, a subcostal view including color flow mapping and/or pulsed Doppler, should be scrutinized for evidence of ASD. On TEE, at least three canonical views should be used to visualize ASD: mid-esophageal 4-chamber view, short axis at the aortic valve view at 60° and bi-caval view at 90° to 120° [
10,
11]. The magnitude and the direction of the shunt flow through an ASD is multifactorial and mainly depends by the size of the defect and the relative diastolic filling properties of the left and right ventricle. A reduction of the LV compliance may increase the left-to-right shunt while an impairment of the right ventricle function may reduce left-to right shunt or even cause a right-to-left shunt. Moreover, the identification of right-to-left shunt may need a saline contrast study. Several grading systems have been developed based on the number of bubbles crossing over the ASD, one of them is as follows: grade 1:<5 bubbles, grade 2: 5 to 25 bubbles, grade 3: >25 bubbles, grade 4 opacification of chamber. Finally, for suspected shunt lesions, TTE uses the ratio of the pulmonary to systemic shunt volume (Qp/Qs) as an established method to assess the hemodynamically significant shunting, usually referred to a net left-to-right shunting >1.5:1 and leads to right ventricle volume overload [
12]. For what has been wrote above and concerning the case reported, it is evident that a “surgical technique guided” and “expert performed” TTE and TEE are crucial for a correct and complete diagnosis of post-surgery uncommon outcomes.
CPET has been established for many years to help to identify causes and severity of functional limitation and dyspnea. The exercise, using with work becoming incrementally harder, is performed on a treadmill or bycicle ergometer. During rest, exercise and recovery the patient breathes through a mouthpiece or a mask, where oxygen consumption and carbon dioxide production, as well as flow at the mouth, are measured and other variables calculated. The principal parameter, peak VO
2, is the amount of oxygen consumed at peak exercise and it is used as the gold standard to quantify the functional capacity and/or exercise limitation. The number of liters of air breathed (VE) required to eliminate 1 liter of CO
2 is the ventilatory efficiency and it increases as dead space or ventilatory efficiency worsens. The PETCO
2 is used for non-invasive estimate of the arterial CO
2 pressure and it derives from muscle metabolism (amount of CO
2 production), from the respiratory rate and from the CO
2 chemoreceptor set point [
8]. Among several purposes, CPET can also be used to diagnose a cardiac shunt [
13]. Specifically, the reversal of the shunt potentially occurred during exercise and when right-to-left shunt occurs, a deoxygenated and CO
2-rich blood diverts to the systemic circulation, leading to a decrease of SpO
2 and simultaneous increase of VCO
2. The chemoreceptor activation and hyperventilation induced to compensate for the amount of CO
2 coming from the right sections of the heart lead to an abnormal decrease in P
ETCO
2 during exercise [
14,
15]. In our case report, CPET showed an early interruption of exercise due to significant reduction of SpO
2 with VE/VCO
2 at the upper limit of the normal values and concomitant abnormal decrease of P
ETCO
2, suggesting a right-to-left shunting through an ASD. Moreover, CPET was important to assess the significant performance improvement without oxygen desaturation during effort after ASD correction.
4. Conclusions
Dyspnea and oxygen desaturation at rest and during exercise are frequent after cardiac surgery with the need of a multiparametric approach. This clinical case report demonstrated the crucial role of “experts performed” and “surgery technique guided” instrumental insights in this common challenge.
Author Contributions
conceptualization, SDM, GC and AS; validation, GC, SDM, AS, CB and BB; writing—original draft preparation, SDM, GC and AS; writing—review and editing, CB, BB, AS, AS, RC, MB. All authors have read and agreed to the published version of the manuscript.”.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| TTE |
transthoracic echocardiogram |
| CPET |
cardiopulmonary exercise test |
| CR |
cardiac rehabilitation |
MVP
LV |
mitral valve prolapse
left ventricular |
| EF |
ejection fraction |
| TEE |
transesophageal echocardiogram |
pO2
pCO2
SpO2 |
oxygen partial pressure
carbon dioxide partial pressure
oxygen saturation |
VO2
VCO2
VE
RER
VE/VCO2 |
oxygen consumption
carbone dioxide production
ventilation
respiratory exchange ratio
ventilation to carbon dioxide ratio |
| PETCO2 |
end-tidal partial pressure of carbon dioxide |
Qp:Qs
ASD |
ratio between pulmonary and systemic flow
atrial septal defect |
References
- Sanders J, Cooper J, Mythen MG, Montgomery HE. Predictors of total morbidity burden on days 3, 5 and 8 after cardiac surgery. Perioper Med (Lond). 2017 Feb 14;6:2. [CrossRef] [PubMed] [PubMed Central]
- Lomivorotov VV, Efremov SM, Kirov MY, Fominskiy EV, Karaskov AM. Low-Cardiac-Output Syndrome After Cardiac Surgery. J Cardiothorac Vasc Anesth. 2017 Feb;31(1):291-308. Epub 2016 Jul 29. [CrossRef] [PubMed]
- Mebazaa A, Pitsis AA, Rudiger A, Toller W, Longrois D, Ricksten SE, Bobek I, De Hert S, Wieselthaler G, Schirmer U, von Segesser LK, Sander M, Poldermans D, Ranucci M, Karpati PC, Wouters P, Seeberger M, Schmid ER, Weder W, Follath F. Clinical review: practical recommendations on the management of perioperative heart failure in cardiac surgery. Crit Care. 2010;14(2):201. Epub 2010 Apr 28. [CrossRef] [PubMed] [PubMed Central]
- Fischer MO, Brotons F, Briant AR, Suehiro K, Gozdzik W, Sponholz C, Kirkeby-Garstad I, Joosten A, Nigro Neto C, Kunstyr J, Parienti JJ, Abou-Arab O, Ouattara A; VENICE study group. Postoperative Pulmonary Complications After Cardiac Surgery: The VENICE International Cohort Study. J Cardiothorac Vasc Anesth. 2022 Aug;36(8 Pt A):2344-2351. Epub 2021 Dec 25. [CrossRef] [PubMed]
- Thomas, RJ. Cardiac Rehabilitation - Challenges, Advances, and the Road Ahead. N Engl J Med. 2024 Feb 29;390(9):830-841. [CrossRef] [PubMed]
- Mezzani A, Agostoni P, Cohen-Solal A, Corrà U, Jegier A, Kouidi E, Mazic S, Meurin P, Piepoli M, Simon A, Laethem CV, Vanhees L. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2009 Jun;16(3):249-67. [CrossRef] [PubMed]
- Guiraudon GM, Ofiesh JG, Kaushik R. Extended vertical transatrial septal approach to the mitral valve. Ann Thorac Surg. 1991 Nov;52(5):1058-60; discussion 1060-2. [CrossRef] [PubMed]
- Bussotti M, Magrì D, Previtali E, Farina S, Torri A, Matturri M, Agostoni P. End-tidal pressure of CO2 and exercise performance in healthy subjects. Eur J Appl Physiol. 2008 Aug;103(6):727-32. Epub 2008 Jun 3. [CrossRef] [PubMed]
- Faletra FF, Saric M, Saw J, Lempereur M, Hanke T, Vannan MA. Imaging for Patient's Selection and Guidance of LAA and ASD Percutaneous and Surgical Closure. JACC Cardiovasc Imaging. 2021 Jan;14(1):3-21. Epub 2020 Jul 15. [CrossRef] [PubMed]
- Rigatelli G, Zuin M. Differences and similarities in interatrial shunts management. Eur J Intern Med. 2024 Feb;120:25-28. Epub 2023 Dec 10. [CrossRef] [PubMed]
- Kheiwa A, Hari P, Madabhushi P, Varadarajan P. Patent foramen ovale and atrial septal defect. Echocardiography 2020; 37: 2172-2184. [CrossRef]
- Rao, PS. Role of Echocardiography in the Diagnosis and Interventional Management of Atrial Septal Defects. Diagnostics (Basel). 2022 Jun 18;12(6):1494. [CrossRef] [PubMed] [PubMed Central]
- Barron AJ, Wensel R, Francis DP, Malik I. The role for cardiopulmonary exercise testing in patients with atrial septal defects: a review. Int J Cardiol 2012; 161: 68-72. [CrossRef]
- Crispino SP, Segreti A, La Porta Y, Liporace P, Carpenito M, Cammalleri V, Grigioni F. A sudden right-to-left shunt: the importance of evaluating patent foramen ovale during exercise. Monaldi Arch Chest Dis. 2023 Mar 7;94(1). [CrossRef] [PubMed]
- Sun XG, Hansen JE, Oudiz RJ, Wasserman K. Gas exchange detection of exercise-induced right-to-left shunt in patients with primary pulmonary hypertension. Circulation. 2002 Jan 1;105(1):54-60. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).