Submitted:
14 March 2025
Posted:
18 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
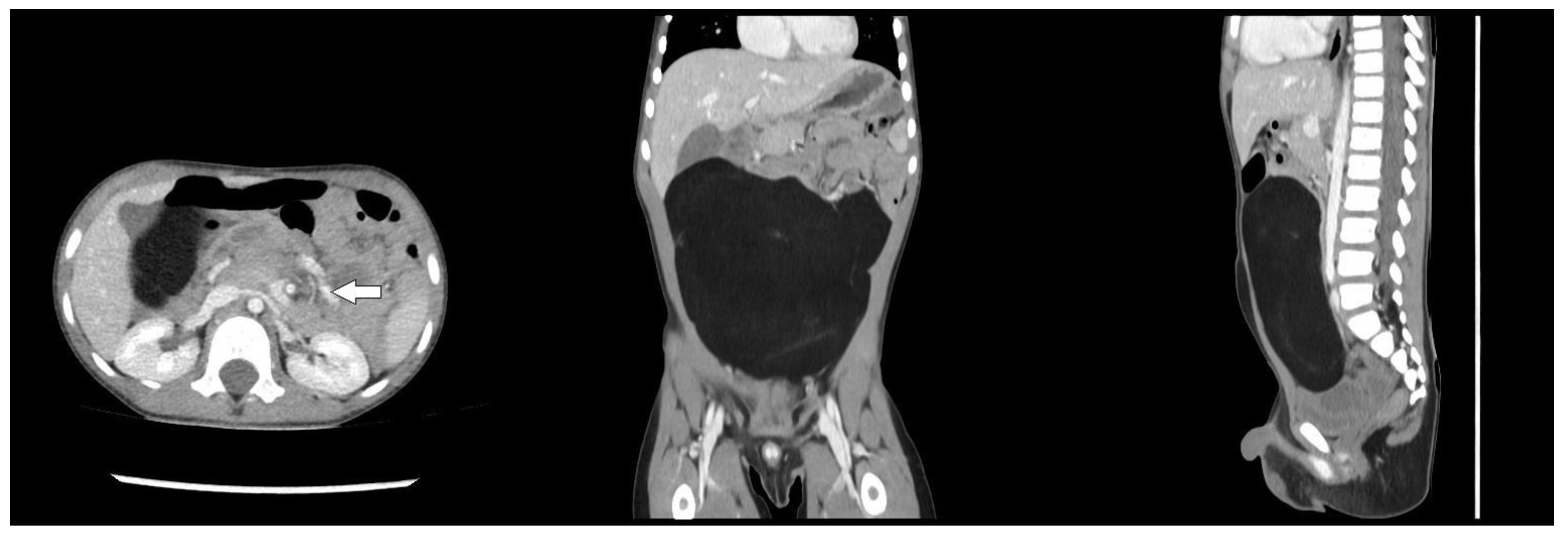
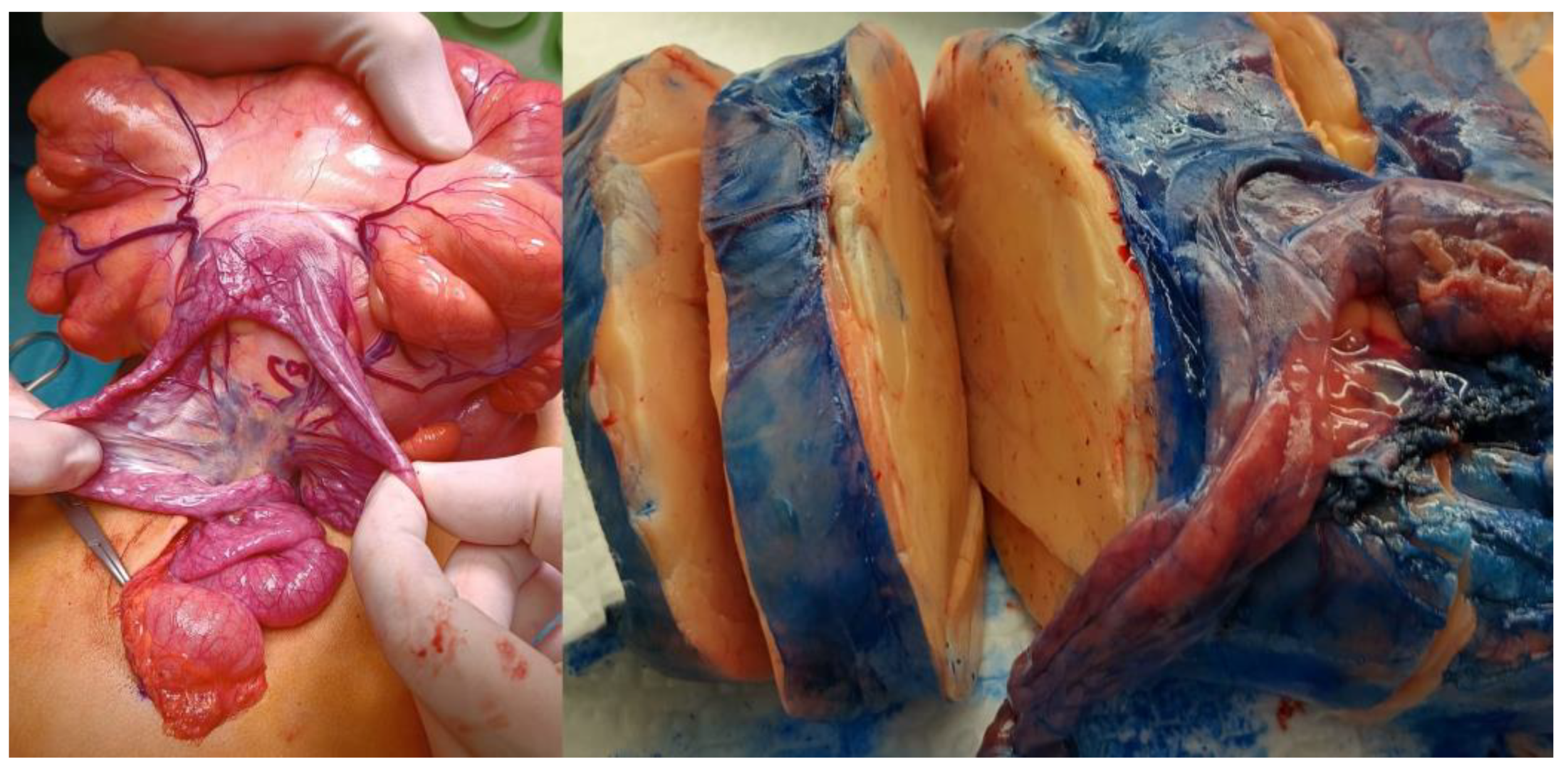
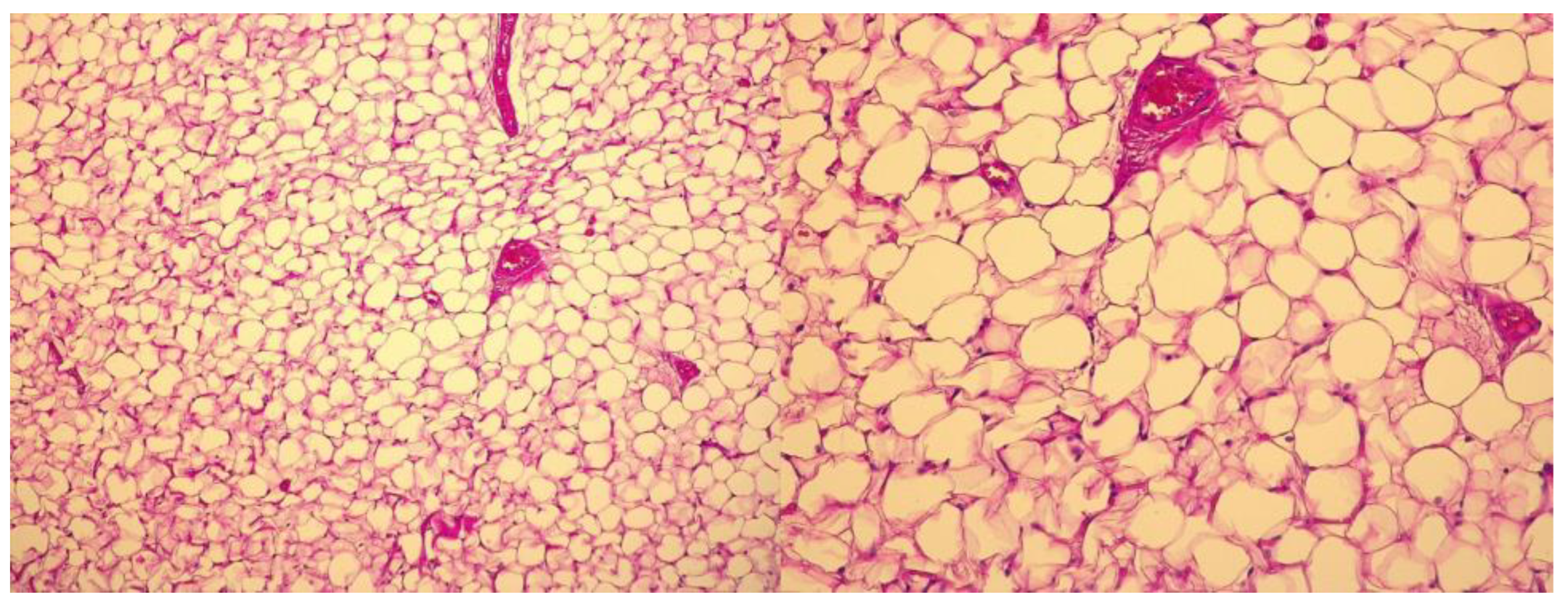
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflict of Interests
References
- Öztaş, T.; Asena, M. Mesenteric lipoma in a child: A case report. Pediatr. Acad. Case Rep. 2023, 2, 53–55. [CrossRef]
- Rwomurushaka, E.S.; Amsi, P.; Lodhia, J. Giant mesenteric lipoma in a pre-school child: a case report. J. Surg. Case Rep. 2024, 2024, rjae698. [CrossRef]
- Hashizume, N.; Aiko, T.; Fukahori, S.; Ishii, S.; Saikusa, N.; Koga, Y.; Higashidate, N.; Sakamoto, S.; Tsuruhisa, S.; Nakahara, H.; et al. Benign mesenteric lipomatous tumor in a child: a case report and literature review. Surg. Case Rep. 2020, 6, 1–6. [CrossRef]
- Azhar, M.; Zamir, N.; Jabbar, A. Giant Mesenteric Lipoma- A Rare Tumour Of Paediatric Age. J Ayub Med Coll Abbottabad. 2021, 33, 339-340.
- Ilhan, H.; Tokar, B.; Is̆iksoy, S.; Koku, N.; Pasaoglu, Ö. Giant mesenteric lipoma. J. Pediatr. Surg. 1999, 34, 639–640. [CrossRef]
- Tayeh, C.; Mneimneh, S.; El-Masri, R.; Daoud, N.; Rajab, M. Giant mesenteric lipoma: A case report and a review of the literature. J. Pediatr. Surg. Case Rep. 2015, 3, 166–170. [CrossRef]
- Malik, H.; Mirza, B.; Talat, N.; Zia, W.; Manzoor, A. Mesenteric Lipoma with Volvulus: A Rare Cause of Acute Abdomen in a Child. J. Coll. Physicians Surg. Pak. 2020, 30, 650–651. [CrossRef]
- Prince, T.C.; Shaffner, L.D. Mesenteric Lipoma in Children. Ann. Surg. 1956, 144, 913–914. [CrossRef]
- Kaniklides, C.; Frykberg, T.; Lundkvist, K. Paediatric Mesenteric Lipoma, An Unusual Cause of Repeated Abdominal Pain. Acta Radiol. 1998, 39, 695–697. [CrossRef]
- D, H.; B, R.; A, E.B.; Z, A.; M, K. The Mesenteric Lipoma in Children. Res. Pediatr. Neonatol. 2021, 5, 444–446. [CrossRef]
- Turk, E.; Edirne, Y.; Karaca, F.; Memetoglu, M.E.; Unal, E.; Ermumcu, O. A Rare Cause of Childhood Ileus: Giant Mesenteric Lipoma and a Review of the Literature. Eurasian J. Med. 2013, 45, 222–225. [CrossRef]
- Ozel, S.K.; Apak, S.; Ozercan, I.H.; Kazez, A. Giant Mesenteric Lipoma as a Rare Cause of Ileus in a Child: Report of a Case. Surg. Today 2004, 34, 470–472. [CrossRef]
- Maree, G.; Gawrieh, B.; Omran, A.; Ali, W. A rare lipoma site in a 1-year-old boy. J. Surg. Case Rep. 2021, 2021, rjab447. [CrossRef]
- Laguna, B.A.; Iyer, R.S.; Rudzinski, E.R.; Roybal, J.L.; Stanescu, A.L. Torsion of a giant mesocolic lipoma in a child with Bannayan-Riley-Ruvalcaba syndrome. Pediatr. Radiol. 2014, 45, 449–452. [CrossRef]
- Wolko, J.D.; Rosenfeld, D.L.; Lazar, M.J.; Underberg-Davis, S.J. Torsion of a giant mesenteric lipoma. Pediatr. Radiol. 2003, 33, 34–36. [CrossRef]
- Prando, A.; Wallace, S.; Marins, J.L.C.; Pereira, R.M.; de Oliveira, E.R.; Alvarenga, M. Sonographic features of benign intraperitoneal lipomatous tumors in children-report of 4 cases. Pediatr. Radiol. 1990, 20, 571–574. [CrossRef]
- Hamidi, H.; Rasouly, N.; Khpalwak, H.; Malikzai, M.O.; Faizi, A.R.; Hoshang, M.M.S.; Maroof, S.; Nasery, M.N.; Farzam, F.; Salehzai, M.; et al. Childhood giant omental and mesenteric lipoma. Radiol. Case Rep. 2016, 11, 41–44. [CrossRef]
- Selman, J.; Bender, J.R. Mesenteric Lipoma in a Child. Radiology 1948, 51, 66–70. [CrossRef]
- Gupta DK, Rohatgi M, Rao PS. Mesenteric lipoma. Indian Pediatr. 1988;25(10):1007-1009.
- Cherian, A.; Singh, S.J.; Broderick, N.; Zaitoun, A.M.; Kapila, L. Small bowel volvulus due to giant mesenteric lipoma. Pediatr. Surg. Int. 2004, 20, 869–871. [CrossRef]
- Kisra, M.; Ettayebi, F.; El Azzouzi, D.; Benhammou, M. Image of the Month—Answer. Arch. Surg. 2006, 141, 1046. [CrossRef]
- Srinivasan, K.; Gaikwad, A.; Ritesh, K.; Ushanandini, K. Giant omental and mesenteric lipoma in an infant. Afr. J. Paediatr. Surg. 2009, 6, 68–9. [CrossRef]
- Ahmed, I.; Singh, S.; Rawat, J.D. Chronic abdominal pain in a child. Saudi J. Gastroenterol. 2011, 17, 295–6. [CrossRef]
- Alireza R, Mohammad SS, Mehrzad M, Houman A. Midgut volvulus caused by mesenteric lipoma. Iran J Pediatr. 2013;23(1):121-123.
- Mozumder, M.R.; Afrin, R.; Biswas, T.; Haque, J.A.; Hoque, T.; Anjum, M.; Tofa, T.T. Mesenteric Lipoma in a Child- A Case Report. J. Dhaka Med Coll. 2024, 31, 258–263. [CrossRef]
- Garge, S.; Sharma, A.; Kelkar, H.; Jajodia, J. A Case of a Giant Mesentric Lipoma in a Two-year-old Child Presenting as Koch’s Abdomen. Apollo Med. 2024, 21, S11–S13. [CrossRef]
- Ogilvy, W.L.; Owen, H.F. Mesenteric lipoma in children. Can J Surg. 1960, 3, 344–6.
- Stransky E, Sevilla-Cabrera R. On a huge intraabdominal mesocolic lipoma in infancy. Ann Paediatr. 1962, 198, 24-34.
- Yang, C.; Wang, S.; Zhang, J.; Kong, X.R.; Zhao, Z.; Li, C.C. An unusual cause of paediatric abdominal pain: Mesenteric masses accompanied with volvulus. Turk. J. Gastroenterol. 2016, 27, 325–329. [CrossRef]
| Authors | Year | Age (months) | Sex | Comorbidities | Symptoms | Symptoms duration | Imaging | Tumor size (mm) | Tumor weight (gr) | Localization | Type of surgery | Intraoperative findings | Complications | LoS (days) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Selman J et al. (18) | 1947 | 48 | F | none | abdominal mass; nausea; vomiting | 4y | X-ray | NR | NR | ileum | laparotomy | NR | none | NR |
| Prince T C et al. (8) | 1956 | 10 | F | NR | abdominal mass | 3 m | X-ray | 200 | NR | ileum | laparotomy | NR | none | 7 |
| Gupta D K et al. (19) | 1988 | 14 | F | NR | NR | NR | NR | 150 | NR | ileum | NR | NR | NR | NR |
| Prando A et al. (16) | 1990 | 30 | M | NR | abdominal mass | NR | X-ray; US | 110x90x50 | NR | jejunum | NR | adherent to the wall of small bowel | NR | NR |
| Kaniklides C et al. (9) | 1998 | 132 | M | NR | abdominal pain; constipation | 8 y | X-ray; US; CT | 220x290x50 | 700 | mesentery | laparotomy | NR | NR | NR |
| Ilhan H et al. (5) | 1999 | 36 | M | none | abdominal distension | 6 m | US; CT | 310x230x120 | 2050 | mesentery | laparotomy | NR | none | 6 |
| Wolko J D et al. (15) | 2003 | 108 | M | Sorbital Intolerance | abdominal pain | 10 d | CT | 100x150 | NR | NR | NR | torsion of the lipoma; small bowel obstruction | none | NR |
| Ozel S K et al. (12) | 2004 | 84 | F | NR | abdominal pain; bilius vomiting | 4 d | X-ray; US; CT | 180x150x50 | NR | ileum | laparotomy | NR | NR | NR |
| Cherian A et al. (20) | 2004 | 168 | F | NR | abdominal pain; bilius vomiting | 8 h | X-ray | 160x150x75 | NR | ileum | laporoscopy; laparotomy | volvulus | none | 7 |
| Kisra M et al. (21) | 2006 | 168 | M | NR | NR | NR | NR | 124x68x110 | NR | ileum | NR | volvulus | NR | NR |
| Srinivasan K G et al. (22) | 2009 | 9 | NR | NR | abdominal distension; diarrhoea | 3 m | US; CT | NR | 1500 | omentum; mesentery; transverse colon | laparotomy | NR | NR | NR |
| Ahmed I et al. (23) | 2011 | 72 | M | none | abdominal pain; abdominal distension; constipation | 2 y | CT | NR | NR | ileum | laparotomy | NR | none | NR |
| Turk E et al. (11) | 2013 | 24 | F | none | abdominal pain, bilius vomiting | 24 h | X-ray; US | 160x150x80 | 770 | ileum | laparotomy | intestinal obstruction with necrosis | none | 5 |
| Alireza R et al. (24) | 2013 | 72 | F | NR | abdominal pain; nausea; vomiting | 2 d | X-ray; US; CT | 130x30x50 | NR | ileum | laparotomy | volvulus | none | NR |
| Tayeh C et al. (6) | 2015 | 24 | M | none | failure to thrive; abdominal distension | 1 y | X-ray; US | 220x190x90 | 1620 | ileum | laparotomy | NR | none | 6 |
| Laguna B A et al. (14) | 2015 | 72 | M | Bannayan-Riley-Ruvelbaca Syndrome | abdominal pain | 12 h | CT | 68x42x83 | NR | mesocolon | laparoscopy | torsion of the lipoma | NR | NR |
| Hamidi H et al. (17) | 2016 | 72 | F | NR | abdominal pain; abdominal distension | 4 y | US; CT | 280x240x100 | NR | NR | laparotomy | NR | none | NR |
| Hashizume N et al. (3) | 2020 | 36 | F | none | abdominal pain; abdominal distension | NR | US; CT; MRI | 80x60 | NR | ileum | laparotomy | NR | none | NR |
| Maree G et al. (13) | 2020 | 12 | M | NR | abdominal distension; diarrhoea | NR | US; CT | 90x110 | NR | jejunum | laparotomy | NR | none | 5 |
| Malik H et al. (7) | 2020 | 72 | F | NR | abdominal pain; vomiting; constipation | 24 h | X-ray | 100x80; 20x20 | NR | ileum | laparotomy | volvulus | none | NR |
| Azhar M et al. (4) | 2021 | 11 | M | none | abdominal distension; constipation; abdominal pain; vomiting | 4m | US; CT | 300x190x120 | NR | ileum | laparotomy | small bowel wrapped around tumor | none | 5 |
| Hanine D et al. (10) | 2021 | 60 | M | NR | abdominal pain | NR | X-ray; US; CT | NR | NR | ileum | laparotomy | NR | none | NR |
| Mozumder MR et al. (25) | 2022 | 96 | F | none | abdominal pain; vomiting | 1.5y | US; CT | 85x65x45 | 150 | ileum | laparotomy | NR | none | NR |
| Oztas T et al. (1) | 2023 | 48 | M | none | abdominal pain; vomiting | NR | X-ray; US; CT | 120x120x70 | NR | ileum | NR | volvulus | none | 6 |
| Rwomurushaka E S et al. (2) | 2024 | 36 | F | NR | abdominal distension; nausea | 1y | US; CT | 170x170x90 | NR | small bowel; mesentery | laparotomy | NR | none | 3 |
| Garge S et al. (26) | 2024 | 24 | M | NR | abdominal distension, abdominal pain, failure to thrive | 6 m | X-ray; US; CT | 150x60x100 | NR | ileum | laparotomy | NR | none | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





