1. Introduction
There is ample evidence nowadays that early enzymatic debridement of clinically deep second and third degree burns with NexoBrid
® (EDNX, MediWound, Yavne, Israel) is a valuable alternative to the surgical standard of care (SOC) consisting of early tangential excision for eschar removal [
1,
2,
3,
4,
5,
6]. Advantages over SOC include its selective burn eschar removal with associated tissue (and healing potential (HP)) preservation, diminished blood loss and, reduced time to complete debridement [
3,
5]. In addition, EDNX reduces the need for general anesthesia, surgery, and autografting as well as the rate of hypertrophic scarring (HTS) compared to the SOC [
3,
5,
6].
Circumferential deep burns pose a significant risk of burn-induced compartment syndrome (BICS). This is caused by the accumulation of interstitial fluid within confined anatomic spaces of the body mainly due to the systemic inflammatory response and fluid resuscitation. The excessive fluid causes the intracompartmental pressures (ICP) to increase, resulting in collapse of the contained vascular and lymphatic structures. This may compromise tissue viability and interfere with abdominal and/or respiratory function [
7]. Intra-abdominal pressure beyond 20mmHg [
8] and compartment pressures of >30mmHg [
9] are generally considered as an indication for immediate intervention. Classically, this is done with surgical escharotomies: longwise subcutaneous incisions through the burned area with extensions on both sides in the non-burned areas hereby releasing the mounting tissue pressure/tension and restore circulation [
10]. However, this approach carries a risk of damaging anatomical structures, bleeding and infection [
7].
Due to the aforementioned characteristics, EDNX can be a valuable alternative to surgical escharotomies in the prevention of BICS although the evidence for this is very limited especially for the thoracic, abdominal and lower limbs area. The statement of the European Consensus Documents that ‘the extremity should be monitored and surgical escharotomy and/or fasciotomy should be performed if signs of deterioration appear’ illustrated the uncertainties about the speed of eschar removal and the associated decrease in elevated pressures [
11].
This case series documents the patients with deep circumferential burns treated with early enzymatic debridement with NexoBrid® in our burn center. To the best of our knowledge, this is the first case series that aims to provide clinical evidence for safe and effective use of NexoBrid® in the prevention of BICS, not only in the upper extremities, but also in lower extremities, thoracic and abdominal regions.
2. Patients and Methods
Since January 2015, EDNX has been routinely used in our burn center for early, selective eschar removal of laser Doppler imaging (LDI, Moor Instruments, Axminster, UK)-blue confirmed deep burns [
6,
12]. However, in this case series, due to clinical signs of BICS, EDNX was used at a very early stage post burn (<24 hours) without prior burn depth assessment with LDI. These patients gave written and oral informed consent for publication of clinical data and images. The Ethical Review Committee of Ghent University hospital approved this single center retrospective database analysis (protocol nr. 2019/1535)
2.1. Rationale for EDNX in BICS Prevention
Given that BICS can progress rapidly and lead to irreversible damage, early intervention is crucial. Although NexoBrid® is primarily indicated for eschar removal, its potential role in BICS prevention remains an area of investigation. It has been suggested that early enzymatic debridement may facilitate tissue decompression, reducing interstitial pressure and preventing the progression of BICS. This study examines whether enzymatic debridement can serve as a timely decompressive strategy in such cases, particularly in various anatomical regions, including the thorax and lower extremities, where evidence remains limited.
This results in the following PICO:
- -
P (Population/Patient/Problem): Patients with circumferential full-thickness burns at risk of BICS.
- -
I (Intervention): Early enzymatic debridement using NexoBrid®.
- -
C (Comparison): Traditional surgical escharotomy.
- -
O (Outcome): Successful prevention of BICS, maintenance of respiratory function, and effective management of circumferential burns.
2.2. Therapeutic Protocol of the Ghent Burn Center Modified for Burn Induced Compartment Syndrome
2.2.1. Admission and Pre-NexoBrid® Procedure
Normally, all burn patients admitted to the burn center of the Ghent University Hospital are clinically assessed by a senior burn specialist using the standard clinical characteristics. As a general rule, an LDI scan is performed for all burn injuries, between 48h and 5 days post-burn, to obtain accurate (> 95%) burn depth assessment [
12,
13,
14,
15,
16,
17,
18]. Burn wounds with a HP>21d are represented by a blue color on the validated LDI color palette. These LDI-blue burn wounds are considered as a clear indication for tangential excision and skin grafting [
19,
20,
21], although in our burn center these wounds are usually debrided with NexoBrid
® [
12].
To prevent BICS, earlier (< 24h after the burn injury) EDNX treatment was required in our group of patients and therefore no LDI scan was performed. In general, for non-sedated patients, diagnosis of BICS is based largely on physical examination and six cardinal clinical manifestations, described as the six P's are 1) pain; 2) poikilothermia; 3) paresthesia; 4) paralysis; 5) pulselessness; and 6) pallor [
22]. The earliest indicator is severe pain while pulselessness, paresthesia, and complete paralysis are found in a late stage of BICS. Additionally, serial measurement of ICP could be helpful in confirming and determining progression of BICS, especially in sedated patients [
22]. Normal interstitial tissue pressure is around 15mmHg [
23]. In one case, a pressure assessment device used in arterial catheters for arterial pressure monitoring was connected to a central venous monitoring system. In another case pressure monitoring was available in the transurinary catheter.
2.2.2. NexoBrid® Procedure
All patients in this case series were in good general health, as assessed by the anesthesiologist or intensive care physician.
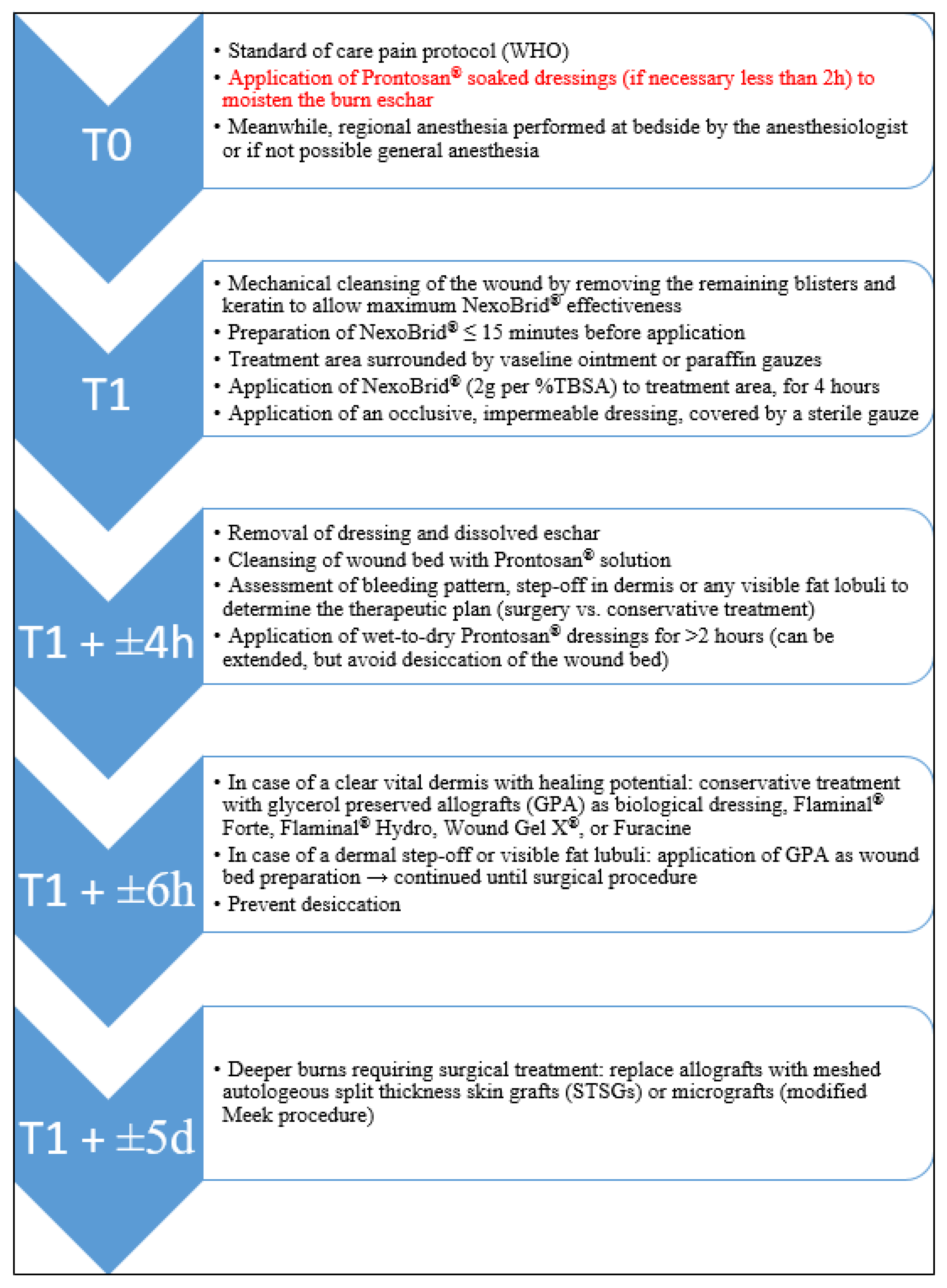
Our standard treatment protocol can be divided into different, time-dependent stages (
Figure 1) [
6]. For the exceptional emergencies described in this case series, some modifications were imposed. During the initial assessment and pain management phase (T0), the Prontosan
® soaked dressings were applied during the time needed to administer adequate regional or general anesthesia by the anesthesiologist, even if this was less than 2 hours. After this initial stage, wound cleansing and NexoBrid
® application was performed (T1). The treated areas were covered with an occlusive, impermeable dressing in a way that frequent observation (every 30 minutes) of the extremity was possible. These regular evaluations during the NexoBrid
® application are not performed in cases without BICS. After four hours the eschar is removed and the wound bed assessed to determine whether surgery or conservative management is appropriate (T1 + ±4 hours). A second assessment is made after two hours of soaking (T1 + ±6 hours). Any further surgical treatment for deeper burns will normally be done within a week (T1 + ±5 days).
2.3. Treatment Until Wound Healing.
After the EDNX procedure, wound management was based on a standard burn care protocol consisting of the application of glycerol-preserved allografts (GPA, Euro Skin Bank, The Netherlands), or of the enzyme alginogels Flaminal
® Forte or Hydro (Flen Health, Kontich, Belgium, Europe) [
24], or the hydrogel Prontosan
® Wound Gel X (B.Braun, Diegem, Belgium, Europe) up to the autografting procedure and/or wound closure (defined as closure of >95% of the involved surface area). The presence of BICS was monitored by examining swelling, tissue appearance, capillary refill and pulse oximeter every hour for the following 24 hours after the EDNX procedure. This paper recommended evaluating the wound bed twice: immediately after removing NexoBrid
® to assess wound bed viability and after the wet-to-dry (WTD) period to make a more complete decision. During these evaluations, wound bed characteristics such as incomplete debridement, visible and/or translucent fat lobules, visible and/or coagulated blood vessels and a dermal step-off in the wound bed combined with a higher range (4-5) in the newly developed wound bed color code, should result in an early and reliable decision for skin grafting [
12].
2.2.4. Eligibility Criteria for the NexoBrid® Procedure and This Case Series
In general, exclusion criteria for NexoBrid® application are a) electrical or chemical burns, b) pregnancy or nursing, c) history of allergy and/or known sensitivity to pineapples, papaya, bromelain or papain, d) patient or the legal representative refused to sign the informed consent form for enzymatic debridement.
For this case series, patients who did not have an enzymatic debridement under general or regional anaesthesia, but who had the SOC with escharotomy to avoid BICS, were excluded.
2.3. Data Collection
We selected all patients who had clinically apparent BICS in different anatomical locations from our secured electronic datasheet. The datasheet was anonymized and collected by the burn surgeons (LR, SM and KC) and the burn care coordinator (HH) and consists of: 1. age, height and weight of the patient, 2. date, cause, location, depth, and extent of the burn, 3. date of the EDNX procedure, 4. need for additional surgical procedures, 5. date of wound closure, 6. data of scar aftercare: pressure garments, hydration therapy with moisturizers and additional (surgical) procedures,… and, 7. date of the last clinical evaluation of the patient.
3. Results
This case series includes four well-documented patients where, due to clinical signs of BICS, EDNX was used in different anatomical locations at a very early stage post burn (<24 hours).
3.1. Case 1: Bilateral Circular Wrist and Hand Burns
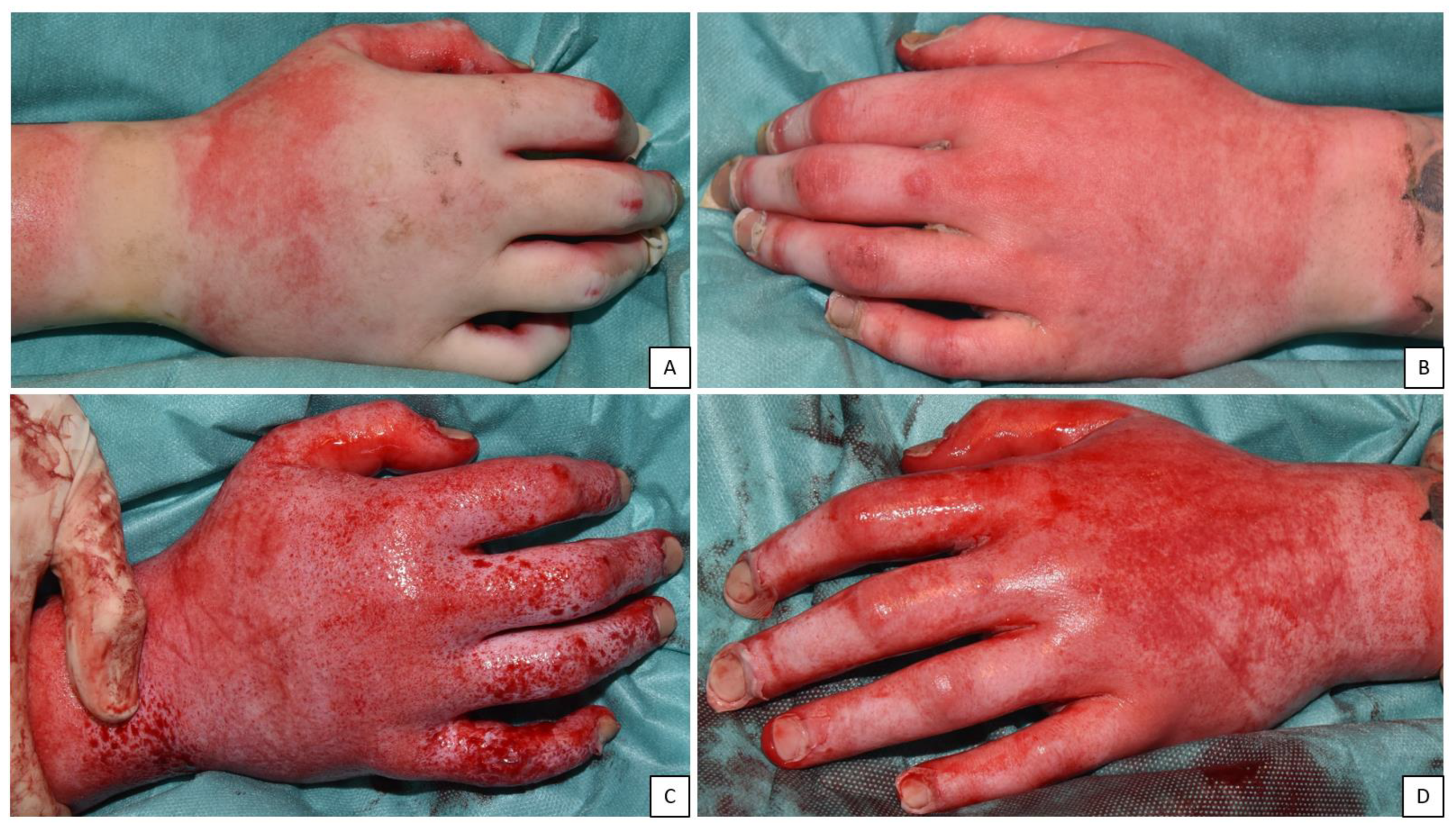
A 33-year-old male accidentally burned himself with hot oil resulting in 11.5% total burn surface area (TBSA) deep second and third degree burns to his face, the dorsum of his hands and the complete circumference of both his wrists. Swelling around the mouth and larynx urged immediate intubation. While the patient was being stabilized during admission in our burn center, increased swelling and tension of his hands in addition to a delayed capillary refill in the non-burned areas of his hands - indicating BICS - were observed (
Figure 2 a), b) and c)). Our modified NexoBrid
® treatment protocol was initiated immediately. Ten grams of NexoBrid
® was used to enzymatically debride both wrist and hand areas. Capillary refill normalized within the first hour of EDNX application. Both his hands remained swollen, yet the tension on his skin during clinical examination diminished significantly (
Figure 2 d), e), and f)). The wound bed after NexoBrid
® removal showed a dermal step-off and translucent fat. No additional surgical escharotomies were necessary and all wounds were eventually covered with allografts. No EDNX-related adverse events were reported during or after the procedure.
One week after the EDNX procedure, the allografts were removed and due to the wound bed characteristics identified, the remaining wounds had to be covered with split thickness skin grafts (STSG). Wound closure was complete 3 weeks post burn (
Figure 3 a), b) and c)). After the swelling of both hands disappeared, their function recovered completely. Both wrists and all the fingers had normal ROM and no paresthesia’s were noted. The patient developed severe hypertrophic scars on both his hands 6 months post burn injury (
Figure 3 d)). These resolved with hydration therapy and pressure garments combined with polyurethane pelottes (at least 30 mmHg) which are all part of our standard adjuvant burn scar treatment protocol. The patient is still in active follow-up (currently four years) (
Figure 3 e)).
3.2. Case 2: Bilateral Arm and Circular Wrist and Hand Burns.
A 21-year-old male was victim of flame burns due to an explosion at work. He suffered 18.5% TBSA deep second and third degree burns to his face, both wrists (circumferential) and hands (circumferential), his lower back and multiple spots on his legs and arms (
Figure 4 a) and b)). After immediate intubation on site he was transferred to our burn unit. His hands and wrists were completely burned which complicated clinical examination for BICS. A consistent increase in swelling of both hands, particularly the right side, with delayed capillary refill of the nail beds - compatible with BICS - urged us to perform enzymatic debridement according to protocol. The burns to his face, lower back and legs were treated with in total 20g NexoBrid
® simultaneously with his wrists and hands without exceeding the recommend 15% TBSA treated. No additional surgical escharotomies were necessary as the swelling of both wrists and hands was significantly reduced at the end of the procedure (
Figure 4 c) and d)). Only the index fingers III, IV and V of the right hand showed signs of translucent fat, suggesting the need for autografting. All other areas treated had wound bed characteristics compatible with spontaneous healing under conservative therapy. No EDNX-related adverse events were reported during or after the procedure.
The left hand healed within 3 weeks with conservative treatment, while part of the right hand (index fingers III, IV and V) was covered with STSGs. The right hand needed 45 days until complete healing (
Figure 5 a) and b)). The patient received standard hydration therapy and wore pressure garments for two consecutive years. Functionality of hand and fingers returned to normal except for a contracture on the fifth finger of the right hand for which the patient still receives physiotherapy. He is still in active follow-up (three years) at our department (
Figure 5 c) and d)).
3.3. Case 3: Unilateral, Circular Lower Leg Burn
A 32-year-old male patient was transferred to our burn unit due to an 8.4% TBSA, circumferential, third degree flame burn on his right lower leg. On admission, his foot and toes on the right side showed signs of venous congestion, were cold and had a delayed capillary refill (
Figure 6 a) and b)). A weak Doppler signal was found on both his tibialis posterior and dorsalis pedis artery. Our standard NexoBrid
® treatment protocol under epidural anesthesia was started immediately after admission. Pressure measurements prior to NexoBrid
® application showed pressures around 60 mmHg in the anterior, lateral and superficial posterior compartment of the lower leg indicating the need of urgent decompression. A total amount of 10g NexoBrid
® was used for debridement of a 1122 cm2 surface area. Intermediate inspection of the toes showed restored color and temperature within one hour after NexoBrid
® application. On removal of NexoBrid
® after four hours, the burns were completely debrided. Subcutaneous fat, nerves and superficial blood vessels were exposed (
Figure 6 c) and d)). Intra-compartment pressures recovered to 20-25 mmHg after the EDNX procedure.
No EDNX-related adverse events were reported during or after the procedure. Due to the wound bed characteristics (e.g. clear visible fat lobules, visible blood vessels), the patient was scheduled for additional debridement and definitive reconstruction with STSGs 5 days after NexoBrid
® application. Due to graft failure (70% of surface area), a second attempt at reconstruction with STSG was made 14 days later. Additional debridement at this stage led to exposure of the tibia, medial malleolus, peroneal and Achilles’ tendon urging free flap reconstruction (
Figure 7 a) and b)). On day 40 after admission, the remaining defects on the lower leg were reconstructed with a free anterolateral thigh (ALT) and superficial circumflex iliac artery perforator (SCIP) flap. Partial necrosis of both flaps was debrided 3 weeks post reconstruction and temporally covered with allografts and one week later the allografts were replaced with STSGs (
Figure 7 c) and d)). Besides some muscle weakness due to immobilization, the patient had no loss of range of motion (ROM) or sensibility issues. He started rehabilitation together with the standard aftercare treatment consisting of hydration, pressure and silicone therapy.
3.4. Case 4: Circular Thorax and Abdomen Burn
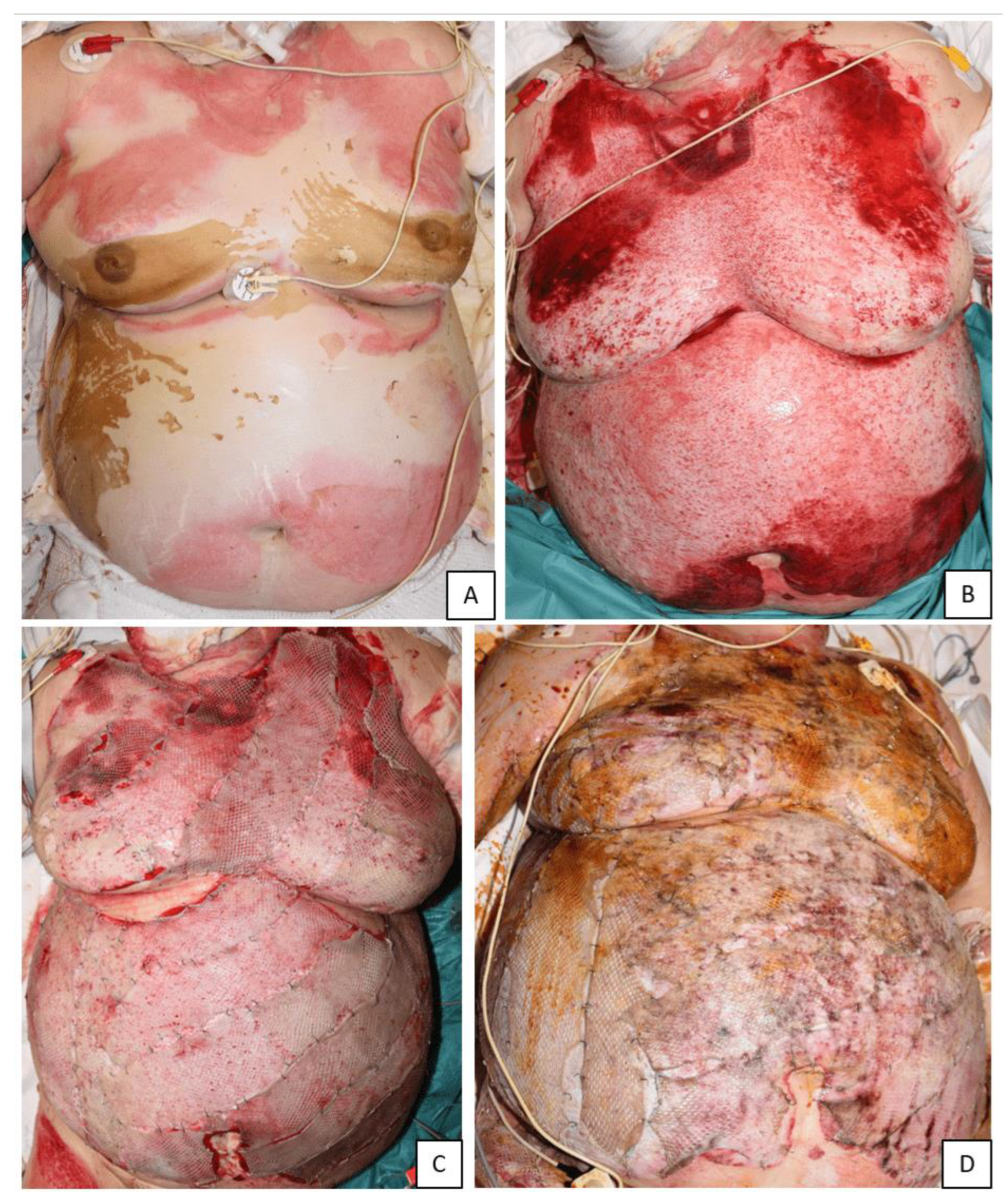
A 60-year-old female patient with a psychiatric history was transferred to our burn unit after she set herself on fire. She had third degree burns on her abdomen, thorax, face and neck. Those on the abdomen and thorax were circular (
Figure 8 a)). Additionally, there were deep second degree burns on her flanks, right upper leg, both her upper arms and left hand. Total %TBSA was estimated at 30.8%. Prior to transfer to our hospital, the patient was intubated in anticipation to suspected air way swelling secondary to inhalation trauma. After intubation there was an immediate need for high airway pressures. Initially with normal oxygen levels, but later followed by a steady increase in oxygen levels to obtain adequate ventilation. Additionally, intra-abdominal pressures rose to 21 mmHg. This urged the need for starting our NexoBrid
® treatment protocol. A total amount of 25g NexoBrid
® was used for debridement of 2720 cm2 surface. Already 30 minutes and 1 hours post application of NexoBrid
®, the intra-abdominal pressures dropped to 18 and 14 mmHg respectively. Intra-abdominal pressure after the procedure varied around 14 mmHg. The urinary output remained normal during the complete treatment period. The wound bed characteristics (translucent fat, visible fat, dermal step-off) showed signs for additional surgical treatment (
Figure 8 b)). All wounds were covered with allografts (
Figure 8 c)). Two days after the burn injury, the remaining burn wounds were scanned with LDI and the LDI-blue burns were treated with NexoBrid
®. High airway pressures in conjunction with high oxygen levels were necessary up to five days after the initial procedure. The patient had a known history of asthma. ENT examination and bronchoscopy showed no signs of severe inhalation trauma. These lasting high airway pressures were linked to the diagnosis of ventilation acquired pneumonia for which the patient was given IV antibiotics. No EDNX-related adverse events were reported during or after the procedure. Due to logistic reasons amid the covid-19 pandemic, the patient was transferred to another burn center on day 6 post NexoBrid
® (
Figure 8 d)). There, all wounds were reconstructed with STSGs according to the Meek technique before starting the rehabilitation trajectory.
4. Discussion
This case series aimed to provide clinical evidence for the safe and effective use of NexoBrid® in the prevention of BICS in all regions of the body. This is extremely important since increased interstitial pressure not only results in a BICS, but also exerts increasing tension on the surrounding, already injured skin, slowly obliterating its already compromised blood supply leading to the propagation and deepening of the original thermal burn.
The diagnosis of BICS is essentially clinical (6P’s). Recognizing an early BICS is a challenge for burn specialists as most of the clinical symptoms often appear late [
25], after the damage - at least at the skin level (burn depth progression)- has occurred, being masked by the normal burn-related symptoms [
26]. In our four cases, three patients were intubated and sedated, making the diagnosis even more difficult. BICS was primarily diagnosed based on the presence of edema, tension and reduced capillary refill (pulselessness), in the last two cases this was confirmed by ICP measurements.
The European Consensus Guidelines, first published in 2017, agreed on two statements regarding the use of NexoBrid
® in preventing BICS [
11]. The panel’s first statement was that ‘enzymatic debridement can be used for early eschar removal in circumferential extremity burns to prevent surgical escharotomy as standard of care but not to replace fasciotomy’. The other statement was that ‘the extremity should be monitored and surgical escharotomy and/or fasciotomy should be performed if signs of deterioration appear’. The first statement was confirmed by a panel of German-speaking EDNX experts based on the study of Fischer et al. [
7] investigating the use of NexoBrid
® for the prevention of surgical escharotomy in the upper limbs [
27]. Both guidelines were followed in the four patients treated in this case series. Fortunately, no deterioration was noted during the procedures, allowing us to avoid the use of surgical escharotomies. This is a major advantage of enzymatic debridement because this approach significantly reduces morbidity: 1) in areas where burn depth is difficult to assess selective enzymatic debridement avoids the lengthwise deep subcutaneous incisions; 2) this avoids the risk for neurovascular damage or the need for autografting this area while the other areas might heal under conservative therapy due to initial clinical overestimation of burn depth; 3) reduced blood loss and, 4) less scars. This reduced morbidity can be illustrated by the first two cases: in the first case, autografts could by placed on a reduced but still present dermal layer of both hands which might explain the excellent results obtained in the long term; in the second case the left hand healed under conservative therapy while only three fingers of the right needed autografting. Moreover, the very early removal of the dead eschar might contribute to the reduction of the eschar-induced inflammatory response and the resulting edema. The bromelain anti-inflammatory effect may also contribute to this phenomenon [
28].
Our burn center started using NexoBrid
® three years after its official approval in Europe. The reason that only four patients - where immediate enzymatic debridement was performed - were included in this case series is that we perform a LDI scan for almost all burn injuries to obtain accurate burn depth assessment which determines an efficient as well as cost-effective therapeutic plan [
12,
13,
14,
15]. This is in contrast to other articles where NexoBrid
® is already generally indiscriminately applied to all burn wounds and this also before 48 hours post burn which might result in overtreatment (e.g. application on superficial partial-thickness burns) and associated unnecessary costs [
1,
2,
3,
4,
5,
29,
30,
31]. In our burn center, NexoBrid
® is only applied several hours post burn in case of clinical manifestations of BICS [
22]. Similar to other papers [
1,
4,
9], in the last two cases, we used ICP to confirm and determine progression of BICS. In contrast to the study of Fischer and colleagues, who excluded patients with a clinically established compartment syndrome (paresthesia, deep tissue pain, pulselessness, compromised distal perfusion) and dry burns, our case series provides added value because all four cases included patients with established BICS and dry burns. All other studies on the use of EDNX for prevention of BICS focused on its application for burns in the upper extremities [
1,
4,
9]. Krieger et al reported reduced interstitial pressures (< 25 mmHg) after NexoBrid
® application in four patients (seven hands), eliminating the need for surgical escharotomies [
4]. Pre-debridement pressures ranged from 35 to as high as 75 mmHg. Schulz et al. added two extra cases (two hands) with reduced compartmental pressures after NexoBrid
® application (16 and 14 mmHg after versus 28 and 31 mmHg before EDNX application) [
1]. Also Mataro et al. claimed that early EDNX debridement can also resolve increased burn-induced interstitial-compartment pressure leading to BICS based on their results on 23 patients [
9]. This case series also showed reduced lower limb and abdominal ICP after NexoBrid
® application. In case 4, the effect on the patients’ respiratory function was less clear: although ventilation pressures could be reduced, the patient developed a pneumonia during admission.
When referring to our proposed PICO, this case series shows encouraging results as a starting point for further controlled trials.
The main argument against the use of EDNX for apparent BICS could be that the total duration of the EDNX protocol might interfere with the safe window before respiratory improvement or irreversible damage to nerves and muscles. Based on the animal study of Krieger et al.[
26], who showed a decrease in pressure within 30 minutes after EDNX application, the paper of Mataro and colleagues [
9] who showed an approximately 60% reduction of the ICP in most cases within 1 hour from EDNX and, and our own data, we believe that EDNX can decrease intra-compartment pressure 30 to 60 minutes after application. However, further research is needed to determine whether this timeframe is consistently adequate for preventing long-term ischemic damage. Pre-soaking should be limited to the time needed to achieve adequate regional or general anesthesia as this is, in our opinion, sufficient to have a sufficient moist burn eschar.
Contrary to most previous studies [
9] and as shown by an earlier study from our department [
6], regional or general anesthesia is always performed bedside at our burn unit. The use of regional or general anesthesia makes it impossible for the patient to report pain or paresthesia which may interfere with post-EDNX clinical follow-up of BICS. Standardized intra-compartment pressure measurements pre- and post-EDNX may be helpful during follow-up. Ideally, these measurements should be performed in any extremity with suspected BICS. These measurements require additional logistics and coordination between all health care providers involved. They also come with a learning curve for both the nurses and the physicians which, in the beginning, slows the standardized work-flow of the burn unit. However, the authors believe that these measurements can be performed in less than 10 minutes once the whole team is accustomed to the procedure. Intra-abdominal or airway pressures should also be documented and compared prior to and after EDNX treatment. Since these parameters are often monitored by the intensive care physician or anesthesiologist, good cooperation and communication between all teams is essential.
5. Conclusions
While surgical escharotomy remains the standard for BICS management, this case series provides preliminary evidence supporting early enzymatic debridement with NexoBrid® as a possible alternative in select cases. However, given the small number of cases, it is premature to conclude that EDNX is an immediate and definitive solution. Instead, these findings indicate that EDNX could be a safe and effective option for BICS prevention, warranting further investigation through larger clinical studies.
Author Contributions
All authors have made substantial contribution to: The conception and design of the study. Acquisition of data. Analysis and interpretation of data. Drafting the article. Revising the article critically for important intellectual content. Final approval of the version to be submitted. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Ghent University hospital (protocol nr. 2019/1535, date of approval 29/11/2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be shared on request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
ALT
BICS |
Anterolateral thigh
Burn induced compartment syndrome |
EDNX
GPA
HP
HTS
ICP
LDI
ROM
SCIP |
Enzymatic debridement with NexoBrid®
Glycerol-preserved allografts
Healing potential
Hypertrophic scarring
Intracompartmental pressures
Laser Doppler imaging
Range of motion
Superficial circumflex iliac artery perforator |
SOC
STSG
TBSA
WTD |
Standard of care
Split thickness skin grafts
Total burn surface area
Wet-to-dry |
| |
|
References
- Schulz A, Shoham Y, Rosenberg L, Rothermund I, Perbix W, Christian Fuchs P, et al. Enzymatic Versus Traditional Surgical Debridement of Severely Burned Hands: A Comparison of Selectivity, Efficacy, Healing Time, and Three-Month Scar Quality. Journal of burn care & research : official publication of the American Burn Association. 2017;38:e745-e55.
- Schulz A, Fuchs PC, Rothermundt I, Hoffmann A, Rosenberg L, Shoham Y, et al. Enzymatic debridement of deeply burned faces: Healing and early scarring based on tissue preservation compared to traditional surgical debridement. Burns : journal of the International Society for Burn Injuries. 2017;43:1233-43. [CrossRef]
- Rosenberg L, Krieger Y, Bogdanov-Berezovski A, Silberstein E, Shoham Y, Singer AJ. A novel rapid and selective enzymatic debridement agent for burn wound management: a multi-center RCT. Burns : journal of the International Society for Burn Injuries. 2014;40:466-74. [CrossRef]
- Krieger Y, Rubin G, Schulz A, Rosenberg N, Levi A, Singer AJ, et al. Bromelain-based enzymatic debridement and minimal invasive modality (mim) care of deeply burned hands. Annals of burns and fire disasters. 2017;30:198-204.
- Krieger Y, Bogdanov-Berezovsky A, Gurfinkel R, Silberstein E, Sagi A, Rosenberg L. Efficacy of enzymatic debridement of deeply burned hands. Burns : journal of the International Society for Burn Injuries. 2012;38:108-12.
- Claes KEY, Amar S, Hoeksema H, Kornhaber R, de Jong A, Monstrey S, et al. Pain management during a bromelain-based selective enzymatic debridement in paediatric and adult burn patients. Burns : journal of the International Society for Burn Injuries. 2021. [CrossRef]
- Fischer S, Haug V, Diehm Y, Rhodius P, Cordts T, Schmidt VJ, et al. Feasibility and safety of enzymatic debridement for the prevention of operative escharotomy in circumferential deep burns of the distal upper extremity. Surgery. 2019;165:1100-5. [CrossRef]
- Newman RK, Dayal N, Dominique E. Abdominal Compartment Syndrome. StatPearls. Treasure Island (FL)2022.
- Mataro I, Lanza A, Di Franco S, Di Franco L, Sangiuolo M, Notaro M, et al. Releasing Burn-Induced Compartment Syndrome by Enzymatic Escharotomy-Debridement: A Case Study. Journal of burn care & research : official publication of the American Burn Association. 2020;41:1097-103. [CrossRef]
- Saffle JR, Zeluff GR, Warden GD. Intramuscular pressure in the burned arm: measurement and response to escharotomy. American journal of surgery. 1980;140:825-31.
- Hirche C, Citterio A, Hoeksema H, Koller J, Lehner M, Martinez JR, et al. Eschar removal by bromelain based enzymatic debridement (Nexobrid((R))) in burns: An European consensus. Burns : journal of the International Society for Burn Injuries. 2017;43:1640-53. [CrossRef]
- Claes KEY, De Decker I, Monstrey S, Shoham Y, Vyncke T, Depypere B, et al. Helpful hints in deciding what and when to operate after enzymatic debridement. Burns : journal of the International Society for Burn Injuries. 2022. [CrossRef]
- Hoeksema H, Van de Sijpe K, Tondu T, Hamdi M, Van Landuyt K, Blondeel P, et al. Accuracy of early burn depth assessment by laser Doppler imaging on different days post burn. Burns : journal of the International Society for Burn Injuries. 2009;35:36-45. [CrossRef]
- Claes KEY, Hoeksema H, Robbens C, Verbelen J, Dhooghe NS, De Decker I, et al. The LDI Enigma, Part I: So much proof, so little use. Burns : journal of the International Society for Burn Injuries. 2021.
- Claes KEY, Hoeksema H, Robbens C, Verbelen J, Dhooghe N, De Decker I, et al. The LDI Enigma Part II: Indeterminate depth burns, man or machine? Burns : journal of the International Society for Burn Injuries. 2021.
- Claes KEY, Hoeksema H, Vyncke T, Verbelen J, De Coninck P, De Decker I, et al. Evidence based burn depth assessment using laser-based technologies: where do we stand? Journal of burn care & research : official publication of the American Burn Association. 2020.
- Wang R, Zhao J, Zhang Z, Cao C, Zhang Y, Mao Y. Diagnostic accuracy of laser Doppler imaging for the assessment of burn depth: a meta-analysis and systematic review. Journal of burn care & research : official publication of the American Burn Association. 2019. [CrossRef]
- Shin JY, Yi HS. Diagnostic accuracy of laser Doppler imaging in burn depth assessment: Systematic review and meta-analysis. Burns : journal of the International Society for Burn Injuries. 2016;42:1369-76. [CrossRef]
- Monstrey SM, Hoeksema H, Baker RD, Jeng J, Spence RS, Wilson D, et al. Reprint of: Burn wound healing time assessed by laser Doppler imaging. Part 2: Validation of a dedicated colour code for image interpretation. Burns : journal of the International Society for Burn Injuries. 2012;38:195-202. [CrossRef]
- Pape SA, Baker RD, Wilson D, Hoeksema H, Jeng JC, Spence RJ, et al. Burn wound healing time assessed by laser Doppler imaging (LDI). Part 1: Derivation of a dedicated colour code for image interpretation. Burns : journal of the International Society for Burn Injuries. 2012;38:187-94. [CrossRef]
- Claes KEY, Hoeksema, H., Robbens, C., Verbelen, J., Dhooghe, D., De Decker, I., Monstrey, S. The LDI Enigma Part II: Indeterminate depth burns, man or machine? Burns: journal of the International Society for Burn Injuries, accepted for publication 25/02/2021. 2021.
- Pechar J, Lyons MM. Acute Compartment Syndrome of the Lower Leg: A Review. The journal for nurse practitioners : JNP. 2016;12:265-70. [CrossRef]
- Kaplan I, White WL. Incisional decompression of circumferential burns. Plastic and reconstructive surgery and the transplantation bulletin. 1961;28:609-18.
- Hoeksema H, Vandekerckhove D, Verbelen J, Heyneman A, Monstrey S. A comparative study of 1% silver sulphadiazine (Flammazine(R)) versus an enzyme alginogel (Flaminal(R)) in the treatment of partial thickness burns. Burns : journal of the International Society for Burn Injuries. 2013;39:1234-41. [CrossRef]
- Orgill DP. Excision and skin grafting of thermal burns. The New England journal of medicine. 2009;360:893-901. [CrossRef]
- Krieger Y, Rosenberg L, Lapid O, Glesinger R, Bogdanov-Berezovsky A, Silberstein E, et al. Escharotomy using an enzymatic debridement agent for treating experimental burn-induced compartment syndrome in an animal model. The Journal of trauma. 2005;58:1259-64. [CrossRef]
- Ziegler B, Corterier C, Kremer T, Lumenta DB, Plock JA, Richter S, et al. [Implementation of treatment by enzymatic debridement in burns: results of an interprofessional German-speaking expert workshop]. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse : Organ der V. 2021;53:175-84.
- Muhammad ZA, Ahmad T. Therapeutic uses of pineapple-extracted bromelain in surgical care - A review. JPMA The Journal of the Pakistan Medical Association. 2017;67:121-5.
- Schulz A, Ribitsch B, Fuchs PC, Lipensky A, Schiefer JL. Treatment of Genital Burn Injuries: Traditional Procedures and New Techniques. Advances in skin & wound care. 2018;31:314-21. [CrossRef]
- Schulz A, Perbix W, Shoham Y, Daali S, Charalampaki C, Fuchs PC, et al. Our initial learning curve in the enzymatic debridement of severely burned hands-Management and pit falls of initial treatments and our development of a post debridement wound treatment algorithm. Burns : journal of the International Society for Burn Injuries. 2017;43:326-36. [CrossRef]
- Cordts T, Horter J, Vogelpohl J, Kremer T, Kneser U, Hernekamp JF. Enzymatic debridement for the treatment of severely burned upper extremities - early single center experiences. BMC dermatology. 2016;16:8. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).