1. Introduction
Eschar removal within the first 72 hours in burned patients has shown to improve functional and aesthetic outcomes, reduce infection and hospital stay [
1]. Surgical debridement is the standard procedure, but it can be traumatic and is not exempt from complications, entails inadvertent resection of viable tissue and facilitates blood and heat loss. In addition, it requires specific surgical equipment and qualified personnel, being a necessity to find other alternatives for burned patients [
2,
3].
Bromelain-based enzymatic debridement (Nexobrid®) is a recent technique that allows prompt debridement for burn patients. It is a plant-based medication that was approved by the European Medicines Agency in 2012 [
4,
5]. It consists of a mixture of proteolytic proteins from pineapple stems that contains the enzyme bromelain. It has been approved in adults for eschar removal of deep partial and full thickness thermal burn injuries [
4,
5]. It has documented advantages compared with surgical debridement, including the reduction of debridement time; leaving clean surgical zones that have enough epidermis for re-epithelization; and reducing the need for surgery and autografts, infection, blood loss and length of hospital stay [
1,
2,
6].
Even though enzymatic debridement is a good option for eschar removal [
3,
7], it has some concerns, such as coagulation disorders [
8]. Furthermore, it is a painful procedure that should be done under pain management protocols [
1,
9]. Some of the recommendations suggest using regional anaesthesia, with or without the placement of perineural catheters with a long-lasting anaesthetic or general anaesthesia when burns are both on the trunk and extremities [
1,
10,
11]. Nevertheless, most of the recommendations are based on expert consensus and the clinical experience of case reports. Based on the above, the main objective of this study is to describe the anaesthetic strategies in burn patients that underwent debridement with Nexobrid® in our unit.
2. Patients and Methods
We conducted a retrospective observational study in burn patients treated with Nexobrid® that were admitted to Vall d´Hebron University Hospital from January 2015 to December 2019. We included patients older than 18 years that were assessed by the anaesthesia team and had deep partial or full thickness thermal burns. Exclusion criteria were patients with electrical or chemical burns and superficial or superficial-partial thickness burns, as well as patients in which the Anaesthesia Department did not participate actively in their pain management or that were on sedation and mechanical ventilation due to their active illness process.
For the data collection, we performed a review on the electronic clinical chart of the included patients. Demographic variables included age, sex, comorbidities, percentage of the total body surface area (%TBSA) burned, burn location, and aetiology. In addition, we collected information related to the anaesthesia procedures performed for pain control, complications derived from the intervention, the need to repeat an anaesthetic technique and the use of opioids as a rescue treatment alternative.
2.1. Procedure Description
At our institution, Nexobrid® is applied after a preoperative assessment, informed consent and following fasting guidelines [
12]. First, the anaesthesia team performs the technique that is considered appropriate to the case and the burned region. Once it is performed, the nursing staff pre-soaks the burn injury, which helps to identify the effectiveness of the anaesthesia technique. After this, Nexobrid® is applied and covered for 4 hours. Then, it is removed by the drag technique and washed energetically. Finally, the wound is covered again until the next day when it is examined by the plastic surgery team. The whole procedure can be painful, which is why the anaesthesia strategy should be long-lasting to offer better comfort to the patient.
In our unit, Nexobrid® is used for deep partial and full thickness thermal burns located on the head and neck, extremities, trunk, and abdomen. It is important to mention that we do not apply it in patients with more than 15% TBSA burned according to medication regulations and current guidelines [
1,
13]. In addition, not all the burn wounds in one patient can be treated by this medication, so we prioritize those regions that are highly functional and can benefit from enzymatic debridement.
2.2. Outcome Measurement
The principal outcome in our study was pain control during the first 48 hours after the application of Nexobrid®. Data was obtained from the clinical charts registered by the nursing staff.
2.3. Statistical Analysis
We performed a descriptive analysis with calculation of frequencies and percentages for qualitative variables, as well as means and medians for quantitative variables. We used standard deviation and interquartile range as dispersion measures when appropriate. Postoperative pain and %TBSA burned were compared. %TBSA burned was subdivided in two groups, one with patients presenting with a %TBSA burned of 10% or lower and another with %TBSA% burned greater than 10%. Postoperative pain and number of affected areas were also compared, dividing patients with a single affected area from those with multiple affected areas. Postoperative pain and burn aetiology, sex, age and single nerve block vs. catheter placement were also assessed. We used Pearson’s chi-squared test to perform inferential analysis, since most of our data were qualitative variables. P-values less than 0.05 (p < 0.05) were considered significant.
2.4. Ethical Considerations
This research was approved by the Ethics Committee of the Vall d´Hebron University Hospital (reference number: PR(AG)161/2020). The certification was issued on 6 May 2020. In addition, it was approved by the Spanish Agency of Medicines and Medical Devices (AEMPS) (LML-BRO-2020-01).
3. Results
During the time of the study, 214 patients received Nexobrid® for enzymatic debridement in our burn unit. Of these, 59 patients were excluded because pain management was not performed by the anaesthesia team. They were patients admitted to the Burn Intensive Care Unit (ICU) that required mechanical ventilation and sedation, and their pain management was addressed by Burn-ICU intensivist. Out of the remaining 155 patients, 12 patients were not enrolled because they had electrical burns and 31 patients were excluded because there were no written records during the use of Nexobrid®. Thus, we had 112 eligible patients for the study.
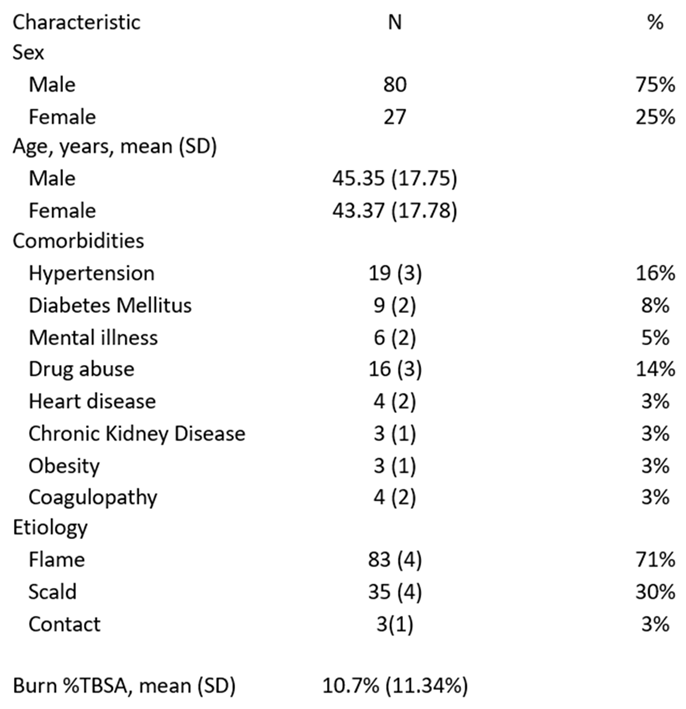
From this population, 75% were male, with a median age of 45.35 years (SD 17.75) and 43.37 years (SD 17.78), respectively. In addition, 13.93% of the patients had two or more comorbidities as described in
Table 1. The mean %TBSA burned was 10.7% (SD 11.34, CI 0–32.93%), and the median for the Abbreviated Burn Severity Index (ABSI) was 5 (IR 2–12). In more than two-thirds of the patients, flame was the mechanism of the burn injury (71%, SD 4%, CI 63–79%), followed by scald (30%, SD 4%, CI 22–38%) and contact (3%, SD 1%, CI 0–5%).
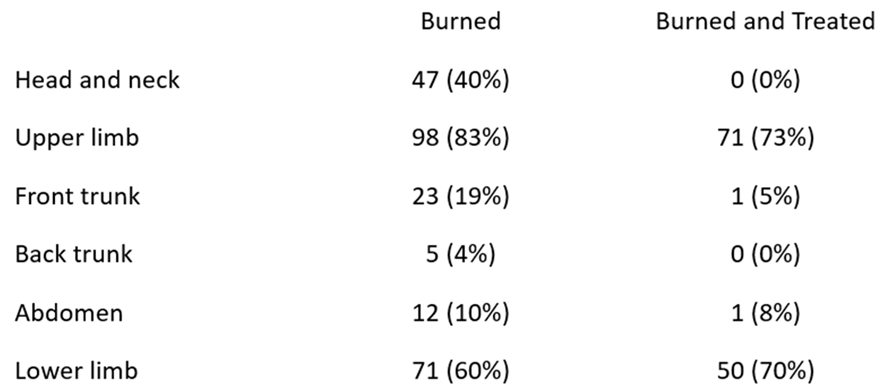
The upper and lower limbs were the most frequent parts of the body that were compromised in our study population (83% and 60%, respectively). Notably, not all burn injuries in a single patient were treated. In our protocol, burned regions located in functional areas were prioritized over others to receive enzymatic debridement. In addition, we had zero reports of patients with head and neck injuries and back and trunk injuries treated with Nexobrid® (
Table 2). This is because they were admitted to the ICU on mechanical ventilation, and their pain management was performed by ICU teams, meeting exclusion criteria.
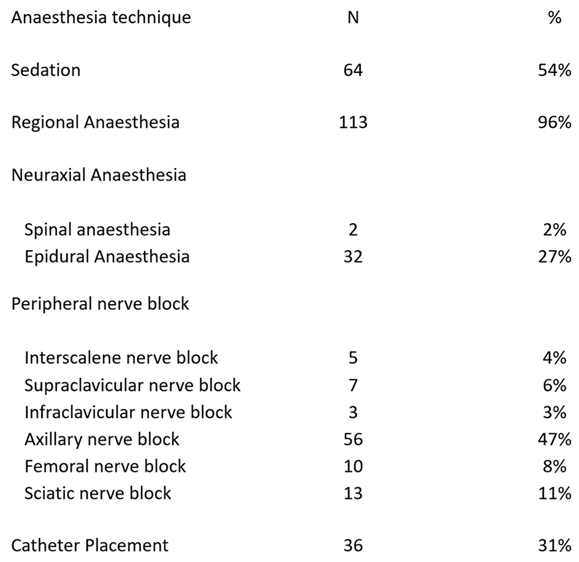
Regional anaesthesia was the most common approach to pain control in our study (96% of the cases; SD 2%, CI 92–99%). Peridural catheter insertion was the most common neuraxial technique performed (27%, SD 4%, CI 19–35%), and axillary nerve block was the most frequent peripheral technique performed (47%, SD 5%, CI 38–56%) (
Table 3). Catheter placement during the technique was performed in 31% of the cases (SD 4%, CI 22–39%). Only nine patients had complications derived from anaesthesia management, including eight patients with hypotension, three patients with nausea and vomiting and one patient with urinary retention.
Pain Control
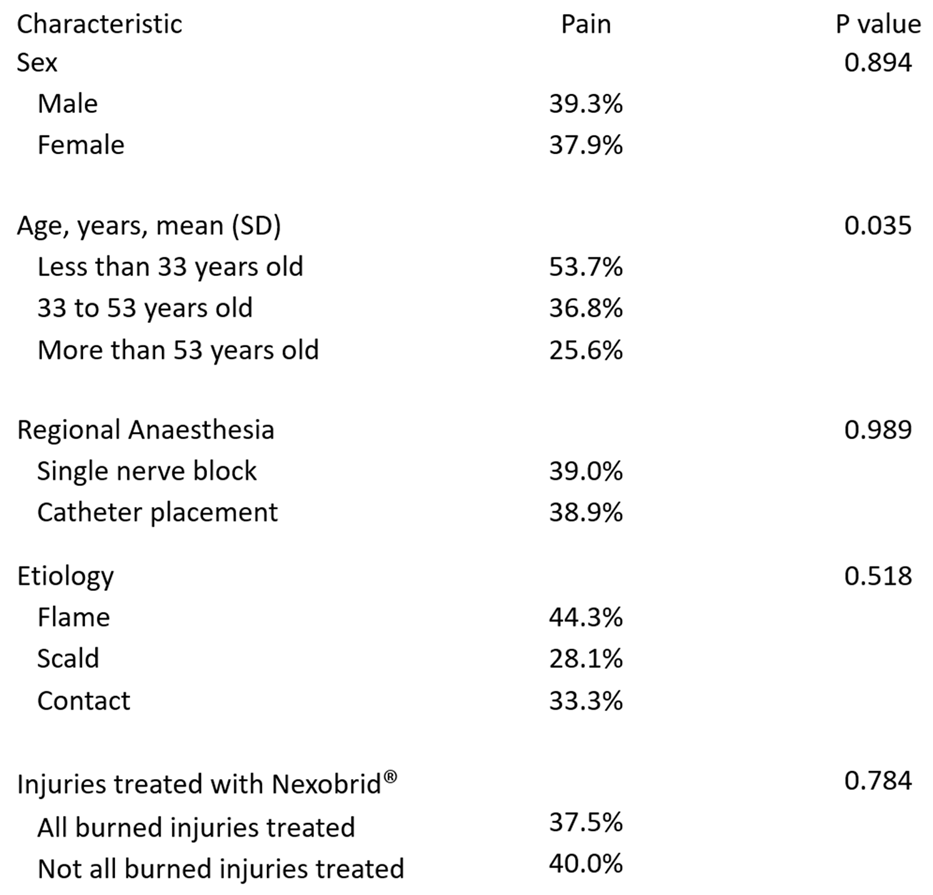
In our study, 61% of the patients reported no pain during the first 48 hours after enzymatic debridement. In 12.5% of the cases, opioids were used for pain relief as rescue treatment, and in 2.7% of the case, the anaesthesia technique needed to be repeated due to lack of effectiveness. There were no differences in pain control in the first 48 hours when a comparison was made between patients receiving a single nerve block and those receiving catheter placement (p = 0.809). Opioid use in patients with continuous infusion of local anaesthetics comprised 38.5% of the cases compared to 61.5% of the cases with single nerve block; however, the difference was not statistically significant (p = 0.319). Notably, there were no differences in pain control between the patients that had all their injuries treated with Nexobrid® compared to those who did not have all their injuries treated with Nexobrid® (p = 0.869). We found a correlation between age and pain. In the group of patients under 30 years old, 53.7% of them reported pain after the procedure compared to 31.17% of the patients that were over this age (p = 0.035). There was no relation between a higher incidence of pain and sex or aetiology of the burn (
Table 4).
4. Discussion
Enzymatic debridement is described as a very painful procedure, in which invasiveness should not be underestimated [
1]. There are not validated protocols to provide analgesia during and after the procedure [
9]. Evidence is based on expert consensus [
1,
10] and the clinical experience of case reports [
11]. Our study included 122 patients, which makes it the largest sample size of patients reported to date.
According to previous studies, regional anaesthesia seems to be superior for pain management compared to sedation [
3,
11,
14]. In our experience and following the recommendations of the clinical guidelines, most of the patients received regional anaesthesia techniques [
1,
9]. We documented appropriate pain control in the first 48 hours in almost two-thirds of the population. However, 39% of the patients reported pain during the first 48 hours after debridement. Notably, only 12.5% of the patients needed opioids for pain relief, suggesting that these patients had moderate to severe pain. One possible reason for this is that some patients had multiple burned regions and not all of them received debridement with Nexobrid®. Therefore, they were not covered by regional anaesthesia techniques. Because there was not enough information in the clinical charts, we could not differentiate if the pain reported was over the area debrided or the other burned regions. In addition, pain in burn patients can be underestimated and techniques, such as patient controlled analgesia, are recommended [
15], since rescue analgesia by nurses on the surgical ward may be less systematic [
16]. In the third place, anxiety and pain in burn patients are strongly associated and are perceived in a similar manner [
17]. We did not use standardized strategies to approach the management of anxiety in our patients, which could influence our pain relief results.
When comparing between a single peripheral nerve block and catheter placement, there were no differences in pain control between these techniques. This is surprising, since based on reported experience, patients had severe pain as the single peripheral nerve block wore off, requiring long-acting rescue opioids [
14]. Capdevila et al. reported a multicentre prospective analysis with continuous peripheral nerve block after orthopaedic surgery, finding that patients had increased pain after 24 hours of the anaesthesia technique [
16]. These results are comparable to our data. One possible explanation is that low volume infusions or low concentrations of local anaesthetics may be insufficient to achieve adequate pain relief when compared to the high volume and high concentrations used in the initial bolus after catheter placement or in the single nerve block technique [
16,
18]. In addition, we were not able to differentiate if the pain reported by our patients was over the area treated with Nexobrid® or a different injured region, which could influence the results when comparing a continuous or single peripheral nerve block. More prospective studies are needed to evaluate whether there is a better strategy over the other.
Notably, Galeiras et al. reported a protocol based on procedural sedation and analgesia in 17 patients treated with Nexobrid® [
9]. They documented, through the Numeric Pain Rating Scale, pain above 4 in 17.6% of the cases. These results were reported only during the procedure. There is no evidence regarding the pain management following enzymatic debridement, so it is unknown whether it is correctly approached and treated in the following hours or days. Our data suggest that it is underestimated, and there is a necessity to find better strategies to offer pain relief in the first 48 hours after the application of Nexobrid®.
Most of the patients included in our research had burn injuries of the extremities. This is because, in our institution, Nexobrid® is a medication that is preserved for specific cases where functional areas of the body are affected. Based on this, most of the patients were suitable for regional anaesthesia techniques. In cases where there was more than one area burned, the team prioritized functional areas in the extremities. Notably, there were no differences in pain control between the patients that had all their injuries treated with Nexobrid® when compared to those who did not have all their injuries treated with Nexobrid®. These findings might be related to the low number of patients in the study and the missing data from the clinical charts. In addition, these results highlight the complexity in the management of pain in burn patients, making it necessary to carry out more research studies for the correct approach.
There are some limitations in our study. First, we could not quantify by objective scales the intensity of the pain in the patients during the first 48 hours after the enzymatic debridement. The results are based on the presence or absence of pain as reported in the clinical history, because the information was gathered by clinical chart review where this data was missing. Second, we could not identify if the pain reported in the charts was in the area treated with Nexobrid® or in a different region in patients with multiple burn injuries. As mentioned before, this information was also recorded in the clinical charts, implying an important bias in our results. Finally, we did not approach the pain management in patients that underwent the procedure and were already on mechanical ventilation and sedation. These patients have a more complex pain control assessment, and there was no information as to whether it was approached correctly.
5. Conclusions
Bromelain-based enzymatic debridement is a painful procedure that requires advanced and specialized anaesthesia management after it is performed. In our experience, regional anaesthesia is the most frequent technique used for pain control, as it is recommended by published data. However, there is still an important quantity of patients that had poor pain control in the first 48 hours after enzymatic debridement. We could not find clear differences in pain relief with continuous nerve blocks over single shots. More studies are needed to assess the best strategy for analgesia during and after the application of Nexobrid®.
References
- Hirche C, Kreken Almeland S, Dheansa B, Fuchs P, Governa M, Hoeksema H, et al. Eschar removal by bromelain based enzymatic debridement (Nexobrid®) in burns: European consensus guidelines update. Burns. 2020;46(4):782–796. [CrossRef]
- Rosenberg L, Krieger Y, Bogdanov-Berezovski A, Silberstein E, Shoham Y, Singer AJ. A novel rapid and selective enzymatic debridement agent for burn wound management: a multi-center RCT. Burns. 2014;40(3):466–474. [CrossRef]
- Schulz A, Perbix W, Shoham Y, Daali S, Charalampaki C, Fuchs PC, Schiefer J. Our initial learning curve in the enzymatic debridement of severely burned hands- Management and pit falls of initial treatments and our development of a post debridement wound treatment algorithm. Burns. 2017;43(2):326–336. [CrossRef]
- European Medicines Agency. Human medicine European public assessment report (EPAR): NexoBrid. Available from: http://www.ema.europa.eu/ [Accessed 10th October 2019].
- European Medicines Agency. Orphan designation: Purified bromelain for the treatment of partial deep dermal and full-thickness burns. Available from: http://www.ema.europa.eu/ [Accessed 10th October 2019].
- Schulz A, Shoham Y, Rosenberg L, Rothermund I, Perbix W, Fuchs PC, et al. Enzymatic versus traditional surgical debridement of severely burned hands: a comparison of selectivity, efficacy, healing time, and three-month scar quality. Journal of Burn Care & Research. 2017;38(4):e745–e755.
- Rosenberg L, Shoham Y, Krieger Y, Rubin G, Sander F, Koller J, et al. Minimally invasive burn care: a review of seven clinical studies of rapid and selective debridement using a bromelain-based debriding enzyme (Nexobrid®). Annals of Burns and Fire Disasters. 2015;28(4):264–274.
- Martín N, Guilabert P, Abarca L, Usua GM, Serracanta J, Colomina MJ. Coagulation abnormalities following NexoBrid use: a case report. Journal of Burn Care & Research. 2018;39(6):1067–1070. [CrossRef]
- Galeiras R, Mourelo M, Pértega S, López ME, Esmorís I. Procedural sedation and analgesia during enzymatic debridement of burn patients. Annals of Burns and Fire Disasters. 2018;31(3):223–227.
- Ranno R, Vestita M, Maggio G, Verrienti P, Melandri D, Orlandi C, et al. Italian recommendations on enzymatic debridement in burn surgery. Burns. 2021;47(2):408–416. [CrossRef]
- Cordts T, Horter J, Vogelpohl J, Kremer T, Kneser U, Hernekamp JF. Enzymatic debridement for the treatment of severely burned upper extremities – early single center experiences. BMC Dermatology. 2016;16(1):8. [CrossRef]
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126(3):376–393.
- Agencia Española de Medicamentos y Productos Sanitarios. Ficha técnica Nexobrid. 2017. Available from: https://cima.aemps.es/cima/dochtml/ft/112803001/#advertencia-tri-ngulo-negro [Accessed 15th April 2021].
- Natalwala I, Kiely J, Kilshaw A, McKay G, Chu V, Phipps A, et al. The Pinderfields hospital pain management protocol for enzymatic debridement of burns wounds. Burns. 2020;46(2):497–500. [CrossRef]
- James DL, Jowza M. Principles of burn pain management. Clinics in Plastic Surgery. 2017;44(4):737–747. [CrossRef]
- Capdevila X, Pirat P, Bringuier S, Gaertner E, Singelyn F, Bernard N, et al. Continuous peripheral nerve blocks in hospital wards after orthopedic surgery: a multicenter prospective analysis of the quality of postoperative analgesia and complications in 1,416 patients. Anesthesiology. 2005;103(5):1035–1045.
- Weinberg K, Birdsall C, Vail D, Marano MA, Petrone SJ, Mansour EH. Pain and anxiety with burn dressing changes: patient self-report. Journal of Burn Care & Rehabilitation. 2000;21(2):155–156; discussion 157–161.
- Ma T, Liu Q, Zhou L, Yue K, Ding Z, Chen B. Continuous nerve block versus single-shot nerve block for total knee arthroplasty: a meta-analysis from randomized controlled trials. Minerva Anestesiologica. 2020;86(2):205–216. [CrossRef]
Table 1.
Demographic characteristics of the studied population.
Table 1.
Demographic characteristics of the studied population.
Table 2.
Description of the burn injury location. In the second row, the number of patients that had a specific burn location is shown. In the third row, the burned locations that were treated with Nexobrid are shown.
Table 2.
Description of the burn injury location. In the second row, the number of patients that had a specific burn location is shown. In the third row, the burned locations that were treated with Nexobrid are shown.
Table 3.
Description of the anaesthesia techniques performed in the study.
Table 3.
Description of the anaesthesia techniques performed in the study.
Table 4.
Comparison of variables with pain in the first 48 hours after enzymatic debridement.
Table 4.
Comparison of variables with pain in the first 48 hours after enzymatic debridement.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).