Introduction
Achalasia is a rare esophageal motility disorder characterised by loss of LES (lower esophageal sphincter) relaxation and afterwards loss of peristalsis in the distal esophagus. [
1] This is theorized to be related to degeneration of neuronal control through loss of ganglion cells in the esophageal wall. [
2] It is unclear what the trigger for this condition is, however several theories revolving around it occurring as a post-viral phenomenon related to Herpes simplex virus (HSV), [
3] Varicella zoster virus (VZV), [
4] and other viral infections. [
5] The exact trigger is however still not exactly elucidated. [
6]
The diagnosis is based on the HRM data as per the Chicago classification version 4.0 (CCv4.0). [
7] This remains the gold standard for diagnosing achalasia with its subtypes, yet the difficulty lies in the multitude of values that are required to establish the diagnosis which makes it difficult for non-experts to interpret these values. These values include IRP (integrated relaxation pressure), DL (distal latency) and distal contractile integral (DCI). [
8]
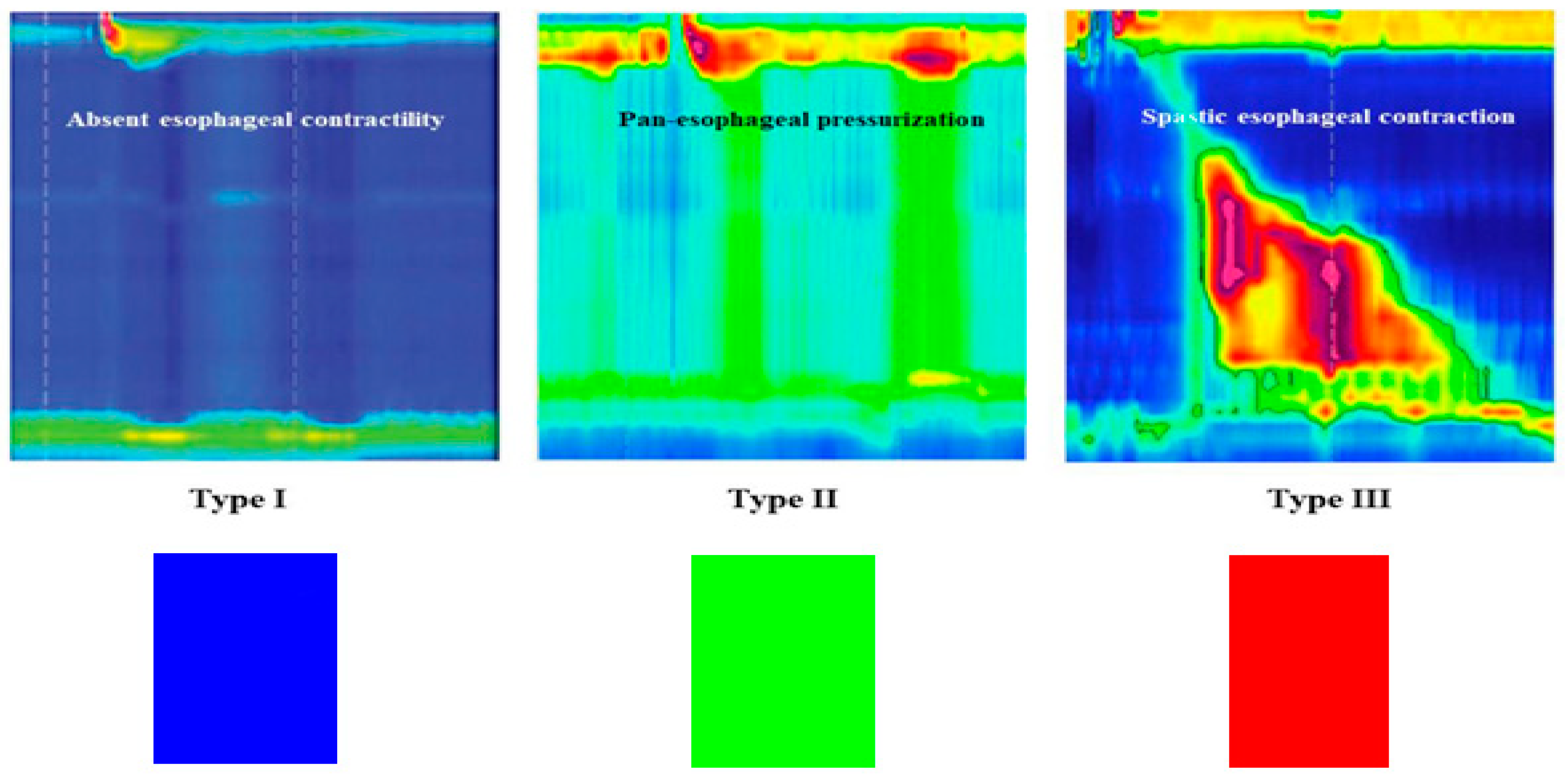
The HRM plots already use color gradients to visualise patterns obtained regarding esophageal pressure patterns such that the blue color indicates minimal pressure, green color indicates moderate pressure and red color indicates high pressure generated. [
9] In spite of this, and to the best extent of our knowledge, we are unaware of any standardized rule for rapid achalasia identification based off the already represented HRM color-coded plots. We hope that the reverse RGB- rule (Blue-Green -Red), which is directly associated to colors obtained through HRM plots, would aid clinicians in easily recognising achalasia. In extension, we hope that this rule will be implemented in AI-assisted software to help expedite esophageal motility disorder diagnostics.
The “Reverse RGB Rule” for Achalasia
The primary colors, described through the mnemonic RGB (Red – Green – blue), constitute the basis for all the colors generated when mixed together, with the red color being at the longest wavelength, green in the middle and blue the shortest wavelength of the three. [
10] These colors constitute the basis for the plots obtained from HRM software, signifying a continuum from low pressure (blue color) to “mid-pressure” (green) to high pressure (red). Type I achalasia involves the absence of peristalsis with minimal pressurization, type II achalasia involves pan-esophageal pressurization while type III achalasia involves the presence of premature contractions with abnormal, spastic peristaltic waves. [
11] The Chicago classification relies heavily on numerical values, mainly the IRP (integrated relaxation pressure), DL (Distal latency) and DCI (distal contractile integral). [
7] These are, however, quite tedious and therefore HRM interpretation has a steep learning curve for early-level trainees. [
12] In
Figure 1, below, we illustrate the typical HRM pattern of each achalasia subtype alongside the association with the earlier mentioned “reverse RGB” rule.
We believe that this rule, albeit appearing simplistic, is an effective rule especially given it already matching the main colors represented in HRMs when diagnosing each achalasia subtype as illustrated in the above figure. Such visual aids reduce the cognitive load associated with diagnostic processes in medicine, which is especially relevant in entry-level trainees. [
13] In addition, the rule may aid in serving as a simplified framework for these trainees and enhance education in this area, especially given the generally poor competency associated with this specific portion of gastroenterology. [
14] Furthermore, the potential for automated pattern recognition of data obtained from HRMs through AI-assisted software is immense, with the possibility of faster and more accurate diagnosis on the basis of such pattern recognition regardless of the numerical data obtained through HRMs. [
15]
In spite of this, there are certain potential limitations to the proposed color-based quick guide. The main one being the lack of validation, as this is necessary to ensure that the color based approach conforms well with the HRM data as per the Chicago classification. In addition, there needs to be multicentre trials to ensure the sensitivity and specificity of this color-based rule for HRM interpretation, alongside inter-observer reliability. To add more, the potential application across other diagnoses within the esophageal motility sphere needs consideration.
Conclusion
The Blue-Green -Red Rule offers a simplified visual classification system for achalasia subtypes, aligning with HRM plot colors for these specific diagnoses. This system may improve clinical decision-making, trainee education with regards to HRM interpretation, and potentially AI-based diagnosis. Further validation with multicenter HRM datasets is needed to confirm the rule’s accuracy and clinical adoption, alongside potential for automated HRM diagnosis.
Funding
No external funding.
References
- Mari A, Baker FA, Pellicano R, Khoury T. Diagnosis and Management of Achalasia: Updates of the last two years. Journal of Clinical Medicine [Internet]. 2021 Aug 16;10(16):3607. [CrossRef]
- Ghoshal UC. Pathogenesis of achalasia cardia. World Journal of Gastroenterology [Internet]. 2012 Jan 1;18(24):3050. [CrossRef]
- Castagliuolo I, Brun P, Costantini M, Rizzetto C, Palù G, Costantino M, Baldan N, Zaninotto G. Esophageal achalasia: Is the herpes simplex virus really innocent? Journal of Gastrointestinal Surgery [Internet]. 2004 Jan 1;8(1):24–30. [CrossRef]
- Naik RD, Vaezi MF, Gershon AA, Higginbotham T, Chen JJ, Flores E, Holzman M, Patel D, Gershon MD. Association of achalasia with active varicella zoster virus infection of the esophagus. Gastroenterology [Internet]. 2021 Apr 29;161(2):719-721.e2. [CrossRef]
- Moradi A, Fazlollahi N, Eshraghi A, Gholipour M, Khoshnia M, Javid N, Montazeri SA, Mikaeli J. Is there any evidence for a viral cause in Achalasia? Middle East Journal of Digestive Diseases [Internet]. 2018 Jun 23;10(3):169–173. [CrossRef]
- Mari A, Khoury T, Sweis R. Achalasia: beyond the basics. Frontline Gastroenterology [Internet]. 2024 Oct 30;flgastro-102822. [CrossRef]
- Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Gyawali CP, Roman S, Babaei A, Mittal RK, Rommel N, Savarino E, Sifrim D, Smout A, Vaezi MF, Zerbib F, Akiyama J, Bhatia S, Bor S, Carlson DA, Chen JW, Cisternas D, Cock C, Coss-Adame E, De Bortoli N, Defilippi C, Fass R, Ghoshal UC, Gonlachanvit S, Hani A, Hebbard GS, Jung KW, Katz P, Katzka DA, Khan A, Kohn GP, Lazarescu A, Lengliner J, Mittal SK, Omari T, Park MI, Penagini R, Pohl D, Richter JE, Serra J, Sweis R, Tack J, Tatum RP, Tutuian R, Vela MF, Wong RK, Wu JC, Xiao Y, Pandolfino JE. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterology & Motility [Internet]. 2020 Dec 29;33(1). [CrossRef]
- Yadlapati R. High-resolution esophageal manometry. Current Opinion in Gastroenterology [Internet]. 2017 Apr 19;33(4):301–309. [CrossRef]
- Nigam GB, Vasant DH, Dhar A. Curriculum review : investigation and management of dysphagia. Frontline Gastroenterology [Internet]. 2021 Aug 3;13(3):254–261. [CrossRef]
- Tedore C, Johnsen S. Using RGB displays to portray color realistic imagery to animal eyes. Current Zoology [Internet]. 2016 Jun 30;63(1):27–34. [CrossRef]
- Kahrilas PJ, Boeckxstaens G. The Spectrum of Achalasia: Lessons from studies of Pathophysiology and High-Resolution Manometry. Gastroenterology [Internet]. 2013 Aug 21;145(5):954–965. [CrossRef]
- Gaddam S, Reddy CA, Munigala S, Patel A, Kanuri N, Almaskeen S, Rude MK, Abdalla A, Gyawali CP. The learning curve for interpretation of oesophageal high-resolution manometry: a prospective interventional cohort study. Alimentary Pharmacology & Therapeutics [Internet]. 2016 Nov 17;45(2):291–299. [CrossRef]
- Young JQ, Van Merrienboer J, Durning S, Cate OT. Cognitive Load Theory: Implications for medical education: AMEE Guide No. 86. Medical Teacher [Internet]. 2014 Mar 4;36(5):371–384. [CrossRef]
- DeLay K, Pandolfino JE, Gyawali CP, Frye J, Kaizer A, Menard-Katcher P, Sloan JA, Gawron AJ, Peterson K, Carlson DA, Khan A, Keswani RN, Yadlapati R. Esophageal Manometry Competency Program improves Gastroenterology Fellow performance in Motility interpretation. The American Journal of Gastroenterology [Internet]. 2020 May 20;115(9):1453–1459. [CrossRef]
- Fass O, Rogers BD, Gyawali CP. Artificial intelligence tools for improving manometric diagnosis of esophageal Dysmotility. Current Gastroenterology Reports [Internet]. 2024 Feb 7;26(4):115–123. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).