Submitted:
04 March 2025
Posted:
05 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Herbal Treatment for Hypothyroidism
2.1. Biomarkers for Diagnosing Hypothyroidism
3. Interventions for Hypothyroidism
3.1. Selenomethionine
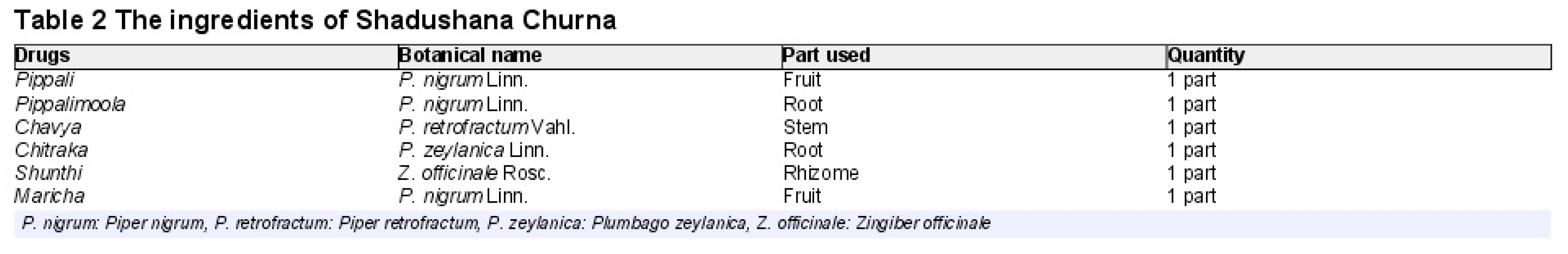
3.2. Shadushana Churna
3.3. Ginger
3.4. Ashwagandha
4. Conclusions
References
- Zúñiga, D.; Balasubramanian, S.; Mehmood, K.T.; Al-Baldawi, S.; Zúñiga Salazar, G. Hypothyroidism and Cardiovascular Disease: A Review. Cureus 2024, 16, e52512. [Google Scholar] [CrossRef] [PubMed]
- Shu, Q.; Kang, C.; Li, J.; Hou, Z.; Xiong, M.; Wang, X.; Peng, H. Effect of Probiotics or Prebiotics on Thyroid Function: A Meta-Analysis of Eight Randomized Controlled Trials. PLOS ONE 2024, 19, e0296733. [Google Scholar] [CrossRef]
- Vol 16 Issue 8, p. 5-6. American Thyroid Association.
- Chiovato, L.; Magri, F.; Carlé, A. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther 2019, 36, 47–58. [Google Scholar] [CrossRef]
- Hennessey, J.V.; Espaillat, R. Subclinical Hypothyroidism: A Historical View and Shifting Prevalence. Int J Clin Pract 2015, 69, 771–782. [Google Scholar] [CrossRef] [PubMed]
- Cherim, A.; Petca, R.-C.; Dumitrascu, M.-C.; Petca, A.; Candrea, E.; Sandru, F. Thyroid Disorders in Systemic Sclerosis: A Comprehensive Review. J Clin Med 2024, 13, 415. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Leung, A.A.C. Evaluation and Management of the Child with Hypothyroidism. World J Pediatr 2019, 15, 124–134. [Google Scholar] [CrossRef]
- Bashkin, A.; Nodelman, M. [THE CLINICAL APPROACH TO DIAGNOSIS AND TREATMENT OF HYPOTHYROIDISM]. Harefuah 2017, 156, 322–325. [Google Scholar]
- Vigone, M.C.; Di Frenna, M.; Weber, G. Heterogeneous Phenotype in Children Affected by Non-Autoimmune Hypothyroidism: An Update. J Endocrinol Invest 2015, 38, 835–840. [Google Scholar] [CrossRef]
- Vacante, M.; Biondi, A.; Basile, F.; Ciuni, R.; Luca, S.; Di Saverio, S.; Buscemi, C.; Vicari, E.S.D.; Borzì, A.M. Hypothyroidism as a Predictor of Surgical Outcomes in the Elderly. Front Endocrinol (Lausanne) 2019, 10, 258. [Google Scholar] [CrossRef]
- Zhou, Q.; Xue, S.; Zhang, L.; Chen, G. Trace Elements and the Thyroid. Front Endocrinol (Lausanne) 2022, 13, 904889. [Google Scholar] [CrossRef]
- Błażewicz, A.; Wiśniewska, P.; Skórzyńska-Dziduszko, K. Selected Essential and Toxic Chemical Elements in Hypothyroidism-A Literature Review (2001-2021). Int J Mol Sci 2021, 22, 10147. [Google Scholar] [CrossRef] [PubMed]
- Sharma, H.; Kakadiya, J. Different Novel Biomarkers Involved in Diagnosing Hypothyroidism. The Egyptian Journal of Internal Medicine 2023, 35, 28. [Google Scholar] [CrossRef]
- Zuhair, V.; Shaikh, A.T.; Shafi, N.; Babar, A.; Khan, A.; Sadiq, A.; Ashraf, M.A.; Nihan, K.; Hamza, M.; Khalid, B.; et al. Role of Supplementation with Selenium and Myo-Inositol vs. Selenium Alone in Patients of Autoimmune Thyroiditis: A Systematic Review and Meta-Analysis 2024.
- Farhangi, M.A.; Dehghan, P.; Tajmiri, S.; Abbasi, M.M. The Effects of Nigella Sativa on Thyroid Function, Serum Vascular Endothelial Growth Factor (VEGF) – 1, Nesfatin-1 and Anthropometric Features in Patients with Hashimoto’s Thyroiditis: A Randomized Controlled Trial. BMC Complement Altern Med 2016, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.B.; Padhar, B.C.; Meena, H.M.L.; Mathur, S.K. Efficacy of Vyoshadi Guggulu and Shadushana Churna in the Management of Subclinical Hypothyroidism: An Open Labelled Randomized Comparative Pilot Clinical Trial. AYU (An International Quarterly Journal of Research in Ayurveda) 2020, 41, 181. [Google Scholar] [CrossRef]
- Ashraf, H.; Heydari, M.; Shams, M.; Zarshenas, M.M.; Tavakoli, A.; Sayadi, M. Efficacy of Ginger Supplementation in Relieving Persistent Hypothyroid Symptoms in Patients with Controlled Primary Hypothyroidism: A Pilot Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Evidence-Based Complementary and Alternative Medicine 2022, 2022, 5456855. [Google Scholar] [CrossRef]
- Sharma, A.K.; Basu, I.; Singh, S. Efficacy and Safety of Ashwagandha Root Extract in Subclinical Hypothyroid Patients: A Double-Blind, Randomized Placebo-Controlled Trial. The Journal of Alternative and Complementary Medicine 2018, 24, 243–248. [Google Scholar] [CrossRef]
- Luo, J.; Zhou, L.; Sun, A.; Yang, H.; Zhang, P.; Liu, K.; Yu, X.; Lin, Y.; Huang, Y.; Han, L. Herbal Medicine for Hashimoto’s Thyroiditis: A Systematic Review and Network Meta-Analysis. Journal of Ethnopharmacology 2024, 323, 117663. [Google Scholar] [CrossRef]
- Wei, M.; Ma, W.; Zhang, W.; Yin, D.; Tang, Y.; Jia, W.; Jiang, Y.; Wang, C.; Gong, Y. Efficacy and Safety of Ophiocordyceps Sinensis in the Treatment of Hashimoto’s Thyroiditis: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2023, 14. [Google Scholar] [CrossRef]
- An, J.H.; Kim, Y.J.; Kim, K.J.; Kim, S.H.; Kim, N.H.; Kim, H.Y.; Kim, N.H.; Choi, K.M.; Baik, S.H.; Choi, D.S.; et al. L-Carnitine Supplementation for the Management of Fatigue in Patients with Hypothyroidism on Levothyroxine Treatment: A Randomized, Double-Blind, Placebo-Controlled Trial. Endocrine Journal 2016, 63, 885–895. [Google Scholar] [CrossRef]
- Zhao, G.; Wang, Z.; Ji, J.; Cui, R. Effect of Coffee Consumption on Thyroid Function: NHANES 2007-2012 and Mendelian Randomization. Front. Endocrinol. 2023, 14. [Google Scholar] [CrossRef]
- Zavros, A.; Andreou, E.; Aphamis, G.; Bogdanis, G.C.; Sakkas, G.K.; Roupa, Z.; Giannaki, C.D. The Effects of Zinc and Selenium Co-Supplementation on Resting Metabolic Rate, Thyroid Function, Physical Fitness, and Functional Capacity in Overweight and Obese People under a Hypocaloric Diet: A Randomized, Double-Blind, and Placebo-Controlled Trial. Nutrients 2023, 15, 3133. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Wei, J.; Wang, L.; Wang, Q.; Zhao, J.; Chen, S.; Wei, F. Effects of Selenium Supplementation on Graves’ Disease: A Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine 2018, 2018, e3763565. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.F.; Venn, B.J.; Manning, P.J.; Cameron, C.M.; Skeaff, S.A. Iodine Supplementation of Mildly Iodine-Deficient Adults Lowers Thyroglobulin: A Randomized Controlled Trial. The Journal of Clinical Endocrinology & Metabolism 2016, 101, 1737–1744. [Google Scholar] [CrossRef]
- Javidi, N.; Khorasani, Z.M.; Salari, R.; Niroumand, S.; Yousefi, M. Achievements in Hypothyroidism Treatment with Herbal Medicine: A Systematic Review of Randomized Controlled Trials. Current Drug Discovery Technologies 2023, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rabbani, E.; Golgiri, F.; Janani, L.; Moradi, N.; Fallah, S.; Abiri, B.; Vafa, M. Randomized Study of the Effects of Zinc, Vitamin A, and Magnesium Co-Supplementation on Thyroid Function, Oxidative Stress, and Hs-CRP in Patients with Hypothyroidism. Biol Trace Elem Res 2021, 199, 4074–4083. [Google Scholar] [CrossRef]
- Yavari, M.; Akbari, M.; Ramezani Ahmadi, A.; Siavash Dastjerdi, M.; Hashemi, M.S. Investigating the Effect of Combined Use of Selenium and Myo-Inositol Supplements on Thyroid Function and Autoimmune Characteristics in Thyroid Disorders: A Systematic Review and Meta-Analysis. Expert Review of Endocrinology & Metabolism 2024, 19, 269–277. [Google Scholar] [CrossRef]
- Nordio, M. A Novel Treatment for Subclinical Hyperthyroidism: A Pilot Study on the Beneficial Effects of l-Carnitine and Selenium. Eur Rev Med Pharmacol Sci 2017, 21, 2268–2273. [Google Scholar]
- Jiang, H.; Chen, X.; Qian, X.; Shao, S. Effects of Vitamin D Treatment on Thyroid Function and Autoimmunity Markers in Patients with Hashimoto’s Thyroiditis—A Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Pharmacy and Therapeutics 2022, 47, 767–775. [Google Scholar] [CrossRef]
- Wang, S.; Wu, Y.; Zuo, Z.; Zhao, Y.; Wang, K. The Effect of Vitamin D Supplementation on Thyroid Autoantibody Levels in the Treatment of Autoimmune Thyroiditis: A Systematic Review and a Meta-Analysis. Endocrine 2018, 59, 499–505. [Google Scholar] [CrossRef]
- Dineva, M.; Fishpool, H.; Rayman, M.P.; Mendis, J.; Bath, S.C. Systematic Review and Meta-Analysis of the Effects of Iodine Supplementation on Thyroid Function and Child Neurodevelopment in Mildly-to-Moderately Iodine-Deficient Pregnant Women. The American Journal of Clinical Nutrition 2020, 112, 389–412. [Google Scholar] [CrossRef]
- Hoang, T.D.; Olsen, C.H.; Mai, V.Q.; Clyde, P.W.; Shakir, M.K.M. Desiccated Thyroid Extract Compared with Levothyroxine in the Treatment of Hypothyroidism: A Randomized, Double-Blind, Crossover Study. J Clin Endocrinol Metab 2013, 98, 1982–1990. [Google Scholar] [CrossRef]
- Shimomura, Y.; Kobayashi, I.; Maruto, S.; Ohshima, K.; Mori, M.; Kamio, N.; Fukuda, H. Effect of Gamma-Oryzanol on Serum TSH Concentrations in Primary Hypothyroidism. Endocrinol Jpn 1980, 27, 83–86. [Google Scholar] [CrossRef]
- Dai, X.; Zhou, Y.; Yu, X. [Effect of ginseng injection in treating congestive heart failure and its influence on thyroid hormones]. Zhongguo Zhong Xi Yi Jie He Za Zhi 1999, 19, 209–211. [Google Scholar] [PubMed]
- Wang, F.; Li, C.; Li, S.; Cui, L.; Zhao, J.; Liao, L. Selenium and Thyroid Diseases. Front Endocrinol (Lausanne) 2023, 14, 1133000. [Google Scholar] [CrossRef] [PubMed]
- Lyons, M.P.; Papazyan, T.T.; Surai, P.F. Selenium in Food Chain and Animal Nutrition: Lessons from Nature -Review-. Asian-Australasian Journal of Animal Sciences 2007, 20, 1135–1155. [Google Scholar]
- Schrauzer, G.N. Selenomethionine: A Review of Its Nutritional Significance, Metabolism and Toxicity. The Journal of Nutrition 2000, 130, 1653–1656. [Google Scholar] [CrossRef] [PubMed]
- Al-Amoudi, W.M. Toxic Effects of Lambda-Cyhalothrin, on the Rat Thyroid: Involvement of Oxidative Stress and Ameliorative Effect of Ginger Extract. Toxicol Rep 2018, 5, 728–736. [Google Scholar] [CrossRef]
- Jafarnejad, S.; Keshavarz, S.A.; Mahbubi, S.; Saremi, S.; Arab, A.; Abbasi, S.; Djafarian, K. Effect of Ginger (Zingiber Officinale) on Blood Glucose and Lipid Concentrations in Diabetic and Hyperlipidemic Subjects: A Meta-Analysis of Randomized Controlled Trials. Journal of Functional Foods 2017, 29, 127–134. [Google Scholar] [CrossRef]
- Mohammed, E.T.; Hashem, K.S.; Ahmed, A.E.; Aly, M.T.; Aleya, L.; Abdel-Daim, M.M. Ginger Extract Ameliorates Bisphenol A (BPA)-Induced Disruption in Thyroid Hormones Synthesis and Metabolism: Involvement of Nrf-2/HO-1 Pathway. Sci Total Environ 2020, 703, 134664. [Google Scholar] [CrossRef]
- Institute of Functional Medicine Specialization The Efficacy of Ashwagandha Root Extract for Hypothyroidism. [Internet]. Available from: Https://Institutodeespecializacionenmedicinafuncional.Com.
- Ashwagandha in hypothyroidism Available from: Ashwagandha in Hypothyroidism.Pdf.
- Sharma, A.K.; Basu, I.; Singh, S. Efficacy and Safety of Ashwagandha Root Extract in Subclinical Hypothyroid Patients: A Double-Blind, Randomized Placebo-Controlled Trial. The Journal of Alternative and Complementary Medicine 2018, 24, 243–248. [Google Scholar] [CrossRef]
- Arumugam, V.; Vijayakumar, V.; Balakrishnan, A.; B Bhandari, R.; Boopalan, D.; Ponnurangam, R.; Sankaralingam Thirupathy, V.; Kuppusamy, M. Effects of Ashwagandha (Withania Somnifera) on Stress and Anxiety: A Systematic Review and Meta-Analysis. EXPLORE 2024, 20, 103062. [Google Scholar] [CrossRef] [PubMed]
- Song, E.; Ang, L.; Lee, M.S. Increasing Trends and Impact of Integrative Medicine Research: From 2012 to 2021. Integr Med Res 2022, 11, 100884. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.A.; Stem, L.A.; Bruehlman, R.D. Hypothyroidism: Diagnosis and Treatment. afp 2021, 103, 605–613. [Google Scholar]
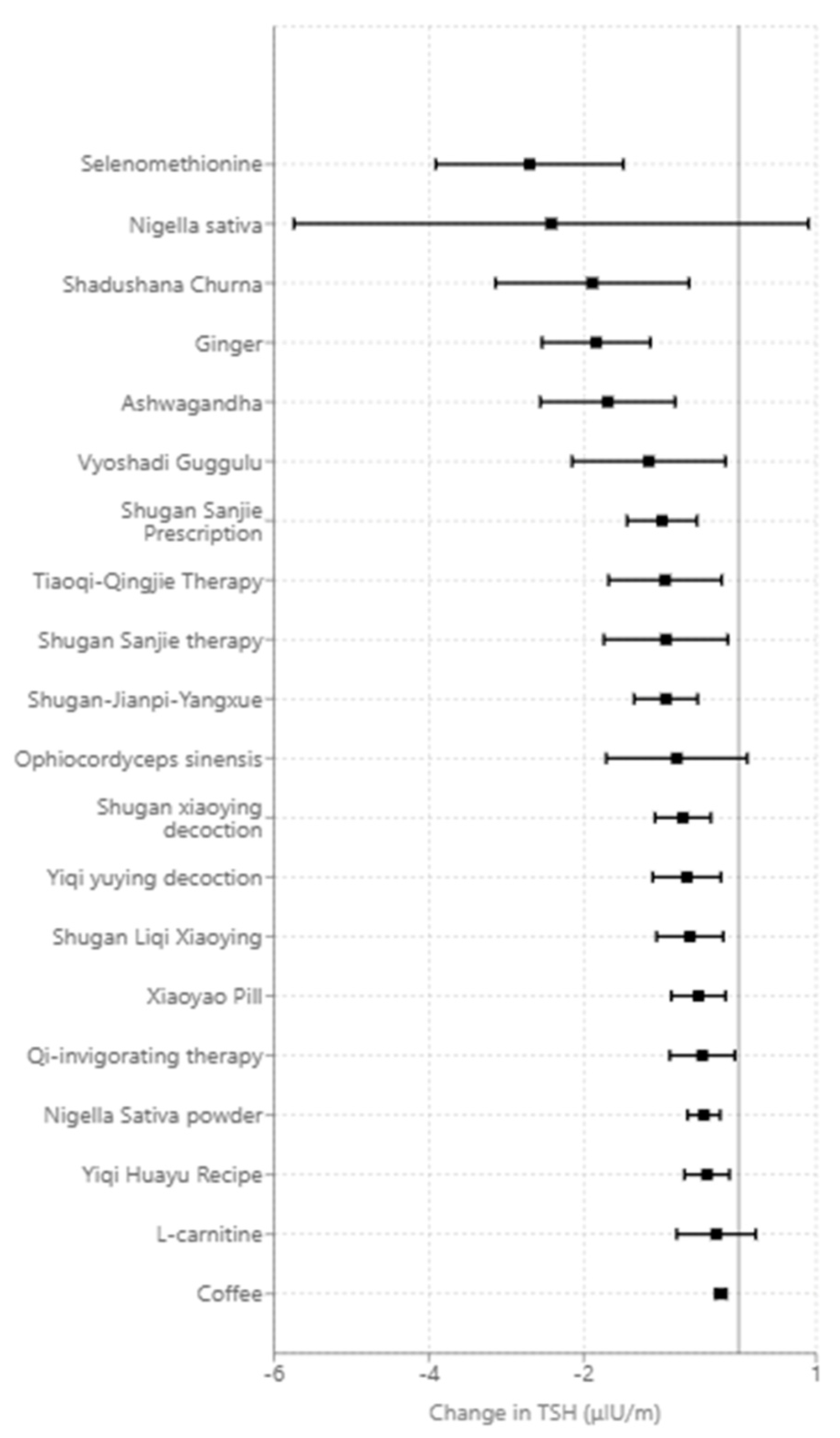
| Intervention | Impact on Thyroid Stimulating Hormone (TSH) (μIU/m) relative to placebo or baseline |
|---|---|
| Selenomethionine and myo-inositol | -3.10 [-4.25,-1.95] [14] |
| Selenomethionine | -2.70[-3.91,-1.49] [14] |
| Nigella sativa | -2.42 [−5.74,0.90] n.s. [15] |
| Shadushana Churna | -1.89[-3.14,−0.64] [16] |
| Ginger | -1.84 [-2.54,-1.14] [17] |
| Ashwagandha | -1.69[-2.56, -0.82] [18] |
| Vyoshadi Guggulu | -1.16[-2.15,-0.16] [16] |
| Shugan Sanjie Prescription | -0.99 [-1.44, -0.68] [19] |
| Tiaoqi-Qingjie Therapy | -0.95 [-1.68, -0.54] [19] |
| Shugan Sanjie therapy | -0.94 [-1.74, -0.50] [19] |
| Shugan-Jianpi-Yangxue medicine | -0.94 [-1.35, -0.66] [19] |
| Ophiocordyceps sinensis | -0.80[-1.71,0.11] n.s. [20] |
| Shugan xiaoying decoction | -0.72 [-1.08, -0.48] [19] |
| Yiqi yuying decoction | -0.67 [-1.11, -0.40] [19] |
| Shugan Liqi Xiaoying formula | -0.63 [-1.06, -0.38] [19] |
| Xiaoyao Pill | -0.52 [-0.87, -0.31] [19] |
| Qi-invigorating phlegm and Blood-Activating Therapy | -0.47 [-0.89, -0.25] [19] |
| Nigella Sativa powder | -0.45 [-0.66, -0.30] [19] |
| Yiqi Huayu Recipe | -0.41 [-0.70, -0.24] [19] |
| L-carnitine | -0.29[-0.80, 0.22] n.s. [21] |
| Coffee | -0.23[-0.30, -0.16] [22] |
| Zinc and Selenium | n.s. [23] |
| Selenium | n.s. [24] |
| Iodine | n.s. [25] |
| Probiotics | n.s. [2] |
| Mentha x Piperita | n.s. [26] |
| Zinc, Vitamin A, and Magnesium Co-supplementation | n.s. [27] |
| Selenium and Myo-inositol | n.s. [28] |
| l-carnitine and selenium | n.s. [29] |
| Vitamin D | n.s. [30]n.s. [31] |
| Iodine | n.s. [32] |
| Thyroid extract | n.s. [33] |
| Gamma-oryzanol (rice bran extract_ | n.s. [34] |
| Ginseng | n.s. [35] |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




