1. Introduction
Coronary artery disease (CAD) is one of the leading causes of death and disability worldwide and although treatment advances have improved survival after the acute coronary syndrome, patients with established CAD have a higher risk of future cardiovascular events [
1]. Variations in the treatment of CAD that are related to gender and ethnicity have been described since the landmark studies in the late 1980s and early 1990s. According to those studies, women and minorities tend to receive less invasive treatment of myocardial infarction, and that has not changed significantly in more recent cohorts [
2].
The relationships between CAD and relevant risk factors have been long time evaluated . Higher prevalence of these risk factors is generally associated with lower socioeconomic status which is present in many ethnic minorities. Risk factor reduction after acute coronary syndrome (ACS), as well adherence to medical therapy, are crucial in lowering morbidity and mortality rate after ACS [
3,
4]. Ethnicity is one of the factors that were found to be associated with different mortality rates but also is correlated with reduced adherence to medical therapy [
5,
6,
7]. One study showed no significant difference in short term adherence to therapy among minorities, but patients among ethnic minority groups were significantly less adherent to preventive therapies at 12 months post- discharge [
8]. However, up-to-date data about long- term adherence to therapy in minorities are scarce.
In Croatia, as well as in many other parts of European Union, one of the most socially and economically disadvantaged group is the Roma minority. Since this group has been reported to be susceptible to an unhealthy lifestyle due to low educational level and poverty it is not surprising that epidemiological studies have revealed a high prevalence of disease-related risk factors and therefore higher prevalence of cardiovascular diseases among Roma population [
9,
10,
11].
On the other hand, little is known about adherence to medical therapy in Roma population, especially in long-term after ACS treatment. Also, invasive treatment strategies that are known to improve survival in ACS have been used less in minorities group [
2]. Nevertheless, data about treatment strategies in ACS in Roma population in Europe are scarce. One important study evaluated 7 year mortality in Roma population after coronary angiography (CAG) and found that all-cause mortality was significantly higher in Roma subgroup [
12]. However, those patients underwent elective CAG, with a substantial number of patients with no obstructive coronary artery disease (especially among non-Roma patients), and no data on CAG or revascularization rates in the setting of acute myocardial infarction (AMI) and ACS.
We conducted this single center retrospective cohort study to explore differences in clinical characteristics and invasive treatment of AMI and long-term overall and composite event-free survival between the Roma population and the majority population (Croatian; Caucasian) living in and around the City of Zagreb and other parts of North-Western Croatia. Secondly, we aimed to assess the association between the adherence to medical therapy after acute coronary syndrome and major adverse cardiovascular events (MACE) throughout long-term follow-up.
2. Materials and Methods
Study Population
We retrospectively analyzed a cohort of 318 consecutive patients with AMI hospitalized in one university hospital center in Croatia in a period from Jun 2011 to Jun 2015. There were 67 Roma patients and 251 age and gender matched non-Roma (all Caucasian) patients treated during the same period. Patients were eligible for registration and followed-up if appropriate ethnicity was confirmed by the patient and patient’s relatives. We included only ACS patients who had clear clinical diagnostic criteria for ST elevation myocardial infarction (STEMI) or moderate or high/very high risk non-ST elevation myocardial infarction (NSTEMI) and underwent coronary angiography (within 12 h of chest-pain onset in case of STEMI or within 72 h of hospital admission in case of NSTEMI), and were discharged in stable condition after initial hospital treatment. Patients who did not survive initial hospitalization for the index ACS event were not included in this long-term follow-up study. There were no differences in proportions of in-hospital mortality, refractory cardiogenic shock at presentation or rates of conservative treatment of AMI between Roma and non-Roma patients treated in our center during the observed period (data not shown).
All patients received appropriate therapies according to guidelines for the treatment of ACS. Demographic, clinical, angiographic, and medical therapy data were collected at hospital discharge. Therapy adherence data were recorded at the end of the follow-up from Feb to May 2020 by telephone visits. In addition to standard demographic, clinical and angiographic data, Syntax score was derived for every patient from the collected angiographic data. Syntax score was calculated for all patients by single operator, not blinded for patient demographics and ethnicity, using the comprehensive on-line Syntax score calculator [
13]. Higher Syntax score represented more complex coronary artery disease. We estimated the renal function using Cockcroft-Gault equation and expressed it as creatinine clearance (CrCl) in ml/min/1.73m2. Education and social-economic status of every patients was self-reported and noted at admission. Poverty line in Croatia is set by the national statistics department at 300 Euros for entire household per month. The index year of enrolment (2011-2013 vs 2014-2015) was also taken in consideration because new P2Y12 inhibitors and new strategies for invasive treatment of NSTEMI entered in our practice in 2014.
After the inclusion, patients were followed-up by accessing data from hospital information system and by telephone visits. Telephone visits were performed for all patients at the end of the follow-up between Feb and May 2020 in order to collect information about therapy adherence and additional events if they were not recorded within the hospital information system. Adherence to medication proposed at discharge and during follow-up was assessed by Morisky Medication Adherence Scale (MMAS-8) questionnaire, designed to analyze patients’ prescription medication habits [
14]. The first seven items in the questionnaire are dichotomous response categories with yes or no answers and the last item was a five point Likert response [
14]. We examined several classes of medical therapy, including statins, β-blockers, ACE inhibitor/ARBs, dual antiplatelet therapy (P2Y12 inhibitors and acetylsalicylic acid). According to answers provided in the MMAS-8 scale patients were classified into three groups: low adherence (MMAS-8 score <6), moderate adherence (MMAS-8 score 6 or 7), and high adherence (MMAS-8 score >7) [
14]. There were 53 Roma patients with available therapy adherence data, and 210 non-Roma patients with adherence therapy data at the end of the follow-up that were included in long-term follow-up analyses of therapy adherence and other important clinical characteristics on adverse events.
Primary outcomes during follow-up were all-cause death after discharge and major adverse cardiac event (MACE) that was a composite of any of the following events: death from cardiovascular cause, stroke, repeated myocardial infarction (MI), symptomatic heart failure requiring ambulatory or hospital specialist care, repeated target lesion revascularization, unplanned revascularization (any) or unplanned cardiac surgery (planned CABG that was organized after patient discharge and complete stabilization was not considered to be a MACE). The study complies with the Declaration of Helsinki and it was approved by the Institutional Review boards of all hospitals included in patient treatment.
Statistical Methods
Normality of distribution of numerical variables was assessed using the Shapiro-Wilk test. None of presented numerical variables followed normal distribution and were presented as median and range and were compared between the groups using the Mann-Whitney test. Categorical variables were presented as frequencies and percentages and were compared between the groups using the χ2 test. Event rates during follow up were assessed using Kaplan-Meier method. Event rate curves were compared univariately using the Mantel-Cox Log-rank test.
Multivariate analyses for all cause death and MACE were done using the Cox regression, with different models fitted. The first regression model (Model A) used only ethnicity as a dependent categorical variable. Therapy adherence data were available only for patients that survived to last follow-up in 2020. Therefore, all relevant variables that differed significantly except for data on therapy adherence presented in
Table 1, were included in the second (Model B: ethnicity, coronary anatomy complexity and left ventricular ejection fraction) and third (Model C: ethnicity, coronary anatomy complexity, left ventricular ejection fraction and all other significantly different variables) multivariate Cox regression models for death and MACE. Fourth Cox regression model (Model D) with all the relevant variables was fitted only for MACE within the selected group of 263 patients (53 Roma and 210 non-Roma patients) that had valid data on therapy adherence and survived until last follow-up in 2020. All models (A to D) were adjusted also for age and index year. Final regression models C and D were selected through a stepwise procedure with the “entry” and “stay” criterion of p≤0.10. To avoid collinearity, variables that assessed same/similar parameters were not used together within one mode (i.e. Syntax score for complexity of coronary artery disease was not used with categorical single-, double- or multivessel disease variable, patients’ income was not fitted together with employment and education etc.). P values <0.05 were considered to be statistically significant. Bonferroni correction for multiple simultaneous comparisons was used where appropriate. All calculations were performed using the IBM SPSS software, version 19 (IBM, USA).
3. Results
The analysis included a total of 318 patients with median age of 58 years (range 27 to 86 years), of which 222 (70%) were male. There were 229 patients with STEMI (72%) and 89 patients with moderate/high/very high risk NSTEMI (28%). Median follow-up time for the whole cohort was 84 months.
Differences in demographic, clinical, laboratory, angiographic, treatment and outcome data between Roma and non-Roma population are presented in
Table 1. Roma population had significantly more unemployed patients with household income below poverty line in Croatia, and had significantly more patients with no education or only elementary school education. Roma patients were more frequently actively smoking tobacco at admission, had more double- or multivessel coronary artery disease on urgent/early coronary angiography and were significantly more frequently scheduled for coronary artery bypass grafting (CABG) after initial coronary angiography. However, there were no differences in revascularization rates (PCI + CABG) after index AMI between Roma and non-Roma subgroups (90% vs 92%, respectively). There were no significant differences in proportions of other relevant risk factors. When analyzing continuous variables between Roma and non-Roma subgroups, Roma patients had significantly higher Syntax score, glycated hemoglobin (HbA1c), and triglyceride levels at admission, whereas their left ventricular ejection fraction (LVEF) at discharge was significantly lower (
Table 1).
At telephone follow-up in 2020, 53 Roma patients that provided data on therapy adherence had significantly lower therapy adherence measured with MMAS-8 scoresheet than 210 non-Roma patients. Roma patients also reported shorter duration of dual antiplatelet therapy after discharge and had lower penetration of statin therapy at last follow-up in comparison to non-Roma patients. Also, more Roma patients developed new-onset diabetes mellitus during follow-up, whereas less Roma patients quit actively using tobacco after discharge compared to non-Roma patients, but those differences were not statistically significant (
Table 1).
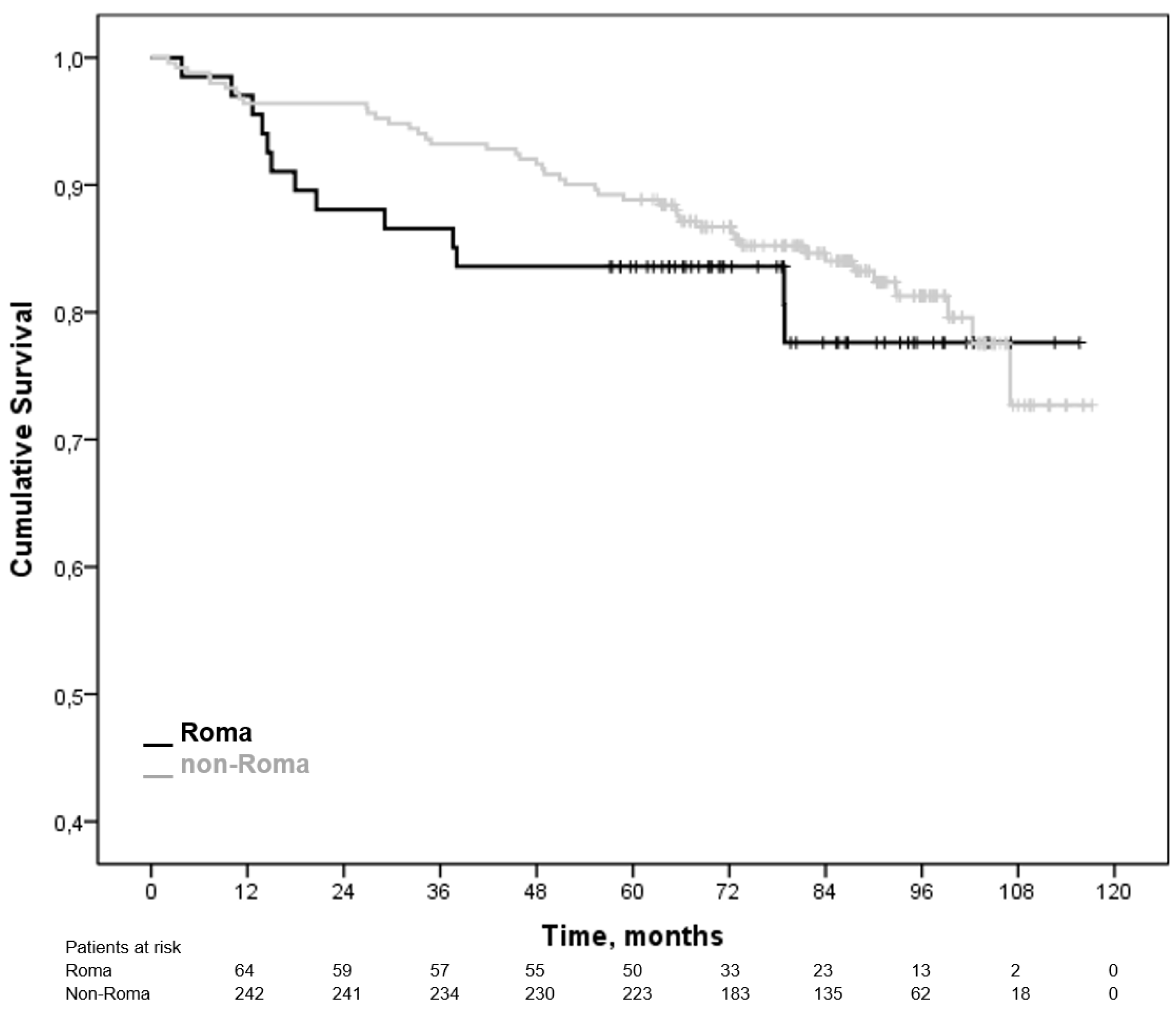
There were no significant differences in cumulative rates of all-cause death and MACE during follow-up (
Table 1). Proportion of Roma patients that died during follow-up was 19%, and was similar to non-Roma patients (relative risk for all-cause death for Roma patients 1.11, 95% CI 0.63-1.93). Roma patients’ time to all cause-death was not significantly different when compared to non-Roma patients (Mantel-Cox Log rank test, p=0,457,
Figure 1).
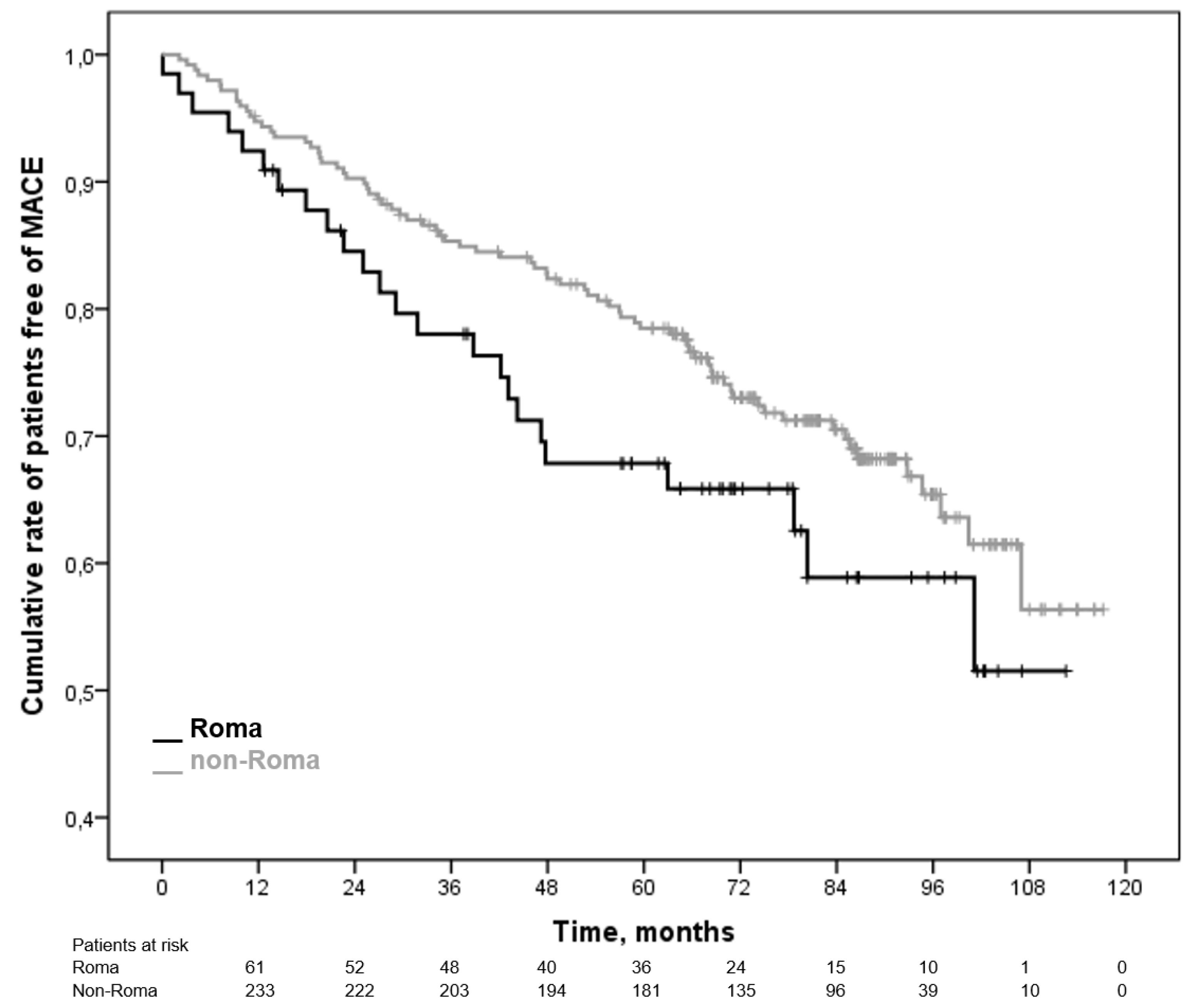
More Roma patients experienced any MACE during follow-up compared to non-Roma patients (37% vs 31% respectively), with more stroke (10% vs 4.5%) and repeated MI events (15% vs 10%, respectively), but that difference was not statistically significant (relative risk for composite MACE for Roma patients 1.19, 95% CI 0.83-1.70). Kaplan-Meier analysis of time-to-MACE showed that more Roma patients experienced MACE during first two years of follow-up (
Figure 2). However, that difference was not statistically significant within the whole follow-up period (Mantel-Cox Log rank test, p=0,129,
Figure 2).
Cox regression Model A showed no significant impact of ethnicity alone (Roma vs non-Roma) on all-cause death or MACE. Model B showed that higher LVEF at discharge was associated with better overall survival irrespective of complexity of coronary artery disease (expressed as Syntax score) and ethnicity. When Model B was fitted for MACE, higher LVEF at discharge and lower Syntax score were independently associated with lower rates of MACE during follow, irrespective of ethnicity. Model C showed that only left ventricular ejection fraction remained independently associated with both overall survival and MACE after including ethnicity, Syntax score, social-economic status, smoking status, HbA1c or triglyceride levels (
Table 2). Finally, Model D - a subgroup regression analysis of MACE in 263 patients (51 Roma and 212 non-Roma patients) that had reliable data on therapy adherence at last telephone visit in 2020, showed that only low adherence to medical therapy was independently associated with more MACE, irrespective of ethnicity, Syntax score, left ventricular ejection fraction, social-economic status, smoking status, HbA1c and triglyceride levels (
Table 2). All regression models (A to D) were adjusted for age and index year of treatment, and both did not abrogate significant results in any of the models.
4. Discussion
Roma patients treated with an invasive strategy for AMI in our center and discharged for ambulatory treatment had significantly worse demographic, socio-economic, and clinical characteristics, and more complex CAD anatomy compared to age and gender matched non-Roma patients treated during the same period. They also had significantly worse medical therapy adherence. However, Roma patients experienced similar rates of revascularization (PCI + CABG), and did not have significantly worse overall survival during long-term follow-up. Their MACE rate was higher, especially within the first two years of follow-up that might reflect aforementioned differences. However, MACE rate during the entire follow-up period was also not significantly higher when compared to non-Roma patients.
This study is the first to bring comprehensive data on patients’ characteristics and revascularization rates after ACS and long-term outcomes among Roma minority in Europe. A study conducted in USA [
15] showed that minorities (i.e. African-American and Hispanics) tended to receive lower rates of revascularization in acute coronary syndrome setting. However, all citizens in Croatia and the EU have health insurance which is not the case in USA, and most probably reflects the differences between the health care systems. Other studies of cardiovascular morbidity which were conducted in the setting of equal access to medical care showed greater differences in patients characteristics between minority and majority populations and lesser differences in mortality rates. Study conducted in Israel [
16] reported similarity between the Arab and non-Arab ACS patients in the time from first medical contact (FMC) to percutaneous coronary intervention and in rates of coronary angiographies. There are great differences among health care systems worldwide which makes them difficult to compare. However, due to the recent increase in the number of refugees from conflict-affected areas, health care systems in EU should adapt to those demographic changes. It is challenging to provide everyone with equal access to acute health care, as well as educating patients in recognizing symptoms that require acute care. In one review about time from onset of chest pain and first medical contact [
17], authors stated that the heterogeneity of the outcome measures of included studies prevented statistical pooling for meta-analysis and therefore data were presented as a narrative summary. That systematic review showed that minority groups had a significant longer delay time from onset of chest pain to medical contact than the majority population. The challenge of patient equality is also present in secondary prevention. Adherence to medical therapy and other secondary prevention measures are shown to reduce mortality, improve quality of life and reduce hospital readmissions [
18,
19]. However, data regarding adherence to medical therapy in minority groups are scarce. Two Swedish studies [
20,
21] have compared migrants and Swedish-born patients’ use of preventive medications but the results were conflicting. Another Scandinavian study [
22] analyzed post-ACS use of secondary prevention among non-Western and Western migrants and Danish-born patients. Non-Western migrants had a higher risk of discontinuation of all medications included in the study, which is in line with our results. However, our study is the first to evaluate adherence to medical therapy and differences in long term outcomes after ACS among Roma minority group and other patients. Worldwide, significant disparities in cardiovascular care of ethnic minorities continue to persist nowadays and are often attributed to more unfavorable risk factors (higher HbA1c and triglyceride levels among Roma) shown also in our study. Other reasons for such disparities can be attributed to socioeconomic factors such as poverty, inadequate education regarding healthy habits and medication adherence [
15,
23], that was also shown among Roma population in our study. Nonetheless, those differences did not produce worse outcomes among Roma population in out study. We did not find negative ethnicity bias regarding revascularization procedures in ACS, most probably explaining the non-significant differences in long term mortality and MACE, irrespective of CAD complexity, unbalanced risk factors and adherence. Current treatment guidelines for patients who present with ACS favor early revascularization with PCI or CABG [24, 25]. In addition, optimal/total revascularization in patients with multi-vessel coronary artery disease has been the main focus of randomized clinical trials performed over the past years [
26]. In our study, overall revascularization rates (percutaneous coronary intervention (PCI) + coronary artery by-pass grafting (CABG)) were not significantly different between the groups. Due to higher SYNTAX score, more Roma patients received CABG as a preferred treatment strategy selected by our heart team. That lead to somewhat decreased rate of repeated PCI among Roma patients, but also explains higher stroke rate during follow-up among Roma population, which is in correlation with previous studies [
26].
Our study also showed that more Roma patients developed new onset of diabetes, and were less adherent to smoking cessation advice and recommended medical therapy. Those findings call for a more aggressive approach not only in the primary but also in secondary prevention and patient education within the treatment of cardiovascular diseases in the Roma population. Educational interventions involving patients from minorities’ background, their family members (or both) to improve adherence to medical treatment as well as other measurements for primary and secondary prevention are in great demand. There has been only few studies investigating the possible role of genetic factors associated with cardiovascular disease. Fiatal et al [
27] concluded that genetic profiling revealed an increased risk of venous thrombosis in the Hungarian Roma population whereas Piko et al [
28] suggested that genetic factors contribute to the higher prevalence of reduced HDL-C levels among Roma, which certainly calls for further research.
Limitations of our work are retrospective study design, small sample of Roma patients with insufficient number of events in the long-term to show how adherence effects future and repeated adverse events (to note are wide confidence intervals for therapy adherence in the final regression model). Although more accurate adherence to medication can be estimated directly, based on the drug or its metabolite concentration in blood and urine that was extremely difficult to achieve. Instead, we used a questionnaire with validated scales [
14]. Also, one must take in consideration that this was a self reported adherence to medical therapy based on a simple questionnaire and that a real adherence to therapy could be even lower because patients generally have a somewhat improved self-image when faced by question on adherence by their caregivers. Our data represents Roma patients seeking medical attention in ACS. We do not know if there were more patients among Roma population not presenting to local or tertiary hospitals with ACS in comparison to majority population. Also, we did not have available reliable data on pain to first medical contact time and no data on total ischemic time which would be an interesting treatment quality measure in STEMI to explore regarding the ethnicity.
5. Conclusions
In conclusion, we showed that Roma minority in Croatia, albeit having significantly more unfavorable socio-economic, clinical and angiographic characteristics, received appropriate revascularization in ACS. Consequently, we found no differences in overall mortality and MACE rates during long-term follow-up. However, Roma patients showed scarce medical therapy adherence related to higher MACE rates during initial two years of follow-up. With appropriate revascularization in ACS, and additional education on more stringent medical therapy and life-style adherence during follow-up, the ethnicity bias in ACS treatment could probably be diminished worldwide, irrespective on general social and economic progress among minorities that require substantially larger political and social action.
Author Contributions
Conceptualization, I.J. , V.H.K and P.V..; methodology, P.V. and V.H.K. ; software, Š.M., and B.S.; validation, I.J. and A.B., formal analysis, I.H.; investigation P.V., V..H.K, I..J., A.J, A.J, H.F, A.B.; data curation, A.J, A.B., H.F. and P.V. writing—original draft preparation, V.H.K and P.V.; writing—review and editing, P.V, V.H.K, I.J., A.B, H.F., I.H., A.J. and A.J.; visualization S.M. and B.S. All authors have read and agreed to the published version of the manuscript.
Funding
No funding has been received for this study.
Conflicts of interest
Authors have no conflicts of interest to declare regarding this work.
References
- Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi SKBM, AlKatheeri R, Alblooshi FMK, Almatrooshi MEAH, Alzaabi MEH, Al Darmaki RS, Lootah SNAH. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus. 2020;12:e9349. [CrossRef]
- Freund KM, Jacobs AK, Pechacek JA, White HF, Ash AS. Disparities by race, ethnicity, and sex in treating acute coronary syndromes. J Womens Health (Larchmt). 2012;21:126-132. [CrossRef]
- Hall SL, and Lorenc T. Secondary prevention of coronary artery disease. Am Fam Physician. 2010;81:289-296.
- Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–186. [CrossRef]
- Borrell LN, and Lancet EA. Race/ethnicity and all-cause mortality in US adults: revisiting the Hispanic paradox. Am J Public Health. 2012;102:836–843. [CrossRef]
- Kohler IV, and Preston SH. Ethnic and religious differentials in Bulgarian mortality, 1993-98. Popul Stud. 2011;65:91–113. [CrossRef]
- Gniwa Omezzine R, Akkara A, Abdelkafi Koubaa A, Belguith Sriha A, Rdissi A, Amamou K. Predictors of Poor Adherence to Hypertension Treatment. Tunis Med. 2019;97:564-571.
- Lauffenburger JC, Robinson JG, Oramasionwu C, Fang G. Racial/Ethnic and gender gaps in the use of and adherence to evidence-based preventive therapies among elderly Medicare Part D beneficiaries after acute myocardial infarction. Circulation. 2014;129:754-63. [CrossRef]
- Ringold D, Orenstein MA, Wilkens E. Roma in an expanding Europe: breaking the poverty cycle. Washington: The World Bank; 2005.
- Fundación Secretariado Gitano. Health and the Roma community, analysis of the situation in Europe: Bulgaria, Czech Republic, Greece, Portugal, Romania, Slovakia, Spain. Madrid: Fundacion Secretariado Gitano; 2009.
- Vozarova de Courten B, de Courten M, Hanson RL, Zahorakova A, Egyenes HP, Tataranni PA, et al. Higher prevalence of type 2 diabetes, metabolic syndrome and cardiovascular diseases in gypsies than in nongypsies in Slovakia. Diabetes Res Clin Pract. 2003;62:95-103. [CrossRef]
- Sudzinova A, Nagyova I, Rosenberger J, Studencan M, Vargova H, Middel B, van Dijk JP, Reijneveld SA. Seven years' mortality in Roma and non-Roma patients after coronary angiography. Eur J Public Health. 2015;25:765-769. [CrossRef]
- Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, Holmes DR Jr, Curzen N, Davierwala P, Noack T, et al; SYNTAX Extended Survival Investigators. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394:1325-1334. [CrossRef]
- Morisky DE, and DiMatteo MR. Improving the measurement of self-reported medication nonadherence: final response. J Clin. Epidem 2011;64:255–267. [CrossRef]
- Graham G, Xiao YY, Rappoport D, Siddiqi S. Population-level differences in revascularization treatment and outcomes among various United States subpopulations. World J Cardiol. 2016;8:24-40. [CrossRef]
- Karkabi B, Zafrir B, Jaffe R, Shiran A, Jubran A, Adawi S, Ben-Dov N, Iakobishvili Z, Beigel R, Cohen M, Goldenberg I, Klempfner R, Flugelman MY, Rubinshtein R. Ethnic Differences Among Acute Coronary Syndrome Patients in Israel. Cardiovasc Revasc Med. 2020 Nov;21(11):1431-1435. [CrossRef]
- Wechkunanukul K, Grantham H, Damarell R, Clark RA. The association between ethnicity and delay in seeking medical care for chest pain: a systematic review. JBI Database System Rev Implement Rep. 2016 Jul;14(7):208-35. [CrossRef] [PubMed]
- Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016;CD001800. [CrossRef]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. [CrossRef]
- Dzayee DAM, Moradi T, Beiki O, Alfredsson L, Ljung R. Recommended drug use after acute myocardial infarction by migration status and education level. Eur J Clin Pharmacol 2015;71:499–505. [CrossRef]
- Ringba¨ck Weitoft G, Ericsson O, Lo¨froth E, Rose´n M. Equal access to treatment? Population-based follow-up of drugs dispensed to patients after acute myocardial infarction in Sweden. Eur J Clin Pharmacol 2008;64:417–424. [CrossRef]
- Frederiksen HW, Zwisler AD, Johnsen SP, Öztürk B, Lindhardt T, Norredam M. Differences in initiation and discontinuation of preventive medications and use of non-pharmacological interventions after acute coronary syndrome among migrants and Danish-born. Eur Heart J. 2018 Jul 1;39(25):2356-2364. [CrossRef] [PubMed]
- Graham G. Racial and Ethnic Differences in acute coronary syndrome and myocardial infarction within the United States: from demographics to outcomes. Clin Cardiol. 2016;39:299-306. [CrossRef]
- Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, et al. ESC Scientific Document Group, 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal, 2020; ehaa575. [CrossRef]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. [CrossRef]
- Ibrahimov F, Yilmaz Y, Ismayilov I, Musayev K, Musayev OO, Alasgarli S, Shahbazova S, Isgenderova M, Jahangirov T. Comparing 5-year outcomes of aorta-coronary bypass surgery and percutaneous coronary intervention performed with new-generation drug-eluting stents in non-diabetic patients with multivessel acute coronary syndrome patients and intermediate syntax score. Medeni Med J. 2020;35(2):121-127. [CrossRef]
- Fiatal S, Pikó P, Kósa Z, Sándor J, Ádány R. Genetic profiling revealed an increased risk of venous thrombosis in the Hungarian Roma population. Thromb Res. 2019 Jul;179:37-44. Epub 2019 May 2. [CrossRef] [PubMed]
- Pikó P, Fiatal S, Kósa Z, Sándor J, Ádány R. Genetic factors exist behind the high prevalence of reduced high-density lipoprotein cholesterol levels in the Roma population. Atherosclerosis. 2017 Aug;263:119-126. Epub 2017 May 26. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).