Submitted:
28 February 2025
Posted:
28 February 2025
You are already at the latest version
Abstract
In dementia care, access to effective psychosocial interventions is often addressed by evidence-based guidelines for care providers. However, it is unclear if current guidelines consider personal characteristics that may impact intervention effectiveness. This study investigates if, and within what framing, dementia care guidelines in Europe address what is effective and for whom. A review of 47 guidelines from 12 European countries was conducted. Content analysis focused on: i) if guidelines recommended specific psychosocial interventions, and how guidelines referred to ii) social health, iii) intersection of social positioning, and iv) inequities in care or outcomes. Thirty-five guidelines (74%) recommended specific psychosocial interventions. Around half referenced aspects of social health and of intersectionality. Thirteen guidelines (28%) referenced inequities. Social health was not explicitly recognised as a mechanism of psychosocial interventions. Only age and comorbidity were consistently considered to impact interventions’ effectiveness. Inequities were acknowledged to arise from within-country regional variations and individual economic status but not linked to (intersectional) individual societal positions such as sex and/or gender, sexuality, and/or religion. Results between European countries were heterogeneous. Current guidelines offer little insight into what works for whom. Policymakers and guideline developers should work with researchers, generating and translating evidence into policy.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Identification of Guidelines
2.3. Data Extraction
| Category | Definition and sub-categories for data extraction |
|---|---|
| Guideline characteristics | Country, title |
| Psychological and social interventions | Following Sikkes et al. (2021): non-pharmacological interventions cover a diverse and broad range of intervention categories including, for instance, cognitive training, physical exercise, dietary treatments, art-oriented therapy, and reminiscence therapy (Scales et al., 2018); “any theoretically based, nonchemical, focused and replicable intervention, conducted with the patient or the caregiver, which potentially provided some relevant benefit” (Olazaran et al., 2010, p.162)
|
| Social health | Health as the ability to adapt and self-manage (Huber et al., 2011). Social health specifically is characterized by i) Capacity to fulfil one’s potential and obligations: the ability of a person (living with or caring for a person with dementia) to function in the society according to their competencies and talents (‘potentials’) in the best possible way and to meet social demands (‘obligations’) on a micro and macro societal level; ii) Manage life with some degree of independence: ability to manage life with some degree of independence, can be operationalized as the ability to preserve autonomy and to solve problems in daily life, as well as to adapt to and cope with the practical and emotional consequences of dementia; iii) Participation in social activities:The act of being occupied or involved with meaningful activities and social interactions and having social ties and relationships, which are meaningful to the person living with dementia themselves (Dröes et al., 2017).
|
| Intersectionality | Intersectionality, as a theory and methodology, acknowledges the complexity and multidimensionality of people’s lives, and highlights that a person - due to her social positioning (e.g. socio-economic factors, sex & gender, ethnicity) - may experience health-related stigma and other disadvantages (Collins et al., 2021; Rai et al., 2020; King et al., 2020).
|
| Inequity / inequality | Inequitable care is the result of ignoring differences or inequalities in health status or in the distribution of health services, or access to health and social care between different population groups (Collins et al., 2021; Rai et al., 2020; Dahlgren & Whitehead, 2007).
|
2.4. Data Analysis and Synthesis
2.5. Public Involvement
3. Results
3.1. Recommended Psychological and Social Interventions
| AT | BE | CZ | DK | DE | ES | IE | IT | NL | PL | PT | UK | Total | |
| Guideline(s) identified (n) | 1 | 1 | 6 | 4 | 4 | 7 | 6 | 1 | 4 | 5 | 3 | 5 | 47 |
| Guideline(s) recommending psychological or social interventions (n) | 0 | 1 | 3 | 4 | 3 | 6 | 4 | 1 | 3 | 2 | 3 | 5 | 35 |
| (Creative) art therapy | x | x | x | 3 | |||||||||
| Assistive technology/ aids/ telecare | x | x | x | 3 | |||||||||
| Care planning | x | 1 | |||||||||||
| Carer interventions (incl. behavioral) | x | x | 2 | ||||||||||
| (Cognitive) behavioral therapy-based intervention/ modification | x | x | x | x | x | x | x | 7 | |||||
| Cognitive rehabilitation (therapy) (also in groups) | x | x | x | x | x | x | x | x | 8 | ||||
| Cognitive restructuring | x | 1 | |||||||||||
| Cognitive stimulation (therapy) (incl. Cogs club) | x | x | x | x | x | x | x | x | x | 9 | |||
| Cognitive training | x | x | x | x | x | x | x | x | 8 | ||||
| Compensatory strategies | x | 1 | |||||||||||
| Conversational coaching/ communication training | x | x | 2 | ||||||||||
| Counselling/ psychotherapeutic interventions | x | x | x | x | 4 | ||||||||
| Dramatherapy | x | x | 2 | ||||||||||
| Dance therapy | x | x | x | x | 4 | ||||||||
| Doll therapy | x | 1 | |||||||||||
| Environmental assessment, modification, and interventions | x | x | x | 3 | |||||||||
| Family/ interpersonal therapy | x | x | x | 3 | |||||||||
| Horticulture therapy/ therapeutic gardens | x | x | 2 | ||||||||||
| Life story work/ review | x | x | x | 3 | |||||||||
| Meeting Center Support Programme | x | 1 | |||||||||||
| Mindfulness | x | x | 2 | ||||||||||
| Music therapy | x | x | x | x | x | x | x | x | 8 | ||||
| Nutritional care | x | 1 | |||||||||||
| Occupational therapy-based interventions | x | x | x | x | x | 5 | |||||||
| Personal validation/ compassion therapy | x | x | x | x | 4 | ||||||||
| Pet-/ animal-assisted therapy | x | x | x | x | 4 | ||||||||
| Physical activity, exercise, fitness, psychomotor therapy (incl. supervised) | x | x | x | x | x | x | x | 7 | |||||
| Physiotherapy | x | x | 2 | ||||||||||
| Psychoeducation (also for carers) | x | x | x | x | x | x | 6 | ||||||
| Reality orientation | x | x | 2 | ||||||||||
| Reminiscence therapy (incl. group format) | x | x | x | x | x | x | x | x | x | x | 10 | ||
| Sensory stimulation therapy (incl. aroma, touch, massage, light, bathing, snoezelen) | x | x | x | x | x | x | x | x | 8 | ||||
| Sleep hygiene | x | x | 2 | ||||||||||
| Speech and language therapy (incl. speaking, chewing, swallowing, breathing exercises) | x | x | x | 3 | |||||||||
| Yoga | x | 1 | |||||||||||
| Different interventions recommended/ country (n) | N/A | 1 | 13 | 10 | 12 | 15 | 22 | 10 | 9 | 12 | 11 | 18 | |
| Guideline(s) with reference(s) to social health (n) | N/A | 0 | 1 | 2 | 2 | 7 | 6 | 0 | 2 | 1 | 1 | 5 | 27 |
| Guideline(s) with reference(s) to intersectionality (n) | N/A | 0 | 1 | 2 | 3 | 7 | 6 | 1 | 1 | 1 | 2 | 4 | 28 |
| Guideline(s) with reference(s) to inequity (n) | N/A | 0 | 0 | 0 | 0 | 1 | 4 | 1 | 2 | 0 | 1 | 4 | 13 |
3.2. ‘Social Health’ in Guidelines on Psychological and Social Interventions for Dementia
3.3. ‘Intersectionality’ in Guidelines on Psychological and Social Interventions for Dementia
3.4. ‘Inequity’ in Guidelines on Psychological and Social Interventions for Dementia
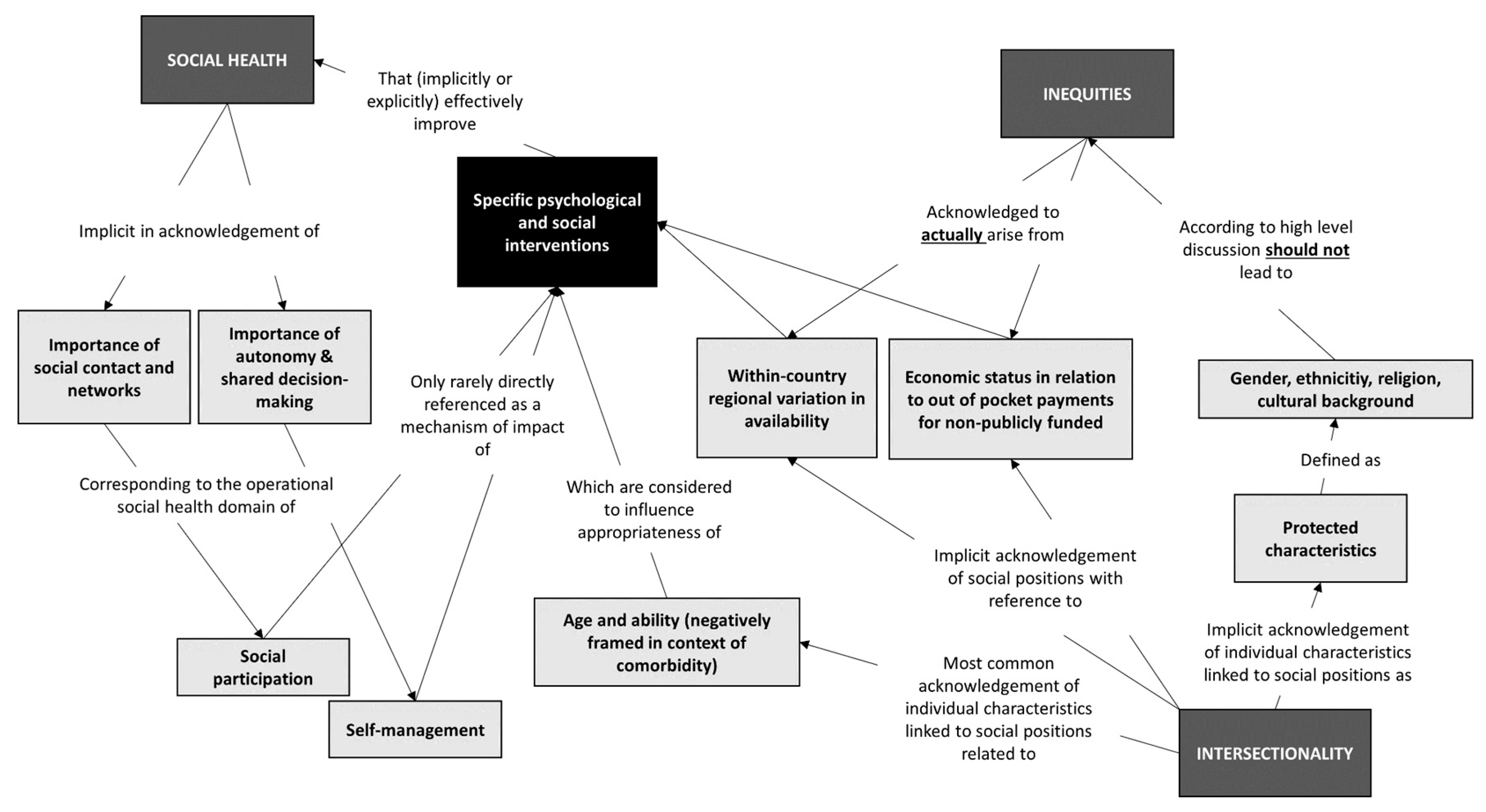
3.5. Relational Analysis: Concept Mapping
3.6. Discussion
3.7. Towards a Biopsychosocial Approach to Dementia Care Across Europe
3.8. Fragmented Use of Conceptual Frameworks Regarding what Is Effective for Whom
3.9. Inequity in Dementia Care Arising from Differences in Guideline and Service Provision
3.10. Public Involvement Perspectives
3.11. Recommendations for Future Research and Policy Making
Recommendations for future research and policy making to improve equitable access to effective dementia care in Europe:
|
3.12. Strength and Limitations
3.13. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alzheimer Europe (2019) Overcoming ethical challenges affecting the involvement of people with dementia in research: recognising diversity and promoting inclusive research .
- Alzheimer Europe 2020: https://www.alzheimer-europe.org/sites/default/files/alzheimer_europe_dementia_as_a_european_priority_%E2%80%93_a_policy_overview_2020.pdf.
- Bentley, A., Morgan, T., Salifu, Y., & Walshe, C. (2021). Exploring the experiences of living with Lewy body dementia: An integrative review. Journal of Advanced Nursing, 77(12), 4632-4645.
- Blotenberg I, Boekholt M, Michalowsky B, Platen M, Rodriguez FS, Teipel S, Hoffmann W, Thyrian JR. What influences life expectancy in people with dementia? Social support as an emerging protective factor. Age Ageing. 2024 Mar 1;53(3):afae044. [CrossRef]
- Buckley, J. S., & Salpeter, S. R. (2015). A risk-benefit assessment of dementia medications: systematic review of the evidence. Drugs & aging, 32, 453-467. [CrossRef]
- Budak, K. B., Atefi, G., Hoel, V., Laporte Uribe, F., Meiland, F., Teupen, S.,... & Roes, M. (2023). Can technology impact loneliness in dementia? A scoping review on the role of assistive technologies in delivering psychosocial interventions in long-term care. Disability and Rehabilitation: Assistive Technology, 18(7), 1107-1119. [CrossRef]
- Cheng, S. T., Li, K. K., Losada, A., Zhang, F., Au, A., Thompson, L. W., & Gallagher-Thompson, D. (2020). The effectiveness of nonpharmacological interventions for informal dementia caregivers: An updated systematic review and meta-analysis. Psychology and Aging, 35(1), 55. [CrossRef]
- Collins, P. H., da Silva, E. C. G., Ergun, E., Furseth, I., Bond, K. D., & Martínez-Palacios, J. (2021). Intersectionality as Critical Social Theory. Contemporary Political Theory, 20(3), 690-725. [CrossRef]
- Dahlgren G., & Whitehead M. (2007). European strategies for tackling social inequalities in health: levelling up part 2. Copenhagen, DK: WHO Regional Office for Europe.
- Dinand, C., Nover, S. U., Holle, D., Zischka, M., & Halek, M. (2016). What is known about the subjective needs of people with behavioural variant frontotemporal dementia? A scoping review. Health & Social Care in the Community, 24(4), 375-385. [CrossRef]
- Dröes, R. M., Chattat, R., Diaz, A., Gove, D., Graff, M., Murphy, K.,... & INTERDEM sOcial Health Taskforce. (2017). Social health and dementia: a European consensus on the operationalization of the concept and directions for research and practice. Aging & mental health, 21(1), 4-17. [CrossRef]
- Eurostat. (2024). Population and population change statistics. Eurostat, available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_and_population_change_statistics#Source_data_for_tables_and_graphs.
- Frederiksen, K. S., Cooper, C., Frisoni, G. B., Frölich, L., Georges, J., Kramberger, M. G.,... & Waldemar, G. (2020). A European Academy of Neurology guideline on medical management issues in dementia. European journal of neurology, 27(10), 1805-1820. [CrossRef]
- Gaugler, J. E., Reese, M., & Mittelman, M. S. (2018). The effects of a comprehensive psychosocial intervention on secondary stressors and social support for adult child caregivers of persons with dementia. Innovation in Aging, 2(2), igy015. [CrossRef]
- Gustafson, P., Abdul Aziz, Y., Lambert, M., Bartholomew, K., Rankin, N., Fusheini, A.,... Crengle, S. (2023). A scoping review of equity-focused implementation theories, models and frameworks in healthcare and their application in addressing ethnicity-related health inequities. Implementation Science, 18(1), 51. [CrossRef]
- Harding, E., Sullivan, M. P., Woodbridge, R., Yong, K. X., McIntyre, A., Gilhooly, M. L.,... & Crutch, S. J. (2018). ‘Because my brain isn’t as active as it should be, my eyes don’t always see’: a qualitative exploration of the stress process for those living with posterior cortical atrophy. BMJ open, 8(2), e018663.
- Hartmann, J., Roßmeier, C., Riedl, L., Dorn, B., Fischer, J., Slawik, T.,... & Diehl-Schmid, J. (2021). Quality of life in advanced dementia with late onset, young onset, and very young onset. Journal of Alzheimer's Disease, 80(1), 283-297. [CrossRef]
- Holthe, T., Halvorsrud, L., & Lund, A. (2022). Digital assistive technology to support everyday living in community-dwelling older adults with mild cognitive impairment and dementia. Clinical Interventions in Aging, 519-544. [CrossRef]
- Huber, M., Knottnerus, J. A., Green, L., Van Der Horst, H., Jadad, A. R., Kromhout, D.,... & Smid, H. (2011). How should we define health?. Bmj, 343.
- Godard-Sebillotte, C., Navani, S., Hacker, G., & Vedel, I. (2024). Considering inequities in national dementia strategies: breadth, depth, and scope. International Journal for Equity in Health, 23(1), 75. [CrossRef]
- James, T., Mukadam, N., Sommerlad, A., Pour, H. R., Knowles, M., Azocar, I., & Livingston, G. (2022). Protection against discrimination in national dementia guideline recommendations: A systematic review. PLoS Medicine, 19(1), e1003860. [CrossRef]
- Jonsson, L., Wimo, A., Handels, R., Johansson, G., Boada, M., Engelborghs, S., Frolich, L., Jessen, F., Kehoe, P. G., Kramberger, M., de Mendonca, A., Jean Ousset, P., Scarmeas, N., Jelle Visser, P., Waldemar, G., & Winblad, B. (2023). The affordability of lecanemab, an amyloid-targeting therapy for Alzheimer's disease: an EADC-EC viewpoint. The Lancet Regional Health Europe, 29, 100657. [CrossRef]
- King, Almack, Jones (Ed.) (2020). Intersections of ageing, gender and sexualities. Multidisciplinary international perspectives. Bristol University Press.
- Lech, S., O’Sullivan, J. L., Drewelies, J., Herrmann, W., Spang, R. P., Voigt-Antons, J. N.,... & Gellert, P. (2021). Dementia care and the role of guideline adherence in primary care: cross-sectional findings from the DemTab study. BMC geriatrics, 21(1), 717. [CrossRef]
- Lim, R. H., Sharmeen, T., & Donyai, P. (2022). How do people with dementia make sense of their medications? An interpretative phenomenological analysis study. International Journal of Geriatric Psychiatry, 37(2). [CrossRef]
- Livingston, G., Huntley, J., Liu, K. Y., Costafreda, S. G., Selbæk, G., Alladi, S.,... & Mukadam, N. (2024). Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. The Lancet, 404(10452), 572-628. [CrossRef]
- Noel-Storr, A. H., Flicker, L., Ritchie, C. W., Nguyen, G. H., Gupta, T., Wood, P.,... & McShane, R. (2013). Systematic review of the body of evidence for the use of biomarkers in the diagnosis of dementia. Alzheimer's & Dementia, 9(3), e96-e105. [CrossRef]
- Ngo, J., & Holroyd-Leduc, J. M. (2014). Systematic review of recent dementia practice guidelines. Age and ageing, 44(1), 25-33. [CrossRef]
- Nguyen, H. V., Mital, S, Knopman, D. S., & Caleb Alexander, G. (2024). Cost-Effectiveness of Lecanemab for Individuals With Early-Stage Alzheimer Disease. Neurology, 102(7).
- Noone, D., Stott, J., Aguirre, E., Llanfear, K., & Spector, A. (2019). Meta-analysis of psychosocial interventions for people with dementia and anxiety or depression. Aging & mental health, 23(10), 1282-1291. [CrossRef]
- McDermott, O., Charlesworth, G., Hogervorst, E., Stoner, C., Moniz-Cook, E., Spector, A.,... & Orrell, M. (2019). Psychosocial interventions for people with dementia: a synthesis of systematic reviews. Aging & mental health, 23(4), 393-403. [CrossRef]
- Millenaar, J. K., de Vugt, M. E., Bakker, C., van Vliet, D., Pijnenburg, Y. A., Koopmans, R. T., & Verhey, F. R. (2016). The impact of young onset dementia on informal caregivers compared with late onset dementia: results from the NeedYD study. The American Journal of Geriatric Psychiatry, 24(6), 467-474. [CrossRef]
- Olazarán, J., Reisberg, B., Clare, L., Cruz, I., Peña-Casanova, J., Del Ser, T.,... & Muñiz, R. (2010). Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dementia and geriatric cognitive disorders, 30(2), 161-178.
- Panagiotidou, N., Dhooper, J., Funk, M., Drew, N., Seeher, K., Dua, T., & Orrell, M. (2024). Towards Establishing Quality Standards on Human Rights for Services in Dementia Care. International Journal of Older People Nursing, 19(5), e12643. [CrossRef]
- Pappadà, A., Chattat, R., Chirico, I., Valente, M., & Ottoboni, G. (2021). Assistive technologies in dementia care: an updated analysis of the literature. Frontiers in psychology, 12, 644587. [CrossRef]
- Pinto-Bruno, Á. C., García-Casal, J. A., Csipke, E., Jenaro-Río, C., & Franco-Martín, M. (2017). ICT-based applications to improve social health and social participation in older adults with dementia. A systematic literature review. Aging & Mental Health, 21(1), 58-65. [CrossRef]
- Pot, A. M., Rabheru, K., & Chew, M. (2023). Person-centred long-term care for older persons: a new Lancet Commission. The Lancet, 401(10390), 1754-1755. [CrossRef]
- Rai, S. S., Peters, R. M., Syurina, E. V., Irwanto, I., Naniche, D., & Zweekhorst, M. B. (2020). Intersectionality and health-related stigma: insights from experiences of people living with stigmatized health conditions in Indonesia. International journal for equity in health, 19, 1-15. [CrossRef]
- Rausch, A., Caljouw, M. A., & van der Ploeg, E. S. (2017). Keeping the person with dementia and the informal caregiver together: A systematic review of psychosocial interventions. International Psychogeriatrics, 29(4), 583-593. [CrossRef]
- Rosen, C. S., Chow, H. C., Greenbaum, M. A., Finney, J. F., Moos, R. H., Sheikh, J. I., & Yesavage, J. A. (2002). How well are clinicians following dementia practice guidelines?. Alzheimer Disease & Associated Disorders, 16(1), 15-23. [CrossRef]
- Sorbi, S., Hort, J., Erkinjuntti, T., Fladby, T., Gainotti, G., Gurvit, H.,... & EFNS Scientist Panel on Dementia and Cognitive Neurology. (2012). EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. European Journal of Neurology, 19(9), 1159-1179. [CrossRef]
- Scales, K., Zimmerman, S., & Miller, S. J. (2018). Evidence-based nonpharmacological practices to address behavioral and psychological symptoms of dementia. The Gerontologist, 58(suppl_1), S88-S102. [CrossRef]
- Sikkes, S. A., Tang, Y., Jutten, R. J., Wesselman, L. M., Turkstra, L. S., Brodaty, H.,... & Bahar-Fuchs, A. (2021). Toward a theory-based specification of non-pharmacological treatments in aging and dementia: focused reviews and methodological recommendations. Alzheimer's & Dementia, 17(2), 255-270. [CrossRef]
- Skivington, K., Matthews, L., Simpson, S. A., Craig, P., Baird, J., Blazeby, J. M.,... & Moore, L. (2021). A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. bmj, 374. [CrossRef]
- Torossian, M. R. (2021). The dignity of older individuals with Alzheimer’s disease and related dementias: A scoping review. Dementia, 20(8), 2891-2915.
- Thijssen, E. H., Verberk, I. M., Kindermans, J., Abramian, A., Vanbrabant, J., Ball, A. J.,... & Teunissen, C. E. (2022). Differential diagnostic performance of a panel of plasma biomarkers for different types of dementia. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring, 14(1), e12285.
- United Nations Department of Economic and Social Affairs Population Division. (2024). 2024 Revision of World Population Prospects. United Nations, Available from: https://population.un.org/wpp/.
- Vasse, E., Vernooij-Dassen, M., Cantegreil, I., Franco, M., Dorenlot, P., Woods, B., & Moniz-Cook, E. (2012). Guidelines for psychosocial interventions in dementia care: a European survey and comparison. International journal of geriatric psychiatry, 27(1), 40-48. [CrossRef]
- Vernooij-Dassen, M., Moniz-Cook, E., Verhey, F., Chattat, R., Woods, B., Meiland, F.,... & de Vugt, M. (2021). Bridging the divide between biomedical and psychosocial approaches in dementia research: the 2019 INTERDEM manifesto. Aging & Mental Health, 25(2), 206-212. [CrossRef]
- Vernooij-Dassen, M., Verspoor, E., Samtani, S., Sachdev, P. S., Ikram, M. A., Vernooij, M. W.,... & Wolf-Ostermann, K. (2022). Recognition of social health: A conceptual framework in the context of dementia research. Frontiers in Psychiatry, 13, 1052009. [CrossRef]
- Vinay, R., & Biller-Andorno, N. (2023). A critical analysis of national dementia care guidances. Health policy, 130, 104736. [CrossRef]
- Waldemar, G., Dubois, B., Emre, M., Georges, J., McKeith, I. G., Rossor, M.,... & Winblad, B. (2007). Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline. European Journal of Neurology, 14(1), e1-e26. [CrossRef]
- Waldorff, F. B., Almind, G., Mäkelä, M., Møller, S., & Waldemar, G. (2003). Implementation of a clinical dementia guideline. Scandinavian journal of primary health care, 21(3), 142-147. [CrossRef]
- World Health Organization. (2017). Global action plan on the public health response to dementia 2017–2025. World Health Organization.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





