1. Introduction
Managing tinnitus and consequently improving the quality of life in patients with otosclerosis presents a significant clinical challenge, as recognized by many otologists and audiologists. Over the years, various therapeutic strategies have been investigated, with recent studies contributing to this area of research. Surgical intervention, particularly stapedectomy, has demonstrated efficacy in reducing tinnitus symptoms associated with otosclerosis [
1]. However, the long-term success of such interventions varies among individuals, particularly due to the availability of multiple surgical techniques [
2] and disease progression. Consequently, further research is required to establish standardized treatment protocols for tinnitus management in this target population group. The challenge is especially significant in patients who are either ineligible for or choose not to undergo surgery. Considering available research, a multidisciplinary approach combining both surgical and non-surgical modalities appears to offer the most promising results in managing tinnitus in otosclerosis patients [1, 3, 4].
In this study, we aim to present the outcomes of tinnitus management in otosclerosis patients who opted not to undergo surgical treatment. Data were collected over a 5-year period from patients in the Otorhinolaryngology Department at The Emergency County Hospital in Craiova, Romania. Patients received oral calcium and fluoride supplements, and tinnitus severity was monitored using the Tinnitus Handicap Inventory (THI) [
5]. To ensure patient safety and monitor for potential adverse effects of calcium and fluoride supplementation, several blood tests were conducted. Liver function was assessed by measuring hepatic enzymes, including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALKP), and acid phosphatase (ACP), as elevated levels of these enzymes may indicate fluoride-induced liver toxicity [
6]. Additionally, serum fluoride levels were measured to evaluate fluoride exposure and potential toxicity [
7]. Diagnostic and follow-up assessments were conducted using pure tone audiometry and impedance tympanometry.
2. Materials and Methods
The current study was conducted between May 2020 and March 2024 within our hospital. The diagnosis of otosclerosis in patients was established through a comprehensive assessment utilizing ear (otic) endoscopy to rule out any tympanic membrane pathology, pure tone audiometry, impedance tympanometry, and stapedial reflex testing [
8]. Transient evoked otoacoustic emissions [
8] were used for differential diagnosis in cases that were clinically ambiguous or presented diagnostic uncertainty.
Out of a total number of 252 otosclerosis patients diagnosed within our medical facility during these 5 years, 176 patients opted not to undergo surgical treatment. Of these, 128 were treated for tinnitus using oral calcium and fluoride supplementation and were subsequently included in the study. The remaining 48 patients were not included in the study, either due to the absence of tinnitus symptoms, ongoing liver disease or anemia, or their refusal to participate. Patient consent for participation in the study was obtained for each individual and attached to their patient files at the date of diagnosis.
Prior to inclusion in the study and initiation of treatment, a computed tomography (CT) scan of the temporal bone [9, 10] was conducted to accurately identify and characterize the typical lesions within the middle ear and cochlear endosteum. Patients enrolled in the study were evaluated for potential prior exposure to fluoride and underwent routine measurements of serum AST, ALT, ALKP, ACP, blood urea and creatinine levels [
6]. This was done to assess for any pre-existing liver or kidney dysfunction, which could contraindicate further administration of calcium and fluoride. As part of the initial blood screening, serum fluoride levels and hemoglobin levels were also assessed. Additionally, patients were questioned about any history of pain or swelling in the joints, renal disorders and calcium oxalate kidney stones, as well as any signs of synovitis or plantar fasciitis [
11]. The final step prior to admission and start of supplementation involved completing the Tinnitus Handicap Inventory (THI) questionnaire and assessing tinnitus severity using a grading scale established by previous research [
5].
These patients were monitored over a three-month period, after which their tinnitus symptoms and treatment responses were systematically reassessed. During this period, hearing levels were not reassessed unless patients presented with new complaints. Significant adverse reactions, such as skin rashes, recurrent vomiting, unexplained fatigue [
11] (indicative of potential anemia), and painful or tender joints, were closely monitored through monthly patient check-ins. The three-month evaluation consisted of repeating pure tone audiometry, conducting the full bloodwork panel, and having patients retake the Tinnitus Handicap Inventory (THI). Patients who demonstrated a reduction in their total THI score were instructed to continue calcium and fluoride supplementation at a reduced dosage. In contrast, patients with no improvement in their scores were discontinued from the supplements and underwent a multidisciplinary reevaluation [
12] to determine an alternative course of therapy.
The selected supplement formulation was Florical (Mericon Industries, Inc., USA). Florical consists of capsules containing 3.75 mg of sodium fluoride and 145 mg of calcium carbonate as the active ingredients. The inactive ingredients included: microcrystalline cellulose (commonly utilized filler and binder that maintains the structural integrity of the capsule), magnesium stearate (an anti-caking agent designed to prevent the ingredients from adhering during manufacturing), silicon dioxide (a flow agent used to enhance the consistency of the powder and prevent clumping), gelatin (the capsule shell is composed of gelatin, facilitating the oral delivery of the active ingredients and is typically sourced from animal products). Patients enrolled in the study were instructed to take three capsules daily, one at the start of each meal. For patients who opted to continue the supplementation after the study was concluded, the recommended dose was one capsule per day.
3. Results
3.1. THI Score Results
The study cohort involves 128 patients diagnosed with otosclerosis, all of whom opted for conservative management of otosclerosis instead of undergoing surgical intervention. The cohort presented with either conductive or mixed hearing loss, with varying degrees of severity ranging from mild to moderate (both 1
st and 2
nd degrees of moderate hearing loss) [
13]. To assess the impact of tinnitus, all patients completed the Tinnitus Handicap Inventory (THI) questionnaire prior to beginning the oral supplementation. The THI scores obtained, which provide a measure of tinnitus-related disability, were categorized into mild (score 18-36), moderate (score 38-56), and severe (score 58-76) levels, according to pre-existent recommendations [
14]. After the 3 months of supplementation, some patients transitioned into the very mild category of tinnitus (score 0-16). Based on existing literature we chose to consider clinical improvement of tinnitus as a decrease of 10 points or more in the THI scores of patients [15, 16]. Variations under 10 points were also considered to be positive or negative impact but were attributed to fluctuations of tinnitus within its chronic state or because of the primary hearing pathology (otosclerosis). An increase in scores of 10 points or more would also be considered a clinically significant worsening of tinnitus.
Before oral supplementation, 41 patients had mild THI scores (mean score in the mild group 24), indicating tinnitus would occasionally interfere with sleep but not with daily activities. Another 60 patients reported a moderate THI (mean score in the moderate group 46), suggesting a more pronounced presence of tinnitus which was perceived even in the presence of environmental sound; the interference with sleep and relaxing activities is not infrequent. The remaining 27 patients exhibited severe THI scores (mean score in the severe group 62), reflecting a significant handicap due to tinnitus. It was continuously perceived and hardly masked by external noise. Most of these patients complained of an altered sleep cycle and compromised relaxing activities. These initial assessments served as the baseline for evaluating the efficacy of the calcium and fluoride supplementation over the following three months.
After 3 months, in the mild group, which consisted of 41 patients, 15 patients (36.59%) achieved a clinically significant reduction (10 points or greater decrease in the THI score). Only one patient showed no change in their scores, and no patients reported increased THI scores. 40 out of 41 patients (97.56%) experienced a decrease in THI scores, confirming a positive effect on tinnitus, even if 32 patients (78.05%) of patients had only minor changes (under 10 points), meaning their THI scores remained within expected variability of tinnitus (physiological fluctuation). 13 patients transitioned to the very mild category of tinnitus after oral supplementation, with final THI scores ranging from 10 to 16. The very mild category of tinnitus is defined by THI pre-existing data as perceived only in silence and easily masked [
5]. It does not interfere with sleep or with daily activities and its the lowest score classifiable by the THI. No patients in this group displayed any changes in their audiometry measured hearing thresholds, but it is worth noting that all patients in the group had mild and 1st degree moderate conductive hearing loss (
Table 1).
In the moderate group, consisting of 60 patients, only 2 patients (3.39%) reached the clinically significant reduction threshold (at least 10 points). 34 patients (57.63%) showed some improvement in scores, but the reduction was mild (under 10 points), falling into the category of physiological fluctuation. 14 patients (23.73%) remained completely stationary, with no change in THI scores. 9 patients (15.25%) showed a small increase in THI scores, but did not exceed 10 points. One female patient was removed from the study and was advised off Florical after describing tender elbow and shoulder joints and pain when lifting weights during the first month of supplementation. 6 patients transitioned into the mild category of tinnitus and one patient to the severe category after the 3 months. While the overall response to supplementation was positive, this group had low decreases in scores and more patients with stationary or heightened scores compared to the mild group. Although the overall response was positive (decreasing scores), there was also greater variability in responses and little scores with a decrease of 10 points or greater. Most patients in this group had moderate conductive or mixed hearing loss (1st and 2nd degrees) and the hearing thresholds were not affected during the 3 months of supplementention (
Table 2).
In the severe group, which included 27 patients, no patients experienced a reduction or an increase in their THI scores equal or greater to 10 points. A number of 6 patients (22.22%) remained completely stationary. The severe group exhibited the least favorable response to treatment, reflected in the low variation of scores. 11 patients (40.74%) showed improvement in THI scores, but none were large enough to be clinically significant (equal or above 10 points). 10 patients (37.04%) experienced worsening of THI scores, though none exceeded a growth equal or larger than 10 points. Within the 10 point decrease, 4 patients transitioned from the severe tinnitus group to the moderate tinnitus group with scores of 56 and 54. Patients in this group had 2nd degree mixed moderate hearing loss and some of the patients with increasing scores displayed a small increase of 5 to 10 dB in their air conduction thresholds in 4 and 8 kHz (
Table 3).
Patients included in the study did not experience uncomfortable side effects from the high dose of Florical, except for one female patient from the moderate tinnitus group who complained of tender and swollen joints and was removed from supplementation. Liver and kidney tests during the supplementation showed a steady increase in monitored serum enzyme levels but without reaching values outside of normal ranges. We did not register any patients who developed anemia or other types of toxicity.
3.2. Statistical Analysis of THI Scores
After obtaining the final THI scores, we employed statistical tests to determine whether the supplementation led to significant reductions in THI scores and whether these reductions varied across the severity groups. The dataset included 127 patients, categorized into three groups: the mild tinnitus group (total n = 41), the moderate tinnitus group (n = 59) and the severe tinnitus group (n = 27). The primary outcome variable, THI score variation (named ‘thi_diff’), was calculated as the difference between the THI score after supplementation and the THI score before supplementation. Negative values indicate an improvement in tinnitus severity.
Based on our established 10 grade score improvement, a binary variable, named ‘significant_thi’, was generated to classify cases where THI scores decreased by 9 or more points, indicating a clinically significant reduction in tinnitus severity. Statistical analyses included descriptive statistics, t-tests, ANOVA, and post-hoc Bonferroni tests to compare changes in THI scores across groups. Shapiro-Wilk tests were used to assess normality of data distribution.
3.2.1. Descriptive Statistics of THI Score Variation
The mean and standard deviation of THI score changes were computed for each group and analyzed (
Table 4).
3.2.2. Normality Test (Shapiro-Wilk)
Shapiro-Wilk tests confirmed that THI score variations in each group followed a normal distribution (p > 0.05 for all groups), justifying the use of parametric tests.
3.2.3. One-Way ANOVA and Post-hoc Comparisons
A one-way ANOVA was conducted to compare THI score variations among groups:
F(2,124) = 51.52, p < 0.0001, indicating a statistically significant difference in THI reductions across severity groups.
-
Post-hoc Bonferroni tests revealed;
Mild vs. Moderate tinnitus: p < 0.0001 (significant difference);
Mild vs. Severe tinnitus: p < 0.0001 (significant difference);
Moderate vs. Severe tinnitus: p = 0.077 (not statistically significant).
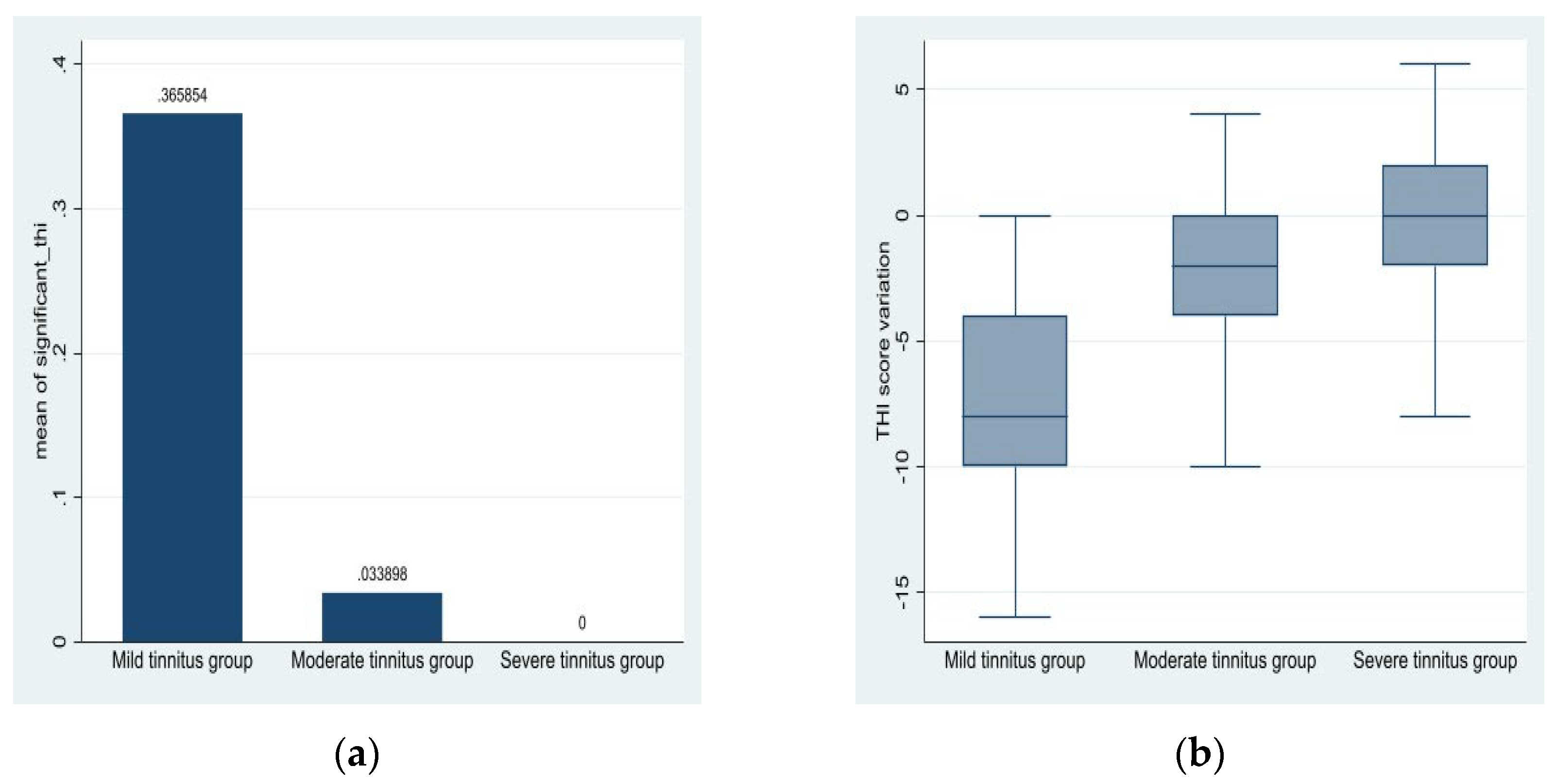
3.2.4. Proportion of Patients with Significant THI Reduction
The proportion of clinically significant THI scores reduction is displayed in
Table 5. The clinically significant reduction is seen in the Mild tinnitus group and can be identified within the Moderate group as well. The Severe group did not exhibit any clinically significant reduction in their scores.
Table 5.
Significant THI Reduction.
Table 5.
Significant THI Reduction.
| Group |
Total Patients |
% Significant Reduction |
| Mild tinnitus |
41 |
36.59% |
| Moderate tinnitus |
59 |
3.39% |
| Severe tinnitus |
27 |
0.00% |
Figure 1.
(a) Mean of the binary variable ‘significant_thi’ per group; (b) THI score variation per group.
Figure 1.
(a) Mean of the binary variable ‘significant_thi’ per group; (b) THI score variation per group.
These findings indicate that supplementation efficacy decreases as tinnitus severity increases. Patients in the mild tinnitus group experienced significantly greater reductions in THI scores than those in moderate or severe groups. The results, besides the clinical improvement stated in the questionnaires, are supported by statistical significance in ANOVA and post-hoc comparisons, reinforcing the idea that greater initial tinnitus severity correlates with lower responses to Florical administration. Florical seems to have a good impact on tinnitus in patients with lower tinnitus scores.
4. Discussion
The Tinnitus Handicap Inventory (THI) is a widely used tool to assess the impact of tinnitus on patients' lives, including patients diagnosed with otosclerosis, especially since tinnitus is a common symptom in otosclerosis, affecting 65-90% of patients and often co-occurring with hearing loss [
17]. For our given topic, we chose THI in order to identify specific complaints and report the severity of tinnitus symptoms in our cohort of patients. The literature indicates that otosclerosis patients often report a range of issues on the THI, with certain items being more frequently highlighted as problematic [
18]. Emotional distress as an aspect of tinnitus, such as frustration and irritability ("Does your tinnitus make you feel anxious?"; "Does your tinnitus make you feel frustrated?"; "Does your tinnitus make you feel depressed?"), were frequently and highly reported (4 points) by our patients. The emotional subscale of the THI, which includes items related to feelings of depression and anxiety, is often highlighted as a significant area of concern in specific studies [
18]. In our study, the emotional distress factor has seen consistent high grades in all patients and some downgrade in patients who have lowering scores. The above-mentioned questions were often graded with a maximum score in our study and consistently present in all patients with high scores.
Social function impairment is present in many tinnitus patients and most often in otosclerosis patients with severe scores on the THI [
18]. Our reports on difficulties in concentration and sleep ("Does your tinnitus make it difficult for you to concentrate?"; "Does your tinnitus make it difficult to sleep?"; "Do you find it difficult to focus on a task because of tinnitus?") showed significant impact on patients in all groups. They were the most constant problem reported with high scores across patients in all our study groups. The lowering of these scores was a consistent find in all patients with decreasing tinnitus symptoms, whether clinically relevant or considered a physiological fluctuation of tinnitus. The functional domain of THI seems most affected in otosclerosis patients [
18] as studies indicate, and was the most constantly improved domain in all our patient groups following Florical administration.
Catastrophic reactions linked to THI items ("Do you feel as though you cannot escape your tinnitus?"; "Because of your tinnitus, do you feel that you have a terrible disease?"), such as fear of severe illness or inability to cope with tinnitus, were not a common report in our study, mostly being graded with 0 score. Current literature suggests these items report directly on the severe and catastrophic impact of tinnitus, its connection to mental health and overall well-being of the patient [
17]. In our study, patients who did grade these questions with at least 2 point saw increasing levels in tinnitus as shown in their increasing scores on the THI. Only a small subset of otosclerosis patients seem to have catastrophic tinnitus manifestations, and in these cases, the etiology of catastrophic symptoms is difficult to attribute to only one factor alone and no matter the treatment option, results seem poor [
19].
The worsening of tinnitus in otosclerosis patients cannot be solely attributed to anxiety, as the relationship between the two may suggest. While anxiety is a significant factor, it is not the only one influencing tinnitus severity. Certain studies [
20] suggest that hearing loss in otosclerosis is the primary driver of tinnitus, rather than anxiety alone. Various studies have explored the correlation between anxiety and tinnitus, but the evidence does not support a direct and unique causal relationship [
21]. Instead, tinnitus severity in otosclerosis patients is likely influenced by a combination of factors. A Mendelian randomization study found no genetic causality between anxiety and tinnitus severity, suggesting that while anxiety and tinnitus are correlated, anxiety alone does not cause tinnitus to worsen [22, 23]. During the COVID-19 pandemic, increased anxiety levels were observed, but this did not correspond to a significant increase in tinnitus severity, further suggesting that anxiety alone does not dictate tinnitus outcomes [
24].
In patients with otosclerosis and tinnitus, the relationship between worsening tinnitus symptoms and lowered air conduction thresholds at 4 and 8 kHz is complex and may have heterogeneous explanations. Some of our patients with increasing THI scores and worsening tinnitus displayed lowered air conduction thresholds at the mentioned frequencies. The progression of otosclerosis can affect hearing thresholds, and surgical interventions like stapedotomy are commonly used to improve hearing levels and alleviate tinnitus [
1]. However, the specific impact on high-frequency air conduction thresholds, such as those at 4 and 8 kHz, requires careful consideration. Studies indicate that otosclerosis leads to elevated air conduction thresholds, particularly in advanced stages. Early otosclerosis shows higher air conduction thresholds compared to controls, and these thresholds are significantly higher in late-stage otosclerosis [
25]. Stapedotomy is shown to significantly improve air conduction thresholds and reduce the air-bone gap, which can lead to improved hearing outcomes [
26]. However, the impact on high-frequency thresholds like 4 and 8 kHz is not consistently detailed across multiple studies. While the focus is often on monitoring speech frequencies, high-frequency hearing can also be affected. Postoperative improvements in air conduction thresholds are noted, but specific data in 4 and 8 kHz improvement or degrading of thresholds are less frequently reported [27, 28]. In the absence of any surgical intervention and other tinnitus medication, the 3-month period in our study seems as not enough time for otosclerosis progression and lowered hearing thresholds. The severity of tinnitus may be to blame for the lowered air conduction levels but a direct link may not be attributed. Even if increasing tinnitus may indicate to a correlation with high-frequency thresholds degradation, the link is not well-documented [17, 29] and should be further investigated.
When a patient with otosclerosis experiences an improvement in tinnitus symptoms under a specific treatment, it can be considered significant, especially in the absence of other tinnitus medications, fact taken into account by our study. This significance is underlined by the fact that chronic tinnitus is considered multifactorial and a challenging symptom to address in general [
30]. Otosclerosis surgery is still a popular treatment option for patients, with studies indicating that a substantial percentage of patients report a reduction or complete cessation of tinnitus post-surgery. For instance, one study found that 82.8% of patients experienced a complete or partial absence of tinnitus one month after surgery [
28]. Another study reported that 89% of patients had cessation of tinnitus one year post-surgery [
29]. Conservative treatments with sodium fluoride and bisphosphonates have been shown to stabilize hearing thresholds and delay the worsening of tinnitus. These treatments are particularly beneficial in the early stages of otosclerosis [31, 32]. The literature on the use of calcium and fluoride specifically for tinnitus in otosclerosis patients is currently limited, and along our promising results, the topic is still open to further research and testing. We consider further long-term studies are needed to assess the sustained efficacy of calcium and fluoride supplementation beyond three months, potentially with larger-scale, multicenter studies and across broader patient populations.
5. Conclusions
While the THI provides valuable insights into the specific complaints of our otosclerosis patients, it is important to consider the broader context of tinnitus management and the current multidisciplinary approach employed by doctors and audiologists which is considered to be most effective. Alongside the promising studies regarding the use of sodium fluoride [31, 32], bisphosphonate [
33] and herbal medicines [
34] for tinnitus control, our study demonstrates that oral calcium and fluoride supplementation may be a beneficial non-surgical option for otosclerosis patients with mild and potentially moderate tinnitus. Further research into the mechanisms by which calcium and fluoride influences tinnitus perception and otosclerosis progression could enhance our understanding of its therapeutic potential and maybe warrant its use in post-surgery patients as well.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Workbook 1, 2, 3 corresponding to tables 1, 2 and 3.
Author Contributions
Conceptualization, A.O. and M.G.G.; methodology, X.X.; software, O.M.Z.; validation, A.E.G., L.B. and I.E.; formal analysis, A.O.; investigation, C.A.M.; resources, C.A.M.; data curation, O.M.Z.; writing—original draft preparation, A.O. and C.A.M.; writing—review and editing, M.G.G. and A.E.G.; visualization, I.E.; supervision, M.G.G.; project administration, A.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Review Board of the University Medicine and Pharmacy of Craiova, Romania (No.17184 / 14 April 2020) and The Emergency County Hospital in Craiova, Romania (No.8621 / 18 April 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, attached to their patient data files and archived.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| THI |
Tinnitus Handicap Inventory |
| AST |
Aspartate aminotransferase |
| ALT |
Alanine aminotransferase |
| ALKP |
Alkaline phosphatase |
| ACP |
Acid phosphatase |
| CT |
Computed tomography |
References
- Šaboviča, J.; Klagiša, R. Stapedoplasty – surgical treatment of hearing loss caused by otosclerosis, Social Welfare: Interdisciplinary Approach 2016, 6(1),126–135. [CrossRef]
- Persson, P.; Harder, H.; Magnuson, B. Hearing results in otosclerosis surgery after partial stapedectomy, total stapedectomy and stapedotomy. Acta Otolaryngol. 1997 Jan;117(1):94-9. [CrossRef]
- Cheng, J.; Chandrasekhar, S.S.; Del Signore, A. Florical and Early Otosclerosis. Otolaryngology–Head and Neck Surgery. [CrossRef]
- Newman, C. W.; Jacobson, G. P.; Spitzer, J. B. Limited evidence for the effect of sodium fluoride on deterioration of hearing loss in patients with otosclerosis: a systematic review of the literature Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology–Head & Neck Surgery 1996, 122(2), 143–148. [CrossRef]
- Shashi, A., Bhardwaj, M. Study on blood biochemical diagnostic indices for hepatic function biomarkers in endemic skeletal fluorosis. Biol Trace Elem Res. 2011 Nov;143(2):803-14. [CrossRef]
- Ferreira, M.K.M.; et al. Biomarkers in the Biomonitoring of Fluoride Toxicity: An Overview. In Biomarkers in Toxicology. Biomarkers in Disease: Methods, Discoveries and Applications: Patel, V.B., Preedy, V.R., Rajendram, R. (eds); Springer, Cham. 2022,1-15. [CrossRef]
- Zafar, N.; Hohman, M.H.; Khan, M.A.B. Otosclerosis. [Updated 2024 Mar 1]. In: StatPearls [Internet]. StatPearls Publishing: Treasure Island (FL), 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560671/.
- Lee, T.L.; Wang, M.C.; Lirng, J.F.; Liao, W.H.; Yu, E.C.; Shiao, A.S. High-resolution computed tomography in the diagnosis of otosclerosis in Taiwan. J Chin Med Assoc. 2009,72(10):527-32. [CrossRef] [PubMed]
- Dudau, C.; Salim, F.; Jiang, D.; Connor, S.E. Diagnostic efficacy and therapeutic impact of computed tomography in the evaluation of clinically suspected otosclerosis. Eur Radiol. 2017,27(3):1195-1201. [CrossRef]
- Riggs, B.L.; Hodgson, S.F.; Hoffman, D.L.; Kelly, P.J.; Johnson, K.A.; Taves, D. Treatment of Primary Osteoporosis With Fluoride and Calcium: Clinical Tolerance and Fracture Occurrence. JAMA. 1980;243(5):446–449. [CrossRef]
- Kleinjung, T., Peter, N., Schecklmann, M. et al. The Current State of Tinnitus Diagnosis and Treatment: a Multidisciplinary Expert Perspective. JARO 2024,413–425. [CrossRef]
- https://www.biap.org/es/recommandations/recommendations/tc-02-classification/213-rec-02-1-en-audiometric-classification-of-hearing-impairments/file.
- McCombe, A.; Baguley, D.; Coles, R.; McKenna, L.; McKinney, C.; Windle-Taylor, P. British Association of Otolaryngologists, Head and Neck Surgeons. Guidelines for the grading of tinnitus severity: the results of a working group commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999. Clin Otolaryngol Allied Sci. 2001 Oct;26(5):388-93. [CrossRef]
- Cabuk, G.B.; Buyuklu, A.F.; Karamert, R.; Aksoy, S. Investigation of the applicability of internet-based approach to subjective tinnitus. Acta Otolaryngol. 2024,Apr;144(4):284-292. [CrossRef]
- Cabuk, G.B.; Buyuklu, A.F.; Karamert, R.; Aksoy, S. Investigation of the applicability of internet-based approach to subjective tinnitus. Acta Otolaryngol. 2024, 144(4), 284–292. [Google Scholar] [CrossRef] [PubMed]
- You, D. U.; Bahng, J. A Study on the Rehabilitation Effects of Tinnitus Counseling for Hearing Aid Users Who Suffer from Tinnitus. Audiology and Speech Research, 2024, 20(4), 217-227.
- Dziendziel, B.; Skarżyński, P.H.; Rajchel, J.J.; Gos, E.; Skarżyński, H. Prevalence and severity of tinnitus in Polish otosclerosis patients qualified for stapes surgery. Eur Arch Otorhinolaryngol. 2019, 276(6), 1585–1590. [Google Scholar] [CrossRef] [PubMed]
- Skarzynski, P.H.; Dziendziel, B.; Gos, E.; Wlodarczyk, E.; Miaskiewicz, B.; Rajchel, J.J.; Skarzynski, H. Prevalence and Severity of Tinnitus in Otosclerosis: Preliminary Findings from Validated Questionnaires. J Int Adv Otol. 2019, 15(2), 277–282. [Google Scholar] [CrossRef] [PubMed]
- Ramos Macías, A.; Falcón González, J.C.; Manrique, M.; Morera, C.; García-Ibáñez, L.; Cenjor, C.; Coudert-Koall, C.; Killian, M. Cochlear implants as a treatment option for unilateral hearing loss, severe tinnitus and hyperacusis. Audiol Neurootol. 2015, 20 Suppl 1, 60–6. [Google Scholar] [CrossRef]
- Goderie, T.; van Wier, M.F.; Lissenberg-Witte, B.I.; Merkus, P.; Smits, C.; Leemans, C.R.; Kramer, S.E. Factors Associated With the Development of Tinnitus and With the Degree of Annoyance Caused by Newly Developed Tinnitus. Ear Hear. 2022 Nov-Dec 01, 43(6), 1807-1815. [CrossRef]
- Lima, A.F.; Moreira, F.C.; Costa, I.E.; Azevedo, C.; Mar, F.; Dias, L. Tinnitus and Otosclerosis: An Exploratory Study about the Prevalence, Features and Impact in Daily Life. Int Arch Otorhinolaryngol. 2021, 26(3), e390–e395. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wakabayashi, S.; Oishi, N.; Shinden, S.; Ogawa, K. Factor analysis and evaluation of each item of the tinnitus handicap inventory. Head Face Med. 2020, 16(1), 4. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Ding, Y. The causal relationship between anxiety and tinnitus severity: a Mendelian randomization study. Egyptian Journal of Medical Human Genetics. 2024. [CrossRef]
- Xia, L.; Wang, J.; Chuan, D.; Fan, J.; Chen, Z. Impact of anxiety associated with COVID 19 on tinnitus. MedRxiv. 2020. [CrossRef]
- Abd-Elhmid, I. H.; Abish, Y. G.; Zaghloul, B. A.; Hussein, H. A.; Ghanem, S. S. Correlation between audiological and radiological findings in otosclerosis: randomized clinical study. The Egyptian Journal of Otolaryngology, 2024, 40(1).
- Albera, A.; Parandero, F.; Andriani, R.; Albera, R.; Riva, G.; Canale, A. Prognostic factors influencing postoperative air-bone gap in stapes surgery. Acta Otorhinolaryngol Ital. 2022, 42(4), 380–387. [Google Scholar] [CrossRef] [PubMed]
- Alam, M. I.; Hossain, M. D.; Asaduzzaman, A. K. M. Audioogical Outcome of Stapedotomy for Primary Otosclerosis. Journal of Bangladesh College of Physicians and Surgeons, 2022, 40(2), 116–120.
- Rajati, M.; Poursadegh, M.; Bakhshaee, M.; Abbasi, A.; Shahabi, A. Outcome of stapes surgery for tinnitus recovery in otosclerosis. Int Tinnitus J. 2012, 17(1), 42–6. [Google Scholar] [PubMed]
- Terzić, N.; Jakovljević, V.L.; Milanović, N.; Jaćimović, V.; Zivić, L. Condition of hearing sense and tinnitus before and after the treatment of otosclerosis. Med Pregl. 2010 Sep-Oct, 63(9-10), 648-51. Serbian. [CrossRef]
- Swain, S. K.; Dubey, D. Current pharmacological treatment of tinnitus. Matrix Science Pharma. 2022, 6(3), 53–57. [Google Scholar] [CrossRef]
- Gogoulos, P.P.; Sideris, G.; Nikolopoulos, T.; Sevastatou, E.K.; Korres, G.; Delides, A. Conservative Otosclerosis Treatment With Sodium Fluoride and Other Modern Formulations: A Systematic Review. Cureus. 2023, 15(2), e34850. [Google Scholar] [CrossRef] [PubMed]
- Hentschel, M.A.; Huizinga, P.; van der Velden, D.L.; Wegner, I.; Bittermann, A.J.; van der Heijden, G.J.; Grolman, W. Limited evidence for the effect of sodium fluoride on deterioration of hearing loss in patients with otosclerosis: a systematic review of the literature. Otol Neurotol. 2014, 35(6), 1052–7. [Google Scholar] [CrossRef] [PubMed]
- Fouad, A.; Mandour, M.; Tomoum, M.O.; Lasheen, R.M. Effectiveness of bisphosphonate for alleviating tinnitus associated with otosclerosis: a prospective case-control study. Eur Arch Otorhinolaryngol. 2025, 282(2), 647–658. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Hu, Y.; Wang, D.; Han, H.; Wang, Y.; Wang, X.; Zhou, Z.; Ma, X.; Dong, Y. Herbal medicines in the treatment of tinnitus: An updated review. Front Pharmacol. 2023 Jan 4, 13, 1037528. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).