Submitted:
11 February 2025
Posted:
13 February 2025
You are already at the latest version
Abstract
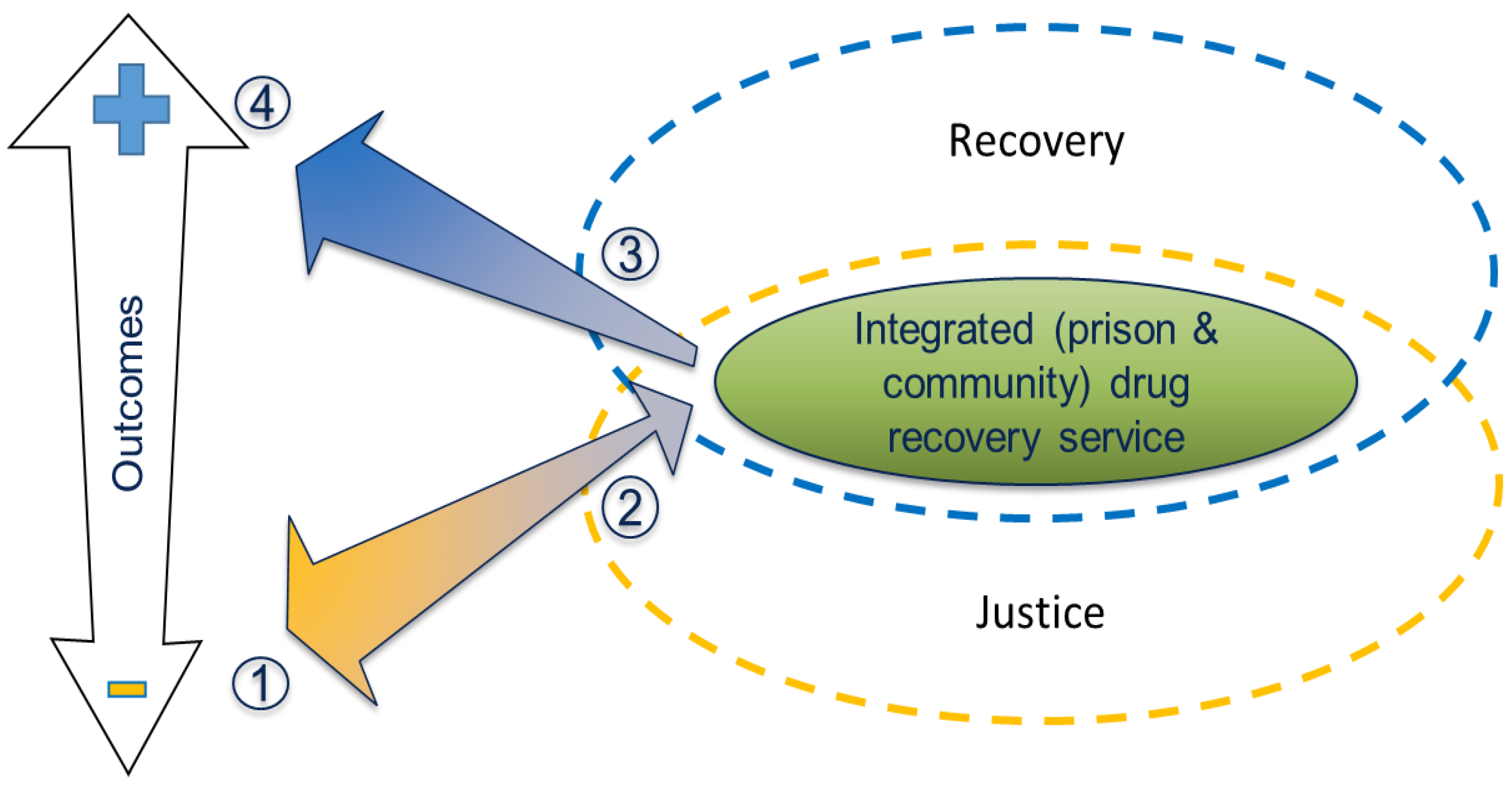
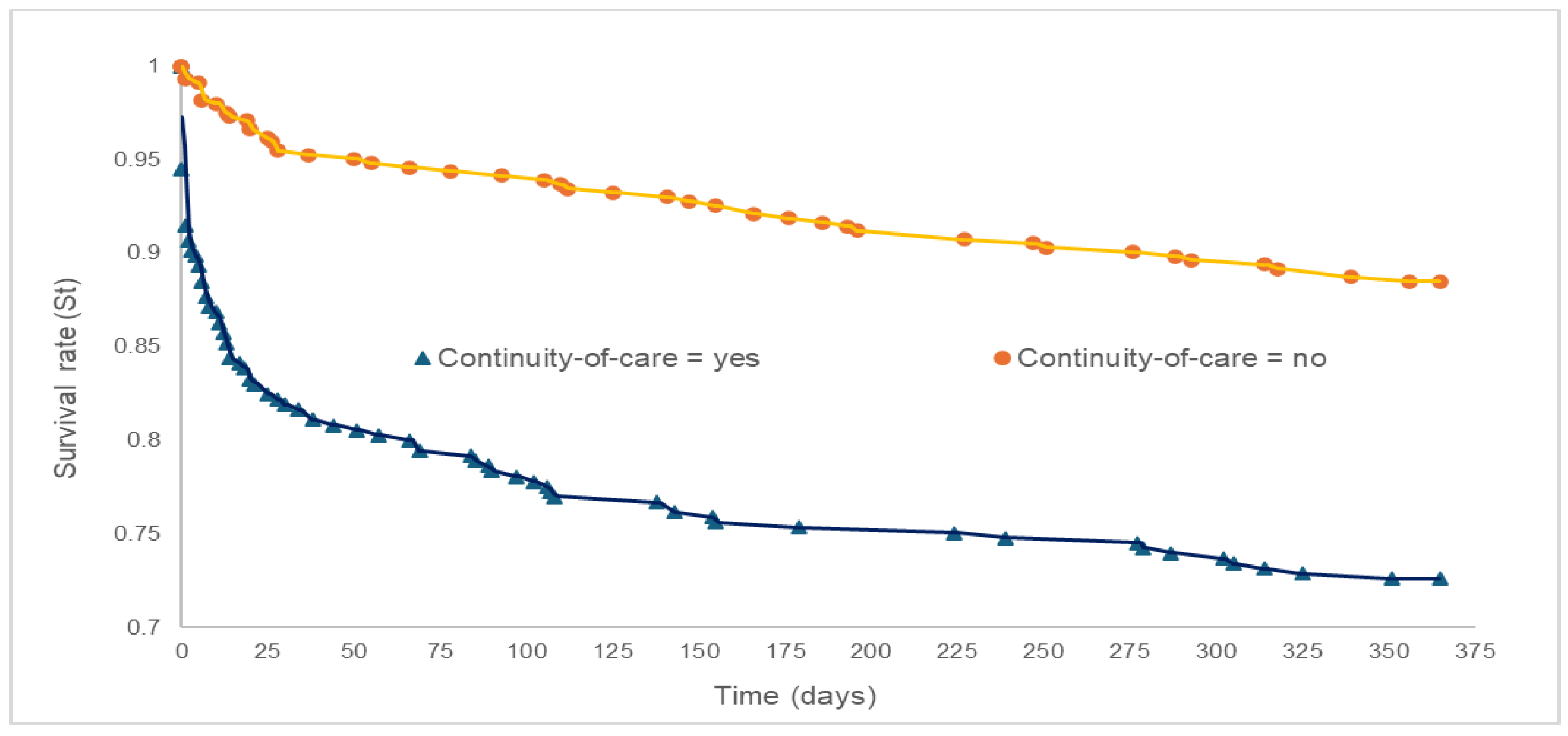
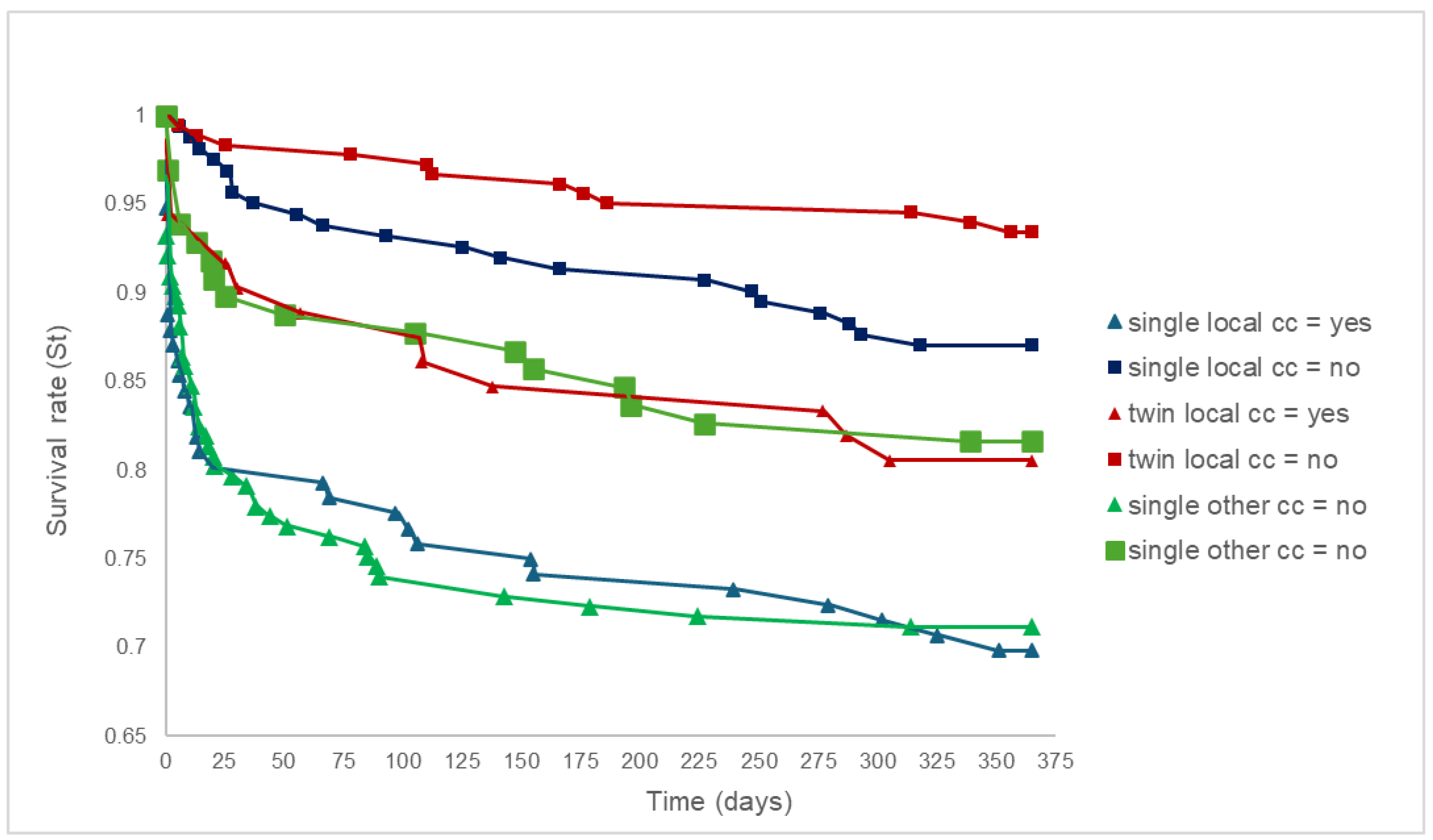
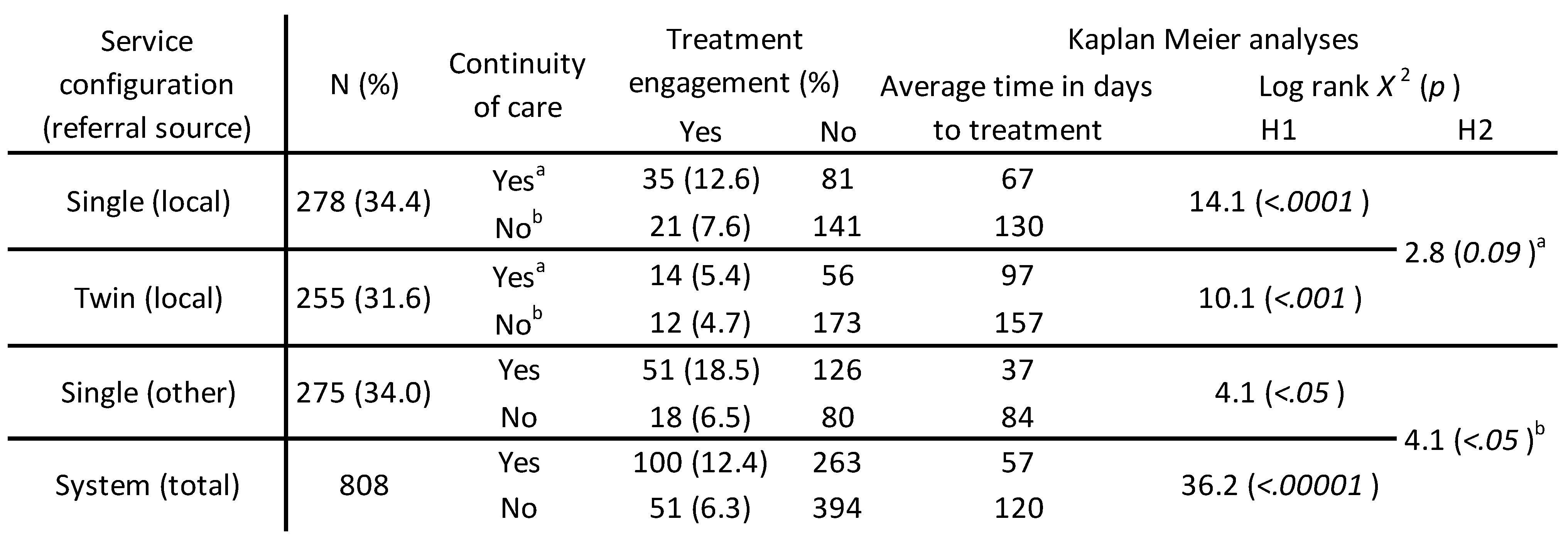
Introduction: This study tests our assumption that continuity-of-care from prison to community increases engagement rates and reduces treatment wait times, hypothesis one (H1). Engaging with drug treatment services may improve health and crime outcomes for this vulnerable population. The study also aims to determine whether a single service delivery model, spanning both prison and community settings, improved these metrics, hypothesis 2 (H2). Method: Over a four-year period, the instances of continuity-of-care, prison release, and treatment start dates were recorded for individuals with substance misuse issues released to a local drug recovery partnership (n=808). All participants were monitored for 365 days after their first release (H1). The same data associated with a subset of this group (n=533), released through the local adult male prison to the local drug treatment services, were compared for the two years before (n=255) and the two years after (n=278) the implementation of the single service delivery model (H2). Data were analysed using right-censored Kaplan Meier Survival Analyses. Results: There was a significant association between system-level prison-to-community continuity-of-care and higher engagement rates, as well as reduced waiting times for community drug treatment (p<.00001). The implementation of single service provision enhanced the performance of prison-to-community continuity-of-care. Specifically, treatment engagements through continuity-of-care increased from 5.4% to 12.7%, and average waiting times decreased from 97 to 67 days. However, due to the small sample size, there was insufficient statistical evidence to support H2. Conclusions: This study confirms that, within our local setting, continuity-of-care care from the prison to community drug treatment leads to higher rates continuity-of-care, treatment engagements and shorter waiting times to community drug treatment (H1 - accepted). Additionally, although not statistically proven (H2 - not accepted), our a priori decision to implement a single-service delivery model appears to have been justified given the observed improvements in these metrics.
Keywords:
Introduction
Discussion:
References
- Aspinall, E. J., Mitchell, W., Schofield, J., Cairns, A., Lamond, S., Bramley, P.,... Hutchinson, S. J. (2016). A matched comparison study of hepatitis C treatment outcomes in the prison and community setting, and an analysis of the impact of prison release or transfer during therapy. Journal of Viral Hepatitis, 23, 1009-1016. [CrossRef]
- Black, C. (2021). Review of drugs part two: prevention, treatment, and recovery. Retrieved from Review of drugs part two: prevention, treatment, and recovery - GOV.UK (www.gov.uk).
- Bailie, R., & Elliot, K. (2016). Offender Health: Partnerships for Excellence. London.
- BBC. (2017). Prison officers in 31 jails set for pay rises of up to £5,000. Retrieved from http://www.bbc.co.uk/news/uk-39014192.
- Checkland, P. (1999). Systems Thinking, Systems Practice. UK: John Wiley & Sons, Ltd.
- Cambell, D. (2016). NHS hospitals in England reveal £2.45bn record deficit. The Guardian. Retrieved from https://www.theguardian.com/society/2016/may/20/nhs-in-england-reveals-245bn-record deficit.
- Checkland, P. (Writer). (2012). On the origins of SSM. In LancasterManagement (Producer), Systems Colloquium in honour of SSM founder Peter Checkland. Lancaster: Lancaster University.
- Chief Inspector of Prisons. (2015). HM Chief Inspector of Prisons for England and Wales Annual Report 2014–15. Retrieved from http://www.justiceinspectorates.gov.uk/hmiprisons/wp content/uploads/sites/4/2015/07/HMIP-AR_2014-15_TSO_Final1.pdf.
- Dyer, W., & Biddle, P. (2013). Prison Health Discharge Planning- Evidence of an Integrated Care Pathway or the End of the Road. Social Policy and Society, 12(4), 521-532. [CrossRef]
- Edwards, B., Gunn, J., Kilgour, J., & Smith, R. (1985). Cooperation between the prison medical service and the NHS: a conversation. Br Med J (Clin Res Ed), 291(6510), 1698-1699. [CrossRef]
- Evans, C., Forrester, A., Jarrett, M., Huddy, V., Campbell, C. A., Byrne, M.,... Valmaggia, L. (2016). Early detection and early intervention in prison: improving outcomes and reducing prison returns. The Journal of Forensic Psychiatry & Psychology, 1-17. [CrossRef]
- Forrester, J. (1968). Principles of Systems (2nd ed.). Waltham, MA: Pegasus communications.
- Forrester, J. (1971). Principles of systems : text and workbook, chapters 1 through 10 (2nd preliminary ed. ed.). Cambridge, Mass.: Wright-Allen Press ; Cambridge.
- From Harm to Hope: A 10-year drugs plan to cut crime and save lives.
- Retrieved from https://www.gov.uk/government/publications/from- harm-to-hope-a-10-year-drugs-plan-to-cut-crime and-save-lives.
- Garnick, D. W., Horgan, C. M., Acevedo, A., Lee, M. T., Panas, L., Ritter, G. A.,... Wright, D. (2014).
- Criminal justice outcomes after engagement in outpatient substance abuse treatment. Journal of Substance Abuse Treatment, 46(3), 295-305. [CrossRef]
- Grace, S., Page, G., Lloyd, C., Templeton, L., Kougali, Z., McKeganey, N.,... Russell, C. (2016). Establishing a ‘Corstonian’ continuous care pathway for drug using female prisoners: Linking Drug Recovery Wings and Women’s Community Services. Criminology and criminal justice. [CrossRef]
- Gulland, A. (2010). Continuity of health care for prisoners on release in England is worsening. BMJ, 340.
- Gossop, M., Trakada, K., Stewart, D., & Witton, J. (2005). Reductions in criminal convictions after addiction treatment: 5-year follow-up. Drug and Alcohol Dependence, 79(3), 295-302. [CrossRef]
- HM Inspectorate of Probation, H. I. o. P. (2016). An Inspection of Through the Gate Resettlement Services for Short-Term Prisoners.
- Home Office. (2004). Reducing Re-offending: National Action Plan. London: Home Office.
- Home Office. (2007). Drug Interventions Record: Completion Guidelines & Business Rules for the Drug, Interventions Record suite of forms, Field by Field Guidance. Retrieved from http://webarchive.nationalarchives.gov.uk/20060919101130/http://drugs.homeoffice.gov.uk/publication-search/dip/DIR_field_by_field?view=Binary.
- Lloyd, C., & Page, G. (2015). Drug Recovery Wing (DRW) Pilots Evaluation. Retrieved from https://www.york.ac.uk/healthsciences/research/mental-health/projects/drugrecoverywingpilotsevaluation/#tab-3.
- MacDonald, M., Williams, J., & Kane, D. (2012). Barriers to implementing throughcare for problematic drug users in European prisons. International Journal of Prisoner Health, 8(2), 68-84. [CrossRef]
- National Institute for Health and Care Excellence. (2014). Continuity of care. Retrieved from http://www.evidence.nhs.uk/search?q=continuity%20in%20care.
- National Treatment Agency. (2008). Health care professionals and partners: NDTMS. Retrieved from http://www.nta.nhs.uk/ndtms.aspx.
- National Treatment Agency. (2009a). Breaking the Link. Retrieved from London: http://www.nta.nhs.uk/uploads/nta_criminaljustice_0809.pdf.
- National Treatment Agency. (2009b). Continuity of Care Guidance. In. London: The Department of Health.
- National Treatment Agency. (2009c). NDTMS.net. Retrieved from https://www.ndtms.net/resources/Guidance/OCU-adult_report_guidance.pdf.
- National Treatment Agency. (2009d). Seven Partnerships in England have been awarded Drug Systems Change Pilot status. Retrieved from http://www.nta.nhs.uk/system-change-pilot.aspx.
- National Treatment Agency. (2012a). Crime halved once drug addicts are on the road to recovery. Retrieved from http://www.nta.nhs.uk/news-2012-crime-halved.aspx.
- National Treatment Agency. (2012b). Estimating the crime reduction benefits of drug treatment and recovery. Retrieved from London: http://www.nta.nhs.uk/uploads/vfm2012.pdf.
- National Treatment Agency. (2012c). The impact of drug treatment on reconviction. Retrieved from London: http://www.nta.nhs.uk/uploads/theimpactoftreatmentonreconviction.pdf.
- National Treatment Agency. (2012d). Value for Money Presentation: Treat addiction, cut crime. London: NTA.
- North East Public Health Observatory. (2001). About the NDTMS. Retrieved from http://www.nepho.org.uk/ndtms/About_Us.
- PriceWaterhouseCoopers. (2008). Government and Public Sector Consulting. Report to the Department of Health and Ministry of Justice: Review of Prison-Based Drug Treatment Funding. Retrieved from London: http://www.parliament.uk/deposits/depositedpapers/2008/DEP2008-1539.pdf.
- Prisons and Drugs Misuse. Retrieved from London: UK Government. (2021).
- Public Health England. (2015). National Drug Treatment Monitoring System (NDTMS) Adult drug treatment business definition. Retrieved from http://www.nta.nhs.uk/uploads/adult-drug-treatment-business-definition-ndtms-data-set-m.pdf.
- Public Health Outcomes Framework. (2025). Public Health Outcomes Framework - Data | Fingertips | Department of Health and Social Care.
- Scaggs, S., Bales, W., Clark, C., Ensley, D., Coltharp, P., G., T., & Blomberg, T. (2015). An Assessment of Substance Abuse Treatment Programs in Florida’s Prisons Using a Random Assignment Experimental Design. Retrieved from US: https://www.ncjrs.gov/pdffiles1/nij/grants/249843.pdf.
- Statistics Kingdom. (2025). Kaplan Meier Survival Analysis: Kaplan Meier and Log Rank.
- Strang, J., Finch, E., Hankinson, L., Farrell, M., Taylor, C., & Gossop, M. (1997). Methadone treatment for opiate addiction: Benefits in the first month. ADDICTION RESEARCH, 5(1), 71-76. [CrossRef]
- The All Party Parliamentary Drugs Misuse Group. (1998). House of Commons - Home Affairs - Appendices to the Minutes of Evidence.
- The Full Fact Organisation. (2017). The state of prisons in England and Wales.
- Retrieved from https://fullfact.org/crime/state-prisons-england-and-wales/.
- Guidance for improving continuity of care between prison and the community (2018).
- Retrieved from London: UK Government. (2021) Guidance for improving continuity of care between prison and the community - GOV.UK.
- Westminster Drug Project (2010). “New Service to Reduce Drug Related Crime in Essex”.
- Retrieved from http://www.wdp-.org.uk/news.php/12/new-service-to-reduce-drug-related crime-in-essex 13th December 2011.
- Yang, Y., Knight, K., Joe, G. W., Rowan-Szal, G. A., Lehman, W. E. K., & Flynn, P. M. (2013). The Influence of Client Risks and Treatment Engagement on Recidivism. Journal of Offender Rehabilitation, 52(8), 544-564. [CrossRef]
 |
| Prison type (context) | Prison-to-community drug treatment engagements (%) | |||
| Year 1 | Year 2 | Year 3 | Year 4 | |
| Local (study) | 113 (27%) | 171 (45%) | 238 (59%) | 169 (68%) |
| Local (matched) | 99 (30%) | 73 (22%) | 161 (60%) | 95 (77%) |
| National (system) | 6544 (24%) | 7894 (34%) | 10159 (42%) | 6396 (47%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





