1. Introduction
Accurate assessment of labor progression is a critical and challenging aspect of clinical obstetrics, directly influencing the success of vaginal delivery and pregnancy outcomes. Traditionally, vaginal examination has been widely employed as the “gold standard” for evaluating labor progression, including fetal head position, orientation, and cervical dilation. While it allows for real-time monitoring, it is significantly influenced by subjective factors, requires extensive training, may cause discomfort to the patient, and poses an increased risk of infection [
1]. Consequently, the need for an objective, non-invasive, and user-friendly assessment method is paramount to improving delivery quality.
In recent years, ultrasound technology has been increasingly adopted for labor monitoring. Compared to vaginal examination, ultrasound provides a more objective, accurate, and reproducible assessment. It allows for a direct visualization of labor progression, reduces the frequency of vaginal exams and infection risks, and is simple to perform and easy to learn. Moreover, ultrasound is unaffected by fetal orientation and can aid in diagnosing umbilical cord prolapse and fetal malposition [
2].
Research has shown that certain ultrasound parameters, such as the angle of progression (AOP) and head-perineum distance (HPD), can be used to predict the mode of delivery and the likelihood of emergency cesarean section in primiparas. These parameters provide clinicians with valuable decision-making tools, enable real-time monitoring of the first stage of labor, and allow for predictions regarding labor duration. Such capabilities facilitate the early detection of abnormal labor progression and timely interventions, thereby improving delivery outcomes [
3,
4].
The clinical value of intrapartum ultrasound is gaining increasing recognition, with broad application prospects. However, the specific application of transperineal ultrasound parameters in labor assessment remains under investigation domestically [
5,
6,
7]. This study employs transperineal ultrasound to accurately measure parameters such as AOP, HPD, and midline angle (MLA) during labor. By analyzing their correlations with delivery mode and labor duration in primiparas, the study aims to provide precise, auxiliary monitoring tools for clinical practice.
2. Materials and Methods
2.1. Patient Population
From September 2023 to September 2024, 144 primiparas in the first stage of labor were recruited from the obstetrics department of our hospital. Inclusion criteria were as follows: gestational age of 38 to 40+6 weeks; singleton pregnancy with cephalic presentation, no pelvic abnormalities, and consent for vaginal delivery trial; normal fetal growth and development; no spontaneous membrane rupture or irregular contractions upon admission; no cervical disease or history of cervical surgery; and no contraindications for vaginal delivery, such as macrosomia or oligohydramnios. Exclusion criteria included abnormal fetal presentation, fetal malformations or intrauterine growth restriction, pregnancy complications (e.g., gestational hypertension, diabetes, hyperthyroidism, or epilepsy), and coagulation disorders. Informed consent was obtained from all subjects involved in the study. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Yongkang First People’s Hospital.
2.2. Methods
Data collection was conducted collaboratively by senior ultrasound specialists and experienced obstetric physicians. The ultrasound specialists were responsible for confirming fetal orientation, fetal head position, anterior-posterior cervical lip distance, and measuring the ultrasound parameters AOP, HPD, and MLA. Obstetricians recorded ultrasound data, performed final data analyses, and evaluated obstetric intervention decisions. Cervical dilation was confirmed by experienced midwives or senior obstetricians through vaginal examination.
All procedures utilized the Mindray M9T ultrasound diagnostic system equipped with a C5-1s abdominal probe. Patients were instructed to empty their bladders and assume the lithotomy position. After disinfecting the perineum 2–3 times, the ultrasound specialist applied coupling gel to the probe, covered it with a thin glove, and performed the examination. The assessments were conducted during contraction intervals, synchronized with vaginal examinations, and completed within five minutes per session. Examinations began at the onset of labor, with measurements taken every two hours during the latent phase and hourly during the active phase until full cervical dilation was achieved.
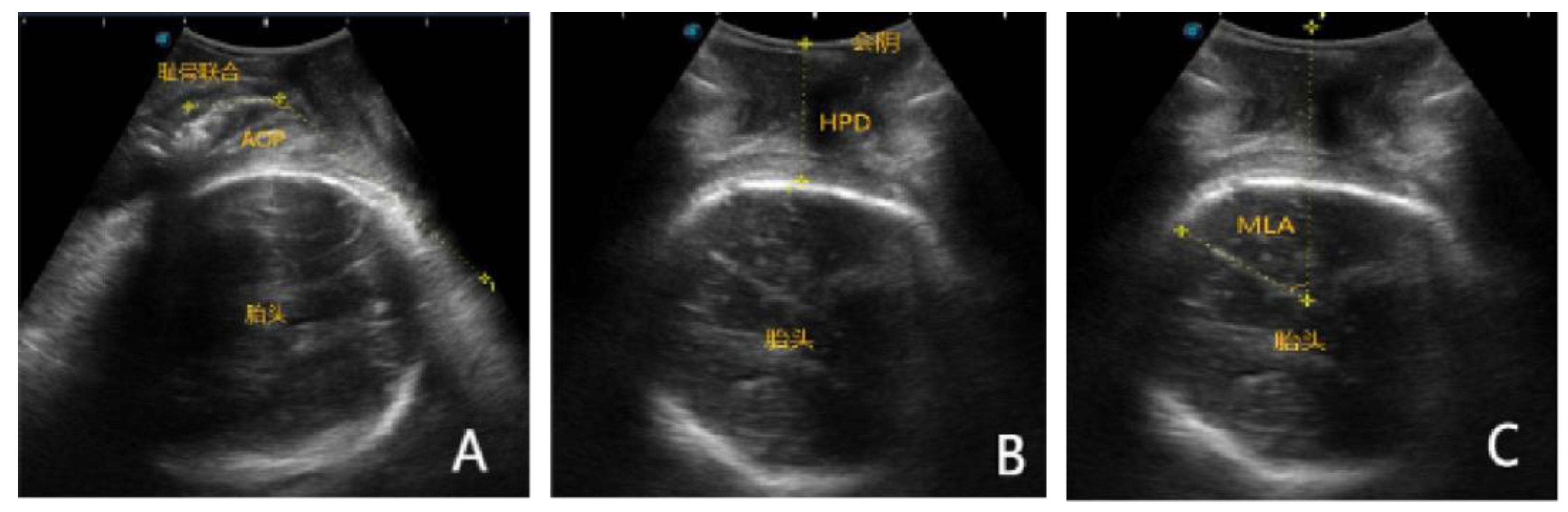
A sagittal plane was used to capture images clearly displaying the pubic symphysis long axis and fetal head contour. The probe was then rotated 90° to obtain a transverse view, ensuring the fetal head contour remained visible for image capture. The transperineal ultrasound probe was positioned sagittally against the perineal skin to measure the angle between the pubic symphysis long axis and a tangent extending from the lower edge of the pubic symphysis to the fetal head arc (AOP,
Figure 1A). In the transverse plane, the distance from the lowest bony point of the fetal head to the perineal skin was measured as HPD (
Figure 1B). The MLA was determined by measuring the angle between the maternal pelvic anteroposterior axis (midline axis) and the fetal midbrain axis in the transverse plane (
Figure 1C).
Each ultrasound measurement was repeated twice, with the final result being the average. Ultrasound examinations were conducted by specialists trained for three months, while vaginal examinations were performed by midwives with over five years of experience. To ensure independence and objectivity, ultrasound specialists and midwives did not share examination results.
2.3. Data Collection
Compare the transperineal ultrasound parameters between the two groups, including fetal orientation, anterior-posterior cervical lip distance, fetal head position, AOP, HPD, and MLA values. Analyze the predictive efficacy of AOP, HPD, and MLA for delivery mode and their correlations with vaginal delivery rates and labor duration.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA). Continuous variables with a normal distribution were expressed as mean ± standard deviation, and comparisons between groups were conducted using independent-sample t-tests. Categorical variables were expressed as percentages (%), and comparisons between groups were performed using the χ² test. Receiver operating characteristic (ROC) curves were plotted to evaluate the predictive efficacy of AOP, HPD, and MLA, with the area under the curve (AUC) calculated. An AUC > 0.5 was considered indicative of diagnostic value. Linear regression analysis was used to assess the relationship between AOP, HPD, MLA, and vaginal delivery rates. Pearson correlation analysis was applied to examine the associations between labor duration and AOP, HPD, and MLA.
3. Results
The patients included in the study were divided into two groups based on the final mode of delivery: the vaginal delivery group (108 cases) and the cesarean section group (36 cases). The baseline data of the two groups were similar, with no significant difference (p > 0.05), as shown in
Table 1.
3.1. Comparison of Transperineal Ultrasound Parameters Between the Two Groups
There was no statistically significant difference between the two groups in fetal position, anterior-posterior cervical distance, or fetal head position during the first stage of labor (p > 0.05). The AOP in the vaginal delivery group was higher than that in the cesarean section group, while the HPD and MLA were lower in the vaginal delivery group compared to the cesarean section group ( p < 0.001), as shown in
Table 2.
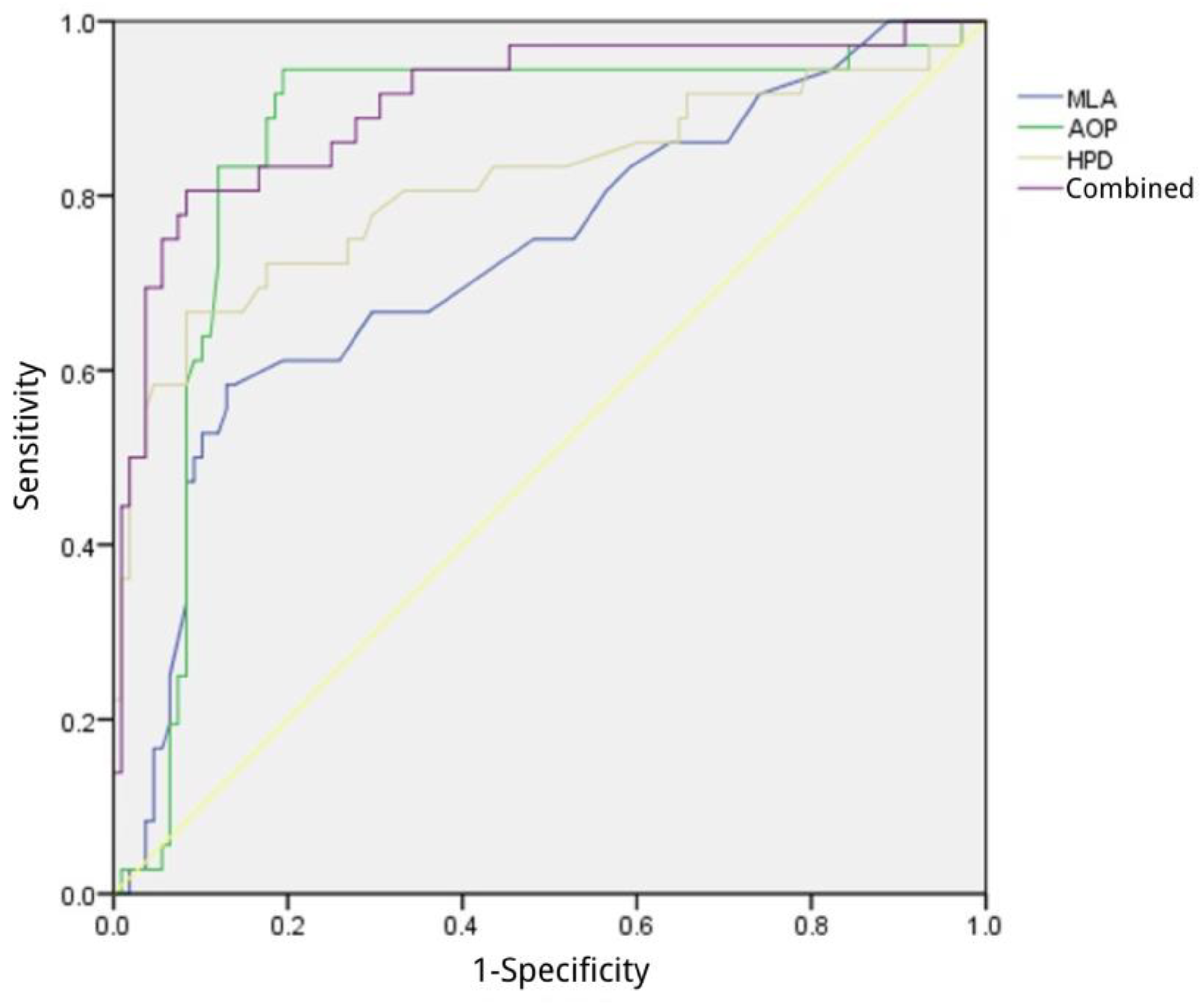
3.2. Predictive Efficiency of AOP, HPD, and MLA for Delivery Mode
When the Youden index for AOP reached its maximum, the corresponding cut-off value was 117.27°, with an AUC of 0.858, sensitivity of 80.55%, and specificity of 94.44%. For HPD, the maximum Youden index corresponded to a cut-off value of 23.13 cm, with an AUC of 0.814, sensitivity of 91.67%, and specificity of 66.67%. MLA achieved its maximum Youden index at a cut-off value of 14.36°, with an AUC of 0.730, sensitivity of 74.07%, and specificity of 58.33%. The combined application of AOP, HPD, and MLA provided the highest predictive value for delivery mode, achieving an AUC of 0.884, sensitivity of 81.48%, and specificity of 97.22%, as shown in
Table 3 and
Figure 2.
3.3. Correlation Between AOP, HPD, MLA and Vaginal Delivery Rate
The parameters AOP, HPD, and MLA were divided into groups based on their median values, and linear regression analysis was performed to examine their association with vaginal delivery rates. The results indicated that the multiple correlation coefficient was 0.511, with a coefficient of determination (R²) of 0.261. The regression equation was established as Y = 0.318 × AOP - 0.173 × HPD - 0.204 × MLA (F = 16.499, p < 0.001).
3.4. Correlation Between AOP, HPD, MLA and Labor Duration
Pearson correlation analysis demonstrated that AOP was negatively correlated with labor duration (p < 0.001), while HPD and MLA were positively correlated with labor duration (p < 0.001), as shown in
Table 4.
4. Discussion
Primiparas often experience fear and anxiety during childbirth due to their lack of experience and unfamiliarity with the new environment. These negative emotions can become obstacles to the smooth progression of labor, potentially leading to labor complications. This may increase the risk of cesarean section and negatively impact uterine contractions, causing prolonged labor and increased bleeding [
8,
9]. Studies indicate that labor progression is closely linked to factors such as the birth canal, uterine power, and fetal condition. It is estimated that 30% to 55% of women opt for cesarean sections due to labor dystocia, which not only imposes physical and mental stress on the mother but also heightens the risk of serious complications such as uterine rupture and postpartum hemorrhage [
10,
11]. Therefore, effective monitoring and precise evaluation of the labor process are crucial to ensuring the safety of both the mother and the baby. Traditional vaginal examinations, due to their subjective nature, carry the risk of misjudgment, which can have adverse effects on maternal and fetal health [
12]. Thus, exploring more scientific and objective monitoring methods is essential.
Ultrasound has become an essential tool in obstetrics for evaluating the progress of labor due to its high accuracy, efficiency, non-invasiveness, and reproducibility. Through ultrasound imaging analysis, fetal conditions can be accurately assessed, and factors such as fetal head molding can be excluded, providing reliable data for monitoring labor progress. Ultrasound also helps in early detection of abnormalities, enabling timely interventions to ensure maternal and fetal safety [
13,
14]. Research has shown that transperineal ultrasound technology is highly feasible for assessing fetal presentation and can assist in predicting the mode of delivery [
15]. Pan WL et al. [
16] used ultrasound parameters for prospective prediction of vaginal delivery, enabling the early identification of abnormal labor progress and facilitating timely interventions, which can optimize delivery outcomes. This highlights the important role of ultrasound in obstetrics, providing strong support for clinical decision-making. Studies have also reported that a larger AOP value suggests a higher likelihood of vaginal delivery, whereas a smaller AOP value increases the risk of cesarean section [
17]. Previous research indicates that transperineal ultrasound parameters have certain predictive value for delivery modes. In this study, ultrasound technology was used to assist clinical delivery decisions, and the results showed that the AOP in the vaginal delivery group was higher, while MLA and HPD values were lower than in the cesarean section group. These findings are consistent with previous studies. Analysis of the ROC curve showed that the combination of AOP, HPD, and MLA had an AUC of 0.884, indicating that monitoring ultrasound parameters like AOP, HPD, and MLA can help predict the delivery mode in full-term women. There was no statistical significance between the two groups in terms of fetal position, cervical anterior-posterior lip distance, and fetal head position during the first stage of labor, which may be due to the dynamic changes in fetal position, uterine contractions, and fetal movements. Additionally, the cervical anterior-posterior lip distance gradually shortens to zero, and fetal head position is influenced by multiple factors.
During normal delivery, the occiput anterior (OA) position is considered the ideal fetal head presentation, but it is relatively rare in clinical practice, occurring in only about 12.67% of cases [
18,
19]. Therefore, the internal rotation of the fetal head is crucial for determining whether the baby can be delivered in the OA position, which is a key factor in the delivery process. AOP describes the angle between the bony part of the fetal head and the bony structures of the pelvic outlet as the fetal head passes through the birth canal. This angle is important for assessing labor progress and determining whether the fetus can pass through the pelvic outlet smoothly [
20,
21]. The current study showed a negative correlation between AOP and delivery time, while MLA and HPD were positively correlated with delivery time. These findings are consistent with those of previous studies [
22,
23,
24] suggesting that ultrasound parameters like AOP, MLA, and HPD are related to delivery time and can reflect labor progression and fetal status. Larger AOP values, and smaller MLA and HPD values, indicate that the fetal head is closer to the perineum, which may shorten the delivery time. However, other studies have suggested that HPD may have a negative correlation with delivery time [
25]. This could be due to differences in study samples, measurement methods, labor complexity, or research design [
26]. Therefore, more high-quality studies are needed to further verify and clarify the exact relationship between AOP, MLA, HPD, and delivery time.
5. Conclusions
In conclusion, intrapartum transperineal ultrasound measurements such as AOP, HPD, and MLA are closely related to both delivery mode and labor duration. Monitoring these ultrasound parameters provides a more comprehensive understanding of the labor process, offering important insights for timely interventions and ensuring maternal and fetal safety.
Author Contributions
Conceptualization, L.F. and H.H.; methodology, L.F.; software, L.F.; formal analysis, L.F.; investigation, L.F., H.S., J.L., X.W., and H.H; data curation, H.S., J.L., X.W.; writing—original draft preparation, L.F.; writing—review and editing, L.F.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Yongkang First People’s Hospital.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AOP |
Angle of progression |
| HPD |
Head-perineum distance |
| MLA |
Midline angle |
| ROC |
Receiver operating characteristic |
| AUC |
Area under the curve |
References
- Dimassi, K.; Hammami, A. Agreement between digital vaginal examination and intrapartum ultrasound for labour monitoring. Journal of Obstetrics and Gynaecology 2022, 42, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Khalil, O.; Elbadawi, E.; Abdelnaby, M.; Zayed, L.H. Assessment of the progress of labor by the use of intrapartum ultrasound. Alexandria Journal of Medicine 2012, 48, 295–301. [Google Scholar] [CrossRef]
- Banos, N.; Perez-Moreno, A.; Julia, C.; Murillo-Bravo, C.; Coronado, D.; Gratacos, E.; Deprest, J.; Palacio, M. Quantitative analysis of cervical texture by ultrasound in mid-pregnancy and association with spontaneous preterm birth. Ultrasound in Obstetrics & Gynecology 2018, 51, 637–643. [Google Scholar]
- Tekesin, I.; Hellmeyer, L.; Heller, G.; Römer, A.; Kühnert, M.; Schmidt, S. Evaluation of quantitative ultrasound tissue characterization of the cervix and cervical length in the prediction of premature delivery for patients with spontaneous preterm labor. American journal of obstetrics and gynecology 2003, 189, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Chor, C.M.; Poon, L.C.Y.; Leung, T.Y. Prediction of labor outcome using serial transperineal ultrasound in the first stage of labor. The Journal of Maternal-Fetal & Neonatal Medicine 2019, 32, 31–37. [Google Scholar]
- Ghi, T.; Contro, E.; Farina, A.; Nobile, M.; Pilu, G. Three-dimensional ultrasound in monitoring progression of labor: a reproducibility study. Ultrasound in Obstetrics and Gynecology 2010, 36, 500–506. [Google Scholar] [CrossRef]
- Jung, J.E.; Lee, Y.J. Intrapartum transperineal ultrasound: angle of progression to evaluate and predict the mode of delivery and labor progression. Obstetrics & Gynecology Science 2024, 67, 1. [Google Scholar]
- Xu, C.; Zhong, W.; Fu, Q.; Yi, L.; Deng, Y.; Cheng, Z.; Lin, X.; Cai, M.; Zhong, S.; Wang, M. Differential effects of different delivery methods on progression to severe postpartum hemorrhage between Chinese nulliparous and multiparous women: a retrospective cohort study. BMC Pregnancy and Childbirth 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Wray, S.; Arrowsmith, S.; Sharp, A. Pharmacological interventions in labor and delivery. Annual Review of Pharmacology and Toxicology 2023, 63, 471–489. [Google Scholar] [CrossRef]
- Dior, U.P.; Kogan, L.; Eventov-Friedman, S.; Gil, M.; Bahar, R.; Ergaz, Z.; Porat, S.; Calderon-Margalit, R. Very high intrapartum fever in term pregnancies and adverse obstetric and neonatal outcomes. Neonatology 2015, 109, 62–68. [Google Scholar] [CrossRef]
- Lowe, N.K. A review of factors associated with dystocia and cesarean section in nulliparous women. Journal of midwifery & women's health 2007, 52, 216–228. [Google Scholar]
- Downe, S.; Gyte, G.M.; Dahlen, H.G.; Singata, M. Routine vaginal examinations for assessing progress of labour to improve outcomes for women and babies at term. Cochrane Database of Systematic Reviews 2013, 7. [Google Scholar] [CrossRef] [PubMed]
- Che Yaacob, N.A.; Nik Muhamad Afendi, N.R.; Zahiruddin Wan Mohammad, W.M.; Zuky Nik Lah, N.A. Association between fetal occiput position and fetal spine following induction of labour (IOL) and birth outcomes: a prospective study. Perinatal Journal 2024, 32. [Google Scholar]
- Malvasi, A.; Gustapane, S.; Malvasi, M.; Vinciguerra, M.; Tinelli, A.; Beck, R. Semeiotics of intrapartum ultrasonography: new diagnostic sonographic sign of fetal malpositions and malrotations. Intrapartum Ultrasonography for Labor Management: Labor, Delivery and Puerperium 2021, 251–273. [Google Scholar]
- Kamel, R.A.; Negm, S.M.; Youssef, A.; Bianchini, L.; Brunelli, E.; Pilu, G.; Soliman, M.; Nicolaides, K.H. Predicting cesarean delivery for failure to progress as an outcome of labor induction in term singleton pregnancy. American journal of obstetrics and gynecology 2021, 224, e601–e609. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.-L.; Chen, L.-L.; Gau, M.-L. Accuracy of non-invasive methods for assessing the progress of labor in the first stage: a systematic review and meta-analysis. BMC Pregnancy and Childbirth 2022, 22, 608. [Google Scholar] [CrossRef] [PubMed]
- Nouri-Khasheh-Heiran, E.; Montazeri, A.; Conversano, F.; Kashanian, M.; Rasuli, M.; Rahimi, M.; Mirpour, M.; Akbari, N. The success of vaginal birth by use of trans-labial ultrasound plus vaginal examination and vaginal examination only in pregnant women with labor induction: a comparative study. BMC Pregnancy and Childbirth 2023, 23, 3. [Google Scholar] [CrossRef]
- Nassr, A.A.; Berghella, V.; Hessami, K.; Bibbo, C.; Bellussi, F.; Robinson, J.N.; Marsoosi, V.; Tabrizi, R.; Safari-Faramani, R.; Tolcher, M.C. Intrapartum ultrasound measurement of angle of progression at the onset of the second stage of labor for prediction of spontaneous vaginal delivery in term singleton pregnancies: a systematic review and meta-analysis. American journal of obstetrics and gynecology 2022, 226, 205–214.e202. [Google Scholar] [CrossRef]
- Dall’Asta, A.; Angeli, L.; Masturzo, B.; Volpe, N.; Schera, G.B.L.; Di Pasquo, E.; Girlando, F.; Attini, R.; Menato, G.; Frusca, T. Prediction of spontaneous vaginal delivery in nulliparous women with a prolonged second stage of labor: the value of intrapartum ultrasound. American journal of obstetrics and gynecology 2019, 221, 642.e641–642.e613. [Google Scholar] [CrossRef]
- Carvalho Neto, R.H.; Viana Junior, A.B.; Moron, A.F.; Araujo Junior, E.; Carvalho, F.H.C.; Feitosa, H.N. Assessment of the angle of progression and distance perineum-head in the prediction of type of delivery and duration of labor using intrapartum ultrasonography. The Journal of Maternal-Fetal & Neonatal Medicine 2021, 34, 2340–2348. [Google Scholar]
- Hjartardóttir, H.; Lund, S.H.; Benediktsdóttir, S.; Geirsson, R.T.; Eggebø, T.M. Fetal descent in nulliparous women assessed by ultrasound: a longitudinal study. American Journal of Obstetrics and Gynecology 2021, 224, 378.e371–378.e315. [Google Scholar] [CrossRef]
- Ali, J.; Hebbar, S. Ultrasound assessment of foetal Head–Perineum distance prior to induction of labour as a predictor of successful vaginal delivery. The Journal of Obstetrics and Gynecology of India 2019, 69, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Bagadia, P.; Suryarao, P.D.; Otiv, S.; Katakdhond, S.S. A Study Of Prediction Of The Mode Of Delivery By Using Transperineal Ultrasonography At Or Before The Onset Of Labor In Nulliparous Women. Journal of Pharmaceutical Negative Results 2022, 3640–3651. [Google Scholar]
- Skinner, S.M.; Giles-Clark, H.J.; Higgins, C.; Mol, B.W.; Rolnik, D.L. Prognostic accuracy of ultrasound measures of fetal head descent to predict outcome of operative vaginal birth: a comparative systematic review and meta-analysis. American Journal of Obstetrics and Gynecology 2023, 229, 10–22.e10. [Google Scholar] [CrossRef] [PubMed]
- Torkildsen, E.; Salvesen, K.; Eggebø, T. Prediction of delivery mode with transperineal ultrasound in women with prolonged first stage of labor. Ultrasound in obstetrics & gynecology 2011, 37, 702–708. [Google Scholar]
- Chan, Y.T.V.; Ng, V.K.S.; Yung, W.K.; Lo, T.K.; Leung, W.C.; Lau, W.L. Relationship between intrapartum transperineal ultrasound measurement of angle of progression and head–perineum distance with correlation to conventional clinical parameters of labor progress and time to delivery. The Journal of Maternal-Fetal & Neonatal Medicine 2015, 28, 1476–1481. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).