Submitted:
22 January 2025
Posted:
23 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
- 1.
- Cholesterol absorption related to cardiovascular disease
- 2.
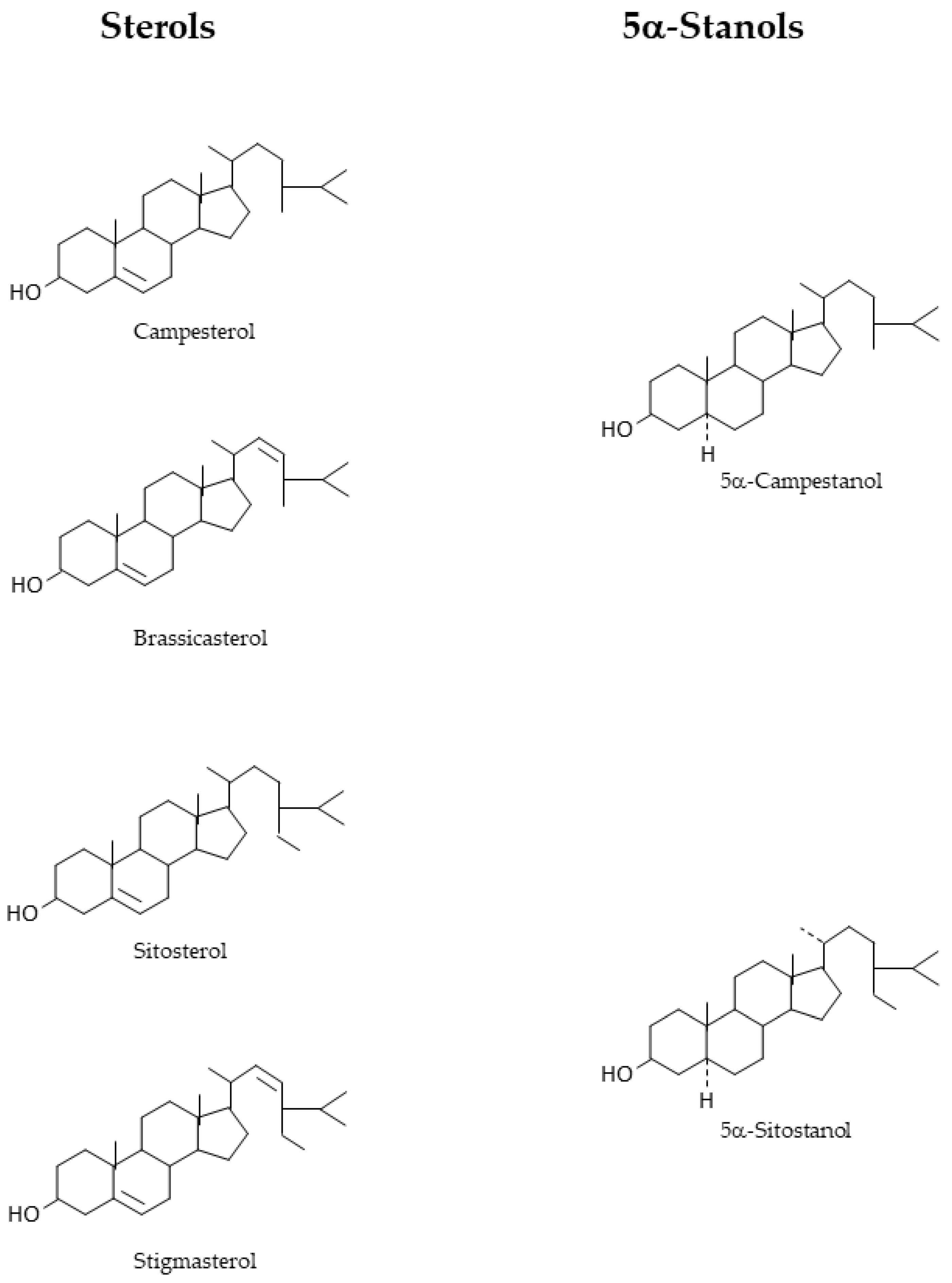
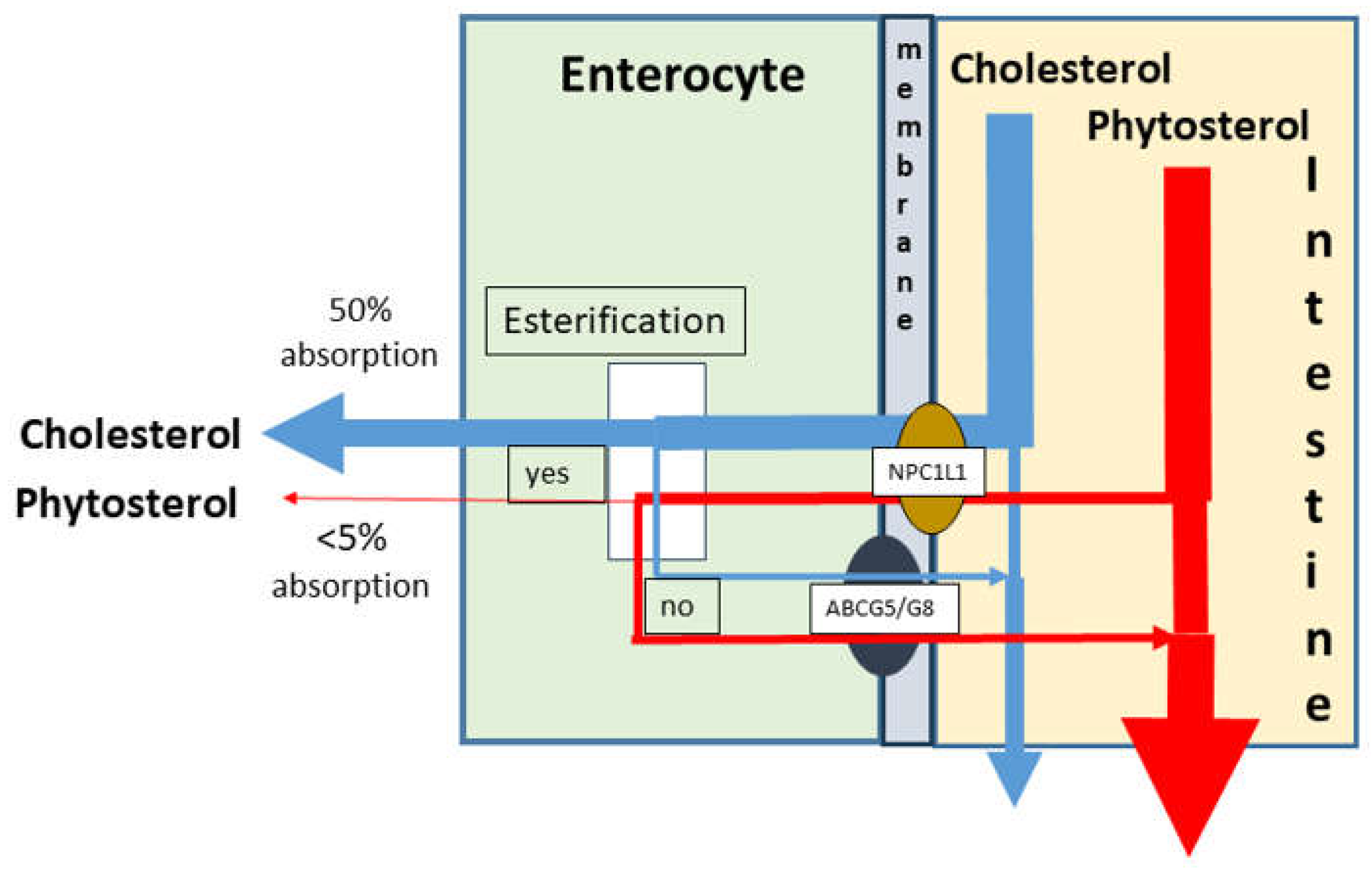
- Absorption of cholesterol and phytosterol absorption
- 3.
- Plasma low density lipoprotein cholesterol lowering
1.1. Pharmaceutical Therapy
1.2. Phytosterol Application
2. Disadvantages and Side Effects of Treatment
2.1. Pharmaceutical Treatment
2.2. Phytosterol Treatment
3. Discussion
3.1. Natural Elimination of Phytosterols from the Human Body
3.2. Phytosterols and Atherosclerotic Risks in Phytosterolemia
3.3. Determination of Clinical Endpoints After Long-Term High-Phytosterol Intake – Possible or Impossible?
3.4. Which Patients Should Strictly Avoid Plant Sterol Supplementation?
3.5. What is the Value of Plasma Phytosterol Concentrations in the Assessment of Risk for Atherosclerosis?
3.6. On the Causality of High-Dose Phytosterol Intake on Development of Atherosclerosis
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Banach, M.; Reiner, Z.; Surma, S.; Bajraktari, G.; Bielecka-Dabrowa, A.; Bunc, M.; Bytyci, I.; Ceska, R.; Cicero, A.F.G.; Dudek, D., et al. 2024 Recommendations on the Optimal Use of Lipid-Lowering Therapy in Established Atherosclerotic Cardiovascular Disease and Following Acute Coronary Syndromes: A Position Paper of the International Lipid Expert Panel (ILEP). Drugs 2024, 84, 1541–1577. [CrossRef]
- Akivis, Y.; Alkaissi, H.; McFarlane, S.I.; Bukharovich, I. The Role of Triglycerides in Atherosclerosis: Recent Pathophysiologic Insights and Therapeutic Implications. Curr Cardiol Rev 2024, 20, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Sascau, R.; Clement, A.; Radu, R.; Prisacariu, C.; Statescu, C. Triglyceride-Rich Lipoproteins and Their Remnants as Silent Promoters of Atherosclerotic Cardiovascular Disease and Other Metabolic Disorders: A Review. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Lütjohann, D.; Klör, H.U.; Stellaard, F. Measurement of Serum Low Density Lipoprotein Cholesterol and Triglyceride-Rich Remnant Cholesterol as Independent Predictors of Atherosclerotic Cardiovascular Disease: Possibilities and Limitations. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Burger, P.M.; Dorresteijn, J.A.N.; Koudstaal, S.; Holtrop, J.; Kastelein, J.J.P.; Jukema, J.W.; Ridker, P.M.; Mosterd, A.; Visseren, F.L.J. Course of the effects of LDL-cholesterol reduction on cardiovascular risk over time: A meta-analysis of 60 randomized controlled trials. Atherosclerosis 2024, 396, 118540. [Google Scholar] [CrossRef] [PubMed]
- Reeskamp, L.F.; Meessen, E.C.E.; Groen, A.K. Transintestinal cholesterol excretion in humans. Curr Opin Lipidol 2018, 29, 10–17. [Google Scholar] [CrossRef]
- Lütjohann, D.; Meese, C.O.; Crouse, J.R., 3rd.; von Bergmann, K. Evaluation of deuterated cholesterol and deuterated sitostanol for measurement of cholesterol absorption in humans. J Lipid Res 1993, 34, 1039–1046. [Google Scholar] [CrossRef]
- Parhofer, K.G. The Treatment of Disorders of Lipid Metabolism. Dtsch Arztebl Int 2016, 113, 261–268. [Google Scholar] [CrossRef]
- Fears, R.; Richards, D.H.; Ferres, H. The effect of compactin, a potent inhibitor of 3-hydroxy-3-methylglutaryl coenzyme-A reductase activity, on cholesterogenesis and serum cholesterol levels in rats and chicks. Atherosclerosis 1980, 35, 439–449. [Google Scholar] [CrossRef]
- Sudhop, T.; Reber, M.; Tribble, D.; Sapre, A.; Taggart, W.; Gibbons, P.; Musliner, T.; von Bergmann, K.; Lütjohann, D. Changes in cholesterol absorption and cholesterol synthesis caused by ezetimibe and/or simvastatin in men. J Lipid Res 2009, 50, 2117–2123. [Google Scholar] [CrossRef]
- Lütjohann, D.; Stellaard, F.; Mulder, M.T.; Sijbrands, E.J.G.; Weingärtner, O. The emerging concept of “individualized cholesterol-lowering therapy”: A change in paradigm. Pharmacol Ther 2019, 199, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Temel, R.E.; Tang, W.; Ma, Y.; Rudel, L.L.; Willingham, M.C.; Ioannou, Y.A.; Davies, J.P.; Nilsson, L.M.; Yu, L. Hepatic Niemann-Pick C1-like 1 regulates biliary cholesterol concentration and is a target of ezetimibe. J Clin Invest 2007, 117, 1968–1978. [Google Scholar] [CrossRef] [PubMed]
- Capuozzo, M.; Ottaiano, A.; Cinque, C.; Farace, S.; Ferrara, F. Cutting-edge lipid-lowering pharmacological therapies: Improving lipid control beyond statins. Hipertens Riesgo Vasc 2025, 10.1016/j.hipert.2024.12.002. [CrossRef]
- Ge, Q.; Yan, Y.; Luo, Y.; Teng, T.; Cao, C.; Zhao, D.; Zhang, J.; Li, C.; Chen, W.; Yang, B.; et al. Dietary supplements: clinical cholesterol-lowering efficacy and potential mechanisms of action. Int J Food Sci Nutr 2024, 75, 349–368. [Google Scholar] [CrossRef] [PubMed]
- Jaceldo-Siegl, K.; Lütjohann, D.; Sirirat, R.; Mashchak, A.; Fraser, G.E.; Haddad, E. Variations in dietary intake and plasma concentrations of plant sterols across plant-based diets among North American adults. Mol Nutr Food Res 2017, 61. [Google Scholar] [CrossRef]
- Ikeda, I.; Sugano, M. Some aspects of mechanism of inhibition of cholesterol absorption by beta-sitosterol. Biochim Biophys Acta 1983, 732, 651–658. [Google Scholar] [CrossRef]
- Ras, R.T.; Geleijnse, J.M.; Trautwein, E.A. LDL-cholesterol-lowering effect of plant sterols and stanols across different dose ranges: a meta-analysis of randomised controlled studies. Br J Nutr 2014, 112, 214–219. [Google Scholar] [CrossRef]
- Chhabria, M.T.; Mahajan, B.M. Update on patented cholesterol absorption inhibitors. Expert Opin Ther Pat 2009, 19, 1083–1107. [Google Scholar] [CrossRef]
- Miszczuk, E.; Bajguz, A.; Kiraga, L.; Crowley, K.; Chlopecka, M. Phytosterols and the Digestive System: A Review Study from Insights into Their Potential Health Benefits and Safety. Pharmaceuticals (Basel) 2024, 17. [Google Scholar] [CrossRef]
- Jefrei, E.; Xu, M.; Moore, J.B.; Thorne, J.L. Phytosterol and phytostanol-mediated epigenetic changes in cancer and other non-communicable diseases: a systematic review. Br J Nutr 2024, 131, 935–943. [Google Scholar] [CrossRef]
- Evtyugin, D.D.; Evtuguin, D.V.; Casal, S.; Domingues, M.R. Advances and Challenges in Plant Sterol Research: Fundamentals, Analysis, Applications and Production. Molecules 2023, 28. [Google Scholar] [CrossRef]
- Gylling, H.; Strandberg, T.E.; Kovanen, P.T.; Simonen, P. Lowering Low-Density Lipoprotein Cholesterol Concentration with Plant Stanol Esters to Reduce the Risk of Atherosclerotic Cardiovascular Disease Events at a Population Level: A Critical Discussion. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Simonen, P.; Oorni, K.; Sinisalo, J.; Strandberg, T.E.; Wester, I.; Gylling, H. High cholesterol absorption: A risk factor of atherosclerotic cardiovascular diseases? Atherosclerosis 2023, 376, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Does Dietary Cholesterol Matter? Curr Atheroscler Rep 2016, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Stellaard, F.; von Bergmann, K.; Sudhop, T.; Lütjohann, D. The value of surrogate markers to monitor cholesterol absorption, synthesis and bioconversion to bile acids under lipid lowering therapies. J Steroid Biochem Mol Biol 2017, 169, 111–122. [Google Scholar] [CrossRef]
- Katsuki, S.; Matoba, T.; Akiyama, Y.; Yoshida, H.; Kotani, K.; Fujii, H.; Harada-Shiba, M.; Ishibashi, Y.; Ishida, T.; Ishigaki, Y.; et al. Association of Serum Levels of Cholesterol Absorption and Synthesis Markers with the Presence of Cardiovascular Disease: The CACHE Study CVD Analysis. J Atheroscler Thromb 2023, 30, 1766–1777. [Google Scholar] [CrossRef]
- Mashnafi, S.; Plat, J.; Mensink, R.P.; Baumgartner, S. Non-Cholesterol Sterol Concentrations as Biomarkers for Cholesterol Absorption and Synthesis in Different Metabolic Disorders: A Systematic Review. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Weingärtner, O.; Weingärtner, N.; Scheller, B.; Lütjohann, D.; Graber, S.; Schafers, H.J.; Bohm, M.; Laufs, U. Alterations in cholesterol homeostasis are associated with coronary heart disease in patients with aortic stenosis. Coron Artery Dis 2009, 20, 376–382. [Google Scholar] [CrossRef]
- Nasu, K.; Terashima, M.; Habara, M.; Ko, E.; Ito, T.; Yokota, D.; Ishizuka, S.; Kurita, T.; Kimura, M.; Kinoshita, Y.; et al. Impact of cholesterol metabolism on coronary plaque vulnerability of target vessels: a combined analysis of virtual histology intravascular ultrasound and optical coherence tomography. JACC Cardiovasc Interv 2013, 6, 746–755. [Google Scholar] [CrossRef]
- Altmann, S.W.; Davis, H.R., Jr.; Zhu, L.J.; Yao, X.; Hoos, L.M.; Tetzloff, G.; Iyer, S.P.; Maguire, M.; Golovko, A.; Zeng, M.; et al. Niemann-Pick C1 Like 1 protein is critical for intestinal cholesterol absorption. Science 2004, 303, 1201–1204. [Google Scholar] [CrossRef]
- Davis, H.R., Jr.; Zhu, L.J.; Hoos, L.M.; Tetzloff, G.; Maguire, M.; Liu, J.; Yao, X.; Iyer, S.P.; Lam, M.H.; Lund, E.G.; et al. Niemann-Pick C1 Like 1 (NPC1L1) is the intestinal phytosterol and cholesterol transporter and a key modulator of whole-body cholesterol homeostasis. J Biol Chem 2004, 279, 33586–33592. [Google Scholar] [CrossRef]
- Zanlungo, S.; Nervi, F. Discovery of the hepatic canalicular and intestinal cholesterol transporters. New targets for treatment of hypercholesterolemia. Eur Rev Med Pharmacol Sci 2003, 7, 33–39. [Google Scholar] [PubMed]
- Zio, S.; Tarnagda, B.; Tapsoba, F.; Zongo, C.; Savadogo, A. Health interest of cholesterol and phytosterols and their contribution to one health approach: Review. Heliyon 2024, 10, e40132. [Google Scholar] [CrossRef] [PubMed]
- Ostlund, R.E., Jr.; McGill, J.B.; Zeng, C.M.; Covey, D.F.; Stearns, J.; Stenson, W.F.; Spilburg, C.A. Gastrointestinal absorption and plasma kinetics of soy Delta(5)-phytosterols and phytostanols in humans. Am J Physiol Endocrinol Metab 2002, 282, E911–916. [Google Scholar] [CrossRef] [PubMed]
- Lütjohann, D.; Bjorkhem, I.; Beil, U.F.; von Bergmann, K. Sterol absorption and sterol balance in phytosterolemia evaluated by deuterium-labeled sterols: effect of sitostanol treatment. J Lipid Res 1995, 36, 1763–1773. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Wang, X.; Wen, D.; Fang, M.; You, C.; Ma, L. Novel Low-Density Lipoprotein Cholesterol Reduction Therapies for the Secondary Prevention of Cardiovascular Disease. Rev Cardiovasc Med 2023, 24, 286. [Google Scholar] [CrossRef]
- Xu, Q.; Zhao, Y.M.; He, N.Q.; Gao, R.; Xu, W.X.; Zhuo, X.J.; Ren, Z.; Wu, C.Y.; Liu, L.S. PCSK9: A emerging participant in heart failure. Biomed Pharmacother 2023, 158, 114106. [Google Scholar] [CrossRef]
- Bilen, O.; Ballantyne, C.M. Bempedoic Acid (ETC-1002): an Investigational Inhibitor of ATP Citrate Lyase. Curr Atheroscler Rep 2016, 18, 61. [Google Scholar] [CrossRef]
- Stellaard, F.; Baumgartner, S.; Mensink, R.; Winkens, B.; Plat, J.; Lütjohann, D. Serum Low Density Lipoprotein Cholesterol Concentration Is Not Dependent on Cholesterol Synthesis and Absorption in Healthy Humans. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Lütjohann, D.; Stellaard, F. Degree of serum LDL cholesterol reduction by simvastatin and ezetimibe is dependent on baseline LDL cholesterol concentration but not on baseline values and changes in cholesterol synthesis and absorption parameters. Int J Clin Pharmacol Ther 2024, 62, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Pollak, O.J. Reduction of blood cholesterol in man. Circulation 1953, 7, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, T.A.; Puska, P.; Gylling, H.; Vanhanen, H.; Vartiainen, E. Reduction of serum cholesterol with sitostanol-ester margarine in a mildly hypercholesterolemic population. N Engl J Med 1995, 333, 1308–1312. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.A. Composition of Plant Sterols and Stanols in Supplemented Food Products. J AOAC Int 2015, 98, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Demonty, I.; Ras, R.T.; van der Knaap, H.C.; Duchateau, G.S.; Meijer, L.; Zock, P.L.; Geleijnse, J.M.; Trautwein, E.A. Continuous dose-response relationship of the LDL-cholesterol-lowering effect of phytosterol intake. J Nutr 2009, 139, 271–284. [Google Scholar] [CrossRef]
- Ostlund, R.E., Jr. Phytosterols and cholesterol metabolism. Curr Opin Lipidol 2004, 15, 37–41. [Google Scholar] [CrossRef]
- Ikeda, I. Factors affecting intestinal absorption of cholesterol and plant sterols and stanols. J Oleo Sci 2015, 64, 9–18. [Google Scholar] [CrossRef]
- Gonzalez, C.P.; Bardolia, C.; Pizzolato, K.; Amin, N.S. Utilizing Pharmacogenomics Results to Improve Statin-Associated Muscle Symptoms. Sr Care Pharm 2024, 39, 151–158. [Google Scholar] [CrossRef]
- Bays, H.E.; Moore, P.B.; Drehobl, M.A.; Rosenblatt, S.; Toth, P.D.; Dujovne, C.A.; Knopp, R.H.; Lipka, L.J.; Lebeaut, A.P.; Yang, B.; et al. Effectiveness and tolerability of ezetimibe in patients with primary hypercholesterolemia: pooled analysis of two phase II studies. Clin Ther 2001, 23, 1209–1230. [Google Scholar] [CrossRef]
- Shrank, W.H.; Choudhry, N.K.; Tong, A.; Myers, J.; Fischer, M.A.; Swanton, K.; Slezak, J.; Brennan, T.A.; Liberman, J.N.; Moffit, S.; et al. Warnings without guidance: patient responses to an FDA warning about ezetimibe. Med Care 2012, 50, 479–484. [Google Scholar] [CrossRef]
- Gylling, H.; Plat, J.; Turley, S.; Ginsberg, H.N.; Ellegard, L.; Jessup, W.; Jones, P.J.; Lütjohann, D.; Maerz, W.; Masana, L.; et al. Plant sterols and plant stanols in the management of dyslipidaemia and prevention of cardiovascular disease. Atherosclerosis 2014, 232, 346–360. [Google Scholar] [CrossRef] [PubMed]
- Plat, J.; Baumgartner, S.; Vanmierlo, T.; Lütjohann, D.; Calkins, K.L.; Burrin, D.G.; Guthrie, G.; Thijs, C.; Te Velde, A.A.; Vreugdenhil, A.C.E.; et al. Plant-based sterols and stanols in health & disease: “Consequences of human development in a plant-based environment?”. Prog Lipid Res 2019, 74, 87–102. [Google Scholar] [CrossRef] [PubMed]
- Weingärtner, O.; Lütjohann, D.; Ji, S.; Weisshoff, N.; List, F.; Sudhop, T.; von Bergmann, K.; Gertz, K.; Konig, J.; Schafers, H.J.; et al. Vascular effects of diet supplementation with plant sterols. J Am Coll Cardiol 2008, 51, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Kohler, J.; Teupser, D.; Elsasser, A.; Weingärtner, O. Plant sterol enriched functional food and atherosclerosis. Br J Pharmacol 2017, 174, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- Gylling, H.; Simonen, P. Phytosterols, Phytostanols, and Lipoprotein Metabolism. Nutrients 2015, 7, 7965–7977. [Google Scholar] [CrossRef]
- Hansel, B.; Carrie, A.; Brun-Druc, N.; Leclert, G.; Chantepie, S.; Coiffard, A.S.; Kahn, J.F.; Chapman, M.J.; Bruckert, E. Premature atherosclerosis is not systematic in phytosterolemic patients: severe hypercholesterolemia as a confounding factor in five subjects. Atherosclerosis 2014, 234, 162–168. [Google Scholar] [CrossRef]
- Teupser, D.; Baber, R.; Ceglarek, U.; Scholz, M.; Illig, T.; Gieger, C.; Holdt, L.M.; Leichtle, A.; Greiser, K.H.; Huster, D.; et al. Genetic regulation of serum phytosterol levels and risk of coronary artery disease. Circ Cardiovasc Genet 2010, 3, 331–339. [Google Scholar] [CrossRef]
- Helgadottir, A.; Thorleifsson, G.; Alexandersson, K.F.; Tragante, V.; Thorsteinsdottir, M.; Eiriksson, F.F.; Gretarsdottir, S.; Bjornsson, E.; Magnusson, O.; Sveinbjornsson, G.; et al. Genetic variability in the absorption of dietary sterols affects the risk of coronary artery disease. Eur Heart J 2020, 41, 2618–2628. [Google Scholar] [CrossRef]
- Wilund, K.R.; Yu, L.; Xu, F.; Vega, G.L.; Grundy, S.M.; Cohen, J.C.; Hobbs, H.H. No association between plasma levels of plant sterols and atherosclerosis in mice and men. Arterioscler Thromb Vasc Biol 2004, 24, 2326–2332. [Google Scholar] [CrossRef]
- Windler, E.; Zyriax, B.C.; Kuipers, F.; Linseisen, J.; Boeing, H. Association of plasma phytosterol concentrations with incident coronary heart disease Data from the CORA study, a case-control study of coronary artery disease in women. Atherosclerosis 2009, 203, 284–290. [Google Scholar] [CrossRef]
- Windler, E.; Beil, F.U.; Berthold, H.K.; Gouni-Berthold, I.; Kassner, U.; Klose, G.; Lorkowski, S.; Marz, W.; Parhofer, K.G.; Plat, J.; et al. Phytosterols and Cardiovascular Risk Evaluated against the Background of Phytosterolemia Cases-A German Expert Panel Statement. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Ras, R.T.; Hiemstra, H.; Lin, Y.; Vermeer, M.A.; Duchateau, G.S.; Trautwein, E.A. Consumption of plant sterol-enriched foods and effects on plasma plant sterol concentrations--a meta-analysis of randomized controlled studies. Atherosclerosis 2013, 230, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Scholz, M.; Horn, K.; Pott, J.; Gross, A.; Kleber, M.E.; Delgado, G.E.; Mishra, P.P.; Kirsten, H.; Gieger, C.; Muller-Nurasyid, M.; et al. Genome-wide meta-analysis of phytosterols reveals five novel loci and a detrimental effect on coronary atherosclerosis. Nat Commun 2022, 13, 143. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Ding, H.; Zhu, H.; Huang, S.; Yan, C.; Chen, Z.Y. Additional mechanism for selective absorption of cholesterol and phytosterols. Food Chem 2024, 458, 140300. [Google Scholar] [CrossRef]
- Glueck, C.J.; Speirs, J.; Tracy, T.; Streicher, P.; Illig, E.; Vandegrift, J. Relationships of serum plant sterols (phytosterols) and cholesterol in 595 hypercholesterolemic subjects, and familial aggregation of phytosterols, cholesterol, and premature coronary heart disease in hyperphytosterolemic probands and their first-degree relatives. Metabolism 1991, 40, 842–848. [Google Scholar] [CrossRef]
- Rajaratnam, R.A.; Gylling, H.; Miettinen, T.A. Independent association of serum squalene and noncholesterol sterols with coronary artery disease in postmenopausal women. J Am Coll Cardiol 2000, 35, 1185–1191. [Google Scholar] [CrossRef]
- Sudhop, T.; Gottwald, B.M.; von Bergmann, K. Serum plant sterols as a potential risk factor for coronary heart disease. Metabolism 2002, 51, 1519–1521. [Google Scholar] [CrossRef]
- Assmann, G.; Cullen, P.; Erbey, J.; Ramey, D.R.; Kannenberg, F.; Schulte, H. Plasma sitosterol elevations are associated with an increased incidence of coronary events in men: results of a nested case-control analysis of the Prospective Cardiovascular Munster (PROCAM) study. Nutr Metab Cardiovasc Dis 2006, 16, 13–21. [Google Scholar] [CrossRef]
- Pinedo, S.; Vissers, M.N.; von Bergmann, K.; Elharchaoui, K.; Lütjohann, D.; Luben, R.; Wareham, N.J.; Kastelein, J.J.; Khaw, K.T.; Boekholdt, S.M. Plasma levels of plant sterols and the risk of coronary artery disease: the prospective EPIC-Norfolk Population Study. J Lipid Res 2007, 48, 139–144. [Google Scholar] [CrossRef]
- Fassbender, K.; Lütjohann, D.; Dik, M.G.; Bremmer, M.; Konig, J.; Walter, S.; Liu, Y.; Letiembre, M.; von Bergmann, K.; Jonker, C. Moderately elevated plant sterol levels are associated with reduced cardiovascular risk--the LASA study. Atherosclerosis 2008, 196, 283–288. [Google Scholar] [CrossRef]
- Prasad, M.; Jayaraman, S.; Eladl, M.A.; El-Sherbiny, M.; Abdelrahman, M.A.E.; Veeraraghavan, V.P.; Vengadassalapathy, S.; Umapathy, V.R.; Jaffer Hussain, S.F.; Krishnamoorthy, K.; et al. A Comprehensive Review on Therapeutic Perspectives of Phytosterols in Insulin Resistance: A Mechanistic Approach. Molecules 2022, 27. [Google Scholar] [CrossRef]
- Fong, V.; Patel, S.B. Recent advances in ABCG5 and ABCG8 variants. Curr Opin Lipidol 2021, 32, 117–122. [Google Scholar] [CrossRef]
- Park, J.H.; Chung, I.H.; Kim, D.H.; Choi, M.H.; Garg, A.; Yoo, E.G. Sitosterolemia presenting with severe hypercholesterolemia and intertriginous xanthomas in a breastfed infant: case report and brief review. J Clin Endocrinol Metab 2014, 99, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Berge, K.E.; Tian, H.; Graf, G.A.; Yu, L.; Grishin, N.V.; Schultz, J.; Kwiterovich, P.; Shan, B.; Barnes, R.; Hobbs, H.H. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science 2000, 290, 1771–1775. [Google Scholar] [CrossRef] [PubMed]
- Kidambi, S.; Patel, S.B. Sitosterolaemia: pathophysiology, clinical presentation and laboratory diagnosis. J Clin Pathol 2008, 61, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Morganroth, J.; Levy, R.I.; McMahon, A.E.; Gotto, A.M., Jr. Pseudohomozygous type II hyperlipoproteinemia. J Pediatr 1974, 85, 639–643. [Google Scholar] [CrossRef]
- Yoshida, A.; Naito, M.; Miyazaki, K. Japanese sisters associated with pseudohomozygous familial hypercholesterolemia and sitosterolemia. J Atheroscler Thromb 2000, 7, 33–38. [Google Scholar] [CrossRef]
- Lee, S.D.; Gershkovich, P.; Darlington, J.W.; Wasan, K.M. Inhibition of cholesterol absorption: targeting the intestine. Pharm Res 2012, 29, 3235–3250. [Google Scholar] [CrossRef]
- Silbernagel, G.; Fauler, G.; Renner, W.; Landl, E.M.; Hoffmann, M.M.; Winkelmann, B.R.; Boehm, B.O.; Marz, W. The relationships of cholesterol metabolism and plasma plant sterols with the severity of coronary artery disease. J Lipid Res 2009, 50, 334–341. [Google Scholar] [CrossRef]
- Weingärtner, O.; Teupser, D.; Patel, S.B. The Atherogenicity of Plant Sterols: The Evidence from Genetics to Clinical Trials. J AOAC Int 2015, 98, 742–749. [Google Scholar] [CrossRef]
- Ballew, S.H.; Matsushita, K. Cardiovascular Risk Prediction in CKD. Semin Nephrol 2018, 38, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Fellstrom, B.C.; Jardine, A.G.; Schmieder, R.E.; Holdaas, H.; Bannister, K.; Beutler, J.; Chae, D.W.; Chevaile, A.; Cobbe, S.M.; Gronhagen-Riska, C.; et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med 2009, 360, 1395–1407. [Google Scholar] [CrossRef] [PubMed]
- Wanner, C.; Krane, V.; Marz, W.; Olschewski, M.; Mann, J.F.; Ruf, G.; Ritz, E.; German, D.; Dialysis Study, I. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 2005, 353, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C.; Kirby, A.; Sourjina, T.; Peto, R.; Collins, R.; et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar] [CrossRef]
- Silbernagel, G.; Fauler, G.; Genser, B.; Drechsler, C.; Krane, V.; Scharnagl, H.; Grammer, T.B.; Baumgartner, I.; Ritz, E.; Wanner, C.; et al. Intestinal cholesterol absorption, treatment with atorvastatin, and cardiovascular risk in hemodialysis patients. J Am Coll Cardiol 2015, 65, 2291–2298. [Google Scholar] [CrossRef]
- Baumgartner, S.; Mensink, R.P.; Konings, M.; Schott, H.F.; Friedrichs, S.; Husche, C.; Lütjohann, D.; Plat, J. Postprandial plasma oxyphytosterol concentrations after consumption of plant sterol or stanol enriched mixed meals in healthy subjects. Steroids 2015, 99, 281–286. [Google Scholar] [CrossRef]
- Baumgartner, S.; Mensink, R.P.; Husche, C.; Lütjohann, D.; Plat, J. Effects of plant sterol- or stanol-enriched margarine on fasting plasma oxyphytosterol concentrations in healthy subjects. Atherosclerosis 2013, 227, 414–419. [Google Scholar] [CrossRef]
- Weingärtner, O.; Ulrich, C.; Lütjohann, D.; Ismail, K.; Schirmer, S.H.; Vanmierlo, T.; Bohm, M.; Laufs, U. Differential effects on inhibition of cholesterol absorption by plant stanol and plant sterol esters in apoE-/- mice. Cardiovasc Res 2011, 90, 484–492. [Google Scholar] [CrossRef]
- Simonen, P.; Nylund, L.; Vartiainen, E.; Kovanen, P.T.; Strandberg, T.E.; Oorni, K.; Wester, I.; Gylling, H. Heart-healthy diets including phytostanol ester consumption to reduce the risk of atherosclerotic cardiovascular diseases. A clinical review. Lipids Health Dis 2024, 23, 341. [Google Scholar] [CrossRef]
| Subjects | Results | Comments | Study |
|---|---|---|---|
| Hypercholesterolemic subjects. 231/364 (m/f) | Cholesterol correlated weakly with plasma campesterol and sitosterol. High campesterol associated with family history of CHD | Exclusion criteria and statin intake not reported. | Glueck et al. 1991[66] |
| Verified CAD (n=48), controls (n=61) | Plasma campesterol- and sitosterol-to-cholesterol ratios were significantly associated with CAD | Statin intake not reported. Women only. | Rajaratnam et al. 2000[67] |
| Patients with (n=26) or without (n=27) CHD family history | FH patients had higher absolute plasma concentrations of campesterol and sitosterol | Lack of a true control group. Statin intake and dietary intake of plant sterols not reported. | Sudhop et al. 2002[68] |
| Cohort study, Cases with coronary events (n=159), controls (n=318) | Cases had elevated absolute plasma sitosterol concentrations. Total cholesterol, LDL-Cholesterol, triglycerides and systolic blood pressure also higher in cases than in controls | CHD risk factors, i.e., LDL-cholesterol not matched between cases and controls. Conclusions drawn based on sitosterol only. Uni-variate analysis only. | Assmann et al. 2006[69] |
| Subjects | Results | Comments | Study |
|---|---|---|---|
| People with family history of CHD 413/619 (m/f) People without family history of coronary heart disease (CHD) 807/619 (m/f) |
Family history for CHD is not associated with elevated plant sterol-to-cholesterol ratios. Plasma sitosterol unrelated to artery calcium score | Large sample size. Age of subjects younger than in other studies. No absolute plasma plant sterol concentrations reported. |
Wilund et al. 2004[60] |
| Nested control study Cases with coronary events; 232/141 (m/f) Controls n = 758 |
Plant sterols not different between cases and controls. Sitosterol-to-cholesterol ratio lower in cases than contros. Campsterol-to-cholesterol ratio not different. |
Large sample size. Adjustent for major risk factors established by multivariate analysis. | Pinedo et al. 2007 Epic-Norfolk cohort[70] |
| Community based cross-sectional N=1,192; 47% male N=125 with CHD |
Plasma plant sterols and their ratios to cholesterol slightly but significantly lower in subjects with CHD compared to subjects without CHD. High plasma sitosterol concentrations associated with a markedly reduced CHD risk (Odd ratio (OR) 0.78;95CI 0.62-0.98. | Sitosterol higher in females than in males. Sitosterol lower in diabetics than in non-diabetics. | Fassbender et al. 2008 Longitudinal Aging Study Amsterdam (LASA)[71] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





