Submitted:
17 January 2025
Posted:
20 January 2025
You are already at the latest version
Abstract
Keywords:
Background
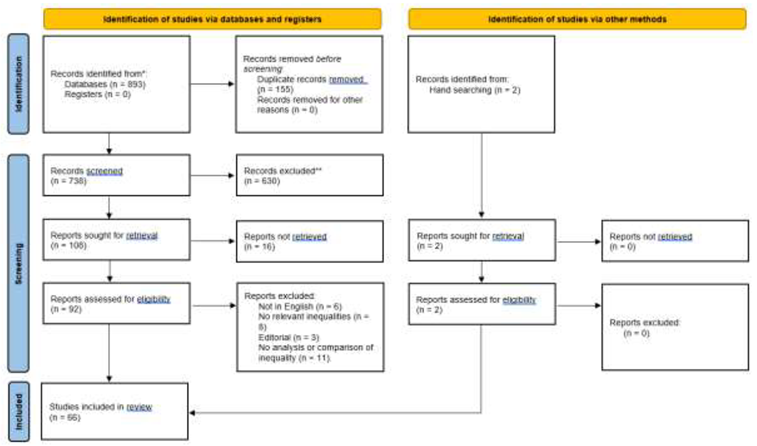
Methods
Study Design
Eligibility Criteria
Information Sources
Study Selection
Data Collection Process
Data Analysis
Results
Synthesis of Results
Geographical Inequalities
Socioeconomics Inequalities
Discussion
Recommendations
- (1)
- State their definition of inequality, inequity or disparities (if these terms are used),
- (2)
- State if they consider the differences between their study populations to be fair or unfair (or if they have made no judgements on this) and, if they consider the differences to be unfair,
- (3)
- State why (and if appropriate, when) they consider this inequality to be unfair (and therefore an inequity).
Limitations
Conclusions
References
- Scotland, N. Strokes: progressive stroke pathway https://www.gov.scot/publications/progressive-stroke-pathway/pages/9/2022.
- Morris, S.; Ramsay, A.I.G.; Boaden, R.J.; Hunter, R.M.; McKevitt, C.; Paley, L.; et al. Impact and sustainability of centralising acute stroke services in English metropolitan areas: retrospective analysis of hospital episode statistics and stroke national audit data. Bmj 2019, 364, l1. [Google Scholar] [CrossRef]
- Bernard, J.; Steinführer, A.; Klärner, A.; Keim-Klärner, S. Regional opportunity structures: A research agenda to link spatial and social inequalities in rural areas. Progress in Human Geography 2023, 47, 103–123. [Google Scholar] [CrossRef]
- Bray, B.D.; Paley, L.; Hoffman, A.; James, M.; Gompertz, P.; Wolfe, C.D.A.; et al. Socioeconomic disparities in first stroke incidence, quality of care, and survival: a nationwide registry-based cohort study of 44 million adults in England. Lancet Public Health 2018, 3, e185–e93. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Subramanian, S.V.; Almeida-Filho, N. A glossary for health inequalities. J Epidemiol Community Health 2002, 56, 647–652. [Google Scholar] [CrossRef] [PubMed]
- McCartney, G.; Collins, C.; Mackenzie, M. What (or who) causes health inequalities: theories, evidence and implications? Health Policy 2013, 113, 221–227. [Google Scholar] [CrossRef]
- Cookson, R.; Propper, C.; Asaria, M.; Raine, R. Socio-Economic Inequalities in Health Care in England. Fiscal Studies 2016, 37, 371–403. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O'Brien, K.K.; Colquhoun, H.; Levac, D.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Health, U.S.o.P. Search Filters for Various Databases https://libguides.sph.uth.tmc.edu/search_filters.
- Y Y, K H, S A, E G, A T, J M. ; et al. Access to Endovascular Thrombectomy for Stroke in Rural Versus Urban Regions. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques 2022, 49, 70–75. [Google Scholar] [CrossRef]
- De Havenon, A.; Sheth, K.; Johnston, K.C.; Delic, A.; Stulberg, E.; Majersik, J.; et al. Acute ischemic stroke interventions in the United States and racial, socioeconomic, and geographic disparities. Neurology 2021, 97, E2292–E303. [Google Scholar] [CrossRef]
- ME; ELG; BN; BS; KA Acute stroke alert activation, emergency service use, and reperfusion therapy in Sweden. Brain and behavior 2017, 7, e00654. [CrossRef] [PubMed]
- Kim, J.Y.; Lee, K.-J.; Kang, J.; Kim, B.J.; Kim, S.-E.; Oh, H.; et al. Acute stroke care in Korea in 2013-2014: National averages and disparities. Journal of Korean Medical Science 2020, 35. [Google Scholar] [CrossRef] [PubMed]
- J Y, ZK L, X X, M L, Y L, LD W. ; et al. Age and geographic disparities in acute ischaemic stroke prehospital delays in China: a cross-sectional study using national stroke registry data. The Lancet regional health Western Pacific 2023, 33, 100693. [Google Scholar] [CrossRef] [PubMed]
- MT C, N J, AJ H, AHY C, TP S, TJ P. ; et al. Air retrieval for clot retrieval; time-metrics and outcomes of stroke patients from rural and remote regions air-transported for mechanical thrombectomy at a state stroke unit. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 2019, 70, 151–156. [Google Scholar] [CrossRef]
- Scott, P.A.; Temovsky, C.J.; Lawrence, K.; Gudaitis, E.; Lowell, M.J. Analysis of Canadian population with potential geographic access to intravenous thrombolysis for acute ischemic stroke. Stroke 1998, 29, 2304–2310. [Google Scholar] [CrossRef]
- H C, L S, N W, Y H, Y L, M D. ; et al. Analysis on geographic variations in hospital deaths and endovascular therapy in ischaemic stroke patients: an observational cross-sectional study in China. BMJ open 2019, 9, e029079. [Google Scholar] [CrossRef]
- PS; WS; AS; MG Are there differences between rural and urban populations in long-term outcome after systemic cerebral thrombolysis in a hospital located in an agricultural region? Australia2014 2014. 2867 p.
- A P, J F, J H, K T, A T, O G. ; et al. Are there socio-economic inequities in access to reperfusion therapy: The stroke 69 cohort. Revue neurologique 2021, 177, 1168–1175. [Google Scholar] [CrossRef]
- KHK; YSR; SDS; SJK Association between neighborhood socioeconomic status and mechanical thrombectomy for acute ischemic stroke: A nationwide multilevel observational study. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 2023, 30, 918–926. [CrossRef]
- AG-A; ACC-P; MC-N; GP-V; FG-R Contribution of Onset-to-Alarm Time to Prehospital Delay in Patients with Ischemic Stroke. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 2019, 28, 104331. [CrossRef]
- Aguiar de Sousa D, Wilkie A, Norrving B, Macey C, Bassetti C, Tiu C. ; et al. Delivery of acute ischaemic stroke treatments in the European region in 2019 and 2020. European Stroke Journal 2023, 8, 618–628. [Google Scholar] [CrossRef]
- CYY; TB; PDP; APK Demographic Disparities in Proximity to Certified Stroke Care in the United States. Stroke 2021, 52, 2571–2579. [CrossRef]
- Mackenhauer, J.; Frischknecht Christensen, E.; Andersen, G.; Mainz, J.; Johnsen, S.P. Disparities in Reperfusion Therapy and Time Delays among Patients with Ischemic Stroke and a History of Mental Illness. Stroke 2022, 53, 3375–3385. [Google Scholar] [CrossRef]
- MAF; JS; CC; DGS; SRL Disparities in the Use of Intravenous t-PA among Ischemic Stroke Patients: Population-based Recent Temporal Trends. United States2019 2019-5. 1243-51 p.
- Llanos-Leyton, N.; Pardo, C.; Pinilla-Monsalve, G.D.; Arango, A.; Valderrama, J.; Pugliese, I.; et al. Disparities Influencing Functional Outcomes Between Rural and Urban Patients With Acute Stroke. Frontiers in Neurology 2022, 13. [Google Scholar] [CrossRef]
- AS; ELG; KA; BN; ME Education level and inequalities in stroke reperfusion therapy: observations in the Swedish stroke register. Stroke 2014, 45, 2762–2768. [CrossRef]
- M O-G, N PdlO, T J, S A, X J, P C. ; et al. Evolution of quality indicators in acute stroke during the RACECAT Trial: Impact in the general population. International journal of stroke : official journal of the International Stroke Society 2023, 18, 229–236. [Google Scholar] [CrossRef]
- Barragán-Prieto, A.; Pérez-Sánchez, S.; Moniche, F.; Moyano, R.V.; Delgado, F.; Martínez-Sánchez, P.; et al. Express improvement of acute stroke care accessibility in large regions using a centralized telestroke network. European Stroke Journal 2022, 7, 259–266. [Google Scholar] [CrossRef]
- JY; NC; PP; JS; JG; RG Gender differences and factors associated with the receipt of thrombolytic therapy in patients with acute myocardial infarction: a community-wide perspective. United States1996 1996-1. 43-50 p.
- Adeoye, O.; Albright, K.C.; Carr, B.G.; Wolff, C.; Mullen, M.T.; Abruzzo, T.; et al. Geographic access to acute stroke care in the United States. Stroke 2014, 45, 3019–3024. [Google Scholar] [CrossRef]
- MK K, R H, P G, AYX Y, AY J, C M. ; et al. Geographic Access to Stroke Care Services in Rural Communities in Ontario, Canada. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques 2020, 47, 301–308. [Google Scholar] [CrossRef]
- Kummer, B.R.; Lerario, M.P.; Hunter, M.D.; Wu, X.; Efraim, E.S.; Omran, S.S.; et al. Geographic analysis of mobile stroke unit treatment in a dense urban area: The new york city metronome registry. Journal of the American Heart Association 2019, 8. [Google Scholar] [CrossRef]
- Suolang, D.; Chen, B.J.; Wang, N.-Y.; Gottesman, R.F.; Faigle, R. Geographic and regional variability in racial and ethnic disparities in stroke thrombolysis in the United States. Stroke 2021, 52, E782–E7. [Google Scholar] [CrossRef]
- SG T, PA B, JH G, DA C, A D, JN F. ; et al. Geographic Disparities in Stroke Outcomes and Service Access: A Prospective Observational Study. Neurology 2022, 99, e414–e426. [Google Scholar]
- Abilleira, S.; Tebé, C.; de la Ossa, N.P.; Ribó, M.; Cardona, P.; Urra, X.; et al. Geographic dissemination of endovascular stroke thrombectomy in Catalonia within the 2011–2015 period. European Stroke Journal 2017, 2, 163–170. [Google Scholar] [CrossRef]
- FAF S, M R, N D-P, J R, T D, MB G. ; et al. Geographical Requirements for the Applicability of the Results of the RACECAT Study to Other Stroke Networks. Journal of the American Heart Association 2023, 12, e029965. [Google Scholar] [CrossRef]
- JL; JL; YM; PP; XH; WG Imbalanced Regional Development of Acute Ischemic Stroke Care in Emergency Departments in China. Emergency medicine international 2019, 2019, 3747910.
- N K, JM O, N S, A Z, A G, JK H.; et al. Influence of geography, stroke timing, and weather conditions on transport and workflow times: Results from a longitudinal 5-year Canadian provincial registry. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2023:15910199231196614.
- Arrich, J.; Müllner, M.; Lalouschek, W.; Greisenegger, S.; Crevenna, R.; Herkner, H. Influence of socioeconomic status and gender on stroke treatment and diagnostics. Stroke 2008, 39, 2066–2072. [Google Scholar] [CrossRef]
- S S, I T, R S, AC V, J D, AT G. ; et al. Late Hospital Arrival for Thrombolysis after Stroke in Southern Portugal: Who Is at Risk? Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 2019, 28, 900–905. [Google Scholar] [CrossRef]
- J F, F R, AM S, L D, N N, K T. ; et al. Measurement of the potential geographic accessibility from call to definitive care for patient with acute stroke. International journal of health geographics 2018, 17, 1. [Google Scholar] [CrossRef]
- Salwi, S.; Kelly, K.A.; Patel, P.D.; Fusco, M.R.; Mistry, E.A.; Mistry, A.M.; et al. Neighborhood Socioeconomic Status and Mechanical Thrombectomy Outcomes. Journal of Stroke and Cerebrovascular Diseases 2021, 30. [Google Scholar] [CrossRef]
- SA; VM; WAJ Outcomes after acute ischemic stroke in the United States: does residential ZIP code matter? England2015 2015-3-15. e001629 p.
- Sun, P.; Zheng, L.; Lin, M.; Cen, S.; Hammond, G.; Joynt Maddox, K.E.; et al. Persistent Inequities in Intravenous Thrombolysis for Acute Ischemic Stroke in the United States: Results from the Nationwide Inpatient Sample. medRxiv. 2023.
- Park, E.H.; Gil, Y.J.; Kim, C.; Kim, B.J.; Hwang, S.-S. Presence of Thrombectomy-capable Stroke Centers within Hospital Service Areas Explains Regional Variation in the Case Fatality Rate of Acute Ischemic Stroke in Korea. Journal of Preventive Medicine and Public Health 2021, 54, 385–394. [Google Scholar] [CrossRef]
- DR R, E M, C M, M P-P, B dT, N S. ; et al. A Prospective Comparative Study of Health Inequalities and the Epidemiology of Stroke in French Guiana and Dijon, France. Frontiers in public health 2022, 10, 849036. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Sandoval, J.L.; Briseño-Godínez, M.E.; Chiquete-Anaya, E.; Arauz-Góngora, A.; Troyo-Sanromán, R.; Parada-Garza, J.D.; et al. Public and Private Hospital Care Disparities of Ischemic Stroke in Mexico: Results from the Primer Registro Mexicano de Isquemia Cerebral (PREMIER) Study. Journal of Stroke and Cerebrovascular Diseases 2018, 27, 445–453. [Google Scholar] [CrossRef]
- M O, Y Z, X W, L S, L B, T R. ; et al. Quantifying regional variations in components of acute stroke unit (ASU) care in the international HeadPoST study. Journal of the neurological sciences 2020, 419, 117187. [Google Scholar] [CrossRef]
- MMK; DN; MFW; BLH Race and income disparity in ischemic stroke care: nationwide inpatient sample database, 2002 to 2008. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 2014, 23, 17–24. [CrossRef]
- Metcalf, D.; Zhang, D. Racial and ethnic disparities in the usage and outcomes of ischemic stroke treatment in the United States. Journal of Stroke and Cerebrovascular Diseases 2023, 32. [Google Scholar] [CrossRef]
- Attenello, F.J.; Adamczyk, P.; Wen, G.; He, S.; Zhang, K.; Russin, J.J.; et al. Racial and socioeconomic disparities in access to mechanical revascularization procedures for acute ischemic stroke. Journal of Stroke and Cerebrovascular Diseases 2014, 23, 327–334. [Google Scholar] [CrossRef]
- Mehta, A.M.; Fifi, J.T.; Shoirah, H.; Shigematsu, T.; Oxley, T.J.; Kellner, C.P.; et al. Racial and socioeconomic disparities in the use and outcomes of endovascular thrombectomy for acute ischemic stroke. American Journal of Neuroradiology 2021, 42, 1576–1583. [Google Scholar] [CrossRef]
- Hammond, G.; Waken, R.J.; Johnson, D.Y.; Towfighi, A.; Joynt Maddox, K.E. Racial Inequities Across Rural Strata in Acute Stroke Care and In-Hospital Mortality: National Trends Over 6 Years. Stroke 2022, 53, 1711–1719. [Google Scholar] [CrossRef]
- N D-P, H T, A B, I G-B, R C, P D. ; et al. Rate of intravenous thrombolysis for acute ischaemic stroke in the North-of-France region and evolution over time. Journal of neurology 2014, 261, 1320–1328. [Google Scholar] [CrossRef]
- Choi, J.C.; Hsia, R.Y.; Kim, A.S. Regional availability of mechanical embolectomy for acute ischemic stroke in California, 2009 to 2010. Stroke 2015, 46, 762–768. [Google Scholar] [CrossRef]
- AJG; SD; DB; WM; FB; HB Regional Deprivation, Stroke Incidence, and Stroke Care—An Analysis of Billing and Quality Assurance Data From the German State of Rhineland-Palatinate. Deutsches Arzteblatt international 2021, 118, 397–402.
- Dwyer, M.; Peterson, G.; Gall, S.; Kinsman, L.; Francis, K.; Ford, K.; et al. Regional differences in access to acute ischaemic stroke care and patient outcomes. Internal Medicine Journal 2020, 50, 965–971. [Google Scholar] [CrossRef]
- ES; GFH; MK; BM Regional differences in acute stroke admission and thrombolysis rates in the German federal state of Hesse. Germany2011 2011-9. 607-11 p.
- VY V, R B, J P, D K, S K, PN S. ; et al. Regional differences in ischemic stroke in India (north vs. south). International journal of stroke : official journal of the International Stroke Society 2019, 14, 706–714. [Google Scholar] [CrossRef]
- Dwyer, M.; Francis, K.; Peterson, G.M.; Ford, K.; Gall, S.; Phan, H.; et al. Regional differences in the care and outcomes of acute stroke patients in Australia: An observational study using evidence from the Australian Stroke Clinical Registry (AuSCR). BMJ Open 2021, 11. [Google Scholar] [CrossRef]
- Maeda, M.; Fukuda, H.; Matsuo, R.; Ago, T.; Kitazono, T.; Kamouchi, M. Regional disparity of reperfusion therapy for acute ischemic stroke in Japan: A retrospective analysis of nationwide claims data from 2010 to 2015. Journal of the American Heart Association 2021, 10. [Google Scholar] [CrossRef]
- Muñoz Venturelli, P.; Robinson, T.; Lavados, P.M.; Olavarría, V.V.; Arima, H.; Billot, L.; et al. Regional variation in acute stroke care organisation. Journal of the Neurological Sciences 2016, 371, 126–130. [Google Scholar] [CrossRef]
- Otsubo, T.; Goto, E.; Morishima, T.; Ikai, H.; Yokota, C.; Minematsu, K.; et al. Regional variations in in-hospital mortality, care processes, and spending in acute ischemic stroke patients in Japan. Journal of Stroke and Cerebrovascular Diseases 2015, 24, 239–251. [Google Scholar] [CrossRef]
- H S, K K, V S, S T, GP C, M N. ; et al. Reperfusion Therapy Frequency and Outcomes in Mild Ischemic Stroke in the United States. Stroke 2020, 51, 3241–3249. [Google Scholar] [CrossRef]
- ECL; KEJM; YW; DSK; RWY; RKW Rural-Urban Disparities in Outcomes of Myocardial Infarction, Heart Failure, and Stroke in the United States. United States2022 2022-1-25. 267-79 p.
- J M, J S, J L, HJ J, H K, J A. ; et al. Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database. International journal of environmental research and public health 2022, 19. [Google Scholar]
- CI; MP; ES; AG Social factors influencing hospital arrival time in acute ischemic stroke patients. Neuroradiology 2012, 54, 361–367. [CrossRef]
- WB; AAR; HJC Socioeconomic disparities in the utilization of mechanical thrombectomy for acute ischemic stroke. United States2014 2014-5. 979-84 p.
- Buus, S.M.O.; Schmitz, M.L.; Cordsen, P.; Johnsen, S.P.; Andersen, G.; Simonsen, C.Z. Socioeconomic Inequalities in Reperfusion Therapy for Acute Ischemic Stroke. Stroke 2022, 53, 2307–2316. [Google Scholar] [CrossRef]
- Ehrlich, M.E.; Han, B.; Lutz, M.; Ghorveh, M.G.; Okeefe, Y.A.; Shah, S.; et al. Socioeconomic Influence on Emergency Medical Services Utilization for Acute Stroke: Think Nationally, Act Locally. Neurohospitalist 2021, 11, 317–325. [Google Scholar] [CrossRef]
- Walter, S.; Fassbender, K.; Easton, D.; Schwarz, M.; Gardiner, F.; Langenberg, F.; et al. Stroke care equity in rural and remote areas - novel strategies. Vessel Plus 2021, 5. [Google Scholar] [CrossRef]
- Hammond, G.; Luke, A.A.; Elson, L.; Towfighi, A.; Joynt Maddox, K.E. Urban-Rural Inequities in Acute Stroke Care and In-Hospital Mortality. Stroke 2020, 51, 2131–2138. [Google Scholar] [CrossRef]
- Kleindorfer, D.; Xu, Y.; Moomaw, C.J.; Khatri, P.; Adeoye, O.; Hornung, R. US geographic distribution of rt-PA utilization by hospital for acute ischemic stroke. Stroke 2009, 40, 3580–3584. [Google Scholar] [CrossRef]
- Stein, L.K.; Maillie, L.; Erdman, J.; Loebel, E.; Mayman, N.; Sharma, A.; et al. Variation in US acute ischemic stroke treatment by hospital regions: Limited endovascular access despite evidence. Journal of NeuroInterventional Surgery. 2023. [CrossRef]
- Quality AfHRa. National (Nationwide) Inpatient Sample (NIS) https://hcup-us.ahrq.gov/news/exhibit_booth/nis_brochure.jsp.
- NHS Core20PLUS5 – An approach to reducing health inequalities for children and young people https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/core20plus5-cyp/.
- Ministry of Housing, C.L.G. English indices of deprivation 2019 https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019: GOV.UK; 2019.
- Mitchell, S.; Potash, E.; Barocas, S.; apos Amour, A.; Lum, K. Algorithmic Fairness: Choices, Assumptions, and Definitions. Annual Review of Statistics and Its Application 2021, 8(Volume 8, 2021):141-63.
- Disparities, O.f.H.I. Health Disparities and health inequalities: Applying all our health https://www.gov.uk/government/publications/health-disparities-and-health-inequalities-applying-all-our-health/health-disparities-and-health-inequalities-applying-all-our-health2022.
| Inequality or Inequity type | Number of measures of this inequality/inequity |
|---|---|
| Geographic | 81 (58.27%) |
| Rurality | 27 (19.42%) |
| Geographic regions | 24 (17.27%) |
| Time or distance to hospital | 22 (15.83) |
| Type or designa[11–76tion of hospitals | 8 (5.76%) |
| Socioeconomic | 58 (51.73%) |
| Income | 17 (12.23%) |
| Medical Insurance status | 17 (12.23%) |
| Education | 12 (8.63%) |
| Deprivation | 7 (5.04%) |
| Employment | 3 (2.16%) |
| Other | 2 (1.44%) |
| Total | 139 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





