Submitted:
02 January 2025
Posted:
03 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Breathwork, Mental Imagery and Insomnia Management
3. Virtual Reality and Insomnia

4. Framework for Insomnia Protocol
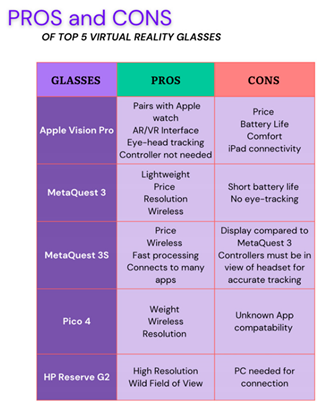
5. Comparison of Virtual Reality Devices for Insomnia Management

6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boeldt, D.; McMahon, E.; McFaul, M.; Greenleaf, W. Using Virtual Reality Exposure Therapy to Enhance Treatment of Anxiety Disorders: Identifying Areas of Clinical Adoption and Potential Obstacles. Front. Psychiatry 2019, 10, 773. [Google Scholar] [CrossRef] [PubMed]
- Raji, M.A.; Olodo, H.B.; Oke, T.T.; Addy, W.A.; Ofodile, O.C.; Oyewole, A.T. BUSINESS STRATEGIES IN VIRTUAL REALITY: A REVIEW OF MARKET OPPORTUNITIES AND CONSUMER EXPERIENCE. Int. J. Manag. Entrep. Res. 2024, 6, 722–736. [Google Scholar] [CrossRef]
- Asemi, A. and A. Ko. Contribution & Power of Virtual Reality in Corporate World: A Conceptual Review. in 2024 Third International Conference on Distributed Computing and High Performance Computing (DCHPC). 2024.
- Afsar, M.M.; Saqib, S.; Ghadi, Y.Y.; Alsuhibany, S.A.; Jalal, A.; Park, J. Body Worn Sensors for Health Gaming and e-Learning in Virtual Reality. Comput. Mater. Contin. 2022, 73, 4763–4777. [Google Scholar] [CrossRef]
- Hamad, A.; Jia, B. How Virtual Reality Technology Has Changed Our Lives: An Overview of the Current and Potential Applications and Limitations. Int. J. Environ. Res. Public Heal. 2022, 19, 11278. [Google Scholar] [CrossRef] [PubMed]
- Trotta, N.; Leccese, A.; Fiore, P.; Meyerbröker, K. Virtual Reality: Characteristics and application in anxiety disorders and other clinical settings. 2023; 92. [Google Scholar] [CrossRef]
- Rockstroh, C.; Blum, J.; Göritz, A.S. Combining VR and Biofeedback. J. Media Psychol. 2020, 32, 176–186. [Google Scholar] [CrossRef]
- Halbig, A.; Latoschik, M.E. A Systematic Review of Physiological Measurements, Factors, Methods, and Applications in Virtual Reality. Front. Virtual Real. 2021, 2. [Google Scholar] [CrossRef]
- de Zambotti, M. , et al., When sleep goes virtual: the potential of using virtual reality at bedtime to facilitate sleep. Sleep, 2020. 43(12).
- Vince, J. Introduction to Virtual Reality; Springer: New York, NY, USA, 2004. [Google Scholar]
- Javvaji, C.K.; Reddy, H.; Vagha, J.D.; Taksande, A.; Kommareddy, A.; Reddy, N.S.; Jr. , A.K. Immersive Innovations: Exploring the Diverse Applications of Virtual Reality (VR) in Healthcare. Cureus 2024, 16. [Google Scholar] [CrossRef]
- Jerdan, S.W.; Grindle, M.; van Woerden, H.C.; Boulos, M.N.K. Head-Mounted Virtual Reality and Mental Health: Critical Review of Current Research. JMIR Serious Games 2018, 6, e14. [Google Scholar] [CrossRef]
- Bhaskar, S.; Hemavathy, D.; Prasad, S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J. Fam. Med. Prim. Care 2016, 5, 780–784. [Google Scholar] [CrossRef] [PubMed]
- Kahn-Greene, E.T.; Killgore, D.B.; Kamimori, G.H.; Balkin, T.J.; Killgore, W.D. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007, 8, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, P.L.; Trontell, M.C.; Mazar, M.F.; Edelman, N.H. Sleep Deprivation Decreases Ventilatory Response to CO2 But Not Load Compensation. Chest 1983, 84, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Olfson, M.; Wall, M.; Liu, S.-M.; Morin, C.M.; Blanco, C. Insomnia and Impaired Quality of Life in the United States. J. Clin. Psychiatry 2018, 79. [Google Scholar] [CrossRef] [PubMed]
- Jerath, R.; Beveridge, C.; Barnes, V.A. Self-Regulation of Breathing as an Adjunctive Treatment of Insomnia. Front. Psychiatry 2019, 9, 780. [Google Scholar] [CrossRef] [PubMed]
- Knutson, K.L.; Spiegel, K.; Penev, P.; Van Cauter, E. The metabolic consequences of sleep deprivation. 11. [CrossRef]
- Palagini, L.; Bianchini, C. Pharmacotherapeutic management of insomnia and effects on sleep processes, neural plasticity, and brain systems modulating stress: A narrative review. Front. Neurosci. 2022, 16, 893015. [Google Scholar] [CrossRef] [PubMed]
- Roth, T. , Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of Clinical Sleep Medicine, 2007. 3(5 suppl): p. S7-S10.
- Shahly, V. , et al., The Associations of Insomnia With Costly Workplace Accidents and Errors: Results From the America Insomnia Survey. Archives of General Psychiatry, 2012. 69(10): p. 1054-1063.
- Jerath, R.; Beveridge, C.; Jensen, M.; Paladiya, R. The Therapeutic Role of Guided Mental Imagery in Treating Stress and Insomnia: A Neuropsychological Perspective. Open J. Med Psychol. 2020, 09, 21–39. [Google Scholar] [CrossRef]
- Manconi, M.; Ferri, R.; Miano, S.; Maestri, M.; Bottasini, V.; Zucconi, M.; Ferini-Strambi, L. Sleep architecture in insomniacs with severe benzodiazepine abuse. Clin. Neurophysiol. 2017, 128, 875–881. [Google Scholar] [CrossRef]
- Felipe Maraucci Ribeiro de, M. , et al., Benzodiazepines and Sleep Architecture: A Systematic Review. CNS & Neurological Disorders - Drug Targets, 2023. 22(2): p. 172-179.
- Avidan, A.; Palmer, L.; Doan, J.F.; Baran, R.W. Insomnia medication use and the probability of an accidental event in an older adult population. Drug, Heal. Patient Saf. 2010, 2, 225–232. [Google Scholar] [CrossRef]
- Datta, K.; Tripathi, M.; Mallick, H.N. Yoga Nidra: An innovative approach for management of chronic insomnia- A case report. Sleep Sci. Pr. 2017, 1, 7. [Google Scholar] [CrossRef]
- Basta, M.; Chrousos, G.P.; Vela-Bueno, A.; Vgontzas, A.N. Chronic Insomnia and the Stress System. 2. [CrossRef]
- Jerath, R.; Edry, J.W.; Barnes, V.A.; Jerath, V. Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. 67. [CrossRef]
- Su, H.; Xiao, L.; Ren, Y.; Xie, H.; Sun, X.-H. Effects of mindful breathing combined with sleep-inducing exercises in patients with insomnia. World J. Clin. Cases 2021, 9, 8740–8748. [Google Scholar] [CrossRef] [PubMed]
- Jerath, R.; Beveridge, C. Harnessing the Spatial Foundation of Mind in Breaking Vicious Cycles in Anxiety, Insomnia, and Depression: The Future of Virtual Reality Therapy Applications. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Pavic, K.; Chaby, L.; Gricourt, T.; Vergilino-Perez, D. Feeling Virtually Present Makes Me Happier: The Influence of Immersion, Sense of Presence, and Video Contents on Positive Emotion Induction. Cyberpsychology, Behav. Soc. Netw. 2023, 26, 238–245. [Google Scholar] [CrossRef]
- Parker, S.; Bharati, S.V.; Fernandez, M. Defining Yoga-Nidra: Traditional Accounts, Physiological Research, and Future Directions. Int. J. Yoga Ther. 2013, 23, 11–16. [Google Scholar] [CrossRef]
- Pandi-Perumal, S.R.; Spence, D.W.; Srivastava, N.; Kanchibhotla, D.; Kumar, K.; Sharma, G.S.; Gupta, R.; Batmanabane, G. The Origin and Clinical Relevance of Yoga Nidra. Sleep Vigil. 2022, 6, 61–84. [Google Scholar] [CrossRef]
- Kavi, P.C. , Chapter 3 - Conscious entry into sleep: Yoga Nidra and accessing subtler states of consciousness, in Progress in Brain Research, T.D. Ben-Soussan, J. Glicksohn, and N. Srinivasan, Editors. 2023, Elsevier. p. 43-60.
- de Mendonça, F.M.R. , et al., Benzodiazepines and Sleep Architecture: A Systematic Review. CNS Neurol Disord Drug Targets, 2023. 22(2): p. 172-179.
- McEntire, D.M.; Kirkpatrick, D.R.; Kerfeld, M.J.; Hambsch, Z.J.; Reisbig, M.D.; Agrawal, D.K.; Youngblood, C.F. Effect of sedative-hypnotics, anesthetics and analgesics on sleep architecture in obstructive sleep apnea. Expert Rev. Clin. Pharmacol. 2014, 7, 787–806. [Google Scholar] [CrossRef] [PubMed]
- Stojanovich, L. , Stress and autoimmunity. Autoimmunity Reviews, 2010. 9(5): p. A271-A276.
- Stojanovich, L.; Marisavljevich, D. Stress as a trigger of autoimmune disease. Autoimmun. Rev. 2008, 7, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Bierhaus, A., P. M. Humpert, and P.P. Nawroth, Linking Stress to Inflammation. Anesthesiology Clinics of North America, 2006. 24(2): p. 325-340.
- Carney, C.E.; Harris, A.L.; Falco, A.; Edinger, J.D. The Relation between Insomnia Symptoms, Mood, and Rumination about Insomnia Symptoms. J. Clin. Sleep Med. 2013, 09, 567–575. [Google Scholar] [CrossRef]
- Bonnet, M.; Arand, D. Hyperarousal and insomnia. Sleep Med. Rev. 1997, 1, 97–108. [Google Scholar] [CrossRef]
- Raja, D. , et al. Exploring the Benefits of Immersion in Abstract Information Visualization. 2004.
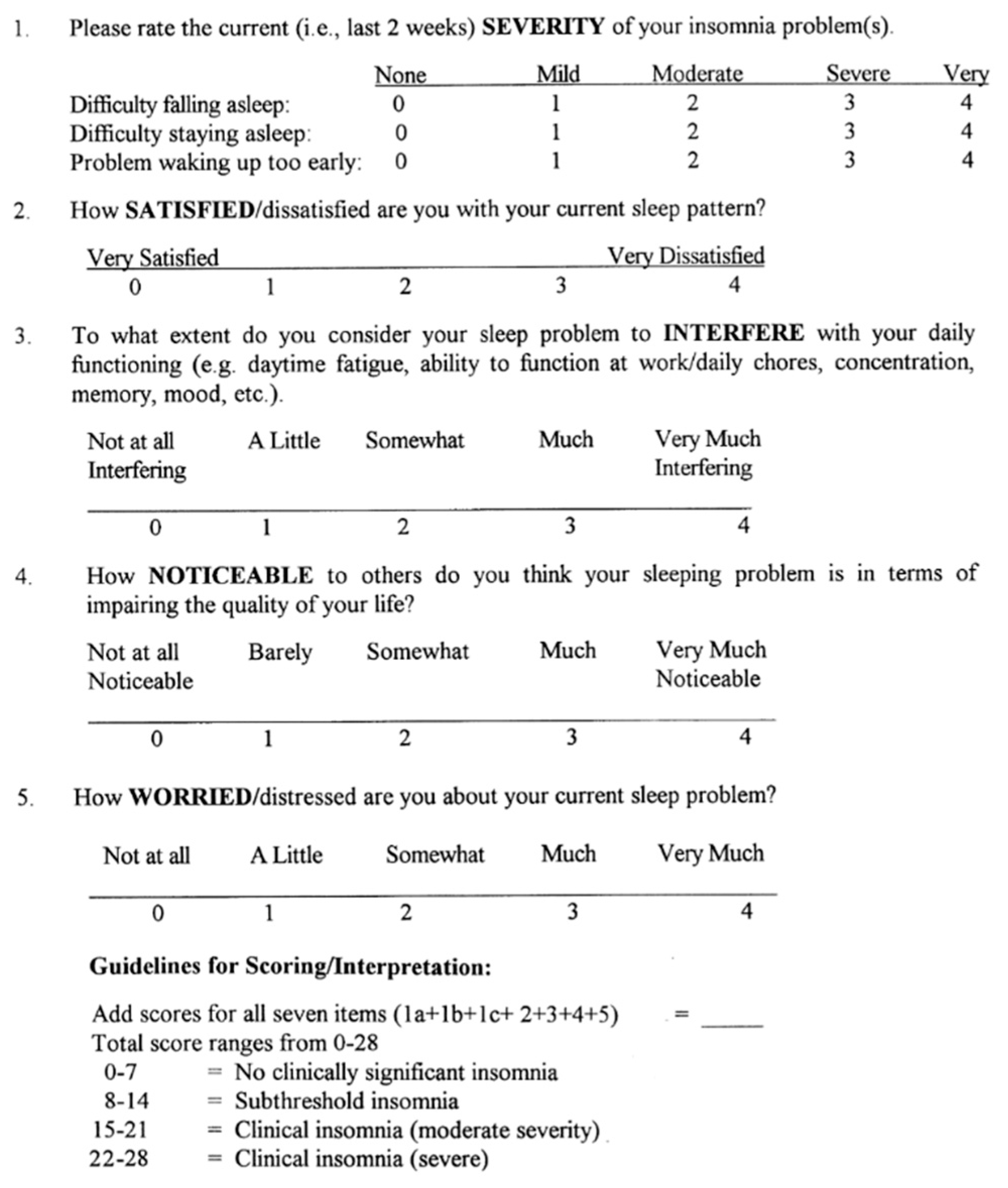
- Bastien, C.H., A. Vallières, and C.M. Morin, Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2001. 2(4): p. 297-307.
- Wan, Y.; Gao, H.; Zhou, K.; Zhang, X.; Xue, R.; Zhang, N. Virtual reality improves sleep quality and associated symptoms in patients with chronic insomnia. Sleep Med. 2024, 122, 230–236. [Google Scholar] [CrossRef]
- Chitra, J.; Eremita, M.D.S. Effect of Virtual Reality on Sleep-Deprived Individuals. Indian J. Psychol. Med. 2023, 45, 610–613. [Google Scholar] [CrossRef]
- Kim, K.-Y.; Hur, M.-H.; Kim, W.-J. Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students. Healthcare 2024, 12, 1581. [Google Scholar] [CrossRef] [PubMed]
- Floris, C.; Solbiati, S.; Landreani, F.; Damato, G.; Lenzi, B.; Megale, V.; Caiani, E.G. Feasibility of Heart Rate and Respiratory Rate Estimation by Inertial Sensors Embedded in a Virtual Reality Headset. Sensors 2020, 20, 7168. [Google Scholar] [CrossRef]
- Riva, G.; Serino, S. Virtual Reality in the Assessment, Understanding and Treatment of Mental Health Disorders. J. Clin. Med. 2020, 9, 3434. [Google Scholar] [CrossRef]
- Jawarneh, M.; Alshar'E, M.; Dewi, D.A.; Al Nasar, M.; Almajed, R.; Ibrahim, A. The Impact of Virtual Reality Technology on Jordan’s Learning Environment and Medical Informatics among Physicians. Int. J. Comput. Games Technol. 2023, 2023, 1–9. [Google Scholar] [CrossRef]
- Hofmann, S.M.; Klotzsche, F.; Mariola, A.; Nikulin, V.; Villringer, A.; Gaebler, M. Decoding subjective emotional arousal from EEG during an immersive virtual reality experience. eLife 2021, 10, e64812. [Google Scholar] [CrossRef] [PubMed]
1 Detailed specific protocols for different grades is an intellectual property of Mind Body Technologies located in Augusta GA. This protocol is designed for use by developers and can be obtained by contacting the company via contact information provided. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




