1. Introduction
The recent coronavirus disease 2019 (COVID-19) pandemic has profoundly impacted public health, society, and the global economy. Estimating the cumulative number of individuals infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated COVID-19-related mortality remains a considerable challenge, primarily due to uncontrolled confounding factors in COVID-19 epidemiology, particularly undertesting and underreporting, especially in underdeveloped regions [
1]. According to the World Health Organization (WHO) COVID-19 dashboard, over 777 million people may have experienced one or more severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and approximately 7.1 million deaths may be attributable to (or associated with) COVID-19 by the end of 2024 [
2]. However, these figures are widely recognized as underestimates, with the WHO suggesting that the actual number of COVID-19 deaths could be up to 2.7 times higher (i.e., approximately 20 million) [
3]. If accurate, this would position COVID-19 as the second deadliest pandemic of the past century, surpassed only by the Spanish flu, which caused an estimated 40–50 million deaths [
4].
Beyond the acute phase, SARS-CoV-2 infection can lead to persistent and complex sequelae, variably defined post COVID, long-COVID, or long-haul COVID syndrome [
5,
6,
7]. This emerging healthcare challenge prompted the WHO to introduce a specific 10
th revision of the International Classification of Diseases (ICD-10) code, U09.9, in October 2021 [
8]. This code, designated as “Post COVID-19 condition, unspecified,” encompasses a range of symptoms persisting or emerging at least three months after initial infection and lasting for over two months, with no alternative explanation [
8]. The introduction of this ICD-10 code has facilitated the systematic classification, monitoring, and study of post COVID cases, enabling healthcare providers and scientists to adopt a more standardized approach.
The WHO estimates the incidence of post COVID syndrome to be 10–20% [
8]. However, this figure may also be underestimated, as evidenced by more recent data. A meta-analysis by Sk Abd Razak et al. [
10], which included 16 studies, estimated the global prevalence of post COVID syndrome at 41.8% (95% confidence interval (CI): 39.7–43.9%). This prevalence showed minor temporal variation, with rates of 45.1% at three months, and 41.3% at both six- and twelve-month post-recovery. Women were found to have a higher prevalence than men (52.8% vs. 41.3%). Children are also affected by post COVID syndrome, as highlighted by a systematic review by Silva et al. [
10], which reported that 29% of children experienced exercise intolerance, while respiratory symptoms and psychological distress affected 10–12% of children three to 12 months post-infection.
Another recent meta-analysis published by Atchley-Challenner et al. [
11] identified the most prevalent symptoms of post COVID syndrome, including respiratory complains (e.g., shortness of breath, fatigue), general pain, cognitive and behavioral impairments (e.g., brain fog, insomnia, anxiety, depression), sensory disturbances (e.g., loss of taste or smell), cardiac symptoms (e.g., palpitations, chest pain), hair loss, fever, and flu-like syndrome. These symptoms collectively contribute to reduce the quality of life [
12] and highlights a significant issue, as the post COVID syndrome could represent an “epidemic within the pandemic” [
13]. The socioeconomic impact of the post COVID condition is also substantial, as increased medical care and hospital admissions have been shown to raise healthcare costs by 23% in the year following an acute SARS-CoV-2 infection [
14], and this economic burden can extend to affected families, causing financial strain and psychological stress [
15].
Although the precise mechanisms underlying post COVID syndrome remain unclear, current hypotheses include viral persistence, autoimmunity, unresolved tissue damage, immune dysregulation, microbiome dysbiosis, endothelial and neuronal inflammation, mitochondrial dysfunction, and formation of microclots [
16]. Risk factors for developing long-term complications include severe acute illness, pre-existing comorbidities, older age, female sex, and lack of vaccination [
17].
Despite progress in characterizing and monitoring long-COVID prevalence and morbidity, specific mortality data attributable to this syndrome are lacking to the best of our knowledge, mostly because of inconsistent definitions, coding inaccuracies, and documentation challenges. To address this gap, we have designed a retrospective study to systematically analyze the burden and demographic characteristics of post COVID mortality, using the U09.9 ICD-10 code and data from the US National Center for Health Statistics.
2. Materials and Methods
We conducted an electronic search in the US National Center for Health Statistics using the Wide-Ranging Online Data for Epidemiologic Research (WONDER) interface, which provides comprehensive statistics derived from death certificates for all US residents [
18]. Specifically, we accessed the "Provisional Multiple Cause of Death" database, which contains population and death count data across the US up to the most recently
censused week. Death certificates include complete demographic, social, and geographic details, along with the primary underlying cause of death.
For this study, we used the primary keyword "Post COVID-19," corresponding to the ICD-10 code U09.9. The search was extended to the period from October 2021 (when the ICD-10 code U09.9 was first introduced) through the end of December 2024. Additional searches were performed using keywords for "gender," "ten-year age groups," and "place of death." In the ICD-10 classification, U09.9 is defined as "post-acute sequela of COVID-19" and encompasses various specific conditions and related ICD-10 codes associated with COVID-19, including chronic respiratory failure (J96.1), loss of smell (R43.8), loss of taste (R43.8), multisystem inflammatory syndrome (M35.81), pulmonary embolism (I26), and pulmonary fibrosis (J84.10) [
19].
The results of our searches were provided as total number of deaths (and percentages), and age-adjusted or crude mortality rate (×100,000) with 95% confidence intervals (95% CI). According to the database, age-adjusted death rates were calculated as weighted averages of age-specific death rates, using a fixed age-specific population as weights to enable comparisons of relative mortality risks among population groups and over time. Statistically significant differences among groups were assessed using one-way analysis of variance (ANOVA) applied to the annual number of deaths, the mean death rate, and its standard error, using StatPages (Interactive Statistical Calculation). Statistical significance was set at p<0.05.
This study was conducted in accordance with the Declaration of Helsinki, the provisions of the relevant local legislation, and was exempt from Institutional Review Board review, as the WONDER database is freely searchable and fully anonymized.
3. Results
The results of our analysis are presented in
Table 1. As of the end of December 2024, a cumulative number of 2,653 US deaths were classified with the ICD-10 U09.9 code for “post COVID” as the primary cause of death, corresponding to an age-adjusted mortality rate of 0.089 (95% CI, 0.085–0.092) ×100,000 population.
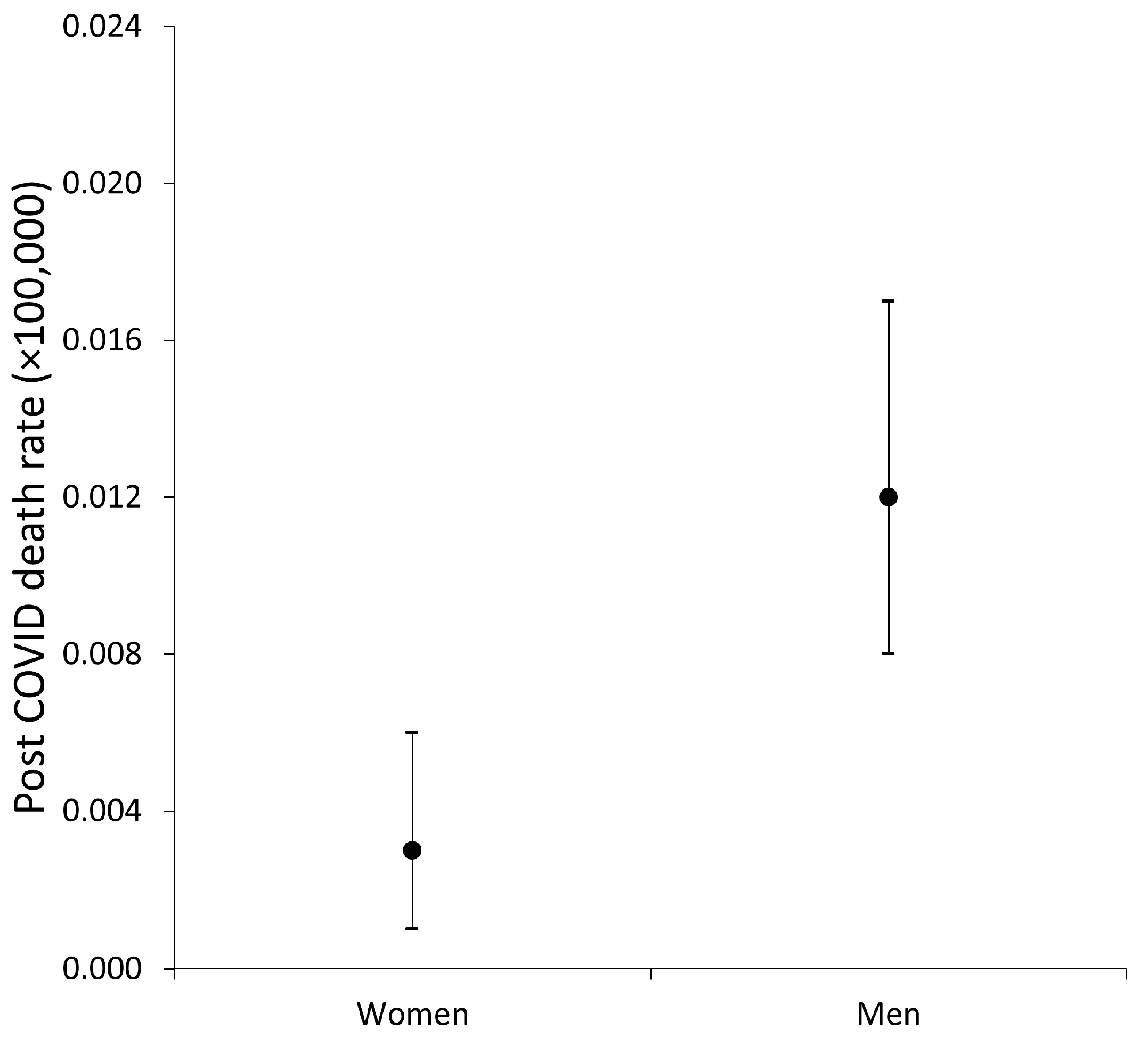
Mortality was significantly higher among males (0.098; 95% CI: 0.092–0.104 ×100,000) compared to females (0.081; 95% CI: 0.077–0.086 ×100,000; f=23.0; p<0.001), with a standardized difference of 0.017 (95% CI: 0.010–0.024) ×100,000 (
Figure 1).
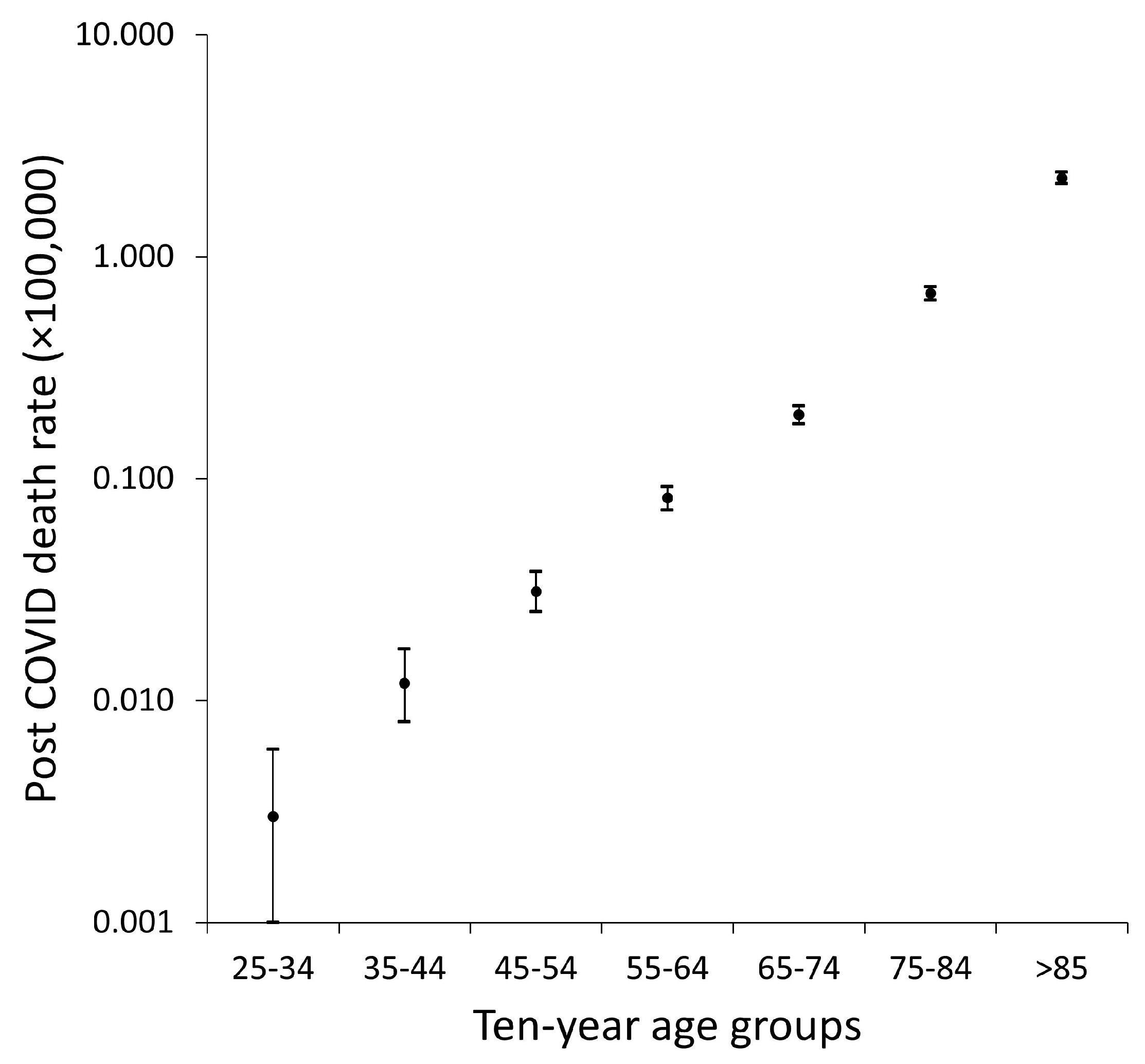
An age-dependent trend was evident, with crude mortality rates for post COVID condition increasing steadily and significantly with advancing age (f=178; p<0.001), as illustrated in
Figure 1. When analyzed on a logarithmic scale, the relationship between crude death rate and age appeared nearly linear (
Figure 2).
The distribution of post COVID condition deaths by place of death is also summarized in
Table 1. Most deaths occurred at the decedent’s home (33.0%), followed by nursing homes or long-term care facilities (26.3%), medical facilities (as inpatients; 24.1%), and hospice facilities (7.7%).
4. Discussion
The findings of this study provide a detailed epidemiological overview of the mortality burden associated with post COVID condition in the US, identified using the ICD-10 U09.9 code within the National Center for Health Statistics. Our analysis highlights significant demographic patterns, emphasizing the complexity and public health implications of this emerging condition.
As of the end of 2024, over 2,600 US deaths have been classified under the ICD-10 U09.9 code, representing a critical yet likely underestimated aspect of the long-term impact of the ongoing COVID-19 pandemic. Although an age-adjusted mortality of 0.089 ×100,000 indicates a relatively infrequent occurrence of deaths directly attributed to post COVID condition at a national level, this rate demonstrates substantial variation across specific subpopulations, reflecting disparities rooted in demographic and social determinants of health. These findings underscore the necessity of targeted analyses and interventions to mitigate the post COVID mortality burden proactively.
The observed higher mortality rate in men compared to women (0.098 vs. 0.081 ×100,000) does not align with the known prevalence of post COVID syndrome in the general population, which has consistently been reported as higher in females than in males. A comprehensive analysis by the Global Burden of Disease Long COVID Collaborators estimated the prevalence of symptom clusters 3 months after acute, symptomatic SARS-CoV-2 infection to be nearly twice as high in females than in males (10.6% vs. 5.4%) [
20]. Similarly, a prospective cohort study involving 377 individuals clinically recovered from acute SARS-CoV-2 infection found females to be over three times more likely to be diagnosed with long-COVID syndrome 1–3 months after viral clearance (adjusted odds ratio (AOR), 3.3; 95% CI, 1.8–6.2) [
21]. Supporting these findings, a nationwide, retrospective cohort study in Scotland [
22] with over 4,676,390 participants showed a higher rate of post COVID syndrome diagnosis in females compared to males (65.1% vs. 50.4%). Similarly, a population-representative survey of over 3,000 US adults aged ≥18 years reported nearly double the prevalence of post COVID syndrome in females compared to males 12 months after acute infection (adjusted prevalence ratio (APR), 1.84; 95% CI, 1.40–2.42) [
23]. Thus, the unforeseen male predominance in post COVID mortality may reflect biological factors such as hormonal differences influencing immune responses and a higher prevalence of comorbidities like cardiovascular disease and diabetes in men. Nonetheless, the significant gender disparity in mortality (0.017×100,000) highlights an actionable difference that warrants further investigation to identify specific interventions in males.
We then observed a clear age-dependent relationship in post COVID mortality, with rates increasing steadily and significantly with advancing age. Unlike the gender effect, age has occasionally been identified as a determinant of post COVID syndrome. In the study by Bai et al. [
21], advanced age was associated with a higher risk of developing long-COVID (AOR, 1.03 per 10-year increase; 95% CI, 1.01–1.05). However, this finding has been contradicted by other epidemiological investigations. A nationwide population cohort study conducted in Scotland and involving 198,096 individuals with acute SARS-CoV-2 infection, reported a higher prevalence of long-COVID symptoms 6 months after recovery in the 40–59 age group, with a substantial decline in prevalence among those aged ≥70 years [
24]. Similarly, the US population-representative survey by Robertson et al. found a lower prevalence of long-COVID syndrome in individuals aged ≥65 years (APR, 0.43; 95% CI, 0.27–0.66) [
23]. However, Ford et al., using data from the US national Household Pulse Survey, reported higher rates of significant activity limitations among adults aged >40 years with long-COVID and a marked 1-year decline in post COVID symptoms was observed primarily in individuals aged <60 years [
25]. This inherently suggests that, although post COVID condition may be more prevalent in younger age groups, its morbidity and mortality consequences appear to be significantly more severe in older individuals. Although the biological relationship between the prevalence and mortality of post COVID syndrome remains unclear, several plausible explanations can be proposed. Older individuals are more likely to experience severe acute disease, prolonged hospitalizations, and complications, making them more susceptible to post COVID sequelae, as clearly by the meta-analysis conducted by Li et al. [
26].
The distribution of post COVID mortality by place of death provides valuable insights into the healthcare settings most affected by the post COVID condition. A substantial proportion of deaths occurred at the decedent’s home (33.0%), followed by nursing homes or long-term care facilities (26.3%). These findings underscore two critical aspects: challenges in care access—such as home deaths potentially reflecting isolation, barriers to timely medical intervention, or under-recognition of post COVID condition [
27,
28]—and the heightened vulnerability of elderly populations residing in long-term care settings, as many individuals in these facilities may already have severe underlying comorbidities that could be exacerbated by post COVID sequelae [
29].
Altogether, our findings highlight the need for a more structured approach to identifying, managing, and preventing post COVID mortality, providing useful recommendations to lower the risk of death from or with post COVID syndrome. In particular, the disproportionate impact on males, older individuals, and residents of long-term care facilities emphasizes the importance of targeted interventions in subjects with post COVID condition. Prioritizing vaccination for these high-risk groups—not only with COVID-19 vaccines but also those for influenza, pneumococci, and respiratory syncytial virus—is crucial to reducing the risk of clinical deterioration and death among vulnerable individuals [
30]. Facilitating access to post COVID care for elderly individuals and those with mobility limitations is also imperative [
31], alongside the expanded use of remote monitoring systems and telehealth to detect health, physical, or cognitive decline promptly [
32]. Moreover, healthcare providers would need enhanced training to improve the recognition and management of post COVID condition, especially outside the hospital environment [
33]. Addressing gender and age disparities in post COVID mortality demands a deeper understanding of the biological and social determinants of health, so that public health initiatives could be more focused on raising awareness and ensuring equitable access to diagnostic and therapeutic resources.
Although our study provides significant insights on post COVID mortality, we acknowledge some limitations in our analysis. First, reliance on the ICD-10 U09.9 code may underestimate the true burden of post COVID deaths, mostly caused by variability in documentation and coding practices across the US. Second, the 2024 data remain provisional, reflecting inherent delays in death certificate processing and reporting through the end of the year. Future studies should hence be aimed to address these limitations by collecting additional information not available through the WONDER interface of the US National Center for Health Statistics, including data on the severity of acute SARS-CoV-2 infection, access to COVID-19 vaccines, ethnic origin, census, and educational level. Continued monitoring of post COVID mortality trends over time will also be critical for understanding the long-term trajectory of this syndrome as the acute phase of the pandemic recedes. Finally, additional research into the precise biological mechanisms underlying post COVID mortality would be essential for developing effective health strategies to mitigate the burden of post COVID deaths.
5. Conclusions
The results of our analysis highlight the significant yet complex impact of post COVID condition on mortality. Although the absolute number of deaths remains relatively low compared to acute COVID-19 fatalities, the observed patterns reveal critical areas for targeted intervention and resource allocation. Addressing the identified disparities and gaps in care will enable healthcare systems to more effectively manage the ongoing burden of post COVID condition and improve outcomes for affected individuals.
Author Contributions
Conceptualization, G.L. and F.S.G.; software, G.L.; formal analysis, G.L.; data curation, G.L.; writing—original draft preparation, G.L.; writing—review and editing, F.S.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, the provisions of the relevant local legislation, and was exempt from Institutional Review Board review, as the CDC WONDER database is freely searchable and fully anonymized.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| COVID-19 |
Coronavirus Disease 2019 |
| WHO |
World Health Organization |
| SARS-CoV-2 |
Severe Acute Respiratory Syndrome Coronavirus 2 |
| ICD-10 |
10th revision of the International Classification of Diseases |
| CI |
Confidence Interval |
| WONDER |
Wide-Ranging Online Data for Epidemiologic Research |
| ANOVA |
One-Way Analysis of Variance |
| AOR |
Adjusted Odds Ratio |
| APR |
Adjusted Prevalence Ratio |
References
- Lippi, G.; Mattiuzzi, C.; Henry, B.M. Uncontrolled confounding in COVID-19 epidemiology. Diagnosis 2022, 10, 200–202. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO COVID-19 dashboard. Available at: https://data.who.int/dashboards/covid19/cases. Last accessed, January 1, 2025.
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2022, 613, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Sampath, S.; Khedr, A.; Qamar, S.; Tekin, A.; Singh, R.; Green, R.; Kashyap, R. Pandemics Throughout the History. Cureus 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Favresse, J.; Plebani, M. Addressing standardized definitions of post-COVID and long-COVID. cclm 2023, 61, 1361–1362. [Google Scholar] [CrossRef]
- Gheorghita, R.; Soldanescu, I.; Lobiuc, A.; Sturdza, O.A.C.; Filip, R.; Bercu, A.C. ; Dimian, M.; Mangul, S.; Covasa, M. The knowns and unknowns of long COVID-19: from mechanisms to therapeutical approaches. Front. Immunol. 2024, 15, 1344086. [CrossRef]
- Gutzeit, J.; Weiß, M.; Nürnberger, C.; Lemhöfer, C.; Appel, K.S.; Pracht, E.; Reese, J.-P.; Lehmann, C.; Polidori, M.C.; Hein, G.; et al. Definitions and symptoms of the post-COVID syndrome: an updated systematic umbrella review. Eur. Arch. Psychiatry Clin. Neurosci. 2024, 1–12. [Google Scholar] [CrossRef]
- World Health Organization. Post COVID-19 condition (Long COVID). Available at: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition. Last accessed, January 1, 2025.
- Razak, R.S.A.; Ismail, A.; Aziz, A.F.A.; Suddin, L.S.; Azzeri, A.; Sha’ari, N.I. Post-COVID syndrome prevalence: a systematic review and meta-analysis. BMC Public Heal. 2024, 24, 1–19. [Google Scholar] [CrossRef]
- da Silva, M.M.; Benites, M.N.; Castro, Y.M.; Moura, P.V.; Zhang, L. Prevalence of symptoms of post-COVID-19 condition (long COVID) in children hospitalized with COVID-19: A systematic review of observational studies. Pediatr. Pulmonol. 2024, 59, 3159–3169. [Google Scholar] [CrossRef]
- Atchley-Challenner, R.; Strasser, Z.; Krishnamoorthy, A.; Pant, D.; Chibnik, L.B.; Karlson, E.W. Long COVID: A Narrative Review and Meta-Analysis of Individual Symptom Frequencies. COVID 2024, 4, 1513–1545. [Google Scholar] [CrossRef]
- Kim, J.; Duru, E.E.; Weir, P.; Lee, S. Long COVID Is Associated with Decreased Quality of Life and Increased Mental Disability. COVID 2024, 4, 1719–1730. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Long COVID: An Epidemic within the Pandemic. COVID 2023, 3, 773–776. [Google Scholar] [CrossRef]
- Scott, A.; Ansari, W.; Khan, F.; Chambers, R.; Benigno, M.; Di Fusco, M.; McGrath, L.; Malhotra, D.; Draica, F.; Nguyen, J.; et al. Substantial health and economic burden of COVID-19 during the year after acute illness among US adults at high risk of severe COVID-19. BMC Med. 2024, 22, 1–19. [Google Scholar] [CrossRef]
- Mukhida, S.; Khan, S. Does long covid-19 affect the quality of life only to Covid-19 patients or family member also? . J. Fam. Med. Prim. Care 2024, 13, 5442–5443. [Google Scholar] [CrossRef] [PubMed]
- Al-Aly, Z.; Topol, E. Solving the puzzle of Long Covid. Science 2024, 383, 830–832. [Google Scholar] [CrossRef]
- Muthuka, J.K.; Nzioki, J.M.; Kelly, J.O.; Musangi, E.N.; Chebungei, L.C.; Nabaweesi, R.; Kiptoo, M.K. Prevalence and Predictors of Long COVID-19 and the Average Time to Diagnosis in the General Population: A Systematic Review, Meta-Analysis and Meta-Regression. COVID 2024, 4, 968–981. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are from the final Multiple Cause of Death Files, 2018-2022, and from provisional data for years 2023-2024, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10-provisional.html on Jan 2, 2025.
- International Classification of Diseases. ICD-10-CM Diagnosis Code U09.9. Available at: https://www.icd10data.com/ICD10CM/Codes/U00-U85/U00-U49/U09-/U09.9. Last accessed, January 1, 2025.
- Global Burden of Disease Long COVID Collaborators; Hanson, S. W.; Abbafati, C.; Aerts, J.G.; Al-Aly, Z.; Ashbaugh, C.; Ballouz, T.; Blyuss, O.; Bobkova, P.; Bonsel, G.; et al. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA 2022, 328, 1604–1615. [CrossRef]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin. Microbiol. Infect. 2021, 28, 611.e9–611e16. [Google Scholar] [CrossRef]
- Jeffrey, K.; Woolford, L.; Maini, R.; Basetti, S.; Batchelor, A.; Weatherill, D.; White, C.; Hammersley, V.; Millington, T.; Macdonald, C.; et al. Prevalence and risk factors for long COVID among adults in Scotland using electronic health records: a national, retrospective, observational cohort study. eClinicalMedicine 2024, 71, 102590. [Google Scholar] [CrossRef]
- Robertson, M.M.; A Qasmieh, S.; Kulkarni, S.G.; A Teasdale, C.; E Jones, H.; McNairy, M.; Borrell, L.N.; Nash, D. The Epidemiology of Long Coronavirus Disease in US Adults. Clin. Infect. Dis. 2022, 76, 1636–1645. [Google Scholar] [CrossRef]
- Hastie, C.E.; Lowe, D.J.; McAuley, A.; Mills, N.L.; Winter, A.J.; Black, C.; Scott, J.T.; O’donnell, C.A.; Blane, D.N.; Browne, S.; et al. True prevalence of long-COVID in a nationwide, population cohort study. Nat. Commun. 2023, 14, 1–6. [Google Scholar] [CrossRef]
- Ford, N.D.; Slaughter, D.; Edwards, D.; Dalton, A.; Perrine, C.; Vahratian, A.; Saydah, S. Long COVID and Significant Activity Limitation Among Adults, by Age — United States, June 1–13, 2022, to June 7–19, 2023. Mmwr-Morbidity Mortal. Wkly. Rep. 2023, 72, 866–870. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhong, X.; Wang, Y.; Zeng, X.; Luo, T.; Liu, Q. Clinical determinants of the severity of COVID-19: A systematic review and meta-analysis. PLOS ONE 2021, 16, e0250602. [Google Scholar] [CrossRef]
- Au, L.; Capotescu, C.; Eyal, G.; Finestone, G. Long covid and medical gaslighting: Dismissal, delayed diagnosis, and deferred treatment. SSM - Qual. Res. Heal. 2022, 2, 100167–100167. [Google Scholar] [CrossRef] [PubMed]
- Sunkersing, D.; Ramasawmy, M.; A Alwan, N.; Clutterbuck, D.; Mu, Y.; Horstmanshof, K.; Banerjee, A.; Heightman, M. What is current care for people with Long COVID in England? A qualitative interview study. BMJ Open 2024, 14, e080967. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.D.; Lone, N.I.; Baillie, J.K. Comorbidities, multimorbidity and COVID-19. Nat. Med. 2023, 29, 334–343. [Google Scholar] [CrossRef]
- Reynard, C.; Campling, J.; Gordon, A.L.; Kassianos, G.; Liu, H.-H.; Richter, A.; Vyse, A.; Wiseman, D.J.; Wright, H.; Ellsbury, G. Adult risk groups for vaccine preventable respiratory infections: an overview of the UK environment. Expert Rev. Vaccines 2024, 23, 1052–1067. [Google Scholar] [CrossRef]
- Choe, E.Y.; Du, Y.; Sun, G. Decline in older adults’ daily mobility during the COVID-19 pandemic: the role of individual and built environment factors. BMC Public Heal. 2022, 22, 1–10. [Google Scholar] [CrossRef]
- Kim, Y.K.; Ang, S. Older Adults With Functional Limitations and Their Use of Telehealth During COVID-19. Res. Aging 2022, 45, 609–619. [Google Scholar] [CrossRef]
- Frenk, J.; Chen, L.C.; Chandran, L.; Groff, E.O.H.; King, R.; Meleis, A.; Fineberg, H.V. Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet 2022, 400, 1539–1556. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).