Submitted:
18 December 2024
Posted:
20 December 2024
You are already at the latest version
Abstract
Virtual reality (VR) demonstrates significant potential to improve rehabilitation outcomes for musculoskeletal conditions and chronic pain. However, the field faces notable challenges, including inconsistent terminology, a lack of specialized/comprehensive software solutions, and an overwhelming variety of hardware options, which can make it difficult for healthcare professionals without technical expertise to identify the most suitable tools for clinical use. This article explores the current state of VR in the rehabilitation of musculoskeletal conditions and chronic pain, focusing on terminology discrepancies, available hardware and software solutions, and key professional associations shaping the field. A review of the current state of terminology is essential to address inconsistencies that risk perpetuating misuse and limiting the applicability of research findings. Building on this review, we propose a conceptual framework for understanding VR that aligns more closely with the capabilities of current VR technology. A comprehensive overview of VR hardware and software can assist healthcare professionals in selecting appropriate technologies for clinical practice, guide researchers in designing interventions, and inform developers on unmet needs in the field. Furthermore, understanding key professional associations provides valuable direction for those engaged in virtual rehabilitation, enabling them to access resources, foster collaboration, and stay informed about the latest advancements in the domain.
Keywords:
1. Introduction
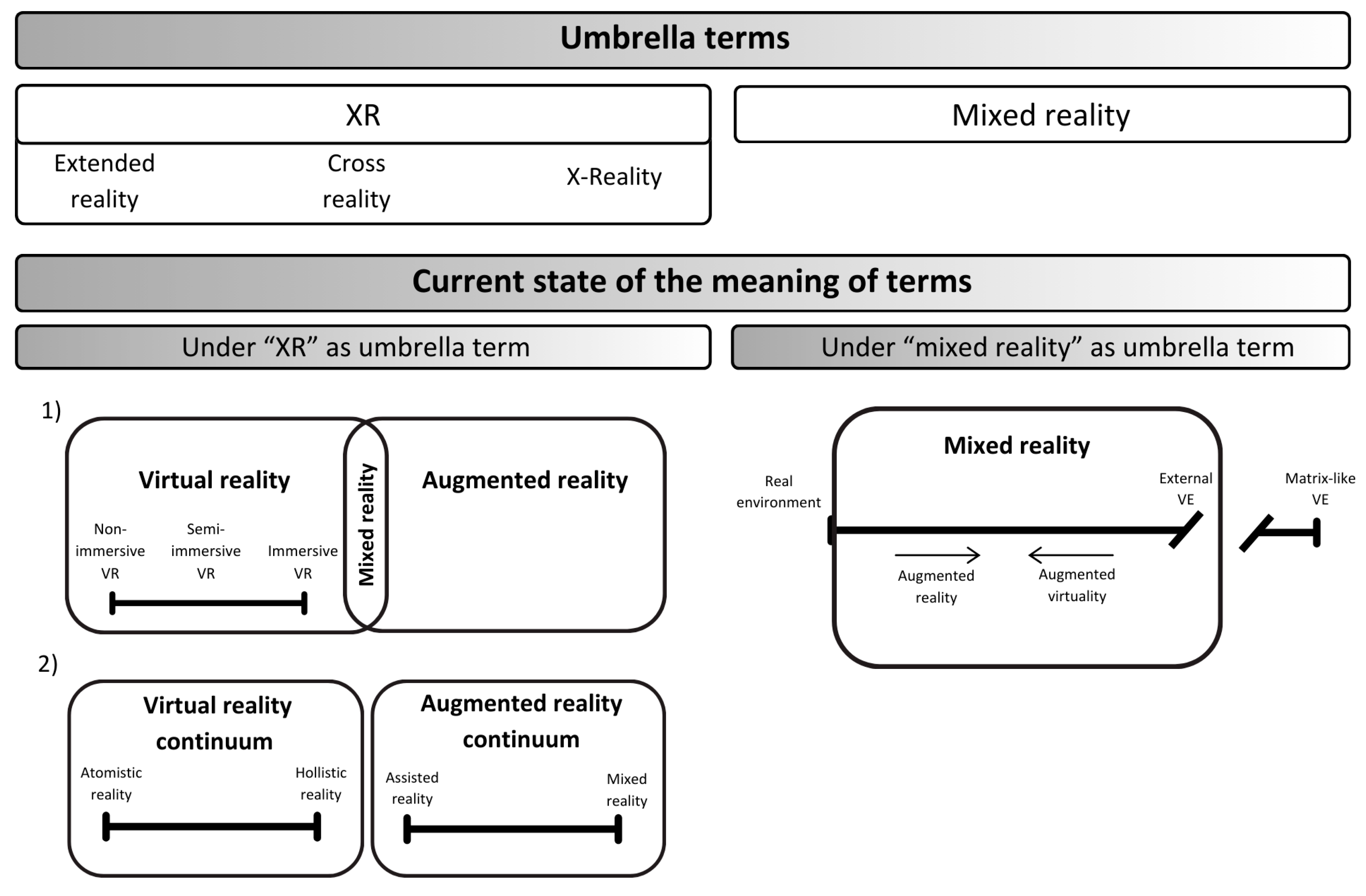
2. The Ambiguity of Virtual Reality Terminology in Healthcare and Beyond
2.1. Modern Definitions and Concepts of Virtual Reality and Related Technologies
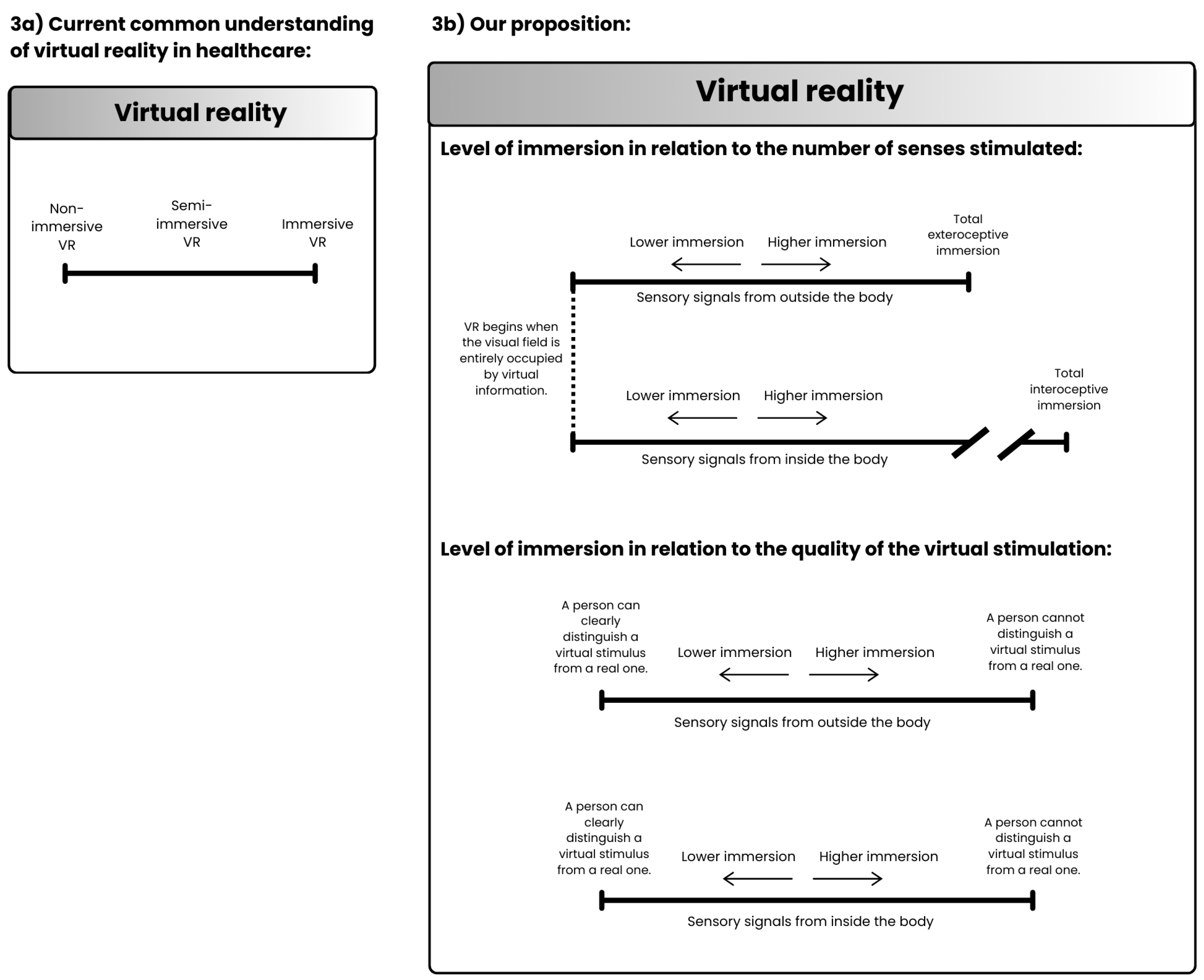
2.2. Categorization of Virtual Reality in Healthcare: Subtypes Based on Levels of Immersion
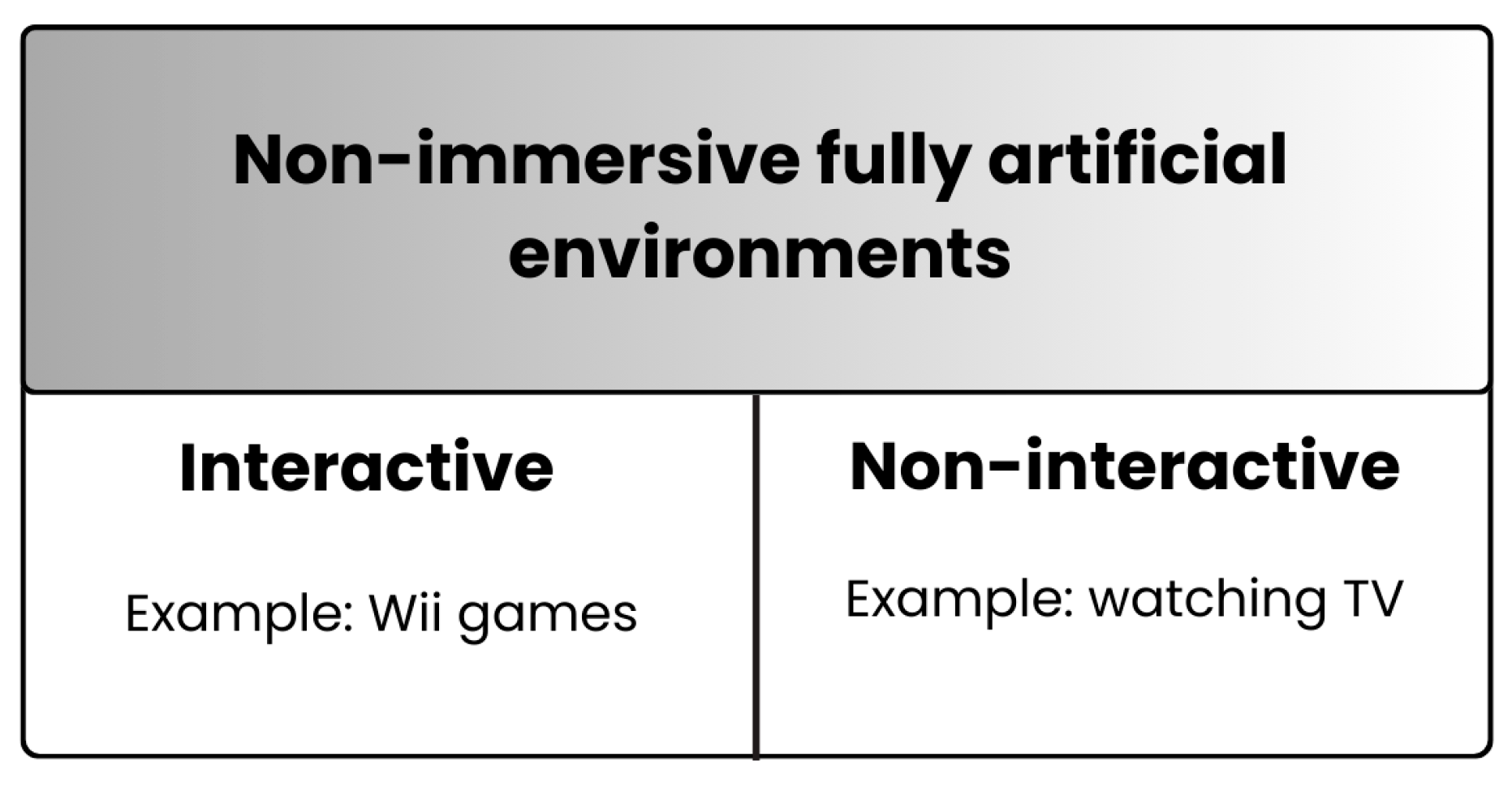
2.3. Rethinking the Meaning of Virtual Reality: A Proposed Framework
Proposition 1: VR begins when visual field is entirely occupied with virtual information.
Proposition 2: What is currently referred to as "non-immersive VR" should be distinguished from VR and excluded from the umbrella term encompassing VR and related technologies.
Proposition 3: VR should be divided into two continua of immersion depth based on exteroceptive and interoceptive system involvement.
Proposition 4: Immersion should be categorized based on the number of stimulated senses and the quality of virtual stimulation.
3. Immersive Virtual Reality: Hardware and Software Perspectives
3.1. Overview of Immersive Virtual Reality Hardware
3.2. Overview of Immersive Virtual Reality Software
4. Key Organizations Advancing Virtual Reality in Healthcare and Rehabilitation
5. Conclusions and Future Directions
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoffman, H.G.; Chambers, G.T.; Meyer, W.J.; Arceneaux, L.L.; Russell, W.J.; Seibel, E.J.; Richards, T.L.; Sharar, S.R.; Patterson, D.R. Virtual Reality as an Adjunctive Non-Pharmacologic Analgesic for Acute Burn Pain during Medical Procedures. Ann Behav Med 2011, 41, 183–191. [CrossRef]
- Noble, T.; Boone, L.; El Helou, A. The Role of Virtual Reality as Adjunctive Therapy to Spinal Cord Stimulation in Chronic Pain: A Feasible Concept? Frontiers in Pain Research 2023, 4. [CrossRef]
- Padilla-Castañeda, M.A.; Sotgiu, E.; Barsotti, M.; Frisoli, A.; Orsini, P.; Martiradonna, A.; Laddaga, C.; Bergamasco, M. An Orthopaedic Robotic-Assisted Rehabilitation Method of the Forearm in Virtual Reality Physiotherapy. J Healthc Eng 2018, 2018, 7438609. [CrossRef]
- Chaplin, E.; Karatzios, C.; Benaim, C. Clinical Applications of Virtual Reality in Musculoskeletal Rehabilitation: A Scoping Review. Healthcare 2023, 11, 3178. [CrossRef]
- Opara, M.; Kozinc, Ž. Which Muscles Exhibit Increased Stiffness in People with Chronic Neck Pain? A Systematic Review with Meta-Analysis. Front Sports Act Living 2023, 5. [CrossRef]
- Cortés-Pérez, I.; Desdentado-Guillem, J.M.; Camacho-Delgado, M.S.; Del Rocío Ibancos-Losada, M.; Obrero-Gaitán, E.; Lomas-Vega, R. Virtual Reality-Based Therapy after Anterior Cruciate Ligament Injury Effectively Reduces Pain and Improves Knee Function, Movement Patterns, and Dynamic Balance: A Systematic Review and Meta-Analysis. Knee Surg Sports Traumatol Arthrosc 2024. [CrossRef]
- Su, S.; Wang, R.; Chen, Z.; Zhou, F.; Zhang, Y. The Effectiveness of Extended Reality on Relieving Pain after Total Knee Arthroplasty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Arch Orthop Trauma Surg 2024, 144, 3217–3226. [CrossRef]
- Kumar, V.; Vatkar, A.J.; Kataria, M.; Dhatt, S.S.; Baburaj, V. Virtual Reality Is Effective in the Management of Chronic Low Back Ache in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur Spine J 2024, 33, 474–480. [CrossRef]
- Li, R.; Li, Y.; Kong, Y.; Li, H.; Hu, D.; Fu, C.; Wei, Q. Virtual Reality-Based Training in Chronic Low Back Pain: Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Med Internet Res 2024, 26, e45406. [CrossRef]
- Ye, G.; Koh, R.G.L.; Jaiswal, K.; Soomal, H.; Kumbhare, D. The Use of Virtual Reality in the Rehabilitation of Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis. Clin J Pain 2023, 39, 491–500. [CrossRef]
- Wang, S.; Sun, J.; Yin, X.; Li, H. Effect of Virtual Reality Technology as Intervention for People with Kinesiophobia: A Meta-Analysis of Randomised Controlled Trials. J Clin Nurs 2023, 32, 3074–3086. [CrossRef]
- Harvie, D.S.; Kelly, J.; Kluver, J.; Deen, M.; Spitzer, E.; Coppieters, M.W. A Randomized Controlled Pilot Study Examining Immediate Effects of Embodying a Virtual Reality Superhero in People with Chronic Low Back Pain. Disabil Rehabil Assist Technol 2024, 19, 851–858. [CrossRef]
- Darnall, B.D.; Krishnamurthy, P.; Tsuei, J.; Minor, J.D. Self-Administered Skills-Based Virtual Reality Intervention for Chronic Pain: Randomized Controlled Pilot Study. JMIR Form Res 2020, 4, e17293. [CrossRef]
- Annesi, J.J.; Mazas, J. Effects of Virtual Reality-Enhanced Exercise Equipment on Adherence and Exercise-Induced Feeling States. Percept Mot Skills 1997, 85, 835–844. [CrossRef]
- Hosseini, M.; Thomas, R.; Pilutti, L.; Fallavollita, P.; Jutai, J.W. Acceptance of Physical Activity Virtual Reality Games by Residents of Long-Term Care Facilities: A Qualitative Study. PLoS One 2024, 19, e0305865. [CrossRef]
- Rauschnabel, P.A.; Felix, R.; Hinsch, C.; Shahab, H.; Alt, F. What Is XR? Towards a Framework for Augmented and Virtual Reality. Comput Human Behav 2022, 133, 107289. [CrossRef]
- Laato, S.; Xi, N.; Spors, V.; Thibault, M.; Hamari, J. Making Sense of Reality: A Mapping of Terminology Related to Virtual Reality, Augmented Reality, Mixed Reality, XR and the Metaverse. In Proceedings of the Proceedings of the 57th Hawaii International Conference on System Sciences; Hawaii International Conference on System Sciences, 2024; pp. 6625–6634.
- Skarbez, R.; Smith, M.; Whitton, M.C. Revisiting Milgram and Kishino’s Reality-Virtuality Continuum. Front Virtual Real 2021, 2. [CrossRef]
- Abbas, J.R.; O’Connor, A.; Ganapathy, E.; Isba, R.; Payton, A.; McGrath, B.; Tolley, N.; Bruce, I.A. What Is Virtual Reality? A Healthcare-Focused Systematic Review of Definitions. Health Policy Technol 2023, 12, 100741. [CrossRef]
- Fijačko, N.; Štiglic, G.; Gsaxner, C.; Chang, T.P.; Greif, R. Rethinking Realities: A Call for Accurate Terminology in EXtended Reality Studies. Resusc Plus 2024, 17, 100558. [CrossRef]
- Apple Vision Pro Available online: https://www.apple.com/apple-vision-pro/ (accessed on 10 December 2024).
- Kordyaka, B.; Park, S.; Krath, J.; Laato, S. Exploring the Relationship Between Offline Cultural Environments and Toxic Behavior Tendencies in Multiplayer Online Games. ACM Transactions on Social Computing 2023, 6, 1–20. [CrossRef]
- Ditchburn, J.-L.; van Schaik, P.; Dixon, J.; MacSween, A.; Martin, D. The Effects of Exergaming on Pain, Postural Control, Technology Acceptance and Flow Experience in Older People with Chronic Musculoskeletal Pain: A Randomised Controlled Trial. BMC Sports Sci Med Rehabil 2020, 12, 63. [CrossRef]
- Gava, V.; Fialho, H.R.F.; Calixtre, L.B.; Barbosa, G.M.; Kamonseki, D.H. Effects of Gaming on Pain-Related Fear, Pain Catastrophizing, Anxiety, and Depression in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Games Health J 2022, 11, 369–384. [CrossRef]
- Fu, H.; Garrett, B.; Tao, G.; Cordingley, E.; Ofoghi, Z.; Taverner, T.; Sun, C.; Cheung, T. Virtual Reality–Guided Meditation for Chronic Pain in Patients With Cancer: Exploratory Analysis of Electroencephalograph Activity. JMIR Biomed Eng 2021, 6, e26332. [CrossRef]
- Nambi, G.; Abdelbasset, W.K.; Alsubaie, S.F.; Saleh, A.K.; Verma, A.; Abdelaziz, M.A.; Alkathiry, A.A. Short-Term Psychological and Hormonal Effects of Virtual Reality Training on Chronic Low Back Pain in Soccer Players. J Sport Rehabil 2021, 30, 884–893. [CrossRef]
- Fatoye, F.; Gebrye, T.; Mbada, C.E.; Fatoye, C.T.; Makinde, M.O.; Ayomide, S.; Ige, B. Cost Effectiveness of Virtual Reality Game Compared to Clinic Based McKenzie Extension Therapy for Chronic Non-Specific Low Back Pain. Br J Pain 2022, 16, 601–609. [CrossRef]
- Afzal, M.W.; Ahmad, A.; Mohseni Bandpei, M.A.; Gillani, S.A.; Hanif, A.; Sharif Waqas, M. Effects of Virtual Reality Exercises and Routine Physical Therapy on Pain Intensity and Functional Disability in Patients with Chronic Low Back Pain. J Pak Med Assoc 2022, 72. [CrossRef]
- Rezaei, I.; Razeghi, M.; Ebrahimi, S.; Kayedi, S.; Rezaeian Zadeh, A. A Novel Virtual Reality Technique (Cervigame®) Compared to Conventional Proprioceptive Training to Treat Neck Pain: A Randomized Controlled Trial. J Biomed Phys Eng 2018. [CrossRef]
- Oliveira, L.K.R.; Marques, A.P.; Andrade, K.F.A.; Assis, J.C.S. de; Brito, A.L.; Souza, G.S.; Callegari, B. Virtual Reality in Improving Anticipatory Postural Adjustments to Step Initiation in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial. Games Health J 2024, 13, 100–108. [CrossRef]
- Henríquez-Jurado, J.M.; Osuna-Pérez, M.C.; García-López, H.; Lomas-Vega, R.; López-Ruiz, M. del C.; Obrero-Gaitán, E.; Cortés-Pérez, I. Virtual Reality-Based Therapy for Chronic Low Back and Neck Pain: A Systematic Review with Meta-Analysis. EFORT Open Rev 2024, 9, 685–699. [CrossRef]
- Elaraby, A.E.R.; Shahien, M.; Jahan, A.M.; Etoom, M.; Bekhet, A.H. The Efficacy of Virtual Reality Training in the Rehabilitation of Orthopedic Ankle Injuries: A Systematic Review and Meta-Analysis. Advances in rehabilitation science and practice 2023, 12, 11795727231151636. [CrossRef]
- García-Sánchez, M.; Obrero-Gaitán, E.; Piñar-Lara, M.; Osuna-Pérez, M.C.; Díaz-Fernández, Á.; Cortés-Pérez, I. Early Rehabilitation Using Virtual Reality-Based Therapy Can Enhance Hip Function and Self-Perception of Improvement Following Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. Geriatr Nurs 2024, 60, 593–601. [CrossRef]
- Skarbez, R.; Smith, M.; Whitton, M. It Is Time to Let Go of “Virtual Reality.” Commun ACM 2023, 66, 41–43. [CrossRef]
- Schuermans, J.; Van Hootegem, A.; Van den Bossche, M.; Van Gendt, M.; Witvrouw, E.; Wezenbeek, E. Extended Reality in Musculoskeletal Rehabilitation and Injury Prevention - A Systematic Review. Physical Therapy in Sport 2022, 55, 229–240. [CrossRef]
- Ziker, C.; Truman, B.; Dodds, H. Cross Reality (XR): Challenges and Opportunities Across the Spectrum. In; 2021; pp. 55–77.
- Yang, Y.; Keivanpour, S.; Imbeau, D. Integrating X-Reality and Lean into End-of-Life Aircraft Parts Disassembly Sequence Planning: A Critical Review and Research Agenda. The International Journal of Advanced Manufacturing Technology 2023, 127, 2181–2210. [CrossRef]
- Gaballa, A.; Cavalcante, R.S.; Lamounier, E.; Soares, A.; Cabibihan, J.-J. Extended Reality “X-Reality” for Prosthesis Training of Upper-Limb Amputees: A Review on Current and Future Clinical Potential. IEEE Trans Neural Syst Rehabil Eng 2022, 30, 1652–1663. [CrossRef]
- Cheung, J.C.-W.; Cheung, D.S.K.; Ni, M.; Chen, K.-W.; Mao, Y.-J.; Feng, L.; Lam, W.-K.; Wong, D.W.-C.; Leung, A.K.-L. X-Reality for Phantom Limb Management for Amputees: A Systematic Review and Meta-Analysis. Engineered Regeneration 2023, 4, 134–151. [CrossRef]
- Combalia, A.; Sanchez-Vives, M. V.; Donegan, T. Immersive Virtual Reality in Orthopaedics—a Narrative Review. Int Orthop 2024, 48, 21–30. [CrossRef]
- Favre, J.; Cantaloube, A.; Jolles, B.M. Rehabilitation for Musculoskeletal Disorders: The Emergence of Serious Games and the Promise of Personalized Versions Using Artificial Intelligence. J Clin Med 2023, 12, 5310. [CrossRef]
- Moreau, S.; Thérond, A.; Cerda, I.H.; Studer, K.; Pan, A.; Tharpe, J.; Crowther, J.E.; Abd-Elsayed, A.; Gilligan, C.; Tolba, R.; et al. Virtual Reality in Acute and Chronic Pain Medicine: An Updated Review. Curr Pain Headache Rep 2024, 28, 893–928. [CrossRef]
- Milgram, P.; Kishino, F. A Taxonomy of Mixed Reality Visual Displays. IEICE Trans Inf Syst 1994, 12, 1321–1329.
- Wei, W.; Tang, H.; Luo, Y.; Yan, S.; Ji, Q.; Liu, Z.; Li, H.; Wu, F.; Yang, S.; Yang, X. Efficacy of Virtual Reality Exercise in Knee Osteoarthritis Rehabilitation: A Systematic Review and Meta-Analysis. Front Physiol 2024, 15. [CrossRef]
- Brady, N.; Dejaco, B.; Lewis, J.; McCreesh, K.; McVeigh, J.G. Physiotherapist Beliefs and Perspectives on Virtual Reality Supported Rehabilitation for the Management of Musculoskeletal Shoulder Pain: A Focus Group Study. PLoS One 2023, 18, e0284445. [CrossRef]
- Thuilier, E.; Carey, J.; Dempsey, M.; Dingliana, J.; Whelan, B.; Brennan, A. Virtual Rehabilitation for Patients with Osteoporosis or Other Musculoskeletal Disorders: A Systematic Review. Virtual Real 2024, 28, 93. [CrossRef]
- Chirico, A.; Lucidi, F.; De Laurentiis, M.; Milanese, C.; Napoli, A.; Giordano, A. Virtual Reality in Health System: Beyond Entertainment. A Mini-Review on the Efficacy of VR During Cancer Treatment. J Cell Physiol 2016, 231, 275–287. [CrossRef]
- Manlapaz, D.G.; Sole, G.; Jayakaran, P.; Chapple, C.M. Exergaming to Improve Balance and Decrease the Risk of Falling in Adults with Knee Osteoarthritis: A Mixed-Methods Feasibility Study. Physiother Theory Pract 2022, 38, 2428–2440. [CrossRef]
- Mete, E.; Sari, Z. The Efficacy of Exergaming in Patients with Knee Osteoarthritis: A Randomized Controlled Clinical Trial. Physiotherapy Research International 2022, 27. [CrossRef]
- Abd-Alrazaq, A.; Al-Jafar, E.; Alajlani, M.; Toro, C.; Alhuwail, D.; Ahmed, A.; Reagu, S.M.; Al-Shorbaji, N.; Househ, M. The Effectiveness of Serious Games for Alleviating Depression: Systematic Review and Meta-Analysis. JMIR Serious Games 2022, 10, e32331. [CrossRef]
- Hadjiat, Y.; Marchand, S. Virtual Reality and the Mediation of Acute and Chronic Pain in Adult and Pediatric Populations: Research Developments. Frontiers in Pain Research 2022, 3. [CrossRef]
- Zhou, S.; Gromala, D.; Wang, L. Ethical Challenges of Virtual Reality Technology Interventions for the Vulnerabilities of Patients With Chronic Pain: Exploration of Technician Responsibility. J Med Internet Res 2023, 25, e49237. [CrossRef]
- Franze, A.; Loetscher, T.; Gallomarino, N.C.; Szpak, A.; Lee, G.; Michalski, S.C. Immersive Virtual Reality Is More Effective than Non-immersive Devices for Developing Real-world Skills in People with Intellectual Disability. Journal of Intellectual Disability Research 2024, 68, 1358–1373. [CrossRef]
- Hao, J.; He, Z.; Yu, X.; Remis, A. Comparison of Immersive and Non-Immersive Virtual Reality for Upper Extremity Functional Recovery in Patients with Stroke: A Systematic Review and Network Meta-Analysis. Neurological Sciences 2023, 44, 2679–2697. [CrossRef]
- Google Cardboard Available online: https://arvr.google.com/cardboard/ (accessed on 11 December 2024).
- Di Lernia, D.; Zaccaro, A.; Herman, A.M.; Villani, V.; Finotti, G.; Costantini, M.; Ferri, F.; Tsakiris, M.; Riva, G. Sonoception: Synthetic Auditory Stimulation of the Insula Alters Proxies of Interoceptive Processing at Behavioral and Cortical Levels. 2023.
- Di Lernia, D.; Lacerenza, M.; Ainley, V.; Riva, G. Altered Interoceptive Perception and the Effects of Interoceptive Analgesia in Musculoskeletal, Primary, and Neuropathic Chronic Pain Conditions. J Pers Med 2020, 10, 201. [CrossRef]
- Björnsdotter, M.; Morrison, I.; Olausson, H. Feeling Good: On the Role of C Fiber Mediated Touch in Interoception. Exp Brain Res 2010, 207, 149–155. [CrossRef]
- Iodice, P.; Porciello, G.; Bufalari, I.; Barca, L.; Pezzulo, G. An Interoceptive Illusion of Effort Induced by False Heart-Rate Feedback. Proceedings of the National Academy of Sciences 2019, 116, 13897–13902. [CrossRef]
- Meta Platforms Available online: https://www.meta.com/ (accessed on 10 December 2024).
- PICO Interactive Available online: https://www.picoxr.com/global (accessed on 10 December 2024).
- Varjo Technologies Oy Available online: https://varjo.com/ (accessed on 10 December 2024).
- HTC Corporation Available online: https://www.vive.com/eu/ (accessed on 10 December 2024).
- Brown, L.; DiCenso-Fleming, T.; Ensign, T.; Boyd, A.J.; Monaghan, G.; Binder, D.S. Chronic Pain Education Delivered with a Virtual Reality Headset in Outpatient Physical Therapy Clinics: A Multi-Site Exploratory Trial. Am J Transl Res 2023, 15, 3500–3510.
- Liikkanen, S.; Mäkinen, M.; Huttunen, T.; Sarapohja, T.; Stenfors, C.; Eccleston, C. Body Movement as a Biomarker for Use in Chronic Pain Rehabilitation: An Embedded Analysis of an RCT of a Virtual Reality Solution for Adults with Chronic Pain. Frontiers in Pain Research 2022, 3. [CrossRef]
- Eccleston, C.; Fisher, E.; Liikkanen, S.; Sarapohja, T.; Stenfors, C.; Jääskeläinen, S.K.; Rice, A.S.C.; Mattila, L.; Blom, T.; Bratty, J.R. A Prospective, Double-Blind, Pilot, Randomized, Controlled Trial of an “Embodied” Virtual Reality Intervention for Adults with Low Back Pain. Pain 2022, 163, 1700–1715. [CrossRef]
- Groenveld, T.D.; Smits, M.L.M.; Knoop, J.; Kallewaard, J.W.; Staal, J.B.; de Vries, M.; van Goor, H. Effect of a Behavioral Therapy-Based Virtual Reality Application on Quality of Life in Chronic Low Back Pain. Clin J Pain 2023, 39, 278–285. [CrossRef]
- Sarig Bahat, H.; Croft, K.; Carter, C.; Hoddinott, A.; Sprecher, E.; Treleaven, J. Remote Kinematic Training for Patients with Chronic Neck Pain: A Randomised Controlled Trial. European Spine Journal 2018, 27, 1309–1323. [CrossRef]
- Cetin, H.; Kose, N.; Oge, H.K. Virtual Reality and Motor Control Exercises to Treat Chronic Neck Pain: A Randomized Controlled Trial. Musculoskelet Sci Pract 2022, 62, 102636. [CrossRef]
- Sarkar, T.D.; Edwards, R.R.; Baker, N. The Feasibility and Effectiveness of Virtual Reality Meditation on Reducing Chronic Pain for Older Adults with Knee Osteoarthritis. Pain Practice 2022, 22, 631–641. [CrossRef]
- Fowler, C.A.; Ballistrea, L.M.; Mazzone, K.E.; Martin, A.M.; Kaplan, H.; Kip, K.E.; Ralston, K.; Murphy, J.L.; Winkler, S.L. Virtual Reality as a Therapy Adjunct for Fear of Movement in Veterans With Chronic Pain: Single-Arm Feasibility Study. JMIR Form Res 2019, 3, e11266. [CrossRef]
- Garrett, B.; Taverner, T.; McDade, P. Virtual Reality as an Adjunct Home Therapy in Chronic Pain Management: An Exploratory Study. JMIR Med Inform 2017, 5, e11. [CrossRef]
- Brown, P.; Powell, W.; Dansey, N.; Al-Abbadey, M.; Stevens, B.; Powell, V. Virtual Reality as a Pain Distraction Modality for Experimentally Induced Pain in a Chronic Pain Population: An Exploratory Study. Cyberpsychol Behav Soc Netw 2022, 25, 66–71. [CrossRef]
- Matthie, N.; Higgins, M.; Doorenbos, A.; Maddox, T.; Jenerette, C. Feasibility of In-Home Virtual Reality for Chronic Pain in Sickle Cell Disease. Pain Management Nursing 2024, 25, 425–431. [CrossRef]
- Safy, O.; Rousseaux, F.; Faymonville, M.-E.; Libbrecht, D.; Fontaine, R.; Raaf, M.; Staquet, C.; Tasset, H.; Bonhomme, V.; Vanhaudenhuyse, A.; et al. Virtual Reality Hypnosis Prior to Radiofrequency Thermocoagulation for Patients with Chronic Pain: An Exploratory Clinical Trial. Front Psychol 2024, 15. [CrossRef]
- Saby, A.; Alvarez, A.; Smolins, D.; Petros, J.; Nguyen, L.; Trujillo, M.; Aygün, O. Effects of Embodiment in Virtual Reality for Treatment of Chronic Pain: Pilot Open-Label Study. JMIR Form Res 2024, 8, e34162. [CrossRef]
- Mazurek, J.; Cieślik, B.; Wrzeciono, A.; Gajda, R.; Szczepańska-Gieracha, J. Immersive Virtual Reality Therapy Is Supportive for Orthopedic Rehabilitation among the Elderly: A Randomized Controlled Trial. J Clin Med 2023, 12, 7681. [CrossRef]
- Yalfani, A.; Abedi, M.; Raeisi, Z. Effects of an 8-Week Virtual Reality Training Program on Pain, Fall Risk, and Quality of Life in Elderly Women with Chronic Low Back Pain: Double-Blind Randomized Clinical Trial. Games Health J 2022, 11, 85–92. [CrossRef]
- Harvie, D.S.; Smith, R.T.; Moseley, G.L.; Meulders, A.; Michiels, B.; Sterling, M. Illusion-Enhanced Virtual Reality Exercise for Neck Pain. Clin J Pain 2020, 36, 101–109. [CrossRef]
- Fuchs, L.; Kluska, A.; Novak, D.; Kosashvili, Y. The Influence of Early Virtual Reality Intervention on Pain, Anxiety, and Function Following Primary Total Knee Arthroplasty. Complement Ther Clin Pract 2022, 49, 101687. [CrossRef]
- Sarig Bahat, H.; Takasaki, H.; Chen, X.; Bet-Or, Y.; Treleaven, J. Cervical Kinematic Training with and without Interactive VR Training for Chronic Neck Pain – a Randomized Clinical Trial. Man Ther 2015, 20, 68–78. [CrossRef]
- Yan, Y.; Chen, K.; Xie, Y.; Song, Y.; Liu, Y. The Effects of Weight on Comfort of Virtual Reality Devices. In; 2019; pp. 239–248.
- Primax Innovation Inc. Available online: https://pimax.com/ (accessed on 10 December 2024).
- BHaptics Inc Available online: https://www.bhaptics.com/tactsuit/ (accessed on 10 December 2024).
- HTC Corporation VIVE Full Face Tracker Available online: https://www.vive.com/us/accessory/vive-full-face-tracker/ (accessed on 10 December 2024).
- MANUS Technology Group Metagloves Pro Available online: https://www.manus-meta.com/products/metagloves-pro (accessed on 10 December 2024).
- HaptX Inc HaptX Gloves G1 Available online: https://haptx.com/gloves-g1/ (accessed on 10 December 2024).
- Mechatech Ltd. AGILEVR Available online: https://www.mechatech.co.uk/agilevr (accessed on 10 December 2024).
- HTC Corporation VIVE Ultimate Tracker Available online: https://www.vive.com/eu/accessory/vive-ultimate-tracker/ (accessed on 10 December 2024).
- PICO Interactive PICO Motion Tracker.
- Sony Electronics Inc Mobile Motion Capture for VR and 3D Contents Creation Available online: https://electronics.sony.com/more/mocopi/all-mocopi/p/qmss1-uscx?srsltid=AfmBOoqRW7frPogXXWVl-ZFNG4s-oiSLNs8c7YI8OewzdIzged0TrYjq (accessed on 10 December 2024).
- Knoxlabs FirstVR - Muscle Displacement Controller Available online: https://www.knoxlabs.com/products/firstvr-muscle-input-controller?srsltid=AfmBOopW335YC1EWb7D64W5_1QP2cxOmKmbzohjPIbVdnLarES042P4x (accessed on 10 December 2024).
- TESLASUIT TESLASUIT Dev Kit Available online: https://teslasuit.io/products/teslasuit-4/ (accessed on 10 December 2024).
- HTC Corporation VIVE Tracker 3.0 Available online: https://www.vive.com/us/accessory/tracker3/ (accessed on 10 December 2024).
- Orbbec Inc Femto Bolt Available online: https://www.orbbec.com/products/tof-camera/femto-bolt/ (accessed on 10 December 2024).
- Meta Meta Quest 3S Breathable Facial Interface Available online: https://www.meta.com/quest/accessories/quest-3s-breathable-facial-interface/?srsltid=AfmBOooPYEOcHGd0rxIzWlN8W1t3ISU_o25t4WT32pXS8lMFO3zG20-d (accessed on 10 December 2024).
- VR TierOne UV-C Disinfection Cabinet for VR TierOne GO Headsets Available online: https://vrtierone.com/products/uv-c-disinfection-cabinet-for-vr-tierone-go-headsets/ (accessed on 10 December 2024).
- Cyberith GmbH Virtualizer ELITE 2 Available online: https://www.cyberith.com/virtualizer-elite/ (accessed on 10 December 2024).
- HTC Vive The VIVE Ultimate Tracker Is Now Third-Party Compatible! Available online: https://www.youtube.com/watch?v=3GXKXCTgNzI (accessed on 10 December 2024).
- Dy, M.; Olazo, K.; Lyles, C.R.; Lisker, S.; Weinberg, J.; Lee, C.; Tarver, M.E.; Saha, A.; Kontson, K.; Araojo, R.; et al. Usability and Acceptability of Virtual Reality for Chronic Pain Management among Diverse Patients in a Safety-Net Setting: A Qualitative Analysis. JAMIA Open 2023, 6. [CrossRef]
- Garcia, L.M.; Birckhead, B.J.; Krishnamurthy, P.; Sackman, J.; Mackey, I.G.; Louis, R.G.; Salmasi, V.; Maddox, T.; Darnall, B.D. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J Med Internet Res 2021, 23, e26292. [CrossRef]
- Jones, T.; Moore, T.; Choo, J. The Impact of Virtual Reality on Chronic Pain. PLoS One 2016, 11, e0167523. [CrossRef]
- Stamm, O.; Dahms, R.; Reithinger, N.; Ruß, A.; Müller-Werdan, U. Virtual Reality Exergame for Supplementing Multimodal Pain Therapy in Older Adults with Chronic Back Pain: A Randomized Controlled Pilot Study. Virtual Real 2022, 26, 1291–1305. [CrossRef]
- Krepkovich, E.; Kaur, M.; Mangum, L.C.; Saliba, S.; Lichter, M.; Olowin, A.; Richardson, N.; Hart, J. Feasibility of a Novel Video Game-Based Electromyography Biofeedback System in Patients With Knee Osteoarthritis. J Sport Rehabil 2022, 31, 937–942. [CrossRef]
- Kragting, M.; Voogt, L.; Coppieters, M.W.; Pool-Goudzwaard, A.L. Visual Feedback Manipulation in Virtual Reality to Influence Pain-Free Range of Motion. Are People with Non-Specific Neck Pain Who Are Fearful of Movement More Susceptible? PLoS One 2023, 18, e0287907. [CrossRef]
- Stanton, T.R.; Gilpin, H.R.; Edwards, L.; Moseley, G.L.; Newport, R. Illusory Resizing of the Painful Knee Is Analgesic in Symptomatic Knee Osteoarthritis. PeerJ 2018, 6, e5206. [CrossRef]
- Lewis, J.S.; Newport, R.; Taylor, G.; Smith, M.; McCabe, C.S. Visual Illusions Modulate Body Perception Disturbance and Pain in Complex Regional Pain Syndrome: A Randomized Trial. European Journal of Pain 2021, 25, 1551–1563. [CrossRef]
- MIRAGE Lab About MIRAGE Available online: https://miragemultisensoryillusions.wordpress.com/about/ (accessed on 10 December 2024).
- XR4REHAB Available online: https://vr4rehab.org/ (accessed on 12 December 2024).
- International Society for Virtual Rehabilitation Available online: https://isvr.org/ (accessed on 12 December 2024).
- The American Medical Extended Reality Association Available online: https://amxra.org/ (accessed on 12 December 2024).
- International Industry Society in Advanced Rehabilitation Technology Available online: https://iisart.org/ (accessed on 12 December 2024).
- International Virtual Reality Healthcare Association Available online: https://ivrha.org/ (accessed on 12 December 2024).
- EuroXR Association Available online: https://www.euroxr-association.org/ (accessed on 12 December 2024).
- XR Association Available online: https://xra.org/ (accessed on 12 December 2024).
- The VR/AR Association Available online: https://www.thevrara.com/ (accessed on 12 December 2024).
- VR for Health Available online: https://vrforhealth.com/ (accessed on 12 December 2024).
- Virtual Reality Society Available online: https://www.vrs.org.uk/ (accessed on 12 December 2024).
- Virtual Reality Marketing Available online: https://go.virtualrealitymarketing.com/ (accessed on 12 December 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




