Submitted:
10 December 2024
Posted:
11 December 2024
You are already at the latest version
Abstract
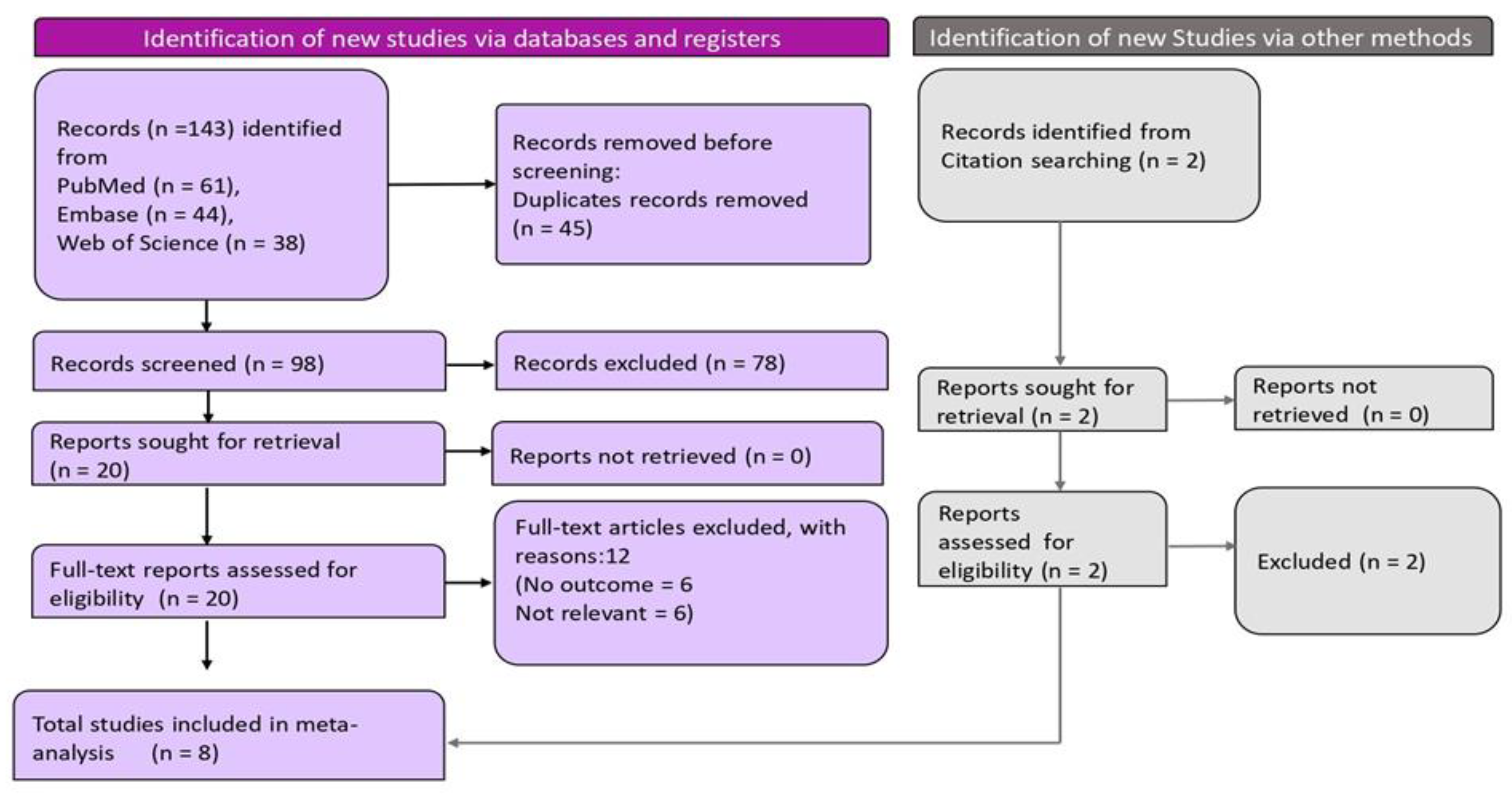
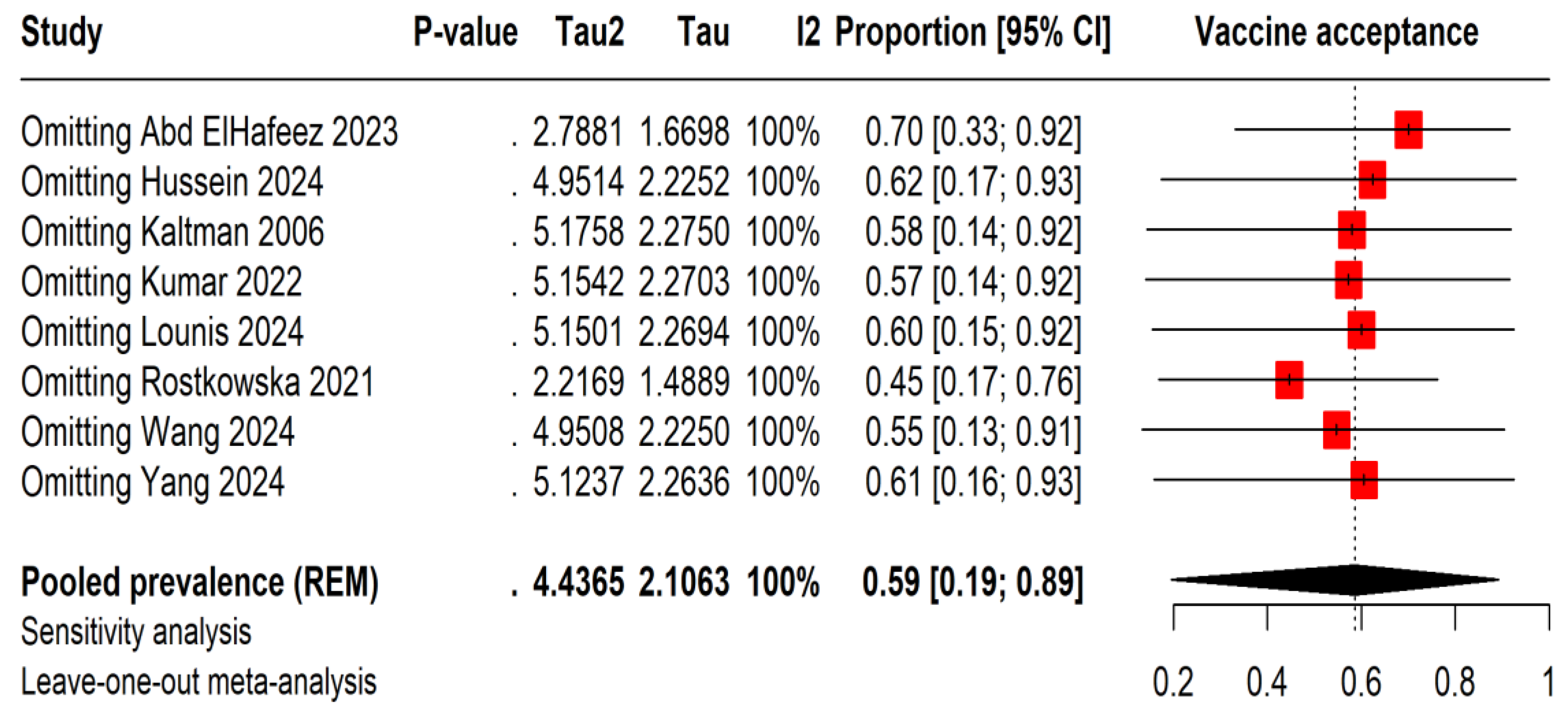
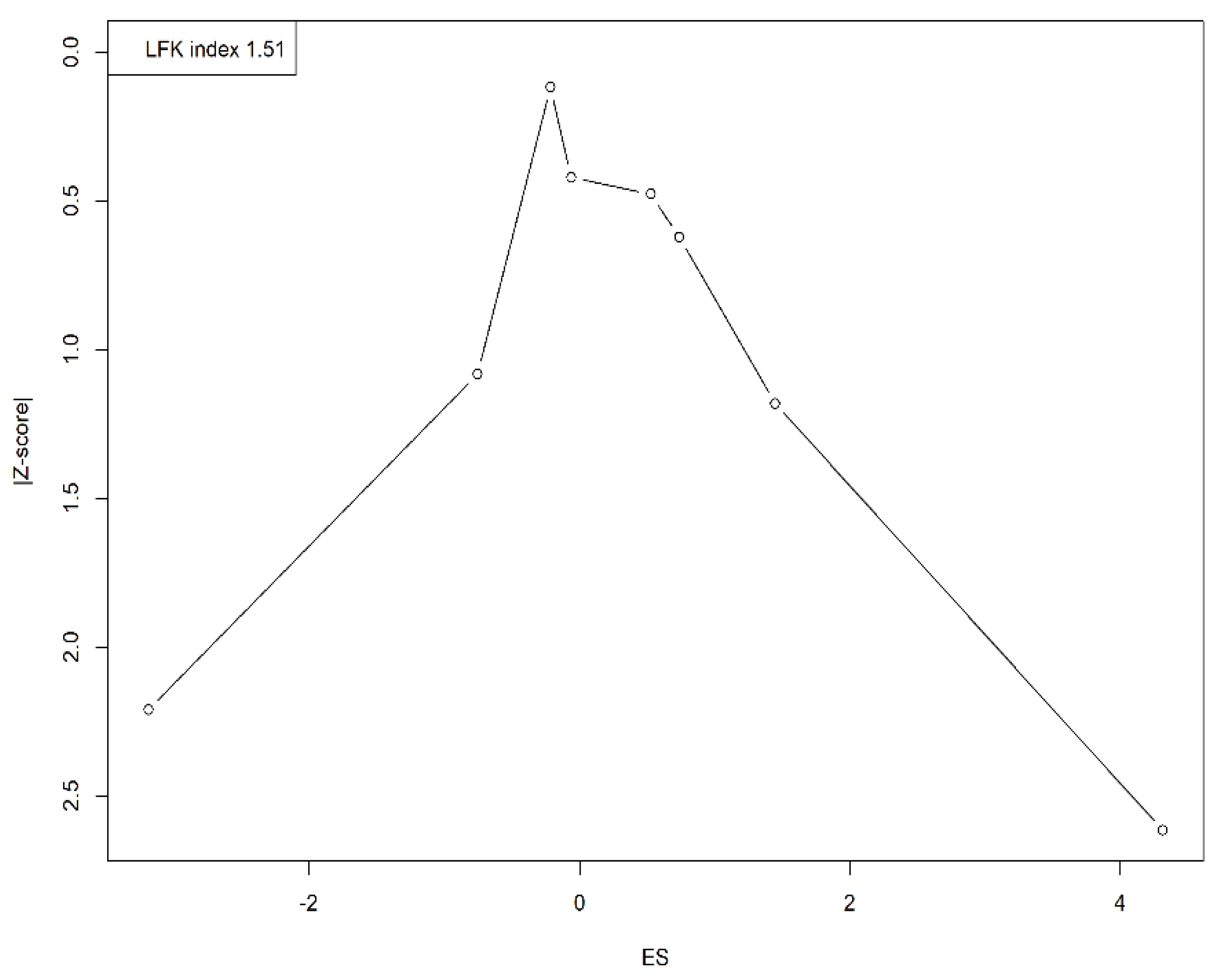
Background: Mpox, formerly known as monkeypox, is a re-emerging viral disease. Vaccine acceptance is crucial for preventing its spread. This systematic review and meta-analysis assessed the acceptance of the Mpox vaccine among student populations. Methods: We searched electronic databases including PubMed, Web of Science, and Embase up to September 14, 2024. The studies included were observational, such as cross-sectional and cohort studies, and specifically assessed vaccine acceptance for Mpox vaccines among students. R version 4.4 was used to perform meta-analysis and sensitivity analyses were conducted to assess the robustness of the findings. Publication bias was evaluated using Doi plots. Results: Of the 143 studies initially identified, eight studies were included in the final analysis, comprising a total of 16,129 participants. The overall vaccine acceptance rate was 58.6%, with considerable variability across studies (I² = 100%). Sensitivity analyses indicated that acceptance rates ranged between 45% and 70%. The Doi plot demonstrated the presence of moderate publication bias. Conclusion: This systematic review and meta-analysis show moderate acceptance of the Mpox vaccine among students. Future studies should investigate the factors influencing vaccine acceptance and design targeted strategies to improve coverage, which will be essential for controlling Mpox and ensuring successful vaccination campaigns.
Keywords:
Introduction
Method
Eligibility Criteria
Search Strategy
Screening and Data Extraction
Quality Assessment
Statistical Analysis
Results
Summary Characteristics of Included Studies
Meta-Analysis
Sensitivity Analysis
Publication Bias
Discussion
Conclusion
Supplementary Materials
Author Contributions
Funding
Data Availability
Acknowledgments
Conflict of Interest
Consent to Participate
Ethics Approval Declaration
Human Ethics and Consent to Participate Declarations
Ethical Approval
References
- Tajudeen YA, Oladipo HJ, Muili AO, Ikebuaso JG. Monkeypox: A review of a zoonotic disease of global public health concern. Health Promotion Perspectives 2023, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- El Dine FB, Gebreal A, Samhouri D, Estifanos H, Kourampi I, Abdelrhem H, et al. Ethical considerations during Mpox Outbreak: a scoping review. BMC Medical Ethics 2024, 25, 79. [Google Scholar] [CrossRef]
- Black S, Rappuoli R. A crisis of public confidence in vaccines. American Association for the Advancement of Science 2010.
- Ellison NB, Steinfield C, Lampe C. The benefits of Facebook “friends:” Social capital and college students’ use of online social network sites. Journal of computer-mediated communication 2007, 12, 1143–1168. [Google Scholar] [CrossRef]
- Cascini F, Pantovic A, Al-Ajlouni Y, Failla G, Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine 2021, 40.
- Al-Jayyousi GF, Sherbash MAM, Ali LAM, El-Heneidy A, Alhussaini NWZ, Elhassan MEA, Nazzal MA. Factors influencing public attitudes towards COVID-19 vaccination: a scoping review informed by the socio-ecological model. Vaccines 2021, 9, 548. [Google Scholar] [CrossRef]
- Wilson RJ, Paterson P, Jarrett C, Larson HJ. Understanding factors influencing vaccination acceptance during pregnancy globally: a literature review. Vaccine 2015, 33, 6420–6429. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi OV, Johnson MS, Ebling S, Amundsen OM, Halsøy Ø, Hoffart A, et al. Risk, trust, and flawed assumptions: vaccine hesitancy during the COVID-19 pandemic. Frontiers in Public Health 2021, 9, 700213. [Google Scholar] [CrossRef]
- Jennings W, Stoker G, Bunting H, Valgarðsson VO, Gaskell J, Devine D, et al. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef] [PubMed]
- Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PloS one 2022, 17, e0265496. [Google Scholar] [CrossRef]
- Mektebi A, Elsaid M, Yadav T, Abdallh F, Assker M, Siddiq A, et al. Mpox vaccine acceptance among healthcare workers: a systematic review and meta-analysis. BMC Public Health 2024, 24, 4. [Google Scholar] [CrossRef]
- Mahameed H, Al-Mahzoum K, AlRaie LA, Aburumman R, Al-Naimat H, Alhiary S, et al. Previous vaccination history and psychological factors as significant predictors of willingness to receive mpox vaccination and a favorable attitude towards compulsory vaccination. Vaccines 2023, 11, 897. [Google Scholar] [CrossRef] [PubMed]
- Wang J, Fu L, Meng H, Wu K, Han B, Lin Y, et al. Knowledge, concerns, and vaccine acceptance related to Mpox (Monkeypox) among university students in North and Northeast China: An online cross-sectional study. Human Vaccines & Immunotherapeutics 2024, 20, 2339922. [Google Scholar] [CrossRef]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. bmj 2021, 372. [Google Scholar] [CrossRef]
- Norris JM, Simpson BS, Ball R, Freeman A, Kirkham A, Parry MA, et al. A Modified Newcastle-Ottawa Scale for Assessment of Study Quality in Genetic Urological Research. Eur Urol. 2021, 79, 325–326. [Google Scholar] [CrossRef] [PubMed]
- Chambers, JM. Software for data analysis: programming with R: Springer; 2008.
- Borenstein M, Cooper H, Hedges L, Valentine J. Heterogeneity in meta-analysis. The handbook of research synthesis and meta-analysis 2019, 3, 453–470. [Google Scholar]
- Thabane L, Mbuagbaw L, Zhang S, Samaan Z, Marcucci M, Ye C, et al. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC medical research methodology 2013, 13, 1–12. [Google Scholar] [CrossRef]
- Furuya-Kanamori L, Barendregt JJ, Doi SA. A new improved graphical and quantitative method for detecting bias in meta-analysis. JBI Evidence Implementation 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Abd ElHafeez S, Gebreal A, Khalil MA, Youssef N, Sallam M, Elshabrawy A, et al. Assessing disparities in medical students’ knowledge and attitude about monkeypox: a cross-sectional study of 27 countries across three continents. Frontiers in Public Health 2023, 11, 1192542. [Google Scholar] [CrossRef] [PubMed]
- Hussein M, Siddiq A, Ismail HM, Mansy N, Ellakwa DE-S, Nassif M, et al. Cross-Country Discrepancies in Monkeypox Vaccine Hesitancy Among Postgraduate and Undergraduate Medical Students. Disaster Medicine and Public Health Preparedness 2024, 18, e82. [Google Scholar] [CrossRef]
- Kaltman S, Tractenberg RE, Taylor K, Green BL. The smallpox vaccine: a multidimensional model of choice. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 2006, 4, 64–73. [Google Scholar] [CrossRef]
- Kumar N, Ahmed F, Raza MS, Rajpoot PL, Rehman W, Khatri SA, et al. Monkeypox cross-sectional survey of knowledge, attitudes, practices, and willingness to vaccinate among university students in Pakistan. Vaccines 2022, 11, 97. [Google Scholar] [CrossRef]
- Lounis M, Hamimes A, Dahmani A. Assessment of Monkeypox (MPOX) Knowledge and Vaccination Intention among Health and Life Sciences Students in Algeria: A Cross-Sectional Study. Infectious Disease Reports 2024, 16, 170–180. [Google Scholar] [CrossRef]
- Rostkowska OM, Peters A, Montvidas J, Magdas TM, Rensen L, Zgliczyński WS, et al. Attitudes and knowledge of European medical students and early graduates about vaccination and self-reported vaccination coverage—multinational cross-sectional survey. International Journal of Environmental Research and Public Health 2021, 18, 3595. [Google Scholar] [CrossRef] [PubMed]
- Yang X, Yang X, Jiang W, Luo N, Hu Y, Yang Y, et al. A cross-sectional investigation of factors influencing mpox vaccine hesitancy for students in Southwest China. Human Vaccines & Immunotherapeutics 2024, 20, 2309704. [Google Scholar]
- Roy DN, Azam MS, Biswas M, Islam E. Potential factors influencing COVID-19 vaccine acceptance and hesitancy among university students in Bangladesh: a cross-sectional comparative study. Epidemiology & Infection. 2023, 151, e11. [Google Scholar]
- Patwary MM, Bardhan M, Haque MZ, Sultana R, Alam MA, Browning M. COVID-19 Vaccine Acceptance Rate and Its Factors among Healthcare Students: A Systematic Review with Meta-Analysis. Vaccines (Basel) 2022, 10. [Google Scholar]
- Geng H, Cao K, Zhang J, Wu K, Wang G, Liu C. Attitudes of COVID-19 vaccination among college students: A systematic review and meta-analysis of willingness, associated determinants, and reasons for hesitancy. Human Vaccines & Immunotherapeutics 2022, 18, 2054260. [Google Scholar] [CrossRef]
- Kelekar AK, Lucia VC, Afonso NM, Mascarenhas AK. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J Am Dent Assoc. 2021, 152, 596–603. [Google Scholar] [CrossRef]
- Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical medicine and health. 2021, 49, 37. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman SK, Musa MS, Tsiga-Ahmed FIi, Sulaiman AK, Bako AT. A systematic review and meta-analysis of the global prevalence and determinants of COVID-19 vaccine acceptance and uptake in people living with HIV. Nature Human Behaviour. 2024, 8, 100–114. [Google Scholar] [CrossRef]
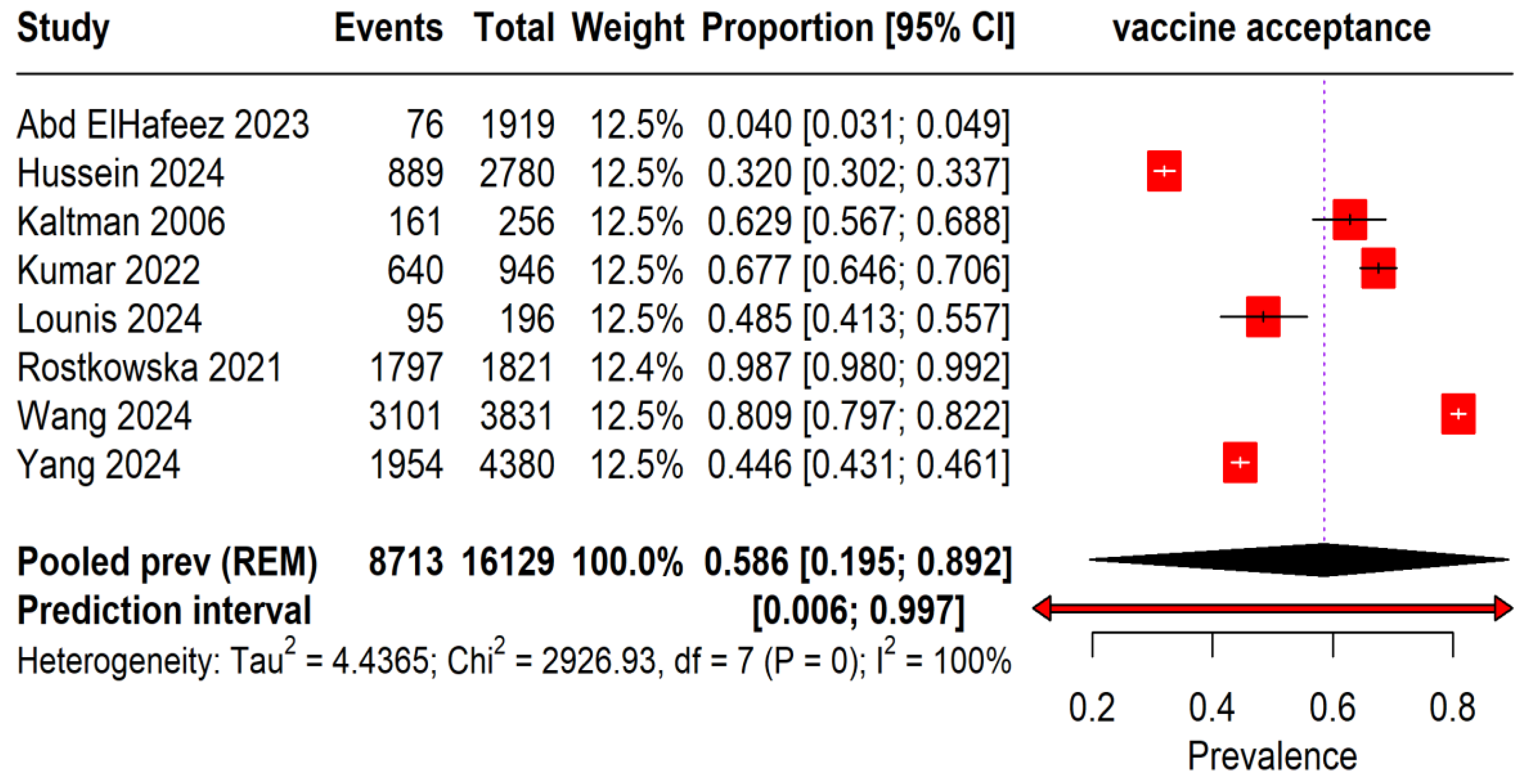
| Author | Country | Study design | Male (n) | Age (mean Years) | Total samples size | Key findings |
|---|---|---|---|---|---|---|
| Abd elhafeez et al. 2023 [20] | Saudi arabia | Cross-sectional study | 882 | 21 | 1919 | Differences in Mpox knowledge among medical students across income levels suggest adding its epidemiology to curricula could enhance disease control. |
| Hussein et al. 2024 [21] | Egypt | Cross-sectional study | 1445 | 22(median) | 2780 | The complex psychological factors affecting vaccination decisions, emphasizing how socio-demographic characteristics, geographic location, awareness, and past experiences shape individual attitudes and societal responsibility towards vaccination. |
| Kaltman 2006 et al. [22] | USA | Cross-sectional study | 0 | 18-32 | 256 | The decision to receive the smallpox vaccine involves a complex set of influences including psychological stress, overall vaccine perceptions, and perceived threats. Utilizing this multifaceted model could help develop methods to increase vaccination rates by addressing the specific causes of vaccine reluctance, thus enhancing public health preparedness. |
| Kumar 2022 et al. [23] | Pakistan | Cross-sectional study | 432 | 18-22 | 946 | Mpox knowledge among university students is moderate, with considerable gaps and generally neutral attitudes. More than half are willing to get vaccinated. These findings underscore the need for improved education and public awareness to enhance Mpox prevention and inform effective vaccination strategies. |
| Lounis 2024 et al. [24] | Algeria | Cross-sectional study | 28 | <20 and > 30 | 196 | Mpox knowledge among Algerian Health and Life Sciences students is limited, yet their support for vaccination mirrors global rates, significant given the absence of reported Mpox cases in Algeria. Enhancing education and awareness is crucial to counter vaccine hesitancy often fueled by conspiracy theories. |
| Rostkowska 2021 et al. [25] | Germany | Cross-sectional study | 555 | 23 | 1821 | European medical students and junior doctors widely acknowledge vaccine safety and efficacy, with minimal skepticism. Females often guide peers on vaccinations. As their education progresses, they increasingly support mandatory healthcare worker vaccinations. However, despite understanding flu vaccine importance, nearly half remain unvaccinated, indicating persistent gaps in vaccine knowledge and practice that necessitate improved education and training. |
| Wang 2024 et al. [13] | China | Cross-sectional study | 1265 | < 20 ≥20 | 3831 | University students display gaps in Mpox knowledge but are positive about vaccination. Recommendations focus on enhancing education through social media and using both international and local vaccines to prevent outbreaks. The study calls for urgent research and targeted actions to increase Mpox awareness and vaccination rates nationwide. |
| Yang 2024 et al. [26] | China | Cross-sectional study | 3712 | 16 > 26 | 4380 | Research reveals that university students in Southwest China are willing to receive the mpox vaccine, influenced by factors such as sexual orientation, STD history, and awareness. To boost vaccine uptake and prevent transmission, enhancing mpox education and promoting vaccine awareness on campuses, especially among MSM students, is recommended. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





