Submitted:
06 December 2024
Posted:
09 December 2024
You are already at the latest version
Abstract
Background: Diabetes affects over 460 million people worldwide and poses a growing public health challenge, driven largely by dietary and lifestyle factors. While type 2 diabetes (T2D) is more prevalent, type 1 diabetes (T1D) presents unique therapeutic challenges, particularly in younger individuals. Advances in diabetes management, such as continuous glucose monitoring (CGM), insulin pumps (IP), and, more recently, smart multiple dose injection (MDI) pens, have significantly enhanced glycemic control and improved patients' quality of life. Aim: This study aims to evaluate the baseline characteristics of patients switching from MDI therapy to the Medtronic Smart MDI system [composed by a smart insulin pen (InPenTM) and a connected CGM Medtronic SimpleraTM sensor] and to assess its impact on glycemic outcomes over different time periods (14, 30, and 90 days). Methods: A retrospective observational study was conducted among adults with T1D who initiated Medtronic Smart MDI therapy. Participants were enrolled voluntarily at the Diabetes and Nutrition Clinic in Ast Fermo, Marche Region, Italy. Glycemic parameters were monitored using CGM data and analyzed with descriptive statistics, including mean, standard deviation (SD), and interquartile range (IQR). Comparisons across time periods were performed using the Wilcoxon signed-rank test, with statistical significance set at p < 0.05. Results: This study involved 21 subjects with a mean age of 51.5 years, a mean BMI of 24.7, and a T1D duration of 21.9 years. After switching from MDI to Medtronic Smart MDI, significant improvements were noted: mean sensor glucose (SG) decreased from 171.0 to 153.5 mg/dL (p = 0.035), Time in Range (TIR) increased from 58.0% to 64.4% (p = 0.005), and a mean Time Above Range (TAR) (>180mg/dL) decreased from 39.0% to 34.2% (p = 0.015). No significant differences were found in Time Below Range (TBR). Conclusion: Transitioning to Medtronic Smart MDI in T1D patients significantly improves glycemic control, notably by reducing average glucose levels and increasing TIR. This integrated approach enhances overall disease management, reducing hyperglycemia while maintaining stable hypoglycemia risk. Further studies are needed to optimize its use in daily practice and long-term care.
Keywords:
1. Background
1.1. Aim
1.1.1. Primary Objective
1.1.2. Secondary Objectives
2. Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. Sample and Criteria
2.4. Endpoints
2.5. Statistical Analysis
2.5.1. General Methodology
2.5.2. Data Analysis
2.5.3. Derived Variables
2.5.4. Handling of Missing Data and Outliers and Validation Requirements
3. Results
3.1. Baseline Characteristics
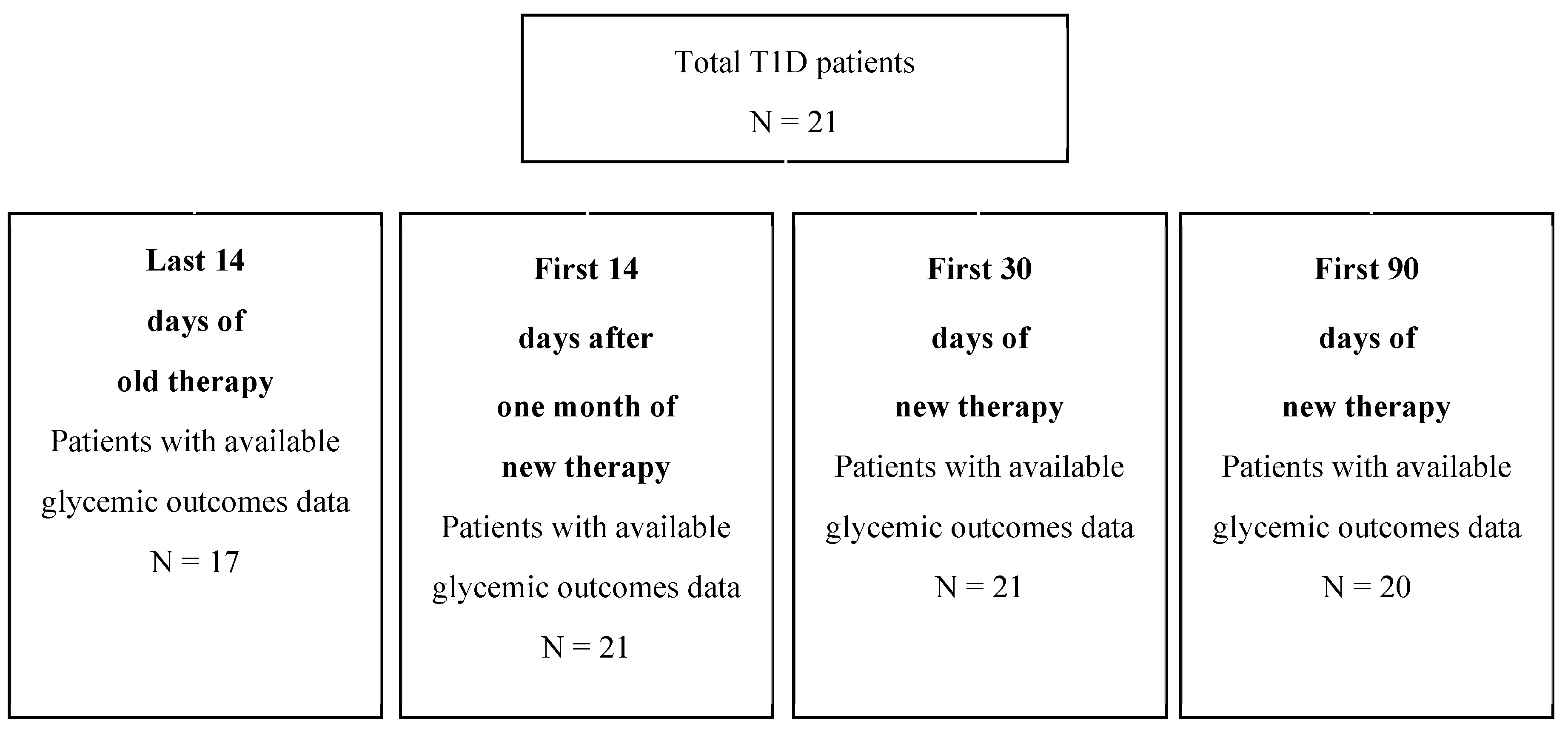
3.2. Time Study
3.3. Sensor Use
3.4. Glycemic Outcomes with Medtronic Smart MDI
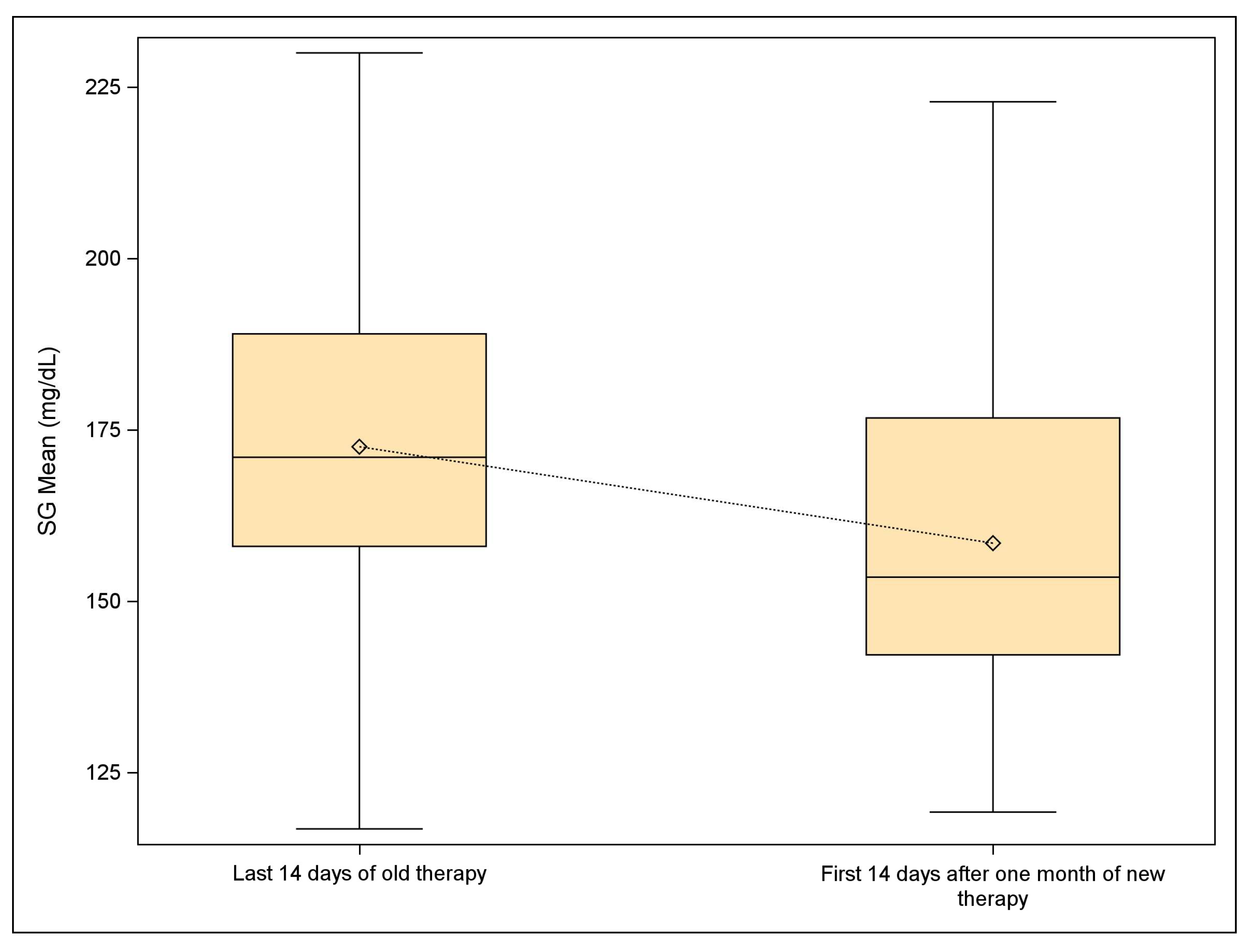
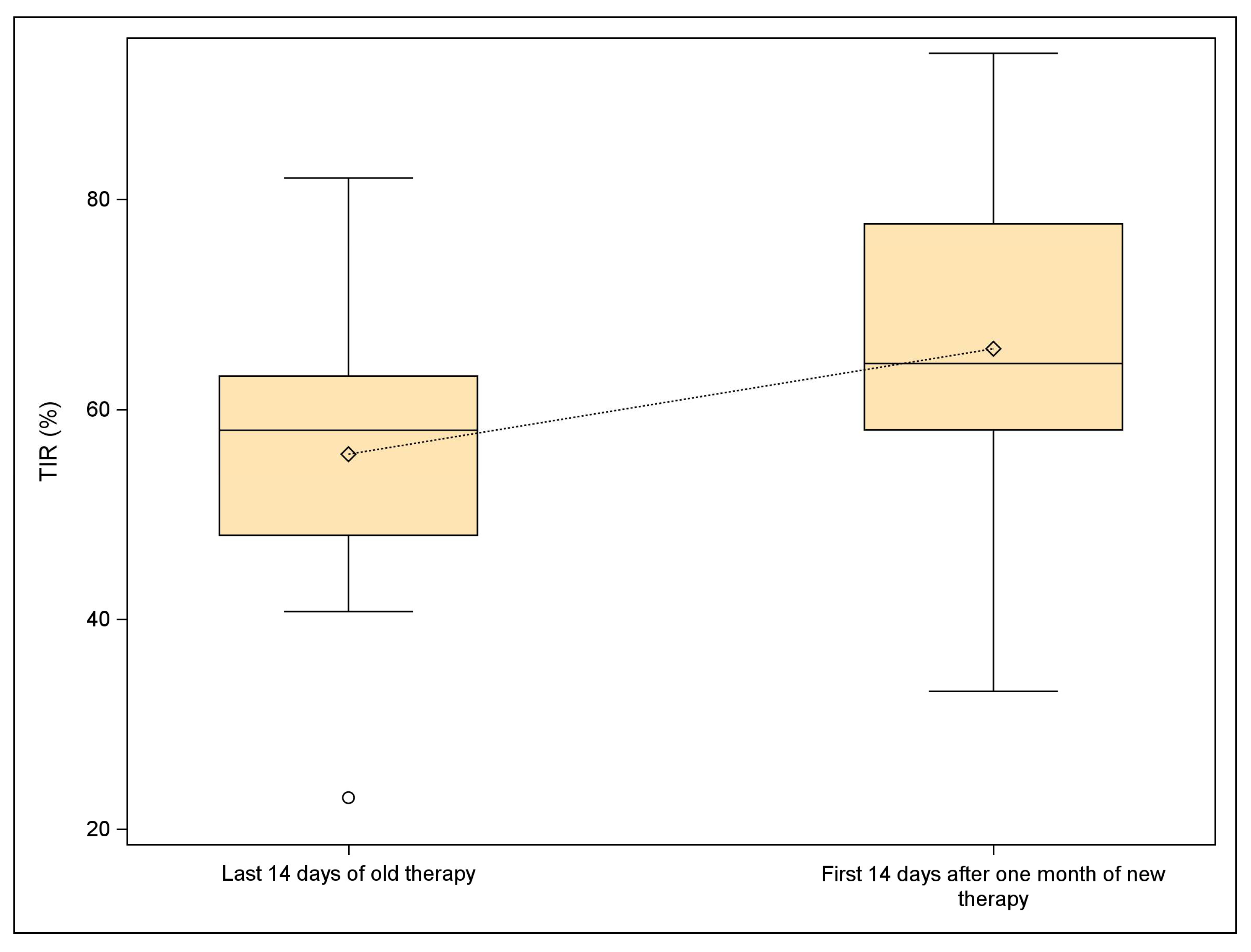
3.5. Comparison Between Standard MDI and Medtronic Smart MDI
3.6. Boxplot Analysis
4. Discussion
Limitations
5. Conclusion
Supplementary Materials
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmad, E.; Lim, S.; Lamptey, R.; Webb, D.R.; Davies, M.J. Type 2 diabetes. Lancet 2022, 400, 1803–1820. [Google Scholar] [CrossRef] [PubMed]
- Magliano, D.J.; Boyko, E.J. Committee IDFDAtes. IDF diabetes atlas. In Idf Diabetes Atlas; International Diabetes Feeration ©: Brussels, Belgium, 2021. [Google Scholar]
- Wong, N.D.; Sattar, N. Cardiovascular risk in diabetes mellitus: Epidemiology, assessment and prevention. Nat. Rev. Cardiol. 2023, 20, 685–695. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Diabetes. Available on: https://www.who.int/news-room/fact-sheets/detail/diabetes (access November 25, 2024).
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2021. Results. Institute for Health Metrics and Evaluation. Available on: https://vizhub.healthdata.org/gbd-results/ (access on November 1, 2024).
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet, 2: 15;402(10397), 1039. [CrossRef]
- GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet, 18 May 1044. [CrossRef]
- Jacobsen LM, Sherr JL, Considine E, Chen A, Peeling SM, Hulsmans M, Charleer S, Urazbayeva M, Tosur M, Alamarie S, Redondo MJ, Hood KK, Gottlieb PA, Gillard P, Wong JJ, Hirsch IB, Pratley RE, Laffel LM, Mathieu C; ADA/EASD PMDI. Utility and precision evidence of technology in the treatment of type 1 diabetes: a systematic review. Commun Med, 1: 2023 Oct 5;3(1), 2023. [CrossRef]
- Mallik R, Kar P, Mulder H, Krook A. The future is here: an overview of technology in diabetes. Diabetologia, 2019. [CrossRef]
- Handelsman Y, Hellman R, Lajara R, Roberts VL, Rodbard D, Stec C, Unger J. American Association of Clinical Endocrinology Clinical Practice Guideline: The Use of Advanced Technology in the Management of Persons With Diabetes Mellitus. Endocr Pract. [CrossRef]
- American Diabetes Association Professional Practice Committee. 7. Diabetes Technology: Standards of Care in Diabetes-2024. Diabetes Care, S: 1;47(Suppl 1). [CrossRef]
- Jayedi, A.; Zargar, M.S.; Emadi, A.; Aune, D. Walking speed and the risk of type 2 diabetes: a systematic review and meta-analysis. Br J Sports Med, 3: 13;58(6). [CrossRef]
- Cao, L.; An, Y.; Liu, H.; Jiang, J.; Liu, W.; Zhou, Y.; et al. Global epidemiology of type 2 diabetes in patients with NAFLD or MAFLD: a systematic review and meta-analysis. BMC Med, 1: 6;22(1). [CrossRef]
- Gregory, G.A.; Robinson, T.I.G.; Linklater, S.E.; Wang, F.; Colagiuri, S.; de Beaufort, C.; Donaghue, K.C. ; International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group; Magliano, D.J.; Maniam, J.; Orchard, T.J.; Rai, P.; Ogle, G.D. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. [CrossRef]
- Anandhakrishnan, A.; Hussain, S. Automating insulin delivery through pump and continuous glucose monitoring connectivity: Maximizing opportunities to improve outcomes. Diabetes Obes Metab. [CrossRef]
- Farhat, I.; Drishti, S.; Bochner, R.; Bargman, R. Do hybrid closed loop insulin pump systems improve glycemic control and reduce hospitalizations in poorly controlled type 1 diabetes? J Pediatr Endocrinol Metab. 2024 Nov 5. [CrossRef]
- Petrelli, F.; Cangelosi, G.; Scuri, S.; Pantanetti, P.; Lavorgna, F.; Faldetta, F.; et al. Diabetes and technology: A pilot study on the management of patients with insulin pumps during the COVID-19 pandemic. Diabetes Res Clin Pract, 1084. [Google Scholar] [CrossRef]
- Petrovski, G.; Al Khalaf, F.; Campbell, J.; Umer, F.; Almajaly, D.; Hamdan, M.; Hussain, K. One-year experience of hybrid closed-loop system in children and adolescents with type 1 diabetes previously treated with multiple daily injections: drivers to successful outcomes. Acta Diabetol. [CrossRef]
- McAuley, S.A.; Lee, M.H.; Paldus, B.; Vogrin, S.; de Bock, M.I.; Abraham, M.B.; et al. ; Australian JDRF Closed-Loop Research Group. Six Months of Hybrid Closed-Loop Versus Manual Insulin Delivery With Fingerprick Blood Glucose Monitoring in Adults With Type 1 Diabetes: A Randomized, Controlled Trial. Diabetes Care, 3024. [Google Scholar] [CrossRef]
- Cobry, E.C.; Kanapka, L.G.; Cengiz, E.; Carria, L.; Ekhlaspour, L.; Buckingham, B.A.; et al. ; iDCL Trial Research Group. Health-Related Quality of Life and Treatment Satisfaction in Parents and Children with Type 1 Diabetes Using Closed-Loop Control. Diabetes Technol Ther. [CrossRef]
- Benioudakis, E.; Karlafti, E.; Kalaitzaki, A.; Kaiafa, G.; Savopoulos, C.; Didangelos, T. Technological Developments and Quality of Life in Type 1 Diabetes Mellitus Patients: A Review of the Modern Insulin Analogues, Continuous Glucose Monitoring and Insulin Pump Therapy. Curr Diabetes Rev, 0311. [Google Scholar] [CrossRef]
- National Health Service (NHS) Digital. National Diabetes Audit 2021-22, type 1 Diabetes – overview. Available on: https://digital. nhs.uk/data-and-information/publications/statistical/national-diabetes-audit-type-1-diabetes/nda-type-1-2021-22-overview (accessed November 24, 2024).
- Foster, N.C.; Beck, R.W.; Miller, K.M.; Clements, M.A.; Rickels, M.R.; DiMeglio, L.A.; et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther, 6: 21(2). [CrossRef]
- Tejera-Pérez, C.; Chico, A.; Azriel-Mira, S.; Lardiés-Sánchez, B.; Gomez-Peralta, F. ; Área de Diabetes-SEEN. Connected Insulin Pens and Caps: An Expert's Recommendation from the Area of Diabetes of the Spanish Endocrinology and Nutrition Society (SEEN). Diabetes Ther, 1077. [Google Scholar] [CrossRef]
- Nimri, R.; Nir, J.; Phillip, M. Insulin Pump Therapy. Am J Ther. [CrossRef]
- Cernea, S.; Raz, I. Insulin Therapy: Future Perspectives. Am J Ther. [CrossRef]
- Nevo-Shenker, M.; Phillip, M.; Nimri, R.; Shalitin, S. Type 1 diabetes mellitus management in young children: implementation of current technologies. Pediatr Res. 2020 Mar;87(4):624-629. [CrossRef]
- Schoelwer, M.J.; DeBoer, M.D.; Breton, M.D. Use of diabetes technology in children. Diabetologia, 2075. [Google Scholar] [CrossRef]
- Ng, S.M.; Wright, N.P.; Yardley, D.; Campbell, F.; Randell, T.; Trevelyan, N.; et al. Long-term assessment of the NHS hybrid closed-loop real-world study on glycaemic outcomes, time-in-range, and quality of life in children and young people with type 1 diabetes. BMC Med, 1: 24;22(1). [CrossRef]
- Lingen, K.; Pikounis, T.; Bellini, N.; Isaacs, D. Advantages and disadvantages of connected insulin pens in diabetes management. Endocr Connect. e: 27;12(11), 2301. [Google Scholar] [CrossRef]
- Gildon, B.W. InPen Smart Insulin Pen System: Product Review and User Experience. Diabetes Spectr. [CrossRef]
- Yoo, J.H.; Kim, J.H. Advances in Continuous Glucose Monitoring and Integrated Devices for Management of Diabetes with Insulin-Based Therapy: Improvement in Glycemic Control. Diabetes Metab J. [CrossRef]
- Ospelt, E.; Noor, N.; Sanchez, J.; Nelson, G.; Rioles, N.; Malik, F.S.; et al. Facilitators and Barriers to Smart Insulin Pen Use: A Mixed-Method Study of Multidisciplinary Stakeholders From Diabetes Teams in the United States. Clin Diabetes. [CrossRef]
- Jendle, J.; Ericsson, Å.; Gundgaard, J.; Møller, J.B.; Valentine, W.J.; Hunt, B. Smart Insulin Pens are Associated with Improved Clinical Outcomes at Lower Cost Versus Standard-of-Care Treatment of Type 1 Diabetes in Sweden: A Cost-Effectiveness Analysis. Diabetes Ther. 2021 Jan;12(1):373-388. [CrossRef]
- Jendle, J.; Pöhlmann, J.; de Portu, S.; Smith-Palmer, J.; Roze, S. Cost-Effectiveness Analysis of the MiniMed 670G Hybrid Closed-Loop System Versus Continuous Subcutaneous Insulin Infusion for Treatment of Type 1 Diabetes. Diabetes Technol Ther. [CrossRef]
- Strengthening the reporting of observational studies in epidemiology, Strobe. Available on: https://www.strobe-statement.org/ (access November 29, 2024).
- Skrivankova, V.W.; Richmond, R.C.; Woolf, B.A.R.; Yarmolinsky, J.; Davies, N.M.; Swanson, S.A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA, 1: 26;326(16), 1614. [Google Scholar] [CrossRef]
- Medtronic. Care link report. Available on: https://www.medtronicdiabetes.com/customer-support/carelink-software-support/carelink-reports (access November 30, 2024).
- Vigersky, R.A.; McMahon, C. The Relationship of Hemoglobin A1C to Time-in-Range in Patients with Diabetes. Diabetes Technol Ther. [CrossRef]
- Puhr, S.; Calhoun, P.; Welsh, J.B.; Walker, T.C. The Effect of Reduced Self-Monitored Blood Glucose Testing After Adoption of Continuous Glucose Monitoring on Hemoglobin A1c and Time in Range. Diabetes Technol Ther. [CrossRef]
- Alazmi, A.A.; Brema, I.; Alzahrani, S.H.; Almehthel, M.S. The Relationship Between Hemoglobin A1c, Time in Range, and Glycemic Management Indicator in Patients With Type 1 and Type 2 Diabetes in a Tertiary Care Hospital in Saudi Arabia. Cureus, e: 6;16(7), 6394. [Google Scholar] [CrossRef]
- Hellman, J.; Hartvig, N.V.; Kaas, A.; Møller, J.B.; Sørensen, M.R.; Jendle, J. Associations of bolus insulin injection frequency and smart pen engagement with glycaemic control in people living with type 1 diabetes. Diabetes Obes Metab. [CrossRef]
- Beck, R.W.; Bergenstal, R.M.; Riddlesworth, T.D.; Kollman, C.; Li, Z.; Brown, A.S.; Close, K.L. Validation of Time in Range as an Outcome Measure for Diabetes Clinical Trials. Diabetes Care. [CrossRef]
- Urakami, T.; Terada, H.; Tanabe, S.; Mine, Y.; Aoki, M.; Aoki, R.; et al. Clinical significance of coefficient of variation in continuous glucose monitoring for glycemic management in children and adolescents with type 1 diabetes. J Diabetes Investig, 1669. [Google Scholar] [CrossRef]
- Schiaffini, R.; Lumaca, A.; Martino, M.; Rapini, N.; Deodati, A.; Amodeo, M.E.; et al. Time In Tight Range in children and adolescents with type 1 diabetes: A cross-sectional observational single centre study evaluating efficacy of new advanced technologies. Diabetes Metab Res Rev. 2024 Jul;40(5):e3826. [CrossRef]
- Eviz, E.; Killi, N.E.; Karakus, K.E.; Can, E.; Gokce, T.; Yesiltepe Mutlu, G.; Hatun, S. Assessing the feasibility of time in tight range (TITR) targets with advanced hybrid closed loop (AHCL) use in children and adolescents: A single-centre real-world study. Diabet Med, 1533. [Google Scholar] [CrossRef]
- Bahillo-Curieses, P.; Fernández Velasco, P.; Pérez-López, P.; Vidueira Martínez, A.M.; Nieto de la Marca, M.O.; Díaz-Soto, G. Utility of time in tight range (TITR) in evaluating metabolic control in pediatric and adult patients with type 1 diabetes in treatment with advanced hybrid closed-loop systems. Endocrine. [CrossRef]
- MacLeod J, Vigersky RA. A Review of Precision Insulin Management With Smart Insulin Pens: Opening Up the Digital Door to People on Insulin Injection Therapy. J Diabetes Sci Technol. [CrossRef]
- MacLeod, J.; Im, G.H.; Smith, M.; Vigersky, R.A. Shining the Spotlight on Multiple Daily Insulin Therapy: Real-World Evidence of the InPen Smart Insulin Pen. Diabetes Technol Ther. [CrossRef]
- Danne, T.P.A.; Joubert, M.; Hartvig, N.V.; Kaas, A.; Knudsen, N.N.; Mader, J.K. Association Between Treatment Adherence and Continuous Glucose Monitoring Outcomes in People With Diabetes Using Smart Insulin Pens in a Real-World Setting. Diabetes Care, 9: 1;47(6), 1003. [Google Scholar] [CrossRef]
- Ekberg, N.R.; Hartvig, N.V.; Kaas, A.; Møller, J.B.; Adolfsson, P. Smart Pen Exposes Missed Basal Insulin Injections and Reveals the Impact on Glycemic Control in Adults With Type 1 Diabetes. J Diabetes Sci Technol. 2024 Jan;18(1):66-73. [CrossRef]
- Adolfsson, P.; Hartvig, N.V.; Kaas, A.; Møller, J.B.; Hellman, J. Increased Time in Range and Fewer Missed Bolus Injections After Introduction of a Smart Connected Insulin Pen. Diabetes Technol Ther. [CrossRef]
- Cangelosi, G.; Mancin, S.; Morales Palomares, S.; Pantanetti, P.; Quinzi, E.; Debernardi, G.; Petrelli, F. Impact of School Nurse on Managing Pediatric Type 1 Diabetes with Technological Devices Support: A Systematic Review. Diseases, 1: 1;12(8). [CrossRef]
- Galindo, R.J.; Ramos, C.; Cardona, S.; Vellanki, P.; Davis, G.M.; Oladejo, O.; et al. Efficacy of a Smart Insulin Pen Cap for the Management of Patients with Uncontrolled Type 2 Diabetes: A Randomized Cross-Over Trial. J Diabetes Sci Technol. [CrossRef]
- Cangelosi, G.; Mancin, S.; Pantanetti, P.; Nguyen, C.T.T.; Morales Palomares, S.; Biondini, F.; Sguanci, M.; Petrelli, F. Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review. Diabetology 2024, 5, 375–388. [Google Scholar] [CrossRef]
- Cranston, I.; Jamdade, V.; Liao, B.; Newson, R.S. Clinical, Economic, and Patient-Reported Benefits of Connected Insulin Pen Systems: A Systematic Literature Review. Adv Ther, 2015. [Google Scholar] [CrossRef]
- Akturk, H.K.; Bindal, A. Advances in diabetes technology within the digital diabetes ecosystem. J Manag Care Spec Pharm, S: Suppl). [CrossRef]
- Tian, T.; Aaron, R.E.; Du Nova, A.Y.; Jendle, J.H.; Kerr, D.; Cengiz, E.; et al. Diabetes Technology Meeting 2023. J Diabetes Sci Technol, 1208. [Google Scholar] [CrossRef]
| Variable | Derivation for a given period |
|---|---|
| Sensor usage (%) | [Number of CGM measurements / (Number of minutes in the period of interest / 5)] * 100 |
| SG mean, SD, and CV | Mean, SD, and CV of CGM measurements |
| TIR metrics | (Number of CGM measurements in the range of interest / Number of CGM measurements) * 100 |
| Measure | Summary Statistic |
Total (N = 21) |
|---|---|---|
| Age (years) | Available Measures (%) | 21 (100.0%) |
| Mean ± SD | 51.5 ± 16.1 | |
| Median (IQR) | 53.0 (40.0-63.0) | |
| Min-Max | 17.0 - 76.0 | |
| Female | % (n/Available Measures) | 38.1% (8/21) |
| BMI | Available Measures (%) | 20 (95.2%) |
| Mean ± SD | 24.7 ± 4.1 | |
| Median (IQR) | 24.7 (23.0-28.6) | |
| Min-Max | 14.6 - 31.1 | |
| Duration of T1D (years) | Available Measures (%) | 20 (95.2%) |
| Mean ± SD | 21.9 ± 12.2 | |
| Median (IQR) | 21.5 (14.5-28.5) | |
| Min-Max | 4.0 - 52.0 | |
| Smoke | ||
| No | % (n/Available Measures) | 55.0% (11/20) |
| Yes | % (n/Available Measures) | 25.0% (5/20) |
| Former smoker | % (n/Available Measures) | 20.0% (4/20) |
| Previous therapy | ||
| SMBG | % (n/Available Measures) | 15.0% (3/20) |
| Other CGM | % (n/Available Measures) | 65.0% (13/20) |
| MEDTRONIC GC | % (n/Available Measures) | 20.0% (4/20) |
| Patient | Previous therapy |
Last 14 days of old therapy |
First 14 days after one month of Medtronic Smart MDI |
First 30 days of Medtronic Smart MDI |
First 90 days of Medtronic Smart MDI |
|---|---|---|---|---|---|
| 1 | SMBG | 95.44 | 93.68 | 94.93 | |
| 2 | None | 89.66 | 60.72 | 80.83 | |
| 3 | Other CGM | 89.0 | 97.89 | 95.58 | 90.99 |
| 4 | SMBG | 92.81 | 96.25 | 96.98 | |
| 5 | Other CGM | 74.0 | 94.00 | 93.31 | 94.22 |
| 6 | Other CGM | 77.0 | 98.66 | 94.21 | 96.47 |
| 7 | Other CGM | 89.0 | 55.13 | 93.24 | 54.00 |
| 8 | Other CGM | 100.0 | 99.43 | 95.89 | 97.25 |
| 9 | SMBG | 97.20 | 95.88 | 96.94 | |
| 10 | MEDTRONIC GC | 92.8 | 95.98 | 94.22 | 94.59 |
| 11 | MEDTRONIC GC | 77.0 | 59.25 | 85.84 | 80.76 |
| 12 | Other CGM | 79.0 | 97.25 | 96.60 | 97.94 |
| 13 | Other CGM | 77.0 | 98.29 | 80.37 | 90.40 |
| 14 | MEDTRONIC GC | 95.2 | 95.19 | 94.46 | 95.61 |
| 15 | Other CGM | 94.0 | 99.68 | 99.63 | |
| 16 | Other CGM | 96.0 | 97.87 | 93.18 | 96.05 |
| 17 | Other CGM | 96.0 | 98.74 | 96.53 | 97.60 |
| 18 | Other CGM | 99.0 | 93.63 | 91.93 | 81.97 |
| 19 | MEDTRONIC GC | 94.5 | 84.40 | 84.86 | 86.92 |
| 20 | Other CGM | 100.0 | 72.00 | 95.50 | 88.99 |
| 21 | Other CGM | 98.0 | 99.98 | 96.40 | 98.01 |
| Measure | Summary Statistic |
First 14 days after one month of Medtronic Smart MDI (N = 21) |
First 30 days of Medtronic Smart MDI (N = 21) |
First 90 days of Medtronic Smart MDI (N = 20) |
|---|---|---|---|---|
| SG mean (mg/dL) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 157.8 ± 26.5 | 161.6 ± 27.4 | 156.6 ± 18.5 | |
| Median (IQR) | 153.5 (142.2-176.7) | 156.5 (141.5-171.1) | 158.2 (140.4-171.3) | |
| Min-Max | 119.2 - 222.9 | 123.1 - 248.3 | 123.9 - 191.3 | |
| SD (mg/dL) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 52.2 ± 13.0 | 55.6 ± 10.7 | 55.0 ± 10.0 | |
| Median (IQR) | 52.5 (45.2-59.5) | 54.7 (48.9-60.4) | 54.0 (49.0-62.0) | |
| Min-Max | 27.4 - 75.0 | 39.3 - 76.6 | 38.2 - 75.6 | |
| CV (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 33.0 ± 5.6 | 34.6 ± 5.1 | 35.2 ± 5.3 | |
| Median (IQR) | 33.6 (28.1-38.0) | 33.3 (30.4-38.7) | 35.5 (29.7-39.5) | |
| Min-Max | 22.9 - 41.3 | 27.4 - 45.3 | 27.4 - 42.6 | |
| TBR2 (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 0.5 ± 0.9 | 0.5 ± 1.1 | 0.6 ± 0.9 | |
| Median (IQR) | 0.0 (0.0-0.4) | 0.1 (0.1-0.4) | 0.1 (0.1-0.5) | |
| Min-Max | 0.0 - 3.3 | 0.0 - 4.7 | 0.0 - 3.0 | |
| TBR1 (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 2.2 ± 2.5 | 2.1 ± 2.3 | 2.4 ± 2.2 | |
| Median (IQR) | 0.8 (0.6-3.2) | 1.4 (0.5-2.9) | 1.4 (0.7-3.6) | |
| Min-Max | 0.0 - 9.5 | 0.0 - 8.6 | 0.0 - 8.0 | |
| TBR (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 2.7 ± 3.3 | 2.7 ± 3.2 | 3.0 ± 3.0 | |
| Median (IQR) | 0.8 (0.6-4.1) | 1.4 (0.6-3.4) | 1.5 (0.9-4.2) | |
| Min-Max | 0.0 - 11.7 | 0.0 - 13.3 | 0.0 - 10.8 | |
| TIR (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 66.5 ± 16.3 | 63.8 ± 16.1 | 66.3 ± 12.5 | |
| Median (IQR) | 64.4 (58.0-77.6) | 64.9 (57.8-72.5) | 64.2 (57.8-76.8) | |
| Min-Max | 33.1 - 97.9 | 18.6 - 87.3 | 43.0 - 89.5 | |
| TAR1 (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 22.9 ± 10.5 | 24.4 ± 9.0 | 23.6 ± 9.0 | |
| Median (IQR) | 26.2 (16.2-29.1) | 24.0 (17.9-30.1) | 22.1 (16.8-29.5) | |
| Min-Max | 1.5 - 42.3 | 10.6 - 43.6 | 8.9 - 44.1 | |
| TAR2 (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 7.9 ± 9.0 | 9.1 ± 10.8 | 7.2 ± 4.8 | |
| Median (IQR) | 4.2 (2.2-12.0) | 6.5 (3.3-9.9) | 6.9 (2.4-10.9) | |
| Min-Max | 0.0 - 38.6 | 0.8 - 49.9 | 1.1 - 16.8 | |
| TAR (%) | Available Measures (%) | 21 (100.0%) | 21 (100.0%) | 20 (100.0%) |
| Mean ± SD | 30.8 ± 16.9 | 33.5 ± 16.8 | 30.7 ± 13.0 | |
| Median (IQR) | 34.2 (19.8-41.3) | 33.4 (22.7-40.2) | 32.7 (20.3-40.0) | |
| Min-Max | 1.5 - 66.0 | 12.3 - 81.0 | 10.0 - 56.9 |
| Measure | Summary statistics |
Last 14 days of old therapy (N = 17) |
First 14 days after one month of new therapy (N = 17) |
p-value |
|---|---|---|---|---|
| SG mean (mg/dL) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.035 |
| Mean ± SD | 172.5 ± 25.3 | 158.5 ± 26.5 | ||
| Median (IQR) | 171.0 (158.0-189.0) | 153.5 (142.2-176.7) | ||
| Min-Max | 116.7 - 230.0 | 119.2 - 222.9 | ||
| SD (mg/dL) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.159 |
| Mean ± SD | 48.3 ± 12.5 | 52.9 ± 12.8 | ||
| Median (IQR) | 47.0 (41.1-54.0) | 52.5 (45.2-59.5) | ||
| Min-Max | 30.0 - 72.0 | 30.0 - 75.0 | ||
| CV (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.009 |
| Mean ± SD | 28.1 ± 6.3 | 33.3 ± 5.4 | ||
| Median (IQR) | 28.1 (25.1-31.7) | 33.6 (28.5-38.0) | ||
| Min-Max | 16.3 - 41.6 | 24.4 - 41.3 | ||
| TBR2 (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.320 |
| Mean ± SD | 1.0 ± 1.5 | 0.6 ± 1.0 | ||
| Median (IQR) | 0.0 (0.0-2.0) | 0.0 (0.0-0.9) | ||
| Min-Max | 0.0 - 5.0 | 0.0 - 3.3 | ||
| TBR1 (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.747 |
| Mean ± SD | 3.1 ± 3.5 | 2.3 ± 2.6 | ||
| Median (IQR) | 1.0 (1.0-6.0) | 0.8 (0.6-3.2) | ||
| Min-Max | 0.0 - 10.0 | 0.2 - 9.5 | ||
| TBR (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.378 |
| Mean ± SD | 4.1 ± 4.8 | 2.8 ± 3.5 | ||
| Median (IQR) | 1.0 (1.0-8.0) | 0.8 (0.6-4.1) | ||
| Min-Max | 0.0 - 12.1 | 0.3 - 11.7 | ||
| TIR (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.005 |
| Mean ± SD | 55.7 ± 13.7 | 65.8 ± 15.6 | ||
| Median (IQR) | 58.0 (48.0-63.2) | 64.4 (58.0-77.6) | ||
| Min-Max | 23.0 - 82.0 | 33.1 - 93.9 | ||
| TAR1 (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.040 |
| Mean ± SD | 27.6 ± 9.0 | 23.3 ± 9.4 | ||
| Median (IQR) | 28.0 (25.0-33.0) | 26.2 (16.8-29.1) | ||
| Min-Max | 5.3 - 40.0 | 5.4 - 42.3 | ||
| TAR2 (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.023 |
| Mean ± SD | 12.6 ± 10.3 | 8.1 ± 9.8 | ||
| Median (IQR) | 12.0 (5.0-14.0) | 3.1 (2.2-12.0) | ||
| Min-Max | 0.5 - 43.0 | 0.0 - 38.6 | ||
| TAR (%) | Available Measures (%) | 17 (100.0%) | 17 (100.0%) | 0.015 |
| Mean ± SD | 40.3 ± 15.0 | 31.4 ± 16.3 | ||
| Median (IQR) | 39.0 (35.0-46.0) | 34.2 (19.8-41.3) | ||
| Min-Max | 5.9 - 76.0 | 5.4 - 66.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





