1. Introduction
Determining renal dimensions is one of the parameters to be considered during the ultrasonographic examination of the urinary system, as it could provide useful clinical information [
1,
2,
3,
4]. Some pathologic conditions, such as acute kidney disease, compensatory hypertrophy, portosystemic shunts, pyelonephritis, amyloidosis, hydronephrosis and neoplasia, can cause slight to severe nephromegaly [
2,
5]. Other conditions such as chronic kidney disease (CKD), congenital hypoplasia and renal dysplasia can determine slight to severe reduction [
2,
5]. In dogs, absolute renal measurements have poor diagnostic clinical value due to the considerable variation in body weight and conformation [
2,
3,
6]. To account for this variability, linear values of healthy kidneys, using body weight and conformations as variables, were proposed [
4]. Methods where the kidney length (KL) is compared to another anatomical structure have also been proposed [
7,
8]. In the method by Mareschal et al., the KL is divided by the aortic luminal diameter (AoD) [
7]. The proposed KL/AoD ratio method resulted in a wide range of normal cut-off values (5.5 – 9.1), resulting in possible overlap between healthy dogs and those with renal disease, consequently limiting the method's clinical usefulness [
2,
3,
9]. Furthermore, the method's efficacy in detecting dogs with CKD has not been established.
We hypothesized that the KL/AoD ratio is a method with high specificity but with a low sensitivity. The primary aim of this study was to investigate the clinical usefulness of the KL/AoD method in detecting dogs with clinical and laboratory results consistent with CKD. The secondary aims were to verify if the previously reported cut-off values [
7] were respected in our sample and to test the effects of variables such as side, body weight, and body size on KL, AoD and KL/AoD ratio in the healthy group.
2. Materials and Methods
2.1. Study Design
This study was prospective, single-institutional, analytical cross-sectional and reference interval in design [
10]. It received approval from the Clinical Ethical Review Board of the University of Napoli "Federico II" (PG/2023/PG0002892).
2.2. Ultrasonographic Examination Protocol
All the ultrasonographic (US) exams were performed at the Interdepartmental Centre of Veterinary Radiology of the University of Napoli "Federico II" with the patient in dorsal or lateral recumbency, using the same ultrasound device (MyLab Class C Vet, Esaote, Genova, Italy). A microconvex or linear, multifrequency electronic probe (model SC3123, 3.5 - 10 MHz and model LA533, 3 - 13 MHz, respectively, Esaote, Genova, Italy) was used depending on the ultrasonographer's preferences, which were mainly based on the best resolution achievable according to the patient's size. All the US exams were performed by the same operator (L.M.), a professor of veterinary radiology with more than 26 years of experience in ultrasonography. The operator was unblinded regarding the patient's clinical status and laboratory blood analysis results, if available during the exam. The KL/AoD ratio has been included in the institutional abdominal ultrasound examination protocol since May 2017 and has been assessed in all patients undergoing abdominal ultrasound using previously established methods [
7]. Briefly, the KL was determined in the dorsal plane, from a subcostal or intercostal acoustic window, depending on patient conformation, and measured on a still frame acquired when the distance between the two poles was maximum and with the renal pelvis clearly delineated. The aorta was assessed from the left flank, and images were acquired in a longitudinal scan just caudal to the root of the left renal artery. The measurements of the AoD were acquired at maximal luminal diameter, excluding the vessel walls, after reviewing the last frames using the cineloop function of the ultrasound device.
2.3. Exclusion Criteria
Exclusion criteria were as follows: (a) US exam performed by a different operator; (b) measurements of both KL and AoD not obtained at the time of the US examination; (c) images deemed to be of inadequate quality (e.g., borders poorly defined, blurred contours); (d) the patient had less than twelve months of age; (e) serum renal function test (creatinine and urea) were not collected within 48 hours before or after the US examination; (f) the patient was under sedation or general anaesthesia.
2.4. Data Recording
The images, signalment, history and clinical data (including serum creatinine and urea levels) of patients undergoing US examination of the abdomen between May 2017 and May 2023 were retrieved from the picture archiving and communication system (dcm4chee-arc-light version 5.11.1,
http://www.dcm4che.org) [
11] and institutional electronic medical record.
The KL and AoD dimensions (in centimetres), breed, sex, weight (in kilograms), age (in years) and results of serum creatinine and urea levels (both expressed in mg/dl) were recorded for each dog included in the preliminary sample in an electronic spreadsheet (Microsoft Excel version 16.52 2021, Microsoft Corp. Redmond, WA, USA). The decision on whether to include or exclude patients from the final sample was made by one of the authors (D.C.), a veterinarian with a Ph.D. in Veterinary Sciences and 5 years of expertise in ultrasonography.
After being included in the final sample, the same author divided dogs into two main groups: "healthy" and "diseased". The subjects included in the diseased group were required to have at least two consecutive tests with creatinine (threshold value of 1.4 mg/dl) and urea (threshold value of 60 mg/dl) levels above the reference values, with the last determination obtained within 48 hours before or after the ultrasound examination [
12]. Furthermore, dogs from the healthy group were subdivided into four sub-groups according to their body weight: toy (≤ 5.4 kg), small (5.5 – 10 kg), medium (10 – 25.9 kg) and large (≥ 26 kg).
2.5. Statistical Analysis
Statistical analyses were performed by one of the authors (D.C.), using commercial statistics software (Prism version 9.5.0 (525), GraphPad Software San Diego, CA, USA and MedCalc version 19.2.6, MedCalc Software Ltd, Ostend, Belgium).
The D'Agostino-Pearson test was used to assess data for normality, and the data were further analyzed according to their distribution. Descriptive statistics, including the mean or median, range (minimum to maximum), standard deviation (SD), and 95% confidence interval (C.I.) of the mean, were calculated for age, body weight, right kidney length (RKL), left kidney length (LKL), AoD, RKL/AoD ratio, and LKL/AoD ratio.
In the healthy group, differences between RKL and LKL were evaluated using the paired t-test and differences between the RKL/AoD and the LKL/AoD using the Wilcoxon signed-rank test. In the same group, differences in KL and AoD among toy, small, medium, and large dogs were assessed using the one-way analysis of variance (ANOVA) with Welch's correction, as variance results were significantly different at the F-test and further analyzed using the Dunnett's multiple comparisons post hoc test. Differences in the KL/AoD ratio were assessed using the Kruskal-Wallis test, and the results were further analyzed using Dunn's multiple comparison post hoc test. Furthermore, in the healthy group, the correlation between the body weight and KL, AoD, and the KL/AoD ratio was investigated using Spearman's rank correlation coefficient (rs) and simple linear regression.
Finally, in the healthy group, the reference range for the KL/AoD ratio was calculated according to the American Society for Veterinary Clinical Pathology guidelines for reference intervals [
13]. Outliers were automatically identified according to Reed et al., and then, data distribution was tested automatically with the D'Agostino-Pearson test [
14]. Reference lower and upper limits, corresponding to the 2.5th and 97.5th fractiles and the corresponding 90% C.I., were then calculated employing nonparametric methods following Clinical Laboratory and Standards Institute recommendations (CLSI C28-A3) [
15,
16].
Differences between healthy and diseased groups in KL and KL/AoD ratio were assessed using the Mann–Whitney U test. Finally, the diagnostic performance of the KL/AoD ratio to discriminate between healthy and diseased dogs was evaluated by receiver-operating characteristic (ROC) curves, following the method proposed by DeLong et al., to obtain the associated area under the curve (AUC) and Youden index (J = sensitivity + specificity−1). A J value < 0.2 indicates poor diagnostic performance, values between 0.2 and 0.5 indicate moderate diagnostic performance and values > 0.5 indicate good diagnostic performance [
17,
18,
19,
20,
21]. In all analyses,
p < 0.05 was considered statistically significant.
3. Results
Of the 1703 US exams performed in the considered period, 227 dogs met the inclusion criteria (87 males, 19 castrated males, 62 females, 59 neutered females). One hundred and eighty-five dogs (81.5%) (72 males, 16 castrated males, 54 female, 43 spayed females) were rated as healthy, and forty-two (18.5%) (15 males, 3 castrated males, 8 female, 16 spayed females) as diseased.
In the healthy group, the mean age was 8(±3) years, and the median body weight was 14kg (range 1.8 – 65 kg). In the diseased group, the mean age was 9(±4) years, and the median body weight was 18kg (range 3 – 35 kg). The absolute number of dogs and the number of diseased dogs for each breed included in the final sample are summarized in
Table S1. Descriptive statistics for RKL, LKL, AoD, RKL/AoD and LKL/AoD for both healthy and diseased groups are summarized in
Table 1.
In the healthy group, the paired t-test revealed no statistical differences between RKL and LKL (p = 0.29). Similarly, the Wilcoxon signed-rank test showed no statistical differences between RKL/AoD and LKL/AoD ratios (p = 0.05). Therefore, in the subsequent statistical analyses, the KL and KL/AoD ratios of the left and right sides were pooled together.
In the healthy group, based on their body weight, 30 (16.22%) were classified as toy-sized, 46 (24.86%) as small-sized, 69 (37.3%) as medium-sized, and 40 (21.62%) as large-sized. Descriptive statistics for KL, AoD and KL/AoD for each sub-group are summarized in
Table 2.
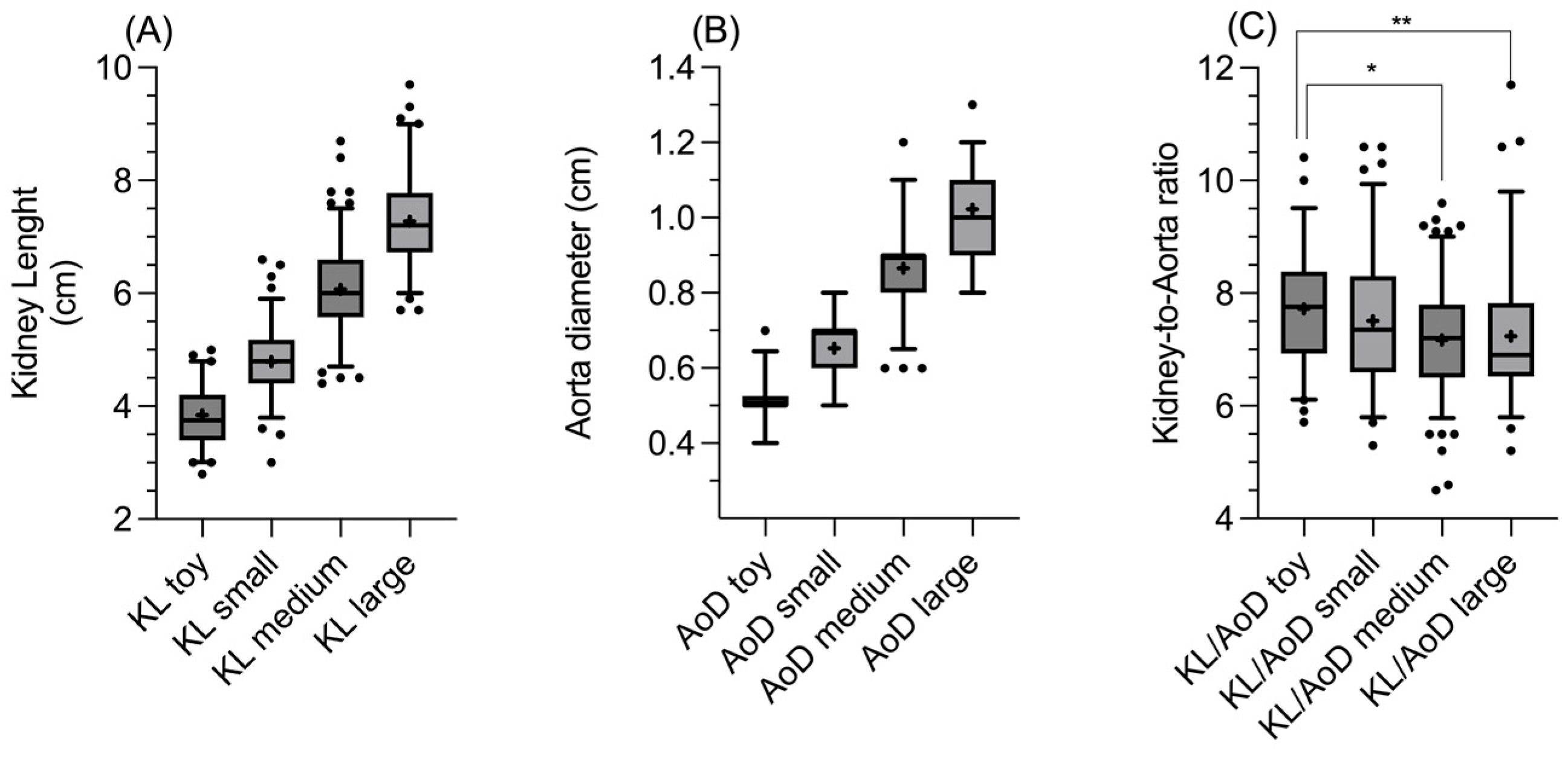
Furthermore, in the healthy group, the one-way ANOVA and Dunnett's multiple comparison tests revealed statistically significant differences among all the four different sub-groups considered for KL (all
p < 0.0001;
Figure 1A) and AoD (all
p < 0.0001;
Figure 1B). Similarly, the Kruskal-Wallis and Dunn multiple comparison tests revealed a statistically significant difference in the KL/AoD ratio between the toy and medium groups and between the toy and large groups (
p = 0.01 and
p = 0.009, respectively;
Figure 1C).
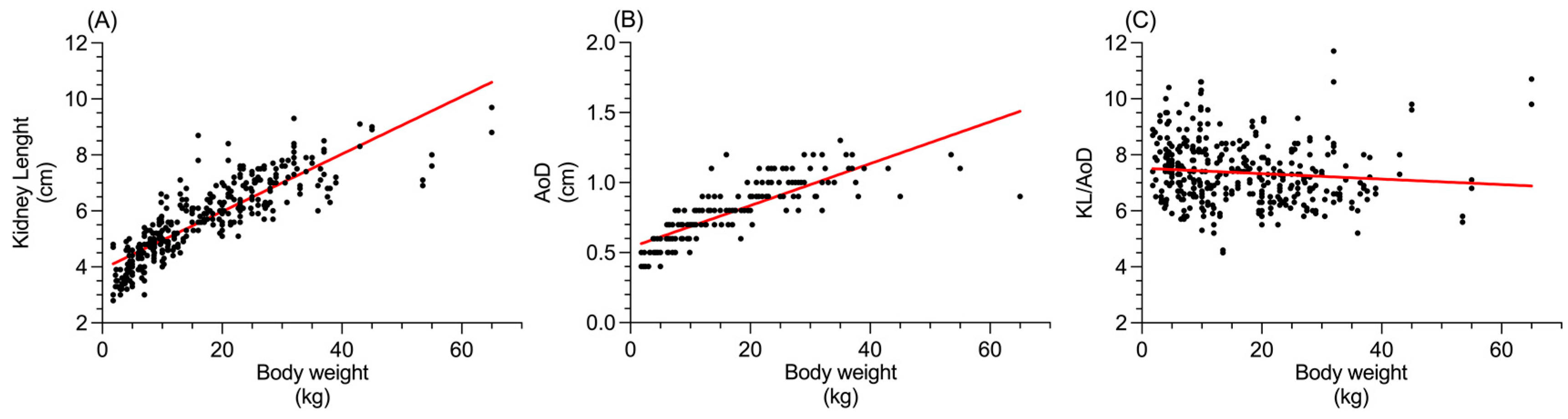
The Spearman's rank correlation coefficient revealed a positive correlation between the body weight and KL (
p < 0.0001; r
s = 0.89;
Figure 2A) and AoD (
p < 0.0001; r
s = 0.90;
Figure 2B), while a slight negative correlation was found between body weight and KL/AoD (
p = 0.0002; r
s = -0.19;
Figure 2C).
The reference intervals, median and range (minimum to maximum) with the relative 90% C.I. for the KL/AoD ratio in the healthy group are summarized in
Table 3.
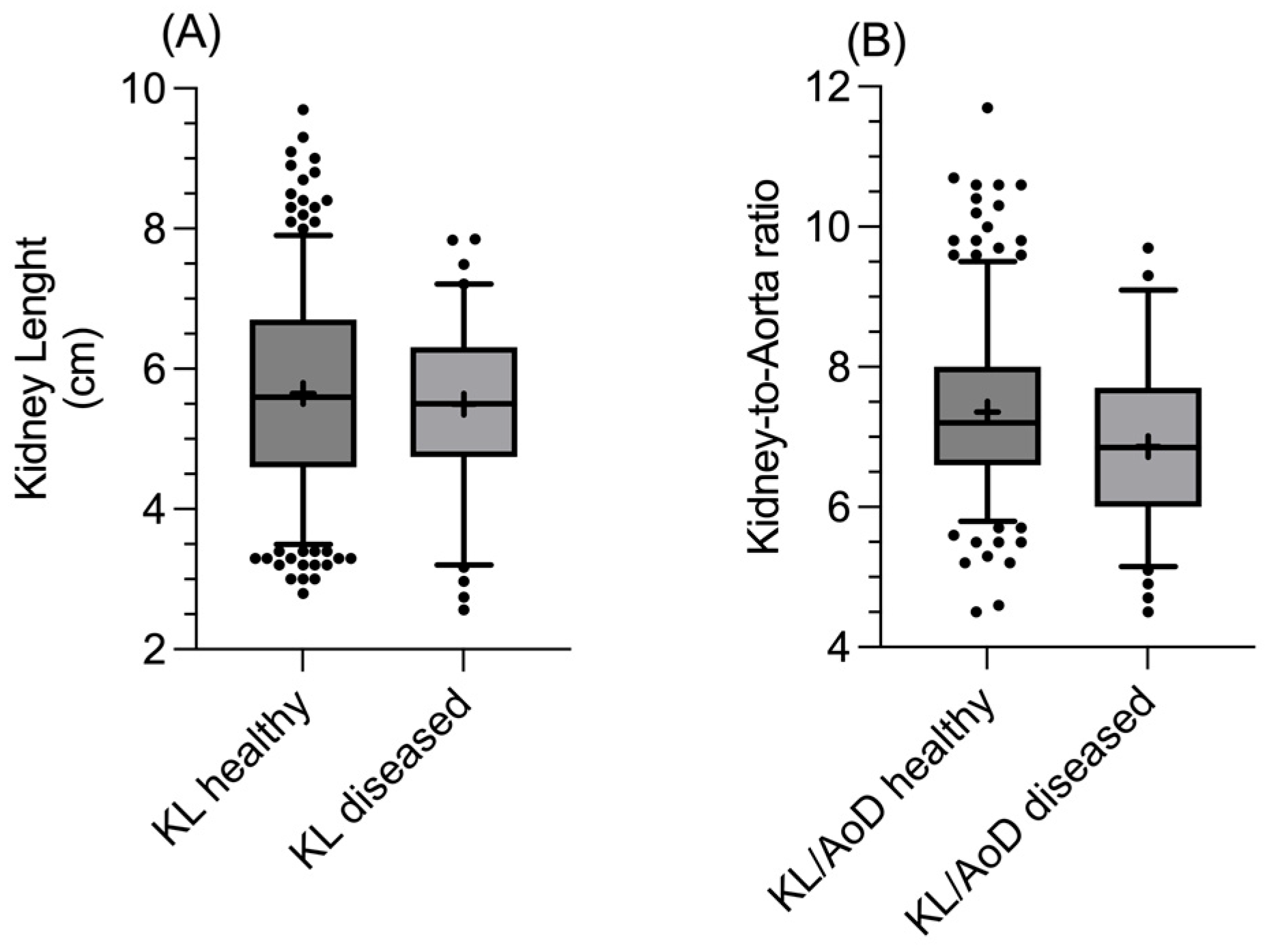
The unpaired t-test did not reveal significant differences in KL (
p = 0.53;
Figure 3A) and AoD (
p = 0.44) between healthy and diseased dogs, while the Mann–Whitney U test found significant differences between the two groups for the KL/AoD ratio (
p = 0.0003;
Figure 3B), with diseased dogs having overall lower values.
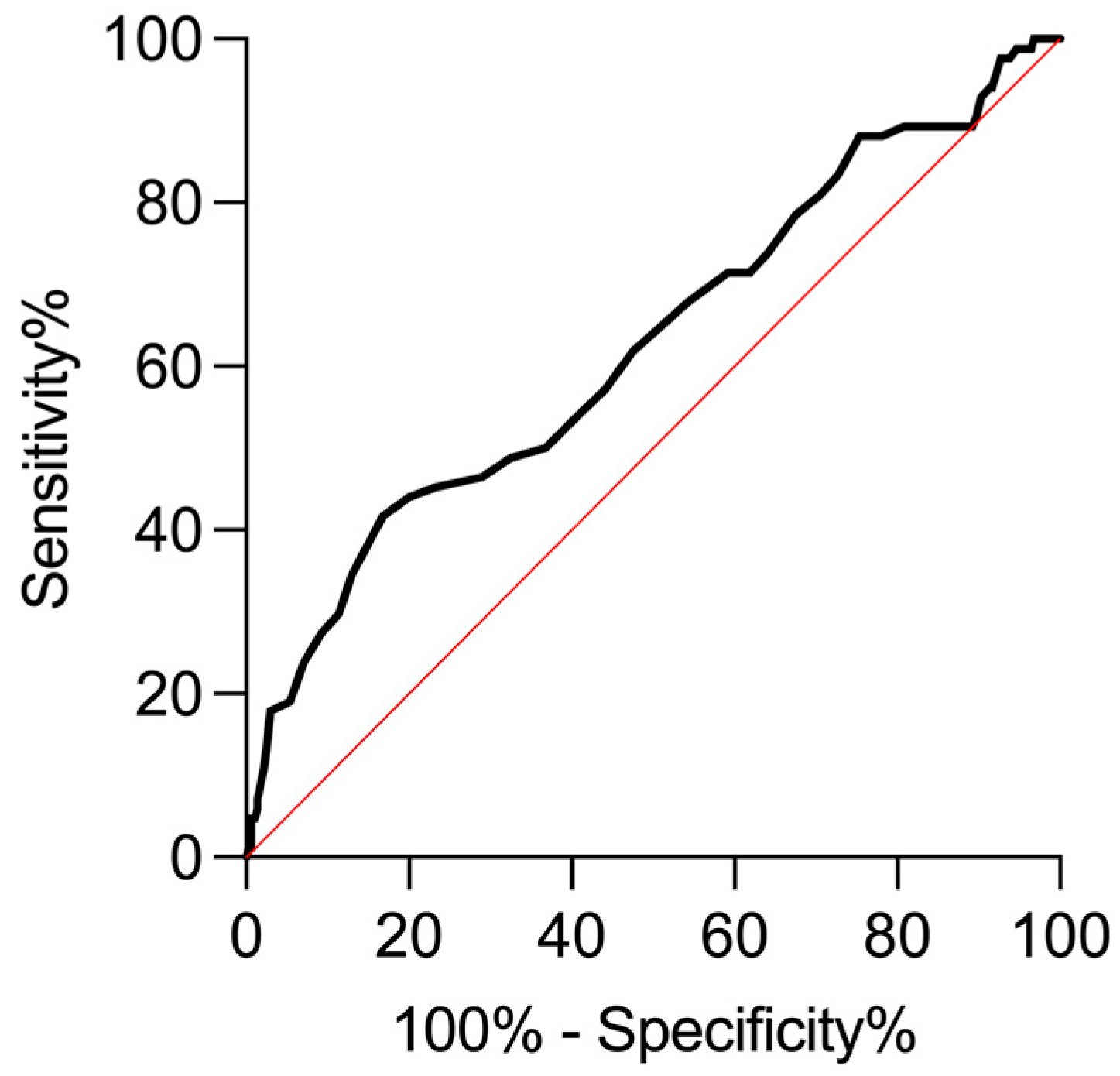
The generated ROC curve for the KL/AoD ratio (
Figure 4) displayed a fair AUC (AUC = 0.62; 95% CI: 0.55–0.69;
p = 0.0003) and a moderate diagnostic performance (J = 0.25), considering the Youden index at KL/AoD = 6.3, where the ROC curve showed a specificity of 83.24% (95% CI: 79.10% – 86.70%) and a sensitivity of 41.67% (95% CI: 31.71%–52.35%). For the lower value of the obtained reference range (KL/AoD = 5.6), the specificity increased to 97.57% (95% CI: 95.44%–98.72%), while the sensitivity decreased to 13.10% (95% CI: 7.47%–21.95%).
4. Discussion
This study evaluated the clinical usefulness of the KL/AoD ratio. It assessed the method's sensitivity and specificity by comparing the results obtained from healthy dogs with those with clinical and laboratory results consistent with CKD. The study's results supported our hypothesis.
The ROC curve demonstrated that for KL/AoD ratio = 5.6 (i.e. the obtained lower reference limit), the specificity is very high (97.57%), while on the other hand, the sensitivity is very low (13.10%). The diagnostic performance of the method was barely moderate considering the Youden index (which combines sensitivity and specificity into a single measure of diagnostic test effectiveness) at KL/AoD ratio = 6.3, where specificity remained excellent (83.24%) while, the sensitivity increased considerably (41.67%).
As expected, the comparison of KL between healthy and diseased dogs, without considering other variables, showed no significant differences, with overlapping values between the two groups. On the other hand, for the KL/AoD ratio, a statistically significant difference was found between healthy and diseased dogs, with the latter showing a lower median and 95% C.I. These results support using this method to normalize the renal dimensions among dogs of different sizes while also suggesting that dogs with CKD generally tend to exhibit a lower KL/AoD ratio. However, the KL/AoD ratio values obtained from the healthy and diseased groups overlap to a certain extent, limiting the clinical usefulness of the method in a clinical scenario. Indeed, dogs with initial CKD may not exhibit significant alterations in renal linear dimensions, causing partial overlap in the KL/AoD ratio values between the two groups and limiting the method sensitivity [
22]. The obtained sensitivity and specificity values result in low false positives, making it highly likely that subjects with values below the reference range are genuinely affected by CKD. Therefore, the authors retainx that the KL/AoD ratio is a valuable tool for confirming the diagnosis of CKD when clinical, laboratory, and additional ultrasonographic findings are consistent with the condition, allowing for greater diagnostic confidence while excluding other causes of elevated serum urea and creatinine levels, since these increase values are not exclusively indicative of CKD [
23].
From our results, and as expected, the KL/AoD ratio is not suitable as a standalone screening method for CKD due to the partial overlap of values between healthy and diseased subjects, which leads to low sensitivity, and many diseased subjects may present values within the range of healthy individuals (false negatives). The reference ranges in our sample for the KL/AoD ratio (i.e. 5.6 – 9.9;
Table 3) are broad and similar to those previously described (i.e. 5.5 - 9.2) [
7]. This wide range is probably related to the randomness of the sample, as it is proved that dogs of the same breed tend to have narrower reference intervals [
9].
To ensure the most accurate measurements, only images in which the cranial and caudal profiles of each kidney were clearly visible were included in the sample, and all measurements were taken during the examination rather than retrospectively. Although, in deep-narrowed chest dogs, the cranial profiles of the RK can be more difficult to delineate due to its subcostal position [
2], in the current study, similar to previous studies [
7,
8,
9] and differently from others [
4,
24,
25], there were no differences between RKL and LKL. Consequently, a single reference interval can be used for both kidneys.
In the original study by Mareschal et al., the AoD measurements acquired on longitudinal scans were more accurate than those acquired on transversal scans, showing a higher degree of inter-observer agreement [
7]. On the contrary, in a later study on growing puppies, the authors suggested acquiring the AoD on transverse scans since, according to them, those are less affected by motion artefacts [
25]. In a study that established the KL/AoD ratio reference interval in clinically healthy whippets, the authors did not find a significant difference between the two scanning planes [
9]. In the present study, the AoD was acquired on longitudinal scans since, according to the literature, transversal scans can be affected by refraction artefacts that can alter image quality [
26,
27]. Although the method proved to have a good inter-operator agreement in the original study [
7], we decided to include only the measurements performed by a single observer to limit the influence of this variable. Furthermore, we also decided to exclude from the final sample dogs that underwent US examination under sedation or general anaesthesia, as the different sedation/anaesthesia adopted protocols could affect blood pressure and, possibly, the AoD. Additionally, only adult dogs were included in the final sample because, as previously demonstrated, growing dogs, particularly those younger than six months, tend to have a higher KL/AoD ratio [
25], and consequently alter the reference values.
The further subdivision of dogs by body size (toy, small, medium, large) revealed significant differences between the groups in the KL and AoD. As expected, large dogs exhibited the largest dimensions for both KL and AoD. Interestingly, toy breeds showed statistically higher mean KL/AoD ratio values than medium and large breeds. This finding aligns with previous studies suggesting that renal dimensions tend to increase progressively with body size, though the rate of increase diminishes at the extremes of body weight, especially compared to aortic dimensions [
4,
28]. Consistently, in the present study, a positive correlation between body weight and KL was observed, though it became less pronounced at the higher extremes of body weight. These observations are further supported by the negative correlation between body weight and the KL/AoD ratio, confirming that at higher body weights, the AoD increases proportionally more than the KL.
The main limitations of our study include the lack of histopathological confirmation of the underlying cause of CKD affecting the dogs in the diseased group since this procedure is rarely performed at our institution. Although unlikely, it is possible that some dogs with altered serum urea and creatinine levels for causes unrelated to CKD were erroneously included in the diseased group.
A second limitation is the reduced number of dogs in the diseased group, resulting from our exclusion criteria where only dogs with a US study performed by the same operator and with laboratory analysis performed within 48 hours from the US study were included. This low number of subjects included in the final sample and the lack of additional data necessary for the staging of the CKD, such as symmetric dimethylarginine levels, urine protein to creatinine ratio and blood pressure, also prevented the staging of the dogs with CKD according to the IRIS guidelines [
12]. Indeed, it would be interesting to assess whether the KL/AoD ratio tends to decrease progressively in subjects with advanced stages of CKD. Another limitation was the lack of information regarding the dogs' hydration status and the presence of cardio-circulatory diseases that may alter the aorta distensibility and, thus, the KL/AoD ratio.
5. Conclusions
This study showed reference ranges for KL/AoD ratio similar to those previously described for a sample of mixed subjects. This range is broad and limits the clinical usefulness of the method, suggesting the determination and use of breed-specific ratios that may be narrower. In the general canine population, a KL/AoD ratio = 6.3, although higher than the lower cut-off value, has good specificity and acceptable sensitivity in confirming CKD in dogs with clinical, laboratory and additional US findings consistent with the disease. It must be kept in mind that the assessment of renal length and renal linear dimensions, in general, is only one of the parameters to be considered during the US exam of the renal system, and other alterations affecting the renal echotexture, echogenicity and perfusion must also be taken into account [
1,
2,
3,
22].
Further studies involving a larger cohort of subjects with confirmed CKD are needed to evaluate variations in the KL/AoD ratio. These studies should consider additional factors such as breed, systemic blood pressure, inter-observer variability, different stages of CKD, operator experience, and the effects of systemic blood pressure and hydration on the measurements.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1. Summary table of the dogs of each breed included in the final sample. The total number of dogs and the number of diseased dogs (in parentheses) are indicated
Author Contributions
Conceptualization, D.C. and L.M.; methodology, D.C. and L.M; software, D.C.; validation, D.C., E.C., P.C, C.S., M.P.P., M.M., G.G., A.G. and L.M.; formal analysis, D.C., and E.C.; investigation, L.M., A.G., D.C., P.C., E.C. and C.S.; resources, D.C., L.M., A.G., E.C., P.C., M.M and C.S.; data curation, D.C., E.C., P.C., L.M. and L.M.X.X.; writing—original draft preparation, D.C.; writing—review and editing, E.C., P.C., C.S., M.P.P., M.M., G.G., A.G. and L.M.; visualization, D.C.; supervision, L.M., A.G., M.P.P. and G.G.; project administration, D.C, L.M. and A.G.; funding acquisition, L.M. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The animal study protocol was approved by the Institutional Ethics Committee of the University of Napoli "Federico II" (PG/2023/PG0002892).
Informed Consent Statement
Informed consent was obtained from the owners of all subjects involved in the study.
Data Availability Statement
Anonymized data supporting reported results are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
List of abbreviations
ANOVA, analysis of variance; AoD, aortic luminal diameter; AoD, aorta luminal diameter; AUC area under the curve, C.I., confidence interval; CKD, chronic kidney disease; KL, kidney length; LKL, left kidney length; RKL, right kidney length; ROC receiver-operating characteristic; SD, standard deviation; US, ultrasonographic.
References
- Seiler, G.S.; Cohen, E.B.; d'Anjou, M.A.; French, J.; Gaschen, L.; Knapp, S.; Salwei, R.M.; Saunders, H.M. ACVR and ECVDI consensus statement for the standardization of the abdominal ultrasound examination. Vet Radiol Ultrasound 2022, 63, 661–674. [Google Scholar] [CrossRef] [PubMed]
- Widmer, W.R.; Mattoon, J.S.; Vaden, S.L. 16 - Urinary tract. In Small Animal Diagnostic Ultrasound (Fourth Edition), Mattoon, J.S., Sellon, R.K., Berry, C.R., Eds.; W.B. Saunders: St. Louis (MO), 2021; pp. 583–634. [CrossRef]
- d’Anjou, M.-A.; Penninck, D. Kidneys and ureters. In Atlas of Small Animal Ultrasonography (Second Edition). Wiley Blackwell 2015, 331-361.
- Barr, F.J.; Holt, P.E.; Gibbs, C. Ultrasonographic measurement of normal renal parameters. Journal of Small Animal Practice 1990, 31, 180–184. [Google Scholar] [CrossRef]
- Seiler, G.S. Chapter 41 - Kidneys and Ureters. In Textbook of Veterinary Diagnostic Radiology (Seventh Edition), Thrall, D.E., Ed.; W.B. Saunders: 2018; pp. 823–845. [CrossRef]
- Hecht, S.; Henry, G.A. Ultrasonography of the Urinary Tract. In Nephrology and Urology of Small Animals; 2011; pp. 128–145. [CrossRef]
- Mareschal, A.; d'Anjou, M.A.; Moreau, M.; Alexander, K.; Beauregard, G. Ultrasonographic measurement of kidney-to-aorta ratio as a method of estimating renal size in dogs. Vet Radiol Ultrasound 2007, 48, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Barella, G.; Lodi, M.; Sabbadin, L.A.; Faverzani, S. A new method for ultrasonographic measurement of kidney size in healthy dogs. J Ultrasound 2012, 15, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Costanza, D.; Pasolini, M.P.; Greco, A.; Mennonna, G.; Auletta, L.; Lamagna, F.; Meomartino, L. Ultrasonographic measurement of kidney-to-aorta parameters in Whippets. Vet Radiol Ultrasound 2021, 62, 476–482. [Google Scholar] [CrossRef]
- Scrivani, P.V.; Erb, H.N. Invited review: study design considerations for clinical research in veterinary radiology and radiation oncology. Vet Radiol Ultrasound 2013, 54, 317–325. [Google Scholar] [CrossRef]
- Costanza, D.; Coluccia, P.; Castiello, E.; Greco, A.; Meomartino, L. Description of a low-cost picture archiving and communication system based on network-attached storage. Veterinary Radiology & Ultrasound 2022, 63, 249–253. [Google Scholar] [CrossRef]
- International Renal Interest Society (IRIS) Ltd. IRIS Staging of CKD Staging of CKD - modified 2023. Available online: http://www.iris-kidney.com/pdf/2_IRIS_Staging_of_CKD_2023.pdf (accessed on 20 November 2024).
- Friedrichs, K.R.; Harr, K.E.; Freeman, K.P.; Szladovits, B.; Walton, R.M.; Barnhart, K.F.; Blanco-Chavez, J. ASVCP reference interval guidelines: determination of de novo reference intervals in veterinary species and other related topics. Vet Clin Pathol 2012, 41, 441–453. [Google Scholar] [CrossRef]
- Reed, A.H.; Henry, R.J.; Mason, W.B. Influence of statistical method used on the resulting estimate of normal range. Clin Chem 1971, 17, 275–284. [Google Scholar] [CrossRef]
- CLSI. Defining, Establishing and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline - Third Edition. CLSI document EP28-A3c 2008.
- Horn, P.S.; Pesce, A.J. Reference intervals: an update. Clin Chim Acta 2003, 334, 5–23. [Google Scholar] [CrossRef]
- Metz, C.E. Basic principles of ROC analysis. Semin Nucl Med 1978, 8, 283–298. [Google Scholar] [CrossRef] [PubMed]
- Metz, C.E. ROC methodology in radiologic imaging. Invest Radiol 1986, 21, 720–733. [Google Scholar] [CrossRef] [PubMed]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 1993, 39, 561–577. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Bragato, N.; Borges, N.C.; Fioravanti, M.C.S. B-mode and Doppler ultrasound of chronic kidney disease in dogs and cats. Veterinary Research Communications 2017, 41, 307–315. [Google Scholar] [CrossRef]
- Lefebvre, H.P. Renal Function Testing. In Nephrology and Urology of Small Animals; 2011; pp. 91–96. [CrossRef]
- Sohn, J.; Yun, S.; Lee, J.; Chang, D.; Choi, M.; Yoon, J. Reestablishment of radiographic kidney size in Miniature Schnauzer dogs. J Vet Med Sci 2017, 78, 1805–1810. [Google Scholar] [CrossRef]
- Kawalilak, L.T.; Pease, A.P.; Nelson, N.C. Evaluation of ultrasonographically determined ratios of kidney length to aorta diameter for assessment of kidney size in healthy young dogs. American Journal of Veterinary Research 2019, 80, 764–770. [Google Scholar] [CrossRef]
- Casella, I.B.; Presti, C.; Porta, R.M.; Sabbag, C.R.; Bosch, M.A.; Yamazaki, Y. A practical protocol to measure common carotid artery intima-media thickness. Clinics (Sao Paulo) 2008, 63, 515–520. [Google Scholar] [CrossRef]
- Pasolini, M.P.; Spinella, G.; Del Prete, C.; Valentini, S.; Coluccia, P.; Auletta, L.; Greco, M.; Meomartino, L. Ultrasonographic assessment of normal jugular veins in Standardbred horses. BMC Veterinary Research 2019, 15, 343. [Google Scholar] [CrossRef]
- Olesen, S.; Genster, H.G. Estimation of renal volume and function in dogs from the radiological appearance. Invest Urol 1970, 7, 363–370. [Google Scholar] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).